LEARNING OBJECTIVES
After reading this article you will be able to:
• explain the concept of risk as it applies to clinical practice
• recognise that risk assessment is much more than gathering and interpreting information to make judgements about future harm
• understand the wider psychological, interactional and system influences on risk assessment in a way that informs better practice.
Clinical risk assessment in the field of mental health is usually conceptualised as a process carried out by clinicians which involves the explicit analysis of pertinent information about a patient to reach a judgement on whether the patient will go on to act in a way that is harmful to themselves or others. This conceptualisation imagines an objective process disconnected from the real-world context in which the assessment occurs. A more informed perspective should delineate the way such judgements may be reached and the influence on doing so of the wider context in which the clinical encounter occurs. This article offers such a perspective in a way that encourages clinicians, organisations and researchers to approach risk assessment differently.
The risk assessment framework described below starts with a description of information gathering. The risk assessor needs to be familiar with factors that have been found to be associated with harm to self or others. These have been described extensively elsewhere (e.g. American Psychiatry Association 2016; Franklin Reference Franklin, Ribeiro and Fox2017) and will not be rehearsed here. The focus of this article is more on how this information should be interpreted in the context of making clinical decisions, and the importance of recognising the impact of broader interpersonal and organisational issues on the day-to-day practice of risk assessment (Fig. 1). Drawing on the empirical evidence base and on clinical experience, we will demonstrate that clinical risk assessment should not be seen as an objective analysis of risk factors to make a prediction about whether or not the patient is going to harm themselves or others in order to decide what to do to prevent that outcome. Rather, it should be seen as a process of gathering and interpreting information in the context of interpersonal relationships to guide collaborative decision-making that aims to improve patient well-being while reducing the likelihood of harm to self or others.
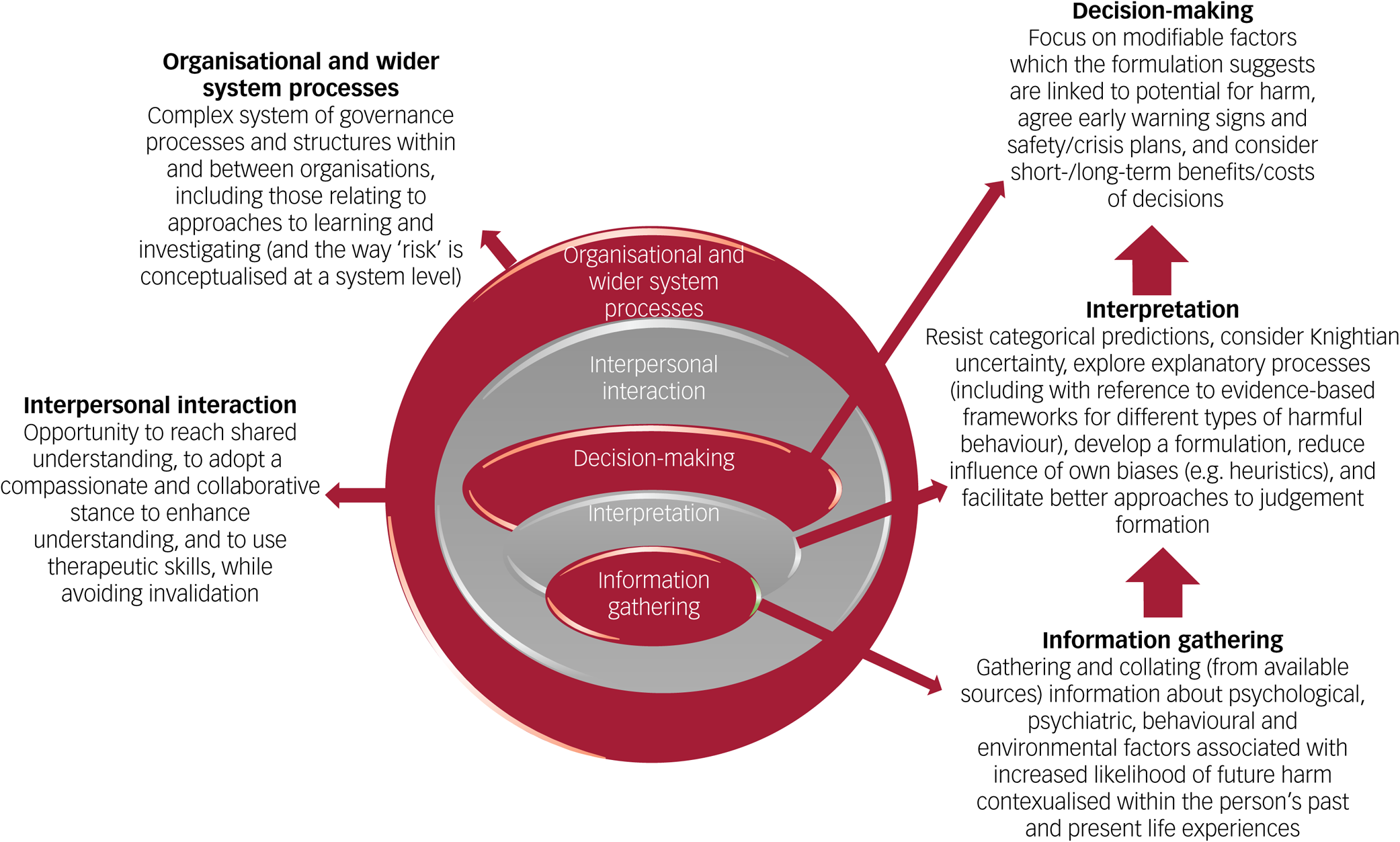
FIG 1 Risk assessment framework.
