Introduction: the rise of the older man living alone
The number of people living alone – including in old age – is on the rise throughout many Western societies (Klinenberg, Reference Klinenberg2012). In Denmark, the context of this study, more than one million citizens live in households with just one person (Statistics Denmark [Danmarks Statistik], 2015b). Public policy strategies to promote ‘ageing in place’ and to reduce institutionalisations have served to further the general development towards living alone in old age (Schön et al., Reference Schön, Lagergren and Kåreholt2016). Until recently, it was predominantly older women who lived alone, but, due to increased male longevity and new family patterns, it is now becoming increasingly common for men too. In Denmark, the prevalence of 65–79-year-old men living alone increased by 47 per cent between 1990 and 2016 (Rasmussen, Reference Rasmussen2016) and, in 2017, 26.6 per cent of men aged 65 and over were living alone (Danish Health Authority [Sundhedsstyrelsen], 2019). Widowers can now expect to live on average ten years on their own (Baes-Jørgensen, Reference Baes-Jørgensen2019).
In this article, the term ‘living alone’ is used to describe a man's living arrangements and should not be confused with social isolation (which refers to a person's level of social integration in the community; Victor et al., Reference Victor, Scambler, Bond and Bowling2000) or loneliness (which refers to a negative experience concerning the subjective evaluation of the quality or quantity of one's relations; Perlman and Peplau, Reference Perlman, Peplau, Duck and Gilmour1981). Still, older men living alone are primarily represented as an at-risk group, and their increasing numbers are mainly viewed as a concern for the welfare state (Leontowitsch et al., Reference Leontowitsch, Fooken and Oswald2019; see also official Danish guidelines for the prevention of diseases and disabilities and for the detection of at-risk groups: Danish Health Authority, 2015, 2017). As a result of this ‘narrative of vulnerability’ (Leontowitsch et al., Reference Leontowitsch, Fooken and Oswald2019), older men are automatically construed as lonely, isolated and otherwise at risk in health-related matters (Mikkelsen, Reference Mikkelsen2016). This is reflected in Danish health-care debates, which spend a considerable amount of time discussing older men as a high-priority group that requires political intervention.
In general, this dominant view on older men living alone is supported by research literature. Although some studies identify living alone as a potential sign of good functioning, particularly among the very old (Ennis et al., Reference Ennis, Larson, Grothaus, Helfrich, Balch and Phelan2014), living alone in old age has been associated with a disadvantaged health status, e.g. a greater risk of social isolation (Kharicha et al., Reference Kharicha, Iliffe, Harari, Swift, Gillmann and Stuck2007), depressive symptoms (Djernes, Reference Djernes2006), poor self-reported health, difficulties carrying out daily activities, worsening function and multiple falls (Kharicha et al., Reference Kharicha, Iliffe, Harari, Swift, Gillmann and Stuck2007), institutionalisation (Pimouguet et al., Reference Pimouguet, Rizzuto, Schön, Shakersain, Angleman, Lagergren, Fratiglioni and Xu2016; Takeuchi et al., Reference Takeuchi, Showa, Kitazawa and Mori2018) and suicide (Turecki and Brent, Reference Turecki and Brent2016). Men living alone have a particularly increased risk of mortality (Kandler et al., Reference Kandler, Meisinger, Baumert and Löwel2007; Staehelin et al., Reference Staehelin, Schindler, Spoerri and Zemp Stutz2012; Pimouguet et al., Reference Pimouguet, Rizzuto, Schön, Shakersain, Angleman, Lagergren, Fratiglioni and Xu2016), functional disability (Nilsson et al., Reference Nilsson, Lund and Avlund2008; Lund et al., Reference Lund, Nilsson and Avlund2010), social isolation and impaired mobility (Shaw et al., Reference Shaw, Fors, Fritzell, Lennartsoon and Agahi2017). The advantage of living with a spouse is also more salient for men, but this advantage decreases with age (Herm et al., Reference Herm, Anson and Poulain2016; see also Gopinath et al., Reference Gopinath, Rochtchina, Anstey and Mitchell2011; Udell et al., Reference Udell, Steg, Scirica, Smith, Ohman, Eagle, Goto, Cho and Bhatt2012; Poulain et al., Reference Poulain, Dal and Herm2016).
