Introduction
Difficulty in establishing control of a patient’s airway during resuscitation is a problem spanning multiple settings and involving many specialties of medicine. However, the difficult airway is perhaps at its most challenging in the prehospital environment with reported first-pass success (FPS) rates for out-of-hospital endotracheal intubation (ETI) ranging from 46.4% to 78.9% over the last 12 years, without much evidence of trends toward improvement.Reference Hubble, Brown, Wilfong, Hertelendy, Benner and Richards1–Reference Peters, van Wageningen and Hendriks6 Patients with similar characteristics are managed in the emergency department (ED) more successfully, with first-pass and overall success rates of 83.0% to 96.0% and 99.4% to 99.7%, respectively.Reference Brown, Bair, Pallin and Walls7,Reference Wong and Ng8
It is, however, an accepted paradigm that emergent airway management outside of the hospital presents a different problem set from that experienced in the ED.Reference Cooney, Murano, Ring, Starr, Beeson and Edgar9,Reference Ambardekar, Walker and McKenzie-Brown10 Further still, data from the far-forward combat setting in Afghanistan’s Helmand Province demonstrate a 36% failure rate among prehospital personnel performing ETI, which comprised the majority (86.6%) of all airway management attempts.Reference Adams, Cuniowski, Muck and De Lorenzo11,Reference Pugh, LeClerc and McLennan12 The alternative approach of cricothyrotomy represents only 5.8% of interventions, but comes with an overall failure rate of 28% to 33% and a 64% complication rate.Reference Adams, Cuniowski, Muck and De Lorenzo11–Reference Barnard, Ervin, Mabry and Bebarta16 Supraglottic airways (SGAs) are an alternative that may be easier to insert, but they are not a definitive airway and may deliver suboptimal ventilation and incomplete protection from aspiration.Reference Ostermayer and Gausche-Hill17
After-action reports from prehospital advanced airway management in combat environments found that 50% of failed attempts were attributable to equipment shortages or malfunctions while an additional 38% were secondary to a lack of training. This is mirrored in the civilian sector where the discussion often focuses on the types of procedures (eg, ETI versus SGA) that are best suited for nonphysician field personnel.Reference Crewdson, Lockey, Roislien, Lossius and Rehn18–Reference Wang, Seitz, Hostler and Yealy20 Despite decades of studies, guidelines informed by experts, and a plethora of marketed airway devices, it is clear is that current airway management solutions are falling short. A new perspective is needed.
Defining the Difficult Airway
There is currently no all-encompassing or universally accepted definition of what constitutes a difficult airway.Reference Yentis21 The American Society of Anesthesiology (ASA; Schaumburg, Illinois USA) defines it as: “a clinical situation in which a conventionally trained anesthesiologist experiences difficulty with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both.”Reference Apfelbaum, Hagberg and Caplan22 Similarly, the Difficult Airway Society in the United Kingdom cites it as: “unsuccessful bag-valve mask [BVM] ventilation, direct laryngoscopy, SGA placement, and/or endotracheal intubation.”Reference Frerk, Mitchell and McNarry23 Both of these definitions narrow the scope of practice to either a single set of physicians or specific interventions; they do not address abnormal patient presentations in austere settings.
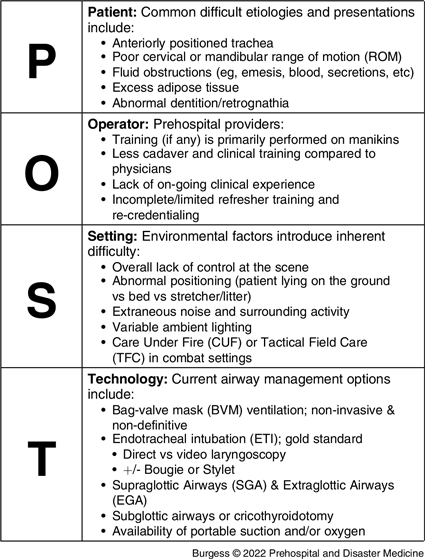
Importantly, no single factor is independently associated with the ability to accurately predict difficulty or failure to place an airway. Huitink and Bouwman underscore this by declaring that the concept of a difficult airway does not exist and is instead: “…a complex situational interplay of patient, practitioner, equipment, expertise, and circumstances.”Reference Huitink and Bouwman24 Furthermore, we propose that the difficult airway is not a diagnosis, but instead is a scenario in which effective airway securement and ventilation is challenging to obtain as a result of the interplay of situational elements. Refocusing the problem from individual elements (such as patient anatomy, perceived training inadequacies, the environment, or lack of technological implements) to an inter-related set of problems closes an important gap in the approach to the difficulty airway. That is, we propose a systematic definition that emphasizes the interactions between the Patient, Operator, Setting, and Technology (POST; Table 1).
