Introduction
Soft tissue sarcomas (STS) are tumours arising from the connective tissues of the human body. They commonly occur in the extremities and trunk wall but also can occur in the head and neck region, torso and retroperitoneum. Reference Hoekstra, Thijssens and van Grinkel1 They are a rare tumour comprising approximately 1% of all malignancies. Reference Hoekstra, Thijssens and van Grinkel1 There are many different histological subtypes of STS, with varying chemo- and radiosensitivities. One of these is myxoid liposarcoma (MLS), a particularly radiosensitive subtype that represents 10% of new STS diagnoses worldwide. Reference Antonescu, Ladanyi, Fletcher, Bridge, Hogendoorn and Mertens2,Reference Lansu, Bovée and Braam3
Sarcomas, including MLS, were classically treated by wide surgical excision due to their infiltrative nature, to prevent the risk of positive margins or microscopic residual disease. Reference Hoekstra, Thijssens and van Grinkel1,Reference Lansu, Bovée and Braam3 However, the development of limb-sparing compartment surgery, later wide-local excision, by Simon and Enneking (1976) Reference Simon and Enneking4 combined with radiotherapy (RT), has shown comparative outcomes in local control and survival. Pollack et al. (1998) Reference Pollack, Zagars and Goswitz5 compared the use of preoperative neoadjuvant radiotherapy (NART) and postoperative adjuvant radiotherapy (ART) suggesting that while they have comparative disease control, they differ in their post-RT impact with NART thought to have more acute complications and ART having late toxicity. NART became the preferred method due to the lower radiation doses and smaller fields required, as well as the reduction of long-term adverse impacts including fibrosis, joint stiffness and oedema which outweigh the risk of acute short-term wound complications (WC). Reference Callaghan, Hasibuzzaman and Rodman6 This was further investigated by a National Cancer Institute of Canada SR-2 randomised phase III clinical trial reported by O’Sullivan (2002) Reference O’Sullivan, Davis and Turcotte7 who presented a benchmark 35% WC rate following NART and defined a major WC as ‘secondary operation under anaesthesia or wound management without secondary operation—wound management includes invasive procedure without GA/regional (mainly aspiration), readmission for wound care such as IV antibiotics or persistent deep packing for 120 days or longer’. This study is a widely quoted reference standard for NART and STS research.
Wound complications have been long identified as a risk factor for poorer outcomes in oncological surgery. They are a poor prognostic factor for squamous cell carcinoma recurrence in head and neck cancers, Reference Jackson and Rice8 as well as breast cancer. Reference Murthy, Thomson and Dodwell9 There have been multiple studies into the risk factors for STS surgery and efforts to control the impact they have. However, WC are still common following resection.
Aims of the Study
The primary focus of this literature review was to investigate the current definitions and incidence of WC following NART and surgery for MLS. The secondary aim was to review a single surgeon series of MLS treated with NART followed by surgery between 2010 and 2022.
During initial scoping, a significant variance in the definitions used for WC and a lack of standardisation were noted. We wanted to investigate this further to see the impact this had on studies and propose a definition of major WC after NART and surgery.
Methods
Embase and Medline databases were searched using the terms ‘myxoid liposarcoma’, ‘preoperative radiotherapy (NART)’ and ‘wound complications’. No time limit was placed on publication date. This identified 30 papers, which were screened against inclusion criteria (myxoid liposarcoma, NART, wound complications) and exclusion criteria (non-English language papers, non-adult cohort, non-MLS and conference article only) resulting in 12 papers. A PRISMA Reference Haddaway, Page and Pritchard10 table demonstrated the process of identification of new studies (Figure 1).

Figure 1. PRISMA flow diagram
A retrospective review of a single surgeon series of 25 patients with MLS treated with NART followed by surgery was carried out after appropriate institutional approvals. All patients had a planned regimen of a Magnetic Resonance Imaging (MRI) scan and ultrasound-guided core needle biopsy for histological confirmation and staging studies, followed by 50 Gray (Gy) NART in 25 fractions. After completion of NART, MRI scans were obtained to assess response and for surgical planning. Preoperative anaesthetic assessment enabled appropriate prehabilitation. Surgery was typically performed 4–6 weeks following NART. All patients had 1·5 g of intravenous cefuroxime at the time of induction of surgery. All tumours were excised with clear margins, preserving maximal function. Early mobilisation was encouraged with appropriate physiotherapy support. The results (wound complication and reoperation rate) were compared with the reviewed literature.