Marital status is not equivalent to but is strongly associated with living arrangements. Depending on whether they are widowers, divorcees or bachelors, Danish men have life expectancies that are on average 5.3–7.1 years shorter than married men (Statistics Denmark, 2013) and, at 65, they can expect to live on average 3.6–3.9 years less than their female counterparts (Statistics Denmark, 2015a). Research also shows that widowers seem to have more difficulties adapting to widowhood than widows. They have more depressive symptoms (Djernes, Reference Djernes2006), have poor psychological wellbeing for a longer time and receive more home care (Hansen and Greve, Reference Hansen and Greve2016). In addition, not having a partner is associated with a greater risk of loneliness (Hansen and Greve, Reference Hansen and Greve2016).
Living alone in old age was once associated with a higher educational level, but this association has recently reversed. Older men with only a basic level of education are now more likely to live alone (Shaw et al., Reference Shaw, Fors, Fritzell, Lennartsoon and Agahi2017). A lower level of education is itself closely associated with decreased longevity and poorer health (Baker et al., Reference Baker, Leon, Smith Greenaway, Collins and Movit2011; Economic Council of the Labour Movement [Arbejderbevægelsens Erhvervsråd], 2016), increased rates of depression (Knesebeck et al., Reference Knesebeck, Lüschen, Cockerham and Siegrist2003) and loneliness (Pinquart and Sorensen, Reference Pinquart and Sorensen2001; Danish Health Authority, 2014; Hansen and Slagsvold, Reference Hansen and Slagsvold2016). Social inequalities in mortality (Huisman et al., Reference Huisman, Read, Towriss, Deeg and Grundy2013) and in health-related measures such as self-rated health, functional ability and comorbidity (Fors et al., Reference Fors, Lennartsson and Lundberg2007; Enroth et al., Reference Enroth, Raitanen, Hervonen and Jylha2013) have been shown to persist into old and very old age. However, conclusions regarding tendencies and gender are divergent and might be subject to cross-cultural variation (Knesebeck et al., Reference Knesebeck, Lüschen, Cockerham and Siegrist2003). Some studies find that inequalities decrease in old age among men in particular (Hoebel et al., Reference Hoebel, Rommel, Schröder, Fuchs, Nowossadeck and Lampert2017), while others find that inequalities are especially persistent in men (Huisman et al., Reference Huisman, Kunst and Mackenbach2003).
Despite the societal interest in older men living alone, this issue has attracted limited attention in the research literature. Furthermore, health-care utilisation for older men has not been well studied, which is why the health-care and social service implications of their increasing numbers remain uncertain. Some studies have found that both living alone (Dreyer et al., Reference Dreyer, Steventon, Fisher and Deeny2018) and having a low socio-economic status (van Doorslaer et al., Reference van Doorslaer, Masseria and Koolman2006) are associated with an increased use of general practitioners (GPs), whereas other studies have found that living alone is associated with a decreased use of GPs (Kharicha et al., Reference Kharicha, Iliffe, Harari, Swift, Gillmann and Stuck2007). Indeed, the ability to live alone could be a sign of good functioning, at least for some men (Covinsky, Reference Covinsky2013; Ennis et al., Reference Ennis, Larson, Grothaus, Helfrich, Balch and Phelan2014), but reports and guidelines from social and health-care systems (National Social Appeals Board [Ankestyrelsen], 2010; Danish Health Authority, 2015, 2017) do not differentiate between sub-groups of men living alone when identifying them as a group of particular concern, though they do elsewhere point to educational level as a risk factor in its own right.
Ageing in place policies make it important to offer services on an informed basis and thereby make it possible to target the neediest groups with the most relevant services. In this article, we provide a multifaceted presentation of older Danish men's health and health-care utilisation when living alone. To the best of our knowledge, we are the first to do this. We contribute to existing research by uniting three different perspectives on older men's health, including register-based information on their health-care utilisation. We compare men living alone to men co-habiting and differentiate between sub-groups of men living alone in order to guide future intervention.
Research design and methods
The purpose of this study is to obtain health information for single-dwelling, older men in Denmark by conducting a statistical analysis of data from three different sources: an online survey among health-care professionals conducted by the authors, a national survey with self-reported health information from the men themselves and a register-based inquiry into the actual use of health-care services. The purpose of this three-part design is to shed light on different aspects of the health and needs of older men living alone. Our purpose is mainly descriptive, since we aim to present this group of men as they currently are. Based on available literature, whenever possible, we differentiate between the educational level, marital status and area of residence.