Case vignette
In academic and practice guidance the notion of risk is often examined in a way that is somewhat removed from real-world clinical practice (Nathan Reference Nathan, Gabbay and Boyle2021b). Key points raised in this article will be examined with reference to practice by using a case vignette that involves possible future harm. Rather than presenting only a patient profile, the following vignette describes a broader set of processes that are often neglected in risk assessment guidance and research and that will be explored in this article.
At the request of the hospital medical team, a liaison psychiatry practitioner Amy assessed Tom, a 37-year-old male who had been deemed medically fit following treatment for an overdose of medication and alcohol. Amy elicited a history of alcohol misuse, depressive symptoms and relationship breakdown. Tom said that he wanted to come into hospital for help to stop drinking. On the basis of her assessment of Tom's ongoing depressive symptoms, his social isolation and the level of his hopelessness and despondency, Amy was concerned about the risk to self and she thought that a brief crisis admission should be considered even though she was mindful that there were no vacant beds in the local psychiatric unit. Nevertheless, according to the local protocol for patients thought to need hospital admission, Amy made a referral to the home treatment team that acted as the ‘gatekeepers’ for acute in-patient services. A member of that team undertook an assessment and concluded that the primary problem was alcohol misuse, which was not a reason for admission to a psychiatric unit. When this was explained to Tom, he became angry and he said that if he was not admitted to hospital he would go out and throw himself off a motorway bridge.
Meaning of risk and related concepts
Risk
To effectively undertake risk-related activities (such as risk assessment and management), we need to be sure that we agree on the meaning of the term ‘risk’. Formal definitions of risk in the context of mental health service provision refer to a future harmful event and generally incorporate its severity, imminence and likelihood or probability. However, we cannot take for granted that the notion of ‘risk’ is applied consistently in clinical practice. A phenomenological analysis of the Royal College of Psychiatrist's report on the assessment and management of risk to others (Royal College of Psychiatrists 2016) found that ‘risk’ was used in a way that conveys variable meanings (e.g. harm, the possibility of harm, characteristics of possible harm, a state with changeable potential for harm, and different states of potential harm) (Nathan Reference Nathan, Gabbay and Boyle2021b). Given the potential for protean interpretations of ‘risk’, we believe it is essential that clinicians, academics and authors of practice guidance are clear about their use of this term. In this article, the term risk is used to describe the ‘possibility of harm’. This conveys that something may occur without necessarily suggesting that it is likely to occur (i.e. it is ‘possible’ but not necessarily ‘probable’) and it leaves room for the further characterisation of the possibility.
To be able to characterise future harmful events, it is first necessary to commit to the types of event under consideration. Guidance does not usually describe this step, but it would seem reasonable to at least consider types of harm suggested by expressed intentions (e.g. Tom's statement about throwing himself off a bridge), a recurrence of harm that has occurred before (e.g. an overdose), other forms of the same category of harm (i.e. other suicidal behaviours) and other categories of harm given a particular mental state (e.g. harm to others linked to Tom's angry hostility). Risk assessment convention dictates that the possibility of any identified plausible future harmful events occurring should be delineated. Therefore, clinicians need to understand different ways of describing the delineation (Box 1) and ensure that their use of a chosen descriptor is valid.
BOX 1 Meaning of risk, prediction, probability and related terms
Risk – The possibility of harm
Prediction – A commitment to a specified future outcome
Probability:
• Classic probability – The fraction of the total number of possibilities of equal likelihood in which the outcome occurs
• Frequentist probability – The frequency of an outcome over a long-run series of event occurrences
• Subjectivist probability – The degree of belief that a specified outcome will occur
Uncertainty – Known and unknown characteristics of the future in which the outcome occurs
Propensity – A property that is causally responsible for the long-run frequency
Prediction
A judgement about whether an event may occur in the future could be presented as a dichotomous prediction, i.e. that harm will or will not occur. Alternatively, judgements about the future could be categorised (e.g. low, medium or high risk). However, such categorical approaches have limited utility in informing clinical decisions so as to meaningfully reduce infrequent high-harm events (Mulder Reference Mulder, Newton-Howes and Coid2016).
Classic probability
The chance of a possible event occurring can also be characterised in terms of probability, which is used to describe the relative frequency of an event. This classic interpretation of probability is the fraction of the total number of possibilities of equal likelihood in which the event occurs (e.g. a 1/6 probability of tossing a three with a fair die). Since the assessment of possible future harm in clinical scenarios such as the case vignette described above does not involve a fixed number of outcomes of equal likelihood, classic probability is not applicable.