Table 1. Breakdown of the Patient, Operator, Setting, and Technology (POST) Acronym and the Factors Associated and Responsible for Creating or Exacerbating Difficult Airway Management in the Prehospital Setting
Patient – Airway Presentation
Screening for potentially difficult airways based on a patient’s presentation and/or anatomy can be performed using a multitude of assessments to include the LEMON acronym (Look-Evaluate-Mallampati score-Obstruction-Neck mobility), upper lip bite test, Cormack-Lehane, Wilson, Mallampati, and Arne scores.Reference Mallampati, Gatt and Gugino25–Reference Khan, Kashfi and Ebrahimkhani31 Unfortunately, they do not accurately account for common field problems such as massive facial trauma or obstructions like blood, mud, and debris in the airway. In combat casualty care, obstructions secondary to trauma were the second leading cause of potentially survivable combat casualty mortality from 2001-2011.Reference Eastridge, Mabry and Seguin32 The 2020 Joint Trauma System Clinical Practice Guideline (JTS CPG) for airway management is a military-focused approach for prolonged field care which outlines two indications for airway management: disrupted face or neck anatomy and insufficient oxygenation or ventilation.Reference Dye, Keenan and Carius33 While the guidelines explicitly leave room for the clinical judgement of the combat medic or corpsman, there is currently no universally effective solution for battlefield injuries requiring airway management.
Operator - Training and Experience
Residency training in emergency medicine and anesthesia is rigorous with ample opportunities for direct clinical experience in airway management. One study identified the number of supervised ETIs necessary to achieve an acceptable level of proficiency, as defined by a FPS rate of 90%, to be 75.Reference Hardy, Maddry and Ng34 Paramedic students, in contrast, performed a mean of nine ETI attempts on training mannequins during their initial training.Reference Wang, Seitz, Hostler and Yealy20,Reference Bucher, Bryczkowski and Wei35 Uhaa, et al reported that out of 77 US Army combat medics, the median number of simulation training intubations was zero, as was the number of real human intubations.Reference Uhaa, Jeschke and Gwynne36 It is also possible that airway management success requires more than just focused training and procedural experience. Clinical judgement may also play a role and might account for the nearly two-fold difference in FPS rates for aeromedical physicians (84.5%) and paramedics (46.6%) in comparable patient groups.Reference Peters, van Wageningen and Hendriks6 Similar trends have been established amongst ground-based Emergency Medical Service teams utilizing physicians and non-physicians in regards to both their first-pass (87.2% versus 69.6%) and overall (99.4% versus 91.7%) success rates.Reference Crewdson, Lockey, Roislien, Lossius and Rehn18 Additionally, a 2013 report from Helmand Province in Afghanistan found a 64.0% overall success rate for combat medics performing prehospital ETI.Reference Adams, Cuniowski, Muck and De Lorenzo11,Reference Pugh, LeClerc and McLennan12 These analyses make clear that there is a significant gap in the relative success of tracheal intubation by field providers. While at least one program reports greater success by emphasizing follow-up training for paramedics in the operating room and the ED, the need to account for the operator and their level of training persists.Reference Trimmel, Beywinkler, Hornung, Kreutziger and Voelckel37
Setting – Prehospital and Battlefield Environments
The prehospital and especially the combat environment present a particular set of unique circumstances. While intuitive, evidence of the differences between in- and out-of-hospital airway management is shown by anesthesia-trained residents encountering a higher rate of both perceived and actual difficulty in the prehospital setting as compared to the operating room.Reference Goldberg38 The factors leading to this are undoubtedly multi-factorial, but likely include abnormal positioning with patients often lying on the ground rather than elevated on a bed or stretcher, a lack of suction or other ancillary support devices, and the presence of extraneous noise, surrounding chaotic activity, and variable ambient lighting. The battlefield with ever-present chaos and danger compounds the significant impact that the environment can have on the patient and provider.
Technology
A survey of emergency medicine residency training directors identifies a dozen airway device categories to master; for just one of those categories, a 2014 paper on prehospital SGAs lists 15 different devices.Reference Ostermayer and Gausche-Hill17,Reference Reeder, Brown and Norris39 Although more devices on the market means more tools in the hands of providers, this does not necessarily equate to improved patient outcomes. Carney, et al published a meta-analysis of multiple databases spanning 1990 to 2020 which demonstrated a lack of any overwhelming benefits to invasive airway management in the prehospital setting in regards to survival, neurological function, return of spontaneous circulation (ROSC), or successful ventilation.Reference Carney, Totten and Cheney40 These findings are mirrored in the context of combat casualty care with an analysis of a 1,267 patient cohort of US Army MEDEVAC casualties supporting the use of BVM ventilation over invasive methodologies, citing no differences in overall survival rates.Reference Hardy, Maddry and Ng34 This same study found that use of a SGA was associated with a higher number of ventilator days, hospital days, and intensive care unit days compared to BVM ventilation alone. As such, device development for the prehospital setting requires an approach that balances the needs and operating environment of the end-user to the availability of evidence.