Part 1: The view from the health-care professionals
First, an electronic survey was conducted with municipal preventive home visitors, which allowed us to obtain a view on these men from the health-care professionals who encounter them in their daily work. According to Danish legislation, municipalities must offer preventive home visits to all citizens when they turn 75 provided that they do not already receive domestic help. Home visitors are nurses or other health professionals who discuss the person's current life situation and possible assistance needs during their visits. They can provide us with an estimate of which men are in need of intervention and what kinds of needs they have. These professionals might also know which men tend to remain ‘invisible’ and do not otherwise have contact with the health-care system.
The electronic questionnaire survey was sent to 271 preventive health-care professionals in the 98 municipalities in Denmark. It consisted of 40 closed questions, primarily of the Likert type. The respondents were able to add comments and elaborate their answers. In order to minimise the risk of subjective generalisations, respondents were asked to answer the questionnaire based on the last older man they had visited who lived alone and whom they would classify as requiring some kind of intervention. The questions sought to clarify social and health conditions of the man in question along with the home visitor's assessment of his needs. In addition, respondents were asked for their overall evaluation of the wellbeing of older men living alone compared with other groups of older people. Finally, they were asked about the adequacy of existing services for this group of men. To increase the response rate, a reminder was sent out two weeks after the original questionnaire.
We expected older men living alone to be considered a challenging group that was hard to reach and engage. We also expected that men with fewer financial means would be overrepresented. The statistical analysis of data was carried out using SPSS version 23. Scores were tested for normality by using the Kolmogorov–Smirnov test. Other tests used were chi-square, Kruskall–Wallis, Mann–Whitney U-test and Spearman's rank correlation.
Men in this study were over 75 years of age. However, the study raised the need to explore men's health at younger ages. We therefore extended the age range in the following studies (Parts 2 and 3) to 60 and over.
Part 2: The view from the men themselves
We used self-reported data to gain a view from the men themselves. As stated in our introduction, it is well established that inequity in health exists and that people with shorter educations exhibit worse health than their longer-educated counterparts. However, little research has been performed on how this intersects with living alone and how it relates to men in particular. The aim of this part of the study was to assess whether single-dwelling, older men rated their own health differently than co-habiting older men and whether there were differences among sub-groups of single-dwelling men as differentiated by educational level, area of residence and marital status. Based on available literature on each of the factors under consideration, we hypothesised that single-dwelling men would have lower health scores than co-habiting men and that, among the single-dwelling men, educational level would be correlated with self-rated health. Following the literature on widowers, we were interested in seeing whether widowers reported more difficulties than divorcees or bachelors. We were also interested to see whether, as indicated by the first part of our study, there were differences between older men living in rural and urban municipalities.
We extracted data from the 2013 version of the National Health Profile, a national survey of health among the Danish population conducted by the five regions, the Ministry of Health and the National Institute of Public Health (SIF) at the University of Southern Denmark. The purpose of this cross-sectional survey is to describe the general health and morbidity of the adult population in Denmark. In total, questionnaires were sent to 300,450 citizens in Denmark over the age of 16. The response rate was 54 per cent. Statistics Denmark has weighted the data for non-response. For the purposes of the present article, we have extracted data on health, wellbeing and social relations.
For self-reported physical and mental health, the survey used the SF-12 questionnaire, which consists of 12 questions inquiring into health-related limitations in physical functioning, social functioning and mental wellbeing within the past four weeks (Ware et al., Reference Ware, Kosinski and Keller1996; Gandek et al., Reference Gandek, Ware, Aaronson, Apolone, Bjorner, Brazier, Bullinger, Kaasa, Leplege, Prieto and Sullivan1998). Answers to the 12 questions feed into a total score for both a physical and a mental health component. A pre-defined cut-off score based on the 10 per cent of the population who scored the lowest in the 2010 National Health Profile demarcates the group with poor health (Danish Health Authority, 2014).
Level of stress was measured with Cohen's Perceived Stress Scale, a validated scale for self-reported stress (Cohen et al., Reference Cohen, Kamarck and Mermelstein1983; Eskildsen et al., Reference Eskildsen, Dalgaard, Nielsen, Andersen, Zachariae, Olsen, Jørgensen and Christiansen2015). The Perceived Stress Scale contains ten questions inquiring into perceived unpredictability, uncontrollability and stressfulness within the last four weeks.