Results
Rates of wound complications and reoperation in included studies
Table 1 demonstrates the rates of WC in the included studies. The average rate of complications was 29·8% (22–47%). There was a 7·7% (0–18%) reoperation rate in these studies. Three included studies were either literature, systematic or meta-analysis reviews of current knowledge. Slump (2019) Reference Slump, Bastiaannet and Halka17 included the total number of patients; however, Callaghan (2020) Reference Callaghan, Hasibuzzaman and Rodman6 and Roohani (2022) Reference Roohani, Ehret and Kobus16 did not include the number of patients within the reported studies.
Table 1. Rates of wound complications and reoperation in included studies

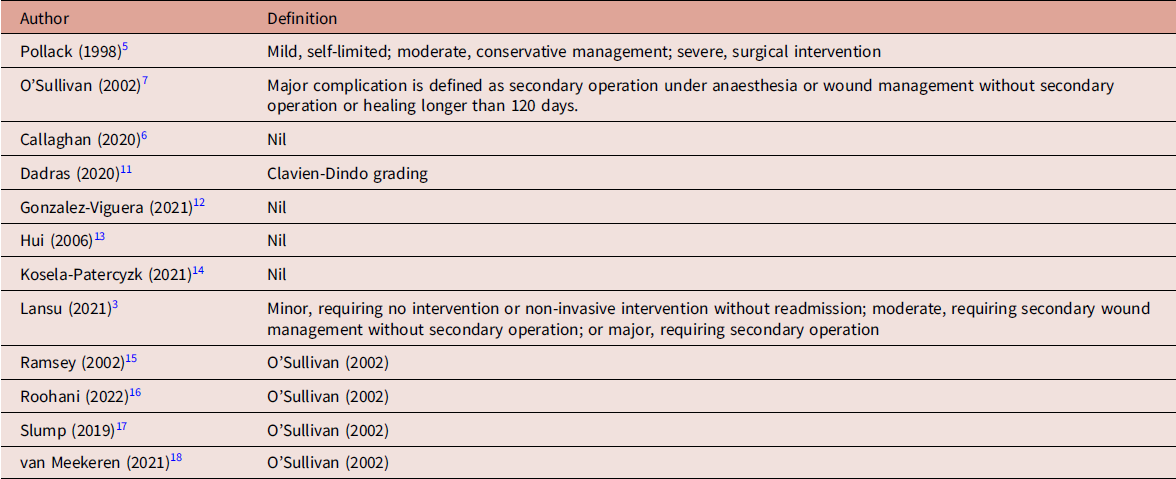
Varying definitions of major wound complications from literature review
Table 2 shows the range of definitions used for WC in the included studies. The five studies listing nil did not use any classification system or did not record any complications at all. Five studies used the O’Sullivan (2002) Reference O’Sullivan, Davis and Turcotte7 definition for a WC (including the original study). One study used the Clavien-Dindo Reference Dindo, Demartines and Clavien19 grading system. Pollack (1998) Reference Pollack, Zagars and Goswitz5 used their own definition for WC.
Table 2. Varying definitions of major wound complications from literature review
Results of single surgeon series
The single surgeon series was a collection of patients with MLS treated at a sarcoma centre between 2010 and 2022. Since 2010, all patients presenting with MLS were considered for NART, the outcomes of which can be seen in Table 3. Twenty-five eligible patients received 50 Gy in 25 fractions preoperatively before undergoing wide-local excision. The ages of included patients were 19–82 years (50 years). Surgery was performed 4–6 weeks following NART completion. All included patients had pre- and post-RT MRI. Twenty-three patients had tumours of the lower limbs, with a size range of 3–30 cm (8·4 cm). Tumour necrosis was identified in 19 patients via histology. Average tumour necrosis was 58% (0–100%), and all surgical excisions had clear margins.
Table 3. Results of single surgeon series

WC, wound complications; LR, local recurrence; BMI, body mass index.
Two patients (8%) had WC. One patient (body mass index (BMI) of 38) underwent excision of a 6 cm MLS of his proximal thigh/groin. He presented 2 weeks later with a discharging wound. There were no microbiological organisms identified. The wound was regularly dressed, and the wound healed by secondary intention at 114 days. The second patient underwent excision of an 8 cm MLS of her lateral thigh/buttock. The wound looked healed at the 2-week review. However, she flew to a holiday destination 3 weeks following surgery and developed a leaking seroma. The wound was regularly dressed by packing the wound cavity, and the wound was found to have healed at 120-day review. Neither patient required readmission or reoperation.