The JTS CPG establishes a minimum, better, and best guideline for airway management equipment with “good” equating to a nasopharyngeal airway (NPA), cricothyrotomy kit, and BVM. “Better” adds an SGA, nasogastric or orogastric tube, and a gum elastic bougie, while “best” includes endotracheal tubes and a direct or video laryngoscope.Reference Dye, Keenan and Carius33 The shortcomings of these guidelines are revealed in a survey of combat medics’ aid bags which found that only 31% of kits contained an SGA, 64% contained a cricothyrotomy kit, and nearly all (93%; 41/44) carried an NPA.Reference Schauer, Naylor, Uhaa, April and De Lorenzo41 The JTS CPG appears to offer few reliably safe and efficacious airway options and sidesteps the reality that most, if not nearly all, cases of significant airway compromise in the prehospital combat environment will be difficult airways.
Redefining the Concept of the Difficult Airway
Shifting from a narrow definition of the difficult airway problem to a systems approach is straightforward: we propose a redefinition that emphasizes the interplay of all factors that result in a situation where a patient cannot be adequately ventilated by way of a secure, protected airway. From a research and development perspective, a system made up of interlinked factors facilitates a comprehensive, multi-disciplinary approach and suggests a new agenda focused on these relationships.
One such way that this systems approach can be implemented is by improving prehospital operator training through examination and quantification of the relationship between the patient and operator. Today’s airway manikin trainers lack anatomical accuracy, even for a healthy, atraumatic patient, much less providing any burdensome anatomy or etiologies representative of real-world scenarios.Reference Blackburn, Wang and Ross42 A relatively unsophisticated but high-yield solution might include the establishment of a set of distorted, traumatic, and troublesome airway manikins that mimic the patient-centric factors most attributed to failed airway management. Realistic training where simulation of real-world scenarios with abnormal positioning, poor lighting, and obstructive gear or clothing might also be effective. Implementation of a systematic, realistic airway management simulation platform could enable examination and measurement of these elements as well as give new combat medics and skilled providers a more meaningful taste of the real issues encountered in the field.
Training may not be the sole answer, as Uhaa, et al found that most combat medics do not receive any hands-on training for advanced airway management.Reference Bucher, Bryczkowski and Wei35 Improving the technology by developing it with an understanding of the prehospital operator’s limited training opportunities could improve airway success. Implementing systems-based approaches will provide device inventors and developers with visibility of the issues and obstacles faced in the field, thereby accelerating the development of new and improved tools. One striking example of this is the infrequency with which portable suction devices are carried by combat medics.Reference Jain, Akhter, Schoppe, Hood and De Lorenzo43 It is conceivable that, with proper suctioning, some patients would get primary relief from airway obstruction and others might benefit from easier securement.
These examples are meant to highlight that by focusing on a POST model of the difficult airway, a research agenda may emerge that highlights the interactions between the model’s four elements rather than attempting to solve the problems of each component in isolation. Formal research on the interplay of these elements could inform the current discussion regarding the degree of training and device optimization required for both civilian and combat medics to improve airway management outcomes for their respective patient populations.
Conclusion
The unique nature and higher prevalence of difficult and failed airway management encountered in prehospital and combat settings prompts a refocusing of the viewpoint on what constitutes a difficult airway. We propose a system in which the components of POST are equally considered, as are the important relationships and interactions between them. Based on this systems approach, we further propose that the difficult airway is one in which ventilation and/or airway protection cannot be established quickly, secondary to the interplay between the POST elements. Examining the interactions between these four aspects of airway management provides a system-based approach better suited to understanding the obstacles faced by combat medics and prehospital personnel alike. This in turn prompts implementation of novel, targeted research efforts utilizing this model as a platform to improve the currently sub-optimal rates of success in prehospital airway management.
Conflicts of interest/funding/disclaimer
R. Lyle Hood and Robert A. De Lorenzo are principals in EmergenceMed, LLC, a medical device R&D firm. No funding was received for this study. The views expressed in this article are those of the authors and do not reflect the official policy or position of the US Army Medical Department, Department of the Army, Department of Defense, or the US Government. This manuscript was presented in the form of a poster at the 2022 Military Health system Research Symposium (MHSRS) on September 13, 2022.