Social relations were measured by questions on the amount of contact with family, friends, neighbours and other acquaintances (structural dimension) and how often the respondent had an unwelcome feeling of being alone (functional dimension, henceforth referred to as ‘unwanted alone’) (Danish Health Authority, 2014).
Statistical analyses were carried out using SPSS version 23. The Kolmogorov–Smirnov test was used to test for normality. For data without normal distribution, Mann–Whitney U-test/Kruskall–Wallis and Spearman's rank correlations were used. Otherwise, groups were compared using chi-square and one-way analysis of variance (ANOVA). Post hoc pairwise comparisons were carried out using Dunn–Bonferroni.
Part 3: The objective use of health-care services
Register-based data were used to achieve an ‘objective’ measure of health behaviour, namely the use of health-care services. The purpose of this part of the study was to uncover how health-care services were used by older men living alone compared with co-habiting older men and to compare sub-groups of older men living alone. These data are centrally registered and administrated by Statistics Denmark.
The analyses were based on a representative sample of the Danish population extracted from Statistics Denmark and consisted of 10 per cent of all Danish men who were over 60 years of age on 1 January 2014. For the sample population, Statistics Denmark drew on a number of health indicators on the registered use of health care: (a) number of hospital admissions, (b) hospitalisation days, (c) number of outpatient medical treatments, (d) number of visits to a GP and (e) use of other health-care services (e.g. ophthalmologist, dermatologist, psychiatrist, dentist or physiotherapist). In addition, the amount of home services (personal care and practical help at home and preventive home visits) was registered. All statements were for 2014.
The statistical analysis of data was carried out using SPSS version 24. The Gaussian distribution was analysed using the Kolmogorov–Smirnov test. In addition to comparisons of men living alone to men co-habiting, the data allowed us to compare sub-groups of men living alone based on educational level, income and area of residence. In the first analysis, using chi-square, we compared the proportion of individuals within each group who had used a given service within the last 12 months. We then looked at the users in each group and compared the amount of usage with the Student's t-test or one-way ANOVA.
Results
The online survey with health-care professionals
In total, 165 preventive home visitors responded to the survey (60.9%); approximately one in four of these (23%) responded with a partial answer; and 97 per cent (N = 160) of the respondents were female. The mean age was 51.7 years (standard deviation (SD) = 8.98) and 44 per cent of the home visitors were more than 55 years old; 92 (55.8%) were trained nurses whereas the remaining participants had other social or health-care educational backgrounds. On average, respondents had been carrying out preventive work for 8.8 years (SD = 5.86). The respondents’ age, educational background or experience were not found to have any significant influence on the responses. Respondents were distributed across 77 of the 98 municipalities in Denmark and distributed representatively between rural and urban municipalities (>150 inhabitants per square kilometre).
The preventive home visitors characterised 48.2 per cent of the men as being in neither a good nor a bad financial situation. They considered more of the men economically well-off (27.3%) than economically disadvantaged (18%) or in financial trouble (1.4%). Reasons for the men living alone were being a widower (70.5%), being divorced (15.8%), no longer cohabiting (5%) and having always lived alone (7.2%); 11.5 per cent of the men had lived alone for 0–1 year, 28.1 per cent for 1–3 years, 29.5 per for 3–10 years and 21.6 per cent for more than ten years.
Compared with preventive home visits in other sections of the population, 72 per cent of the preventive home visitors considered it a particularly challenging task to work with older men living alone; 91 per cent of the survey respondents called for new social and health-care services tailored to the needs of this group of men. The Kruskal–Wallis test showed a significant difference in estimated wellbeing between older men living alone, co-habiting older men and older women living alone (χ2(2) = 27.56, p < 0.001). Post hoc pairwise comparison showed that older men living alone differed significantly in a negative direction from co-habiting older men (p < 0.001) and older women living alone (p < 0.001). However, it should be stated that, although just 1 per cent of preventive home visitors described the wellbeing of older men living alone, in general, as ‘very good’, 41 per cent rated their general wellbeing as ‘good’ and no one described it as ‘very poor’.
Significant differences in responses between preventive home visitors in rural and urban municipalities were found regarding the men's need for help to pass the time (χ2 = 9.78, degrees of freedom (df) = 4, p = 0.04), which was higher in urban municipalities. Preventive home visitors in urban municipalities also had more experiences of not being able to offer an older man living alone the kind of social or health-care service they deemed appropriate for him (76.2% in urban municipalities versus 50.6% in rural municipalities; χ2 = 7.62, df = 1, p = 0.006). It was a more widespread opinion in rural municipalities that the older men regarded the services they were offered as relevant (76.5% versus 59.5%; χ2 = 3.91, df = 1, p = 0.048).