In Table 3, you can see this compared to the average identified in 1·4·1 Table 1. The average follow-up was 64 months (9–120 months). There was one (4%) local recurrence in this cohort and 20 (80%) are still alive. Five patients developed metastases, and of these, one patient is still alive.
Discussion
O’Sullivan Reference O’Sullivan, Davis and Turcotte7 in his 2002 paper gave specifics to what would count as a ‘major wound complication’ as well as a time limit of 120 days for prolonged healing. This was an improvement on the definition that Pollack (1998) Reference Pollack, Zagars and Goswitz5 used, describing only mild, moderate and severe based on the intervention required—conservative, medical or surgical management. This was a necessary adaptation as more modern interventions such as radiological drainage would not fit into the original categories. The O’Sullivan definition is one of the most used classifications within sarcoma surgery and NART, and is the most commonly used classification within the reviewed literature.
This is compared to the other studies included in the review which simply listed the complications that occurred. The 2021 Gonzalez-Viguera Reference González-Viguera, Reynés-Llompart and Lozano12 paper investigated the role of radiomic features in the prognostication for sarcoma surgery. It reported a 20% complication rate from 25 total patients. The complications described state ‘dehiscence’, ‘infection’ and ‘septic shock’ without going into further detail about the complications described and did not provide a time limit for included complications. Hui (2006) Reference Hui, Ngan and Wong13 in a single centre series of 67 patients also only reported the complications that occurred. Forty-one percent of the included patients suffered a wound complication. This included minor and major dehiscence, but it was not clearly defined what separates these two criteria. Three percent of patients suffered from ‘delayed healing’ in the Hui study, but it was not reported what time limit was used for this. The study by Kosela-Patercyzk (2021) Reference Koseła-Paterczyk, Teterycz and Spałek14 which investigated hypofractionation radiotherapy listed the complications included. Twenty-four percent of the 311 included patients suffered an acute WC. The authors defined prolonged healing as longer than 1 month (30 days) and provided data on reoperation, with 7·3% of patients requiring secondary surgery. It is not clearly shown what the indication was for secondary surgery or the procedure that was performed. Lansu (2021) Reference Lansu, Bovée and Braam3 reported the Dose Reduction of Preoperative Radiotherapy in Myxoid Liposarcoma (DOREMY) trial, a multicentre prospective trial investigating hypofractionation NART for MLS. They reported a 22% total WC rate under their own definition of ‘minor, requiring no intervention or non-invasive intervention without readmission; moderate, requiring secondary wound management without secondary operation; or major, requiring secondary operation’. Alongside the lack of standardisation of definitions, prolonged healing was not included as a complication.
Dadras (2020) Reference Dadras, Koepp and Wallner11 was the only recent study to use an alternative standardised method of classification. The Clavien-Dindo classification system Reference Dindo, Demartines and Clavien19 was originally designed by Clavien in 1992 and expanded by Dindo in 2004 with the aim to create a broad quality assessment tool for use in any part of the world by any grade of trainee. While it is a thorough assessment tool, it does not provide a time limit for which complications can occur, unlike O’Sullivan who used 120 days. Similarly, it does not include prolonged wound healing as a complication. The complications it was originally assessed against were complications suffered by patients of general surgeons and not orthopaedic surgeons. Dadras does make an interesting statement that ‘most risk factors for wound complications are inherent to the patient cohort (morbidity) or due to the disease (stage or operative time) and less to do with surgical practice’.
Callaghan (2020) Reference Callaghan, Hasibuzzaman and Rodman6 focused on the pathophysiology of wound complications. They detailed the current literature on the physiology of normal wound healing and pathophysiology of wound complications. It discusses how radiotherapy increases the activity of reactive oxygen species and pro-inflammatory cytokines causing fibrosis and cell death. A greater understanding of the pathophysiology involved in complications and delayed healing will allow improved techniques for improved outcomes.
There have been attempts to identify risk factors for WC. A systematic review and meta-analysis by Slump (2019) Reference Slump, Bastiaannet and Halka17 assessed 21 studies, including 5,628 patients. WC rates were reported in 18 studies and varied from 17·6 to 48%. Meta-analyses identified an overall rate of 30·2%. Smoking, diabetes status and obesity were found to be the highest patient risk factors; however, there is a broad range of methodology used by the included studies and a lack of uniformity in the reporting of outcomes and definitions. Lower limb tumours were found to be the highest tumour-related risk factor, but there was a lack of consistency of what was counted as ‘lower limb’ as some groin/gluteal areas were included. Finally, the timing of surgery following RT remains controversial, alongside variation in practice, making direct comparisons challenging.