Frequentist probability
A related interpretation of probability is the frequentist view, which represents probability as a ‘long-run frequency over a large number of repetitions of an experiment’ (Blitzstein Reference Blitzstein and Hwang2019). This would produce the same probability of tossing a three with a fair die, but it could also be used to reach an informed probability for an outcome when rolling an unfair die (i.e. where the possibilities are not equally likely). Clinical scenarios such as the one presented in the vignette are unique instances that cannot be replayed. Thus, even putting aside the obvious ethical objections, allowing a series of instances to play would not be the same as rolling the same die in an unchanging environment. Therefore, frequentist probability is meaningless in a unique clinical situation. However, there remains a question about the applicability to practice of data-sets from comparable groups of patients. For instance, in relation to a discrete outcome such as suicide, one could use the positive predictive value of a suicide risk assessment model derived from group-level data as the probability of a patient identified as ‘high risk’ subsequently dying by suicide. However, once it is recognised that a patient presentation at a point in time is a unique instance and that the patient's future will be influenced by a unique set of countless environmental and psychological factors in constant interplay, the limitations of using a data-set to inform decision-making in a single clinical encounter become apparent (Nathan Reference Nathan, Gabbay and Boyle2021b).
Uncertainty
Economists have long recognised that probability in the classic or frequentist sense cannot be used for decision-making in the context of a single unique instance (Sakai Reference Sakai2016). Frank Knight reserved the term ‘risk’ for those scenarios in which the probability distribution of the outcome is known, and instead used the term ‘uncertainty’ for those scenarios in which the situation is so unique that probability distributions are not available (Sakai Reference Sakai2016). Critically in the context of mental health risk assessments, Knightian uncertainty seems more applicable since we cannot reliably distinguish what will occur from what will not occur. This uncertainty has two underlying components: epistemic uncertainty, resulting from a lack of knowledge, and aleatory uncertainty, resulting from random or chance events (Large Reference Large, Ryan and Carter2017). If it is accepted that one cannot accurately determine much of what is going to happen in the future (including events that might have a bearing on the occurrence of harm-related outcomes), then it follows that much of the uncertainty about a particular future harm-related outcome is aleatory (Large Reference Large, Ryan and Carter2017). The vignette illustrates that in such clinical settings the uncertainty arises in a scenario involving agents making interdependent choices with strategic dimensions. This raises as yet unanswered questions about whether game theory modelling might offer greater insights into likely outcomes. To do so, account would need to be taken of the role of emotions in decision-making.
Subjective probability
Another interpretation of probability that does not rest on an imagined or actual series of trials is subjective probability. In this case, probability is conceptualised as a feature of the person undertaking the assessment rather than of the real world and is quantified on a scale of the degree of belief (Biedermann Reference Biedermann, Bozza and Taroni2017). For instance, in the case vignette above, Amy felt that Tom should have a brief crisis admission, whereas the home treatment team practitioner felt otherwise. This discrepancy in opinion could be understood as arising owing to differences in both Amy's and the home treatment team practitioner's prior assumptions. Amy may have recently seen a very similar patient who subsequently died by suicide, therefore leading her to believe that Tom is presenting as higher risk warranting admission.
Propensity
One may also consider the properties of the entity that are causally responsible for the long-run frequency (such as the physical property of a rolled die). This is known as propensity. The propensity notion has advantages over the frequentist perspective because it can be used for a single event. Its use in mental health scenarios would also encourage a focus on the mental processes (the properties that are causally responsible for action) and, by extension, on consideration of factors that might influence these processes. In this way, talk of propensity shifts the focus from abstract disembodied concepts (such as probability) to the mind of the person.
Risk assessment framework
Information gathering
Risk assessment should not be seen as a stand-alone clinical activity. It is heavily dependent on a comprehensive psychiatric assessment, which involves integrating information from an interview with, and examination of, the patient together with data from other sources (e.g. personal and professional informants, and the available records). Certain parts of that assessment are especially pertinent to judgements about the possibility of harm. These include psychological, behavioural or environmental occurrences, which have been found in group-level quantitative studies to be associated with an increased likelihood of future harm to self or others (American Psychiatry Association 2016; Franklin Reference Franklin, Ribeiro and Fox2017). For instance, these studies have demonstrated that some of the elements contained in the case vignette are associated with an increased likelihood of suicide: these include a history of overdose, comorbid psychiatric disorder, alcohol misuse, relationship breakdown and feelings of hopelessness.
Special attention should be given to the characteristics of violent or suicidal ideation (e.g. frequency and intensity) and associated behaviours (e.g. intent, planning, actions) (Borges Reference Borges, Nazem and Matarazzo2019). Suicidal ideation refers to thoughts about ending one's life, which may be categorised as ‘active’ (i.e. thoughts, and a plan, to die) or ‘passive’ (i.e. thoughts to die, but no plan) (Turecki Reference Turecki, Brent and Gunnell2019). Although the clinician should pay attention to any statements suggesting a pattern of thinking, feeling and planning that is relevant to the potential for future harmful actions, it should also be recognised that internal experiences relevant to future actions are not experienced as circumscribed and unchanging entities in the way descriptors such as active or passive ideation suggest. Similarly, taking a phenomenological approach to explore mind-based correlates of disturbed behaviour is likely to lead to a more fine-grained and case-specific causal understanding of the behaviour than is possible when working just at the level of diagnosis or symptoms (Nathan Reference Nathan, Whyler and Wilson2020).