The 16 items regarding identified needs of older men living alone (Table 1) were divided into three groups: social and psychological needs, somatic health and health promotion needs, and practical needs (see Figure 1). Based on the responses, a mean score was calculated for each of these groups (1 = to a large extent … 5 = not at all). There were significant differences between the three groups of needs (one-way ANOVA, F(2) = 141.278, p < 0.001). Post hoc analyses showed that social and psychological needs were significantly more prominent than somatic health/health promotion needs and practical needs (p = 0.02), and that somatic health/health promotion needs were significantly more widespread than practical needs (p = 0.03).
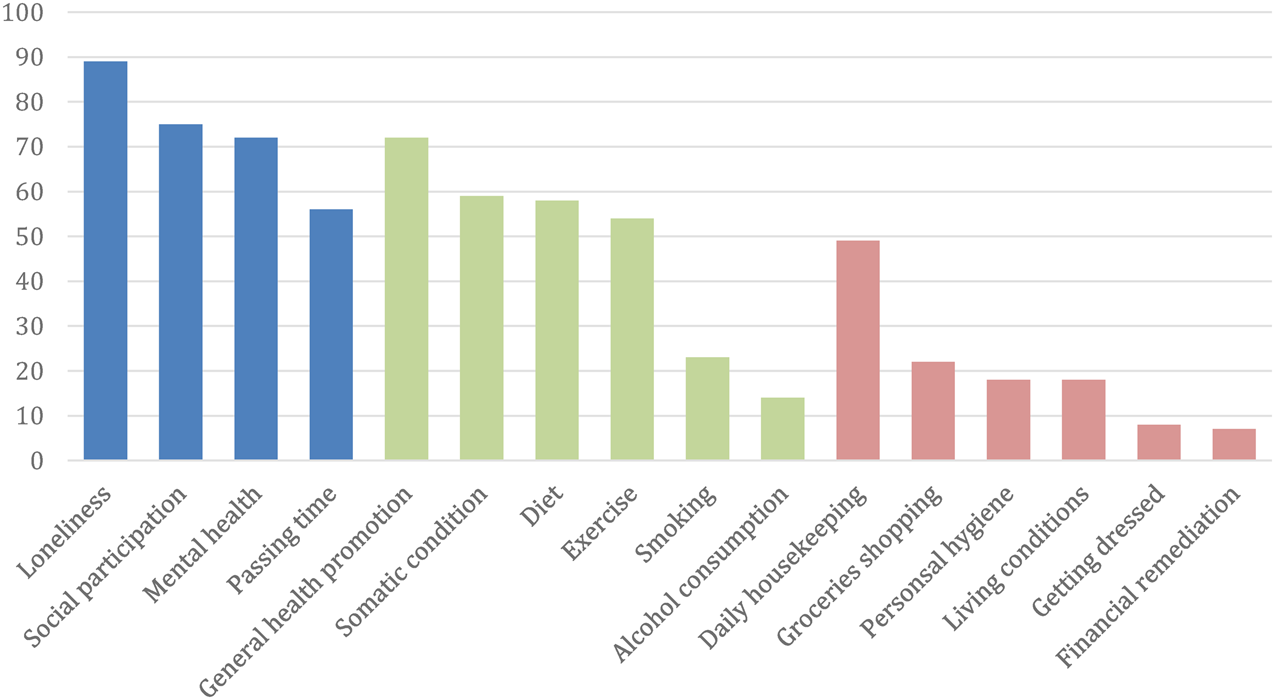
Figure 1. Needs split into the categories of social and psychological (four items), somatic health and health promotion (six items) and practical needs (six items).