One potential route to minimise the rates of WC is to minimise the impact of radiotherapy. STS, particularly MLS, has historically been treated with 50 Gy in 25 fractions, described as normofractionation. Hypofractionation uses reduced radiotherapy doses and duration of treatment. Roohani (2022) Reference Roohani, Ehret and Kobus16 systematically reviewed hypofractionation in patients with high-grade STS. 25 Gy in 5 fractions (5×5 Gy) was found to have no change in rates of adverse events compared to historical normofractionation regimens and found a comparative local controls rate with a reduced duration in therapy. It also discussed the benefits of hypofractionation due to the reduced impact on patients and economic advantage. The WC rates within these studies were comparable to normofractionation reported rates. Kosela-Patercyzk (2021) Reference Koseła-Paterczyk, Teterycz and Spałek14 who investigated the same 5×5 Gy regimen had similar outcomes. They also suggest the difference between radiotherapy modalities, such as Intensity Modulated Radiotherapy (IMRT) used by modern studies, and the conventional external beam therapy used by O’Sullivan could impact wound complication rates. The DOREMY trial reported by Lansu (2021) Reference Lansu, Bovée and Braam3 investigated an alternate hypofractionation regime of 36 Gy in 18 fractions with comparable outcomes to normofractionation rates.
Ramsey (2022) Reference Ramsey, Walker and Wetzel15 investigated if broadening antibiotics prophylaxis for STS to include anaerobic cover lowered the risk of WC. Patients who were treated with a first-generation cephalosporin were compared with a group who received cephalosporin plus metronidazole. Twenty-seven percent of patients receiving cephalosporin only developed WC, as opposed to 17% in the combined group, using the O’Sullivan (2002) definition. The overall WC rate was 26%. The retrospective nature and small patient numbers make comparing this data challenging.
The single surgeon series found a major WC rate of 8%, and no patients required readmission or reoperation. Though it is not possible to compare varying historic patient cohorts in the literature, the single surgeon series experience indicates that NART-related WC may not be as high as the reported literature. Many factors, though speculative, may help to improve outcomes for patients and reduce WC. Prior to surgery, using prehabilitation to correct anaemia and improve nutritional status, alongside early home recovery once medically fit, may help to improve outcomes. Allowing a suitable time length (4–6 weeks) following NART to allow the skin to recover, without allowing fibrosis to develop, is also a key factor in optimising wound healing. Utilising antibiotic prophylaxis at induction, excising adequate ellipse of skin for large tumours to reduce potential seroma cavity and reducing any dead space following removal of the tumour, alongside meticulous wound closure, are also important. Postoperatively, drains should not be removed until less than 50 mL per 24-hour period, with the avoidance of chemical venous thromboembolism (VTE) prophylaxis alongside this (unless history of VTE with preference to mechanical VTE prophylaxis and early mobilisation). The location of the tumour (the groin and buttock), high BMI and long-distance flight travel following surgery may have contributed to the two major WC seen.
The main area requiring improvement that was identified in this review was the lack of standardisation. Having a standardised definition of WC may improve the quality of reporting from future studies. From our study and series review, we propose an updated definition of a major WC—the occurrence of any/all of the following may be classified as a major WC:
-
1) Any repeat surgery for wound treatment requiring local or general anaesthetic including debridement, operative drainage, secondary or repeated wound closure including any free tissue transfer or skin graft
-
2) Any invasive procedure with/without anaesthesia including aspiration
-
3) Inpatient treatment for wound infection—for example, intravenous antibiotics
-
4) >120-day treatment with wound dressing materials
However, international consensus may be required to validate the proposal.
The predominant difficulty with sarcoma studies is the rarity of the disease. This results in high variability in practices across sarcoma centres. Alongside this, each subtype reacts differently to treatment, so there is no one-size-fits-all approach to this disease. Due to this, there is a large amount of retrospective cohort studies. There is also a lack of standardisation of definitions used in relation to NART, surgery and STS, causing a large amount of physician bias in clinical management. One example of this is what is counted as ‘lower limb’ with several studies including buttock tumours and several others excluding them. The single surgeon series is a retrospective study selectively evaluating MLS, a subtype of a radiosensitive STS, while the comparative literature includes multiple subtypes. It is also difficult to define the factors from a surgeon’s practice, alongside patient comorbidities, which may have influenced primary wound healing.
Conclusion
This literature review identified that there was a lack of consistency between the definitions used for major wound complications and period. The single surgeon series showed that major wound complications were lower than reported literature. An updated definition is proposed for the evaluation of major wound complications in relation to NART and surgery.
Financial support
No financial support.