If an assessment entailed merely compiling a list of case-based factors that theoretically may increase the likelihood of a high-harm outcome, it would be of limited use for decision-making in an individual scenario (American Psychiatric Association 2016). Instead, the relevance of these factors should be understood in the context of the person's current experiences and triangulated with other sources of information, such as a collateral history from a family member. Moreover, the assessment should attempt to uncover underlying psychosocial processes that explain how the factors interact to influence this person's behaviour (as explained below).
Interpretation
Despite the identification of factors that predict suicide or serious violence, it has not been possible to translate this literature into clinically useful predictive tools (Mulder Reference Mulder, Newton-Howes and Coid2016). Although a meta-analysis of prospective studies predicting suicide following self-harm found four risk factors with robust effect sizes (previous self-harm, suicidal intent, physical health problems and male gender) they were ‘unlikely to be of much practical use because they are comparatively common in clinical populations’ (Mulder Reference Mulder, Newton-Howes and Coid2016). The study's authors, who also reviewed a range of risk scales, concluded that ‘the idea of risk assessment as prediction is a fallacy and should be recognised as such’. Another meta-analysis concluded that no unique set of risk factors could be reliably linked to an outcome of suicide, with predictive ability found to have not improved over the past 50 years (Franklin Reference Franklin, Ribeiro and Fox2017). There are a number of reasons. First, risk factors are non-specific and are shared by many individuals; for instance, the presence of mental illness is considered a risk factor for a suicide, despite the fact that most people with mental illness will not die by suicide (Franklin Reference Franklin, Ribeiro and Fox2017). Second, suicide risk is influenced by a complex combination of interacting factors, with each individual factor only having a weak association with the rare outcome of suicide (Zortea Reference Zortea, Cleare and Melson2020). Third, although clinicians are tasked with determining risk over periods of hours or days, most studies are not focused on acute or short-term prediction and therefore, unsurprisingly, longer follow-ups within studies did not improve prediction power and, in some cases, significantly weakened it (Ribeiro Reference Ribeiro, Franklin and Fox2015). It should be mentioned, though, that a case has been made for the use of probability scores from a risk assessment tool to complement an individual needs-based assessment, although how the clinician uses the scores requires further empirical examination.
Believing that it is possible to categorise patients accurately may even be harmful. Potential problems include unnecessarily applying more restrictive approaches to all those categorised as ‘high risk’ and directing resources away from the ‘low-risk’ groups despite these groups containing most of those who go on to die by suicide (because they are much larger in absolute terms) (Mulder Reference Mulder, Newton-Howes and Coid2016). Additional problems may arise as a consequence of an innate tendency of humans to automatically assign people to broad categories and then to make predictions about them on the basis of the assigned category rather than person's unique characteristics (Liberman Reference Liberman, Woodward and Kinzler2017). In the risk assessment/management context, this may lead to the clinician inflexibly adhering to beliefs about the patient's assigned risk categorisation even in the light of emerging evidence to the contrary. As will be discussed below, such inflexibility can encourage a countertherapeutic stance. In forensic mental health services, risk categorisation is still used, but its effectiveness in reducing violence remains to be determined (Challinor Reference Challinor, Ogundalu and McIntyre2021).
Uncertainty versus predictions and probabilities
Although there may be an emerging consensus that categorical prediction has no place in an individual clinical risk assessment in general psychiatric settings (e.g. Graney Reference Graney, Hunt and Quinlivan2020), there remains a question about the role of probabilistic approaches. In other fields, such as economics and geopolitics, it has been demonstrated that the practice of actively thinking probabilistically is associated with more accurate subjective probability estimates of future events (Tetlock Reference Tetlock, Mellers and Scoblic2017). However, there is a difference between improving the accuracy of these estimates and the use of the estimates to inform clinical decisions. To use a probability estimate to inform a categorical decision (e.g. to admit the patient or not) requires a threshold to be applied, which inevitably turns the estimate into a category (and therefore subject to the problems of using predictive categories).