Table 1. Needs of older men living alone as seen by preventive home visitors
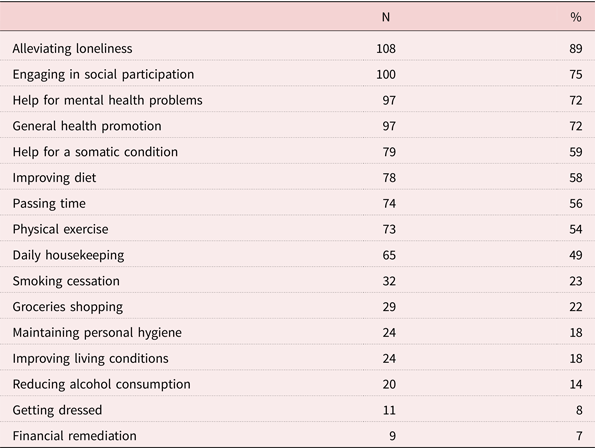
Note: Answers ‘to some extent’ and ‘to a large extent’ collated.
The main needs of older men living alone seem to be related to social and psychological matters, with social participation and loneliness standing out. The need for help with practical matters such as getting dressed, maintaining personal hygiene, shopping for food, improving living conditions or managing finances were assessed as virtually non-existent. For these categories, the options ‘to a lesser extent’, ‘almost not’ and ‘not at all’ combined accounted for 78–93 per cent of the answers and, for all of these categories, the most frequent answer was ‘not at all’. A need for cleaning and other housekeeping seemed more prevalent.
There were no differences in the needs of divorcees, widowers or bachelors, except divorcees were more often in need of financial help (χ2(4) = 9.94, p = 0.04).
Time lived alone was associated with the need for help to pass the time. Men who had lived alone for less than a year had the highest need, and men who had lived alone for more than ten years had the lowest need, when tested with Spearman's rank correlation coefficient (r s(121) = 0.195, p = 0.008). Time lived alone was also associated with the need for help to handle a somatic disease (r s(121) = 0.209, p = 0.02), though this association might be explained by a presumably larger mean age for men living alone for a long time.
A poorer financial situation (as estimated by the preventive home visitors) was furthermore associated with needs related to smoking (χ2(3) = 9.04, p = 0.03), hygiene (χ2(3) = 11.77, p < 0.001) and living conditions (χ2(3) = 10.57, p < 0.001). A better financial situation, on the other hand, was associated with an increased need for help to deal with alcohol consumption (χ2(3) = 12.42, p < 0.001).
Self-reported data from the older men
Out of a total of 29,791 men aged over 60, 5,791 state that they live alone (19.4%). Of these, 1,877 (32.4%) are divorced, 2,144 (37.0%) are widowers and 1,224 (21.1%) are unmarried; 457 (7.9%) are married but live alone. The men living alone were categorised according to self-declared highest level of education. We used five categories based on the Danish educational system: primary education, lower education and three categories of further education: short (1–2 years), middle (3–4.5 years) and long (5–6 years). Those men with an unspecified level of education (‘other education’, N = 427; ‘under education’, N = 32) were not included in the data material. There is an age difference between the groups (F(6) = 12.346, p = 0.007). A post hoc test shows that men with long, further education and men with a primary education are slightly older than the intermediate groups (p = 0.02).
The results are summarised in Tables 2–5. It is noteworthy that older men living alone rate their physical and mental health, level of stress, perceived social support and feelings of being unwanted alone as worse than older men who are co-habiting and, in all cases, the differences are highly significant (p < 0.001). In addition, regarding social relations, a Mann–Whitney test showed significant differences between men living alone and men co-habiting concerning contact with family (U = 40,138,523.5, Z = 11.75, p < 0.001), friends (U = 38,693,864.0, Z = 12.88, p < 0.001), neighbours (U = 40,991,276.5, Z = 5.63, p < 0.001) and other acquaintances (U = 34,251,683.0, Z = 9.88, p < 0.001). Though most differences are in favour of men co-habiting, it is noteworthy that, regarding contact with friends, men living alone appear more frequently at both extremes, with 6.1 per cent saying they ‘never’ have contact with friends and 28.7 per cent saying they have contact ‘on a daily basis’, whereas the corresponding numbers for co-habiting men are 1.8 and 15.8 per cent, respectively.
Table 2. Health scores (self-rated) by living arrangement
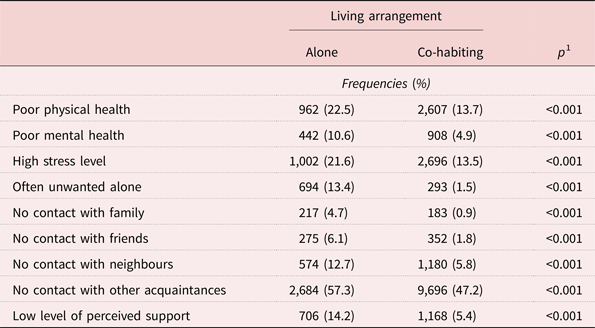
Note: 1. Mann–Whitney U-test.
Table 3. Health scores (self-rated) among older men living alone by area of residence
Note: 1. Mann–Whitney U-test.
Table 4. Health scores (self-rated) among older men living alone by marital status
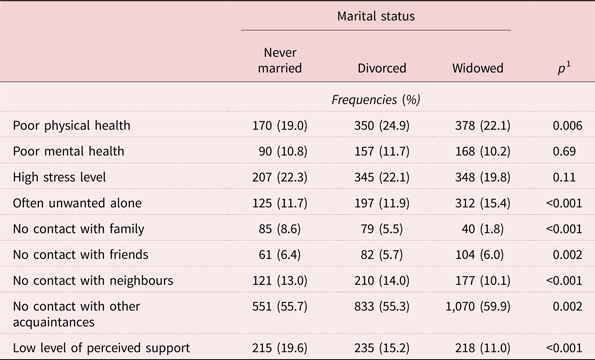
Note: 1. Kruskal–Wallis H test.
Table 5. Health scores (self-rated) among older men living alone by educational level
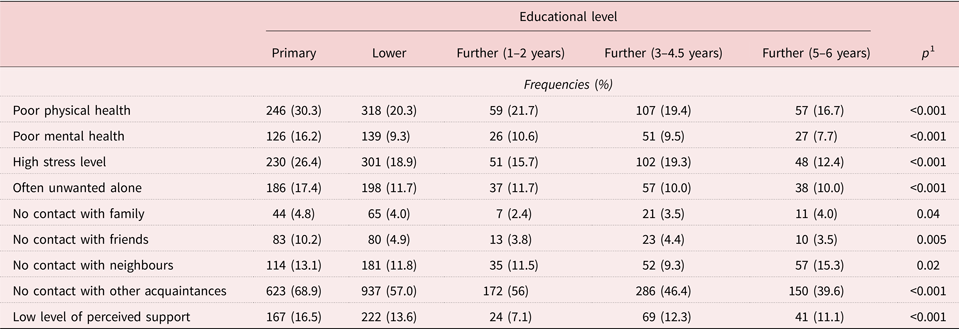
Note: 1. One-way analysis of variance.
We then compared sub-groups of older men living alone with each other. A one-way ANOVA test showed significant differences between educational groups on both the physical health score (F(4, 3,806) = 25.513, p < 0.001) and the mental health score (F(4, 3,806) = 15.177, p < 0.001). There were also significant differences in perceived stress (F(4, 4,045) = 22.197, p < 0.001). Table 6 shows the mean score for each educational level. A higher score indicates better self-perceived mental and physical health measured with the SF-12, while a higher stress score indicates a higher self-perceived stress level measured with the Perceived Stress Scale. Remarkably, among the older men living alone, pairwise comparison showed that men with a primary education score significantly lower than those with longer educations on 11 of the 12 items of the SF-12, the exception being the item ‘Have you been feeling sad?’, where there are no differences. On the total SF-12 score, pairwise comparison showed that men with a primary education score significantly lower than all other educational groups (in all cases p < 0.001). On the Perceived Stress Scale, men with a primary education score significantly higher than men with a long, further education on five out of the ten items and significantly higher than all other educational groups on the total score (in all cases p < 0.001). On the mental health score, only men with a primary education differed significantly in a negative direction from the other groups (in all cases p < 0.001). Finally, there were significant differences between groups on measures of feeling unwanted alone (χ2(12) = 46.20, p < 0.001) and perceived social support (χ2(12) = 42.36, p < 0.001), where men with a primary education stood out for negative reasons.
Table 6. Mean score on selected health measures by educational level
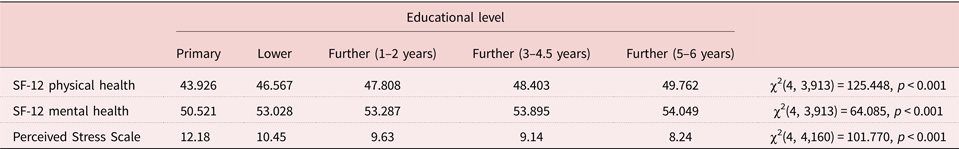
Note: SF-12: 12-item short-form health questionnaire.