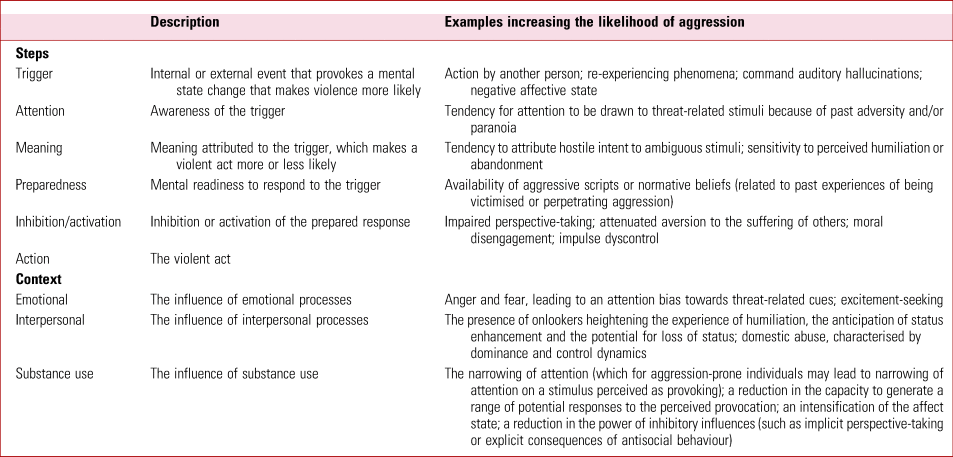
The concept of ‘uncertainty’, which acknowledges that the probabilities of the outcomes are unknown or meaningless (Park Reference Park and Shapira2017), more accurately represents the realm in which mental health clinicians undertake risk assessments and it encourages a focus on reducing uncertainty rather than predicting outcomes or quantifying the probability of their occurrence. Accepting that we are dealing with Knightian uncertainty, in that the probability distribution of future harmful events in the case of a given patient is unknown, reduces our need to think of the future in terms of predictions and probabilities. The focus should then shift from trying to compute the likelihood of outcomes to instead concentrating on characterising future scenarios of interest and the circumstances that would appreciably increase the likelihood of harm. In the psychiatric context, this can be facilitated by formulation, which brings together relevant factors in a way that produces an explanatory framework for the behaviour of interest. This is commonly done by assigning factors different explanatory functions, such as predisposing, precipitating, perpetuating and protective. Using formulation as an explanatory framework and scenarios to speculate about the future are important steps in approaches to risk assessment and management in forensic settings. Formulations can be further enhanced by exploring the proximal mental processes that are hypothesised to cause the behaviour (i.e. the propensity) (Nathan Reference Nathan, Whyler and Wilson2020). Existing explanatory models of suicidal and violent behaviour can serve as evidence-based frameworks to assist the clinician (Klonsky Reference Klonsky2018) (Box 2 and Table 1). Such models describe how combinations of many risk factors create pathways towards the emergence of harmful ideation and behaviour, and reserve particular focus, as a result of being set within the ideation-to-action framework, on the factors that govern the transition from ideation to action (Zortea Reference Zortea, Cleare and Melson2020).
BOX 2 Explanatory frameworks of proximal mental processes related to suicidal behaviour
Interpersonal theory of suicide (IPTS) (van Orden Reference van Orden, Witte and Cukrowicz2010) – Thwarted belongingness (unmet need to belong) and perceived burdensomeness (perception of being a burden to others) lead to suicidal desire. Exposure to painful and provocative events (e.g. childhood adversity, adult trauma, self-injury) causes habituation to fear and pain, which can result in the capability to enact suicide.
Integrated motivational-volitional model (IMV) (O'Connor Reference O'Connor and Kirtley2018) – A tripartite model in which (1) the pre-motivational phase, comprising life circumstances and events, provides a contextual background for (2) the motivational phase, when defeat and humiliation appraisals lead to a state of entrapment in which suicidal behaviour is seen as a salient solution to life circumstances and suicidal ideation and intent develop, followed by (3) the volitional phase, in which the suicidal behaviour occurs. Progression through these phases is influenced by moderators (e.g. social problem-solving, memory biases and rumination, thwarted belongingness, burdensomeness, social support).
Three-step theory (3ST) (Klonsky Reference Klonsky2018) – Step 1: the combination of pain that is experienced as punishing (particularly psychological pain consequent on aversive stimuli, such as conflict, loss, physical ill health) and hopelessness (about the pain diminishing) lead to suicidal ideation; step 2: suicidal ideation is heightened by disrupted connectedness (primarily to other people, but also to a job, project, interest, etc.); and step 3: progression from ideation to action depends on suicide capacity, which is made up of the dispositional (e.g. pain sensitivity), acquired (e.g. habituation to experiences associated with pain) and practical (e.g. knowledge of and access to lethal means).
Fluid vulnerability theory (FVT) (Rudd Reference Rudd and Ellis2006) – Takes account of the variable nature of suicide risk over time (such as rapid changes in ideation) by delineating chronic and acute suicide risk. Acute episodes of risk are time-limited and driven largely by situation and contextual variables (e.g. severity and mix of current symptoms, life stressors, substance misuse, access to method). Chronic (or baseline/residual) risk describes an enduring individual vulnerability for suicidality or an acute risk episode and is based on a disparate range of factors, including adversity, genetic history, biology/physiology, and cognitive, affective and motivational dispositions.
TABLE 1 Explanatory framework of mental processes related to violent behaviour
Making use of case-based explanatory models
Although clinical experience suggests that the explanatory models (or elements thereof) often have utility in explaining a single instance of behaviour, a model should not be seen to have universal applicability and there should not be indiscriminate top-down imposition (Hjelmeland Reference Hjelmeland and Loa Knizek2019). Furthermore, just because a model may represent a parsimonious theory to understand the behaviour in a way that guides clinical decision-making does not mean that it leads to highly accurate predictions of future behaviour (Klonsky Reference Klonsky, Saffer and Bryan2020). Analysis of previous suicidal, self-harm or aggressive behaviours should inform the explanatory processes that are relevant to this case. This can be done using a chain analysis, which involves a collaborative exploration with the patient of the vulnerability factors and prompting events for, and the consequences of, the target thoughts/behaviour (Borges Reference Borges, Nazem and Matarazzo2019). The use of such explanatory models can be illustrated in the context of the vignette presented above. It turned out that Tom's feelings of hopelessness and despondency tended to become more intense when the relationship problems were such that he could not see a way out of his predicament and an end to his anguish. If Amy was familiar with the evidence-based explanatory frameworks related to suicidal behaviour (and in particular the integrated motivational-volitional model), then she would be more likely to ask relevant questions and to explore further for other relevant processes (e.g. defeat and humiliation). Tom may, in response, feel reassured that his problems are being properly understood and he may be left with more insight into why he sometimes experienced thoughts of ending his life (which otherwise may have felt frighteningly unpredictable).
Even with the use of an agreed model to characterise possible future scenarios, within- and between-assessor differences may contribute to variability among assessor judgements. For example, affective processes, which may change over time in the same individual, have a strong influence on risk perception (through the automatic deployment of the affect heuristic). Thus, clinicians’ feelings (as distinct from their knowledge) about an intervention are liable to influence their perception of its effectiveness (including in relation to managing the potential for harm). Risk perception may also be dependent on the readiness with which examples relevant to the scenario under consideration come to mind (i.e. the availability heuristic), which is liable to differ depending on the assessor's previous experience. Assessors should be aware of the potential for biased judgements and the need to resist automatic risk categorisations in favour of a detailed analysis with the intention of reducing uncertainty.
As well as the effect of heuristics on decision-making, certain practitioner characteristics have been shown to contribute to better judgement formation. Subject-matter expertise is necessary, but not sufficient (Tetlock Reference Tetlock, Mellers and Scoblic2017). For instance, an individual's willingness to accept the role of change and the potential to cultivate this type of judgement formation, together with active open-mindedness, are associated with better judgements about future events (Tetlock Reference Tetlock, Mellers and Scoblic2017).
Decision-making
Although any categorical or dimensional outputs of risk assessment methods may not be usable in individual instances of clinical decision-making, the constituent elements of the risk assessment may still have some utility for risk management. Risk management involves addressing current modifiable factors that the explanatory formulation suggests increase the likelihood of high-harm behaviour, including any specific treatment needs (e.g. depression or substance misuse) (Large Reference Large, Ryan and Carter2017). Ways of bolstering factors that the formulation suggests reduce the likelihood of future harm should be explored with the patient. The management plan should also consider early warning signs for a high-risk mental state and steps to be taken in this event. Specific safety or crisis plans (which focus on stressors, warning signs, self-management strategies, social support and crisis resources) have been shown to reduce subsequent suicidal behaviours (e.g. Nuij Reference Nuij, van Ballegooijen and de Beurs2021).
Although it has to be accepted that the current empirical evidence undermines the case for the routine clinical use of categorical risk predictions, it does leave an outstanding question about how clinicians should take account of risk when faced with options that can only be implemented in categorically distinct forms. In the vignette presented above, one of the issues under consideration was admission to hospital. Clinical experience would suggest that the decision is often framed as being dependent on whether or not the patient is going to imminently act on urges to cause harm (to self in the vignette) but, as has been explained, this cannot be accurately predicted. It is possible to conceive the use of a probability estimate, but it would require the data-set from which the estimate is drawn to be relevant to the scenario (i.e. from a sample of patients assessed following an overdose rather than an in-patient sample about to be discharged). Also, to use a number from a continuous scale to make a categorical decision requires the establishment of thresholds (with or without the scope for justified discretion). Before introducing such an approach, further empirical testing would be necessary.
An alternative approach would be to use the unique case-based explanatory formulation in collaboration with the patient to consider the factors that increase the likelihood of the behaviour and potential ways to address modifiable factors so as to reduce that likelihood. It would still be necessary to come to a categorical decision, but this approach has the advantage of focusing attention on what can be done to adjust the modifiable circumstances (and this may include the use of therapeutic skills during the assessment), which in turn may assist the clinician in combatting their own automatic and biased categorical assumptions.
It needs also to be recognised that in practice the system places demands on the clinician that are sometimes in competition. Although the imperative to help the patient's emotional well-being may not conflict with the requirement to reduce the likelihood of high-harm outcomes, sometimes it does. For example, although admission may be thought necessary to manage dangerous levels of self-harm, in some cases the in-patient environment may exacerbate some of the underlying processes contributing to self-harm. For example, the use of medication and/or physical restrictions to address acute mental state changes may reinforce certain pre-existing processes contributing to a tendency to self-harm (such as difficulties understanding and reflecting on the mental states of others, which may lead to a dependence on the overt physical representations of the intentions of others provided by medication and physical restrictions). Therefore, the clinician needs to consider the possibility that the way of managing the potential for harm in the short term (i.e. admission) will further compromise the patient's well-being. Also, there may be service-level pressures (which can be manifest in interpersonal tension between ‘referrers’ and ‘gatekeepers’) to avoid admission, which are often related to the need to manage a finite resource under pressure. Thus, the clinician's final decision is influenced by judgements about future unpredictable harms and benefits within a complex system of pressures and relationships.
Interaction
If risk assessment is framed solely as a process of gathering and interpreting information about the patient to reach a judgement about the possibility of future adverse incidents, then the discussion with the patient is liable to become transactional, in that the primary goal is to elicit information. To the contrary, the interaction should be seen as an opportunity to reach a shared understanding of risk and to positively influence the patient's mental state and their representations of mental healthcare professionals in a way that may have a bearing on their future behaviour (including behaviour that has the potential to harm themselves or others). The clinician should adopt a compassionate and collaborative stance in which they actively and supportively listen with the aim of enhancing understanding (or reducing uncertainty) rather than reaching a categorical position about risk (Large Reference Large, Ryan and Carter2017).
There may be a legitimate difference of view between the clinician and patient about the next steps (e.g. whether to admit a patient who is feeling suicidal), but the clinician needs to be careful that their explanation for their decision does not constitute invalidation of the patient's experiences. The false belief that the patient can be definitely allocated to a risk category may lead the clinician to have an undue sense of confidence in their judgement, and then convey this false confidence to the patient in a way that invalidates the patient's experiences and feelings. There is empirical evidence to show that a collaborative assessment that emphasises respect, compassion, curiosity, a desire to help, flexibility and the relational nature of the assessment is associated with symptom reduction and patient self-enhancement (e.g. Durosini Reference Durosini and Aschieri2021) and it has been proposed that a positive therapeutic relationship may reduce risk (Royal College of Psychiatrists 2016).
Learning and investigating
The approach to learning from untoward incidents is relevant to the practice of risk assessment because in making decisions in acute psychiatric scenarios, clinicians are influenced not only by the clinical information available to them, but also by the wider context in which they practice (Nathan Reference Nathan and Wilson2021a). Such learning, typically through investigations, takes a deterministic perspective that does not readily apply within complex systems (such as mental health services), in which the underlying determinants of change are uncertain and non-stationary.
Although scrutinising the past in light of the outcome seems the best way to reach an explanation of why the outcome occurred, it can lead to problems when judging whether the decision was the correct one or not. The usual approach to investigating an incident (e.g. by an internal investigation, an external review or the coronial process) is to work back from the outcome to identify factors and decision points that appear to have a causal link with the outcome. This approach encourages decision-making to be tested in light of the outcome, i.e. would the outcome have been different if a different decision had been made? It is well recognised that looking back from the outcome makes the assessor susceptible to hindsight bias, which leads to an overestimation of the foreseeability of the outcome (Roese Reference Roese and Vohs2012) and that the resulting investigations can contribute to a culture in which clinicians feel that they are liable to be blamed for unpredictable outcomes (Munro Reference Munro2019). However, more fundamentally, the decision maker is in effect being tested against a standard that is almost impossible to meet. Not only do they not know the outcome, but as articulated above the empirical evidence also suggests that even if they had fully considered the relevant risk factors, that outcome would have been nigh on impossible to predict in an individual case. Another way of illustrating the contradiction is to consider the decision not only in light of actual events but also in the counterfactual scenario in which the outcome did not occur. Concluding that it was reasonable in the latter scenario but not in the former means that the clinician is placed in the unenviable position of being assessed by a standard that is not known at the time of making the decision and only becomes known after a future unlikely and unpredictable outcome has occurred (Bhandari Reference Bhandari, Thomassen and Nathan2022).
What is the relevance of this to practice? At the time of making a critical clinical decision, as well as thinking about the possibility of future harm enacted by the patient, clinicians’ decisions are also influenced by an in-the-moment contemplation of an unfavourable future appraisal of their decision-making in the event of a serious adverse event occurring (even though the event is unlikely) (Nathan Reference Nathan and Wilson2021a). The issues can be illustrated by a development of the scenario presented in the vignette above. Although Amy remained of the view that admission was indicated, there had been previous tension between her and the home treatment practitioner and she did not have the confidence to contest the decision to decline admission. She also had on her mind thoughts about a member of her team who was still off work for stress due to the experience of the way she was questioned in both an internal investigation and coroner's inquest in a separate case 6 months before. When Amy told Tom that he had to go home, he abruptly left the hospital. In Amy's clinical entry she justified her decision not to pursue the option of admission by stating that although Tom ‘threatened’ to throw himself off a motorway bridge this appeared to be for ‘secondary gain’ (to secure admission) and she thought that because he was talking about events in the future the risk of suicide was not high. Thus, although in reality clinicians are unable to reliably predict the outcome, they are prone to hold in mind an approach that relies on a deterministic predictive model (in which an outcome is an inevitable result of the antecedent causes), further encouraging the spurious categorisations of patients as high or low risk, the use of such categorisation to allocate resources and the adoption of defensive practices (Munro Reference Munro2019). Amy would, she thought, have felt more able to take a different approach to the dilemma she faced if it was clear to her that in the event of a future untoward incident, the investigation would not use the outcome as a basis for judging her actions and account was taken of the real-time complexity of the situation. She would have felt less motivated to use a spurious risk categorisation to defend herself against what she imagined, from the perspective of a hindsight-armed investigator or coroner, could look like a ‘missed opportunity’. More importantly, by feeling able to acknowledge with Tom (and in her clinical entry) that she remained concerned about the risk, the encounter would have been more validating and there would have been greater opportunity for the collaborative exploration of alternative options to admission, which as noted above may have reduced risk.
Therefore, the issue is not just agreeing how to conceptualise risk assessment, but also agreeing how to conceptualise the system in which the risk assessment activity occurs. Rather than conceptualising a deterministic system (i.e. one in which the future state of every aspect of the system can be described), risk assessment should be characterised as an informed process to reduce uncertainty within a complex system of unknowable future states. More research is needed before firm recommendations can be given about alternative models to learn from adverse incidents, but possible approaches include appraising any decision of interest in light of a counterfactual scenario in which the outcome did not occur, appraising decisions against pre-agreed standards, appraising decisions without knowledge of the outcome and/or focusing on potential latent factors (i.e. systems, processes and training) rather than just linear cause-and-effect ones (Bhandari Reference Bhandari, Thomassen and Nathan2022).
Conclusions
As yet, it has not been possible to produce a method for an individual clinician to accurately predict whether or not the patient they are assessing at a single point in time will go on act in a way that seriously harms themselves or others in the near future. It remains to be determined whether the alternative approach of attempting to apply a quantitative estimate to possible future events has applicability in such a single instance. Given that a person's future behaviour is dependent on the interplay over time between their actions (which are in turn dependent on innumerable and often unknowable mental processes) and the environment in which they will exist (which takes the form of a complex and dynamic system of other unpredictable and interdependent agents), it seems unlikely that accurately foretelling a single person's future will be possible anytime soon. In the meantime, a faith in this possibility can interfere with the goal of risk assessment, which should be to inform clinical decisions with the aim of reducing the likelihood of future serious harm while at the same time improving patient health and well-being. Oversimplified categorical judgements are not just liable to be wrong. The rigid and overconfident adherence to such judgements can also undermine the therapeutic potential of the assessment.
An awareness of the factors that have been found at a group level to be associated with an increased likelihood of harmful events is still important. Armed with such an awareness the clinician can reach an informed conclusion about the type of harm that the risk management plan should address and can engage the patient in a discussion about strategies to address those factors that are modifiable. However, the success of new models of risk assessment will not merely be a function of the components of those models. Attention also needs to be paid to clinician-based and system-based issues that have a bearing on the implementation of the model. If, as the empirical evidence suggests, humans are naturally inclined to categorise and to be subject to unthinking biases in forming judgements about the future, then attention also needs to be given to enhancing the psychological competencies of risk assessors and incident investigators, so that they are more able to resist these inclinations and remain actively open-minded. Furthermore, for as long as the wider system takes a deterministic approach in judging previous decisions in light of an adverse outcome, then clinicians (who, the empirical evidence suggests, have an eye to the anticipated findings of such investigations in their day-to-day practice) will find it difficult to lose faith in the deterministically informed assumption that the future can be read. Developing, implementing and researching risk assessment requires clarity about the goal of this clinical activity, its meaning in real-world settings (which should take into account the wider system as well as the individual clinical encounter) and the human factors that can interfere with the achievement of the goal.
Author contributions
R.N. conceived the article and was responsible for the figure and table. R.N. and S.B. reviewed the relevant literature and drafted and edited the manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.
MCQs
Select the single best option for each question stem
1 As regards probability and uncertainty:
a frequentist probability is the long-run frequency over a large number of repetitions of an experiment
b classic probability is the fraction of the total number of possibilities of different likelihoods in which the event occurs
c classic probability is directly relevant to clinical risk assessments
d the term ‘uncertainty’ applies when the probability distribution of the outcome is known
e subjective probability is equivalent to propensity.
2 Which of the following a statements on information gathering for risk assessment is false?
a risk assessment should not be seen as a stand-alone clinical activity
b a phenomenological approach is likely to produce a more case-specific understanding than a diagnostic approach
c risk factors should be understood in the context of the person's current experiences
d it is good practice to seek information from a range of sources
e all suicidal ideation can be defined as either passive or active.
3 As regards risk assessment:
a the use of risk assessment tools enables clinicians to predict future violent and suicidal acts
b the idea of risk assessment as prediction is fallacy
c risk factors tend to occur very rarely in clinical practice
d serious harm outcomes are common in psychiatric practice
e risk categorisation is unlikely to be harmful.
4 In relation to human factors relevant to risk assessment, which of the following is false?
a the availability heuristic refers to the influence on probability judgements of the readiness with which relevant examples come to mind
b affective processes within the assessor may influence the perception of risk
c assessors should ignore their own potential biases when undertaking risk assessments
d active open-mindedness is associated with better judgements about future events
e assessors’ willingness to accept the role of change is associated with better judgements about future events.
5 In the context of investigating and learning from adverse incidents:
a hindsight bias refers to the tendency to retrospectively underestimate the foreseeability of a known outcome
b concluding that a decision was incorrect in light of the actual adverse outcome but would have been correct if that outcome had not occurred is a good way of testing clinical decision-making
c deterministically judging clinical decisions in the knowledge of the outcome generally proves helpful in learning from adverse outcomes
d when making decisions in acute psychiatric scenarios, clinicians are liable to contemplate an unfavourable appraisal of their decisions in the event of an adverse outcome
e risk assessment in practice should depend on a deterministic conceptualisation of reality.
MCQ answers
1 a c 2 e c 3 b c 4 c 5 d







eLetters
No eLetters have been published for this article.