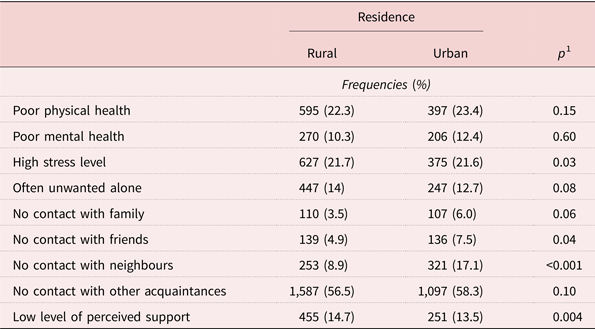
When differentiating between rural and urban living, there were no significant differences on the physical and mental health components or the stress score. Small but significant differences emerged on the availability of social support (Mann–Whitney, U = 3,327,542, Z = −2.916, p = 0.004) in favour of the urban residents: 13.5 per cent of urban residents felt they never had anyone to talk to when in trouble or need of support and 15.1 per cent felt they sometimes did; for residents of rural areas, these numbers were 14.7 and 15.6 per cent, respectively. Significant differences between the groups also exist regarding contact with friends (Mann–Whitney, U = 3,181,289, Z = −2.005, p = 0.04) and neighbours (Mann–Whitney, U = 2,856,571, Z = −7.365, p < 0.001), both in favour of the rural residents. Whereas 7.5 per cent of men living alone in urban areas are never in contact with friends and 17.1 per cent never get in touch with neighbours, this is the case for just 4.9 and 8.9 percent, respectively, of men living alone in rural areas. There were no significant differences regarding contact with family, other acquaintances and feeling unwanted alone.
Widowers were prevalent in the responses in our first sub-study, so we compared answers based on reason for living alone to see if any self-reported differences emerged. No differences were found when comparing mental health or level of stress, but a significant difference was found on physical health (F(4, 4,666) = 3.643, p = 0.006). Nineteen per cent of the men who had never married reported poor physical health, compared with 22.1 per cent of widowers and 24.9 per cent of divorcees. Substantial differences appear on the social measures, as shown in Table 4. Regarding the perceived social support, men who have never been married score lower than widowers with divorcees scoring in between (Kruskal–Wallis, χ2(2) = 99.66, p < 0.001), but this pattern is the opposite for feeling unwanted alone, with widowers reporting this to a higher degree (Kruskal–Wallis, χ2(2) = 40.92, p < 0.001). Significant differences exist between groups concerning social contacts but no unequivocal pattern appears. Differences are small but significant regarding contact with friends (Kruskal–Wallis, χ2(2) = 12.60, p = 0.003) and more pronounced in the case of family (Kruskal–Wallis, χ2(2) = 230.93, p < 0.001) and neighbours (Kruskal–Wallis, χ2(2) = 31.81, p < 0.001), all in disfavour of men who have never been married. Whereas divorcees have the greater degree of contact with friends, widowers are more in contact with family and neighbours. Small but significant differences exist in contact with former colleagues, with widowers being less in contact, divorcees more and never married men falling in between (Kruskal–Wallis, χ2(2) = 12.60, p = 0.002).
Registry-based information of use of health-care services
For the third part of the study, the sample population consisted of 57,966 men above the age of 60, of whom 14,505 were living alone and 43,461 were co-habiting. The mean age of those living alone (72.5 years) was significantly higher than of those co-habiting (70.1 years, p = 0.007). Therefore, direct age standardisation was conducted when comparing the two groups. The weights used correspond to the age distribution in the Danish population in 2014.
For older men, living alone is associated with a significantly greater probability of having used a GP, a psychiatrist, preventive home visits and domestic help within the last 12 months compared with co-habiting (see values in Table 7). In addition, older men living alone visit the GP more frequently, with a mean of approximately one extra visit per year. Living alone is associated with a shorter duration of domestic care but a longer duration of practical help. Finally, it is also associated with a higher number and a longer duration of hospital admissions compared with co-habiting men. Living alone is, on the other hand, associated with a smaller probability of using a dentist, physiotherapist, ophthalmologist, dermatologist and outpatient hospital visits. For those utilising these services, however, men living alone use a physiotherapist, dermatologist and outpatient hospital visits to a greater extent than co-habiting men.
Table 7. Health service utilisation by living arrangements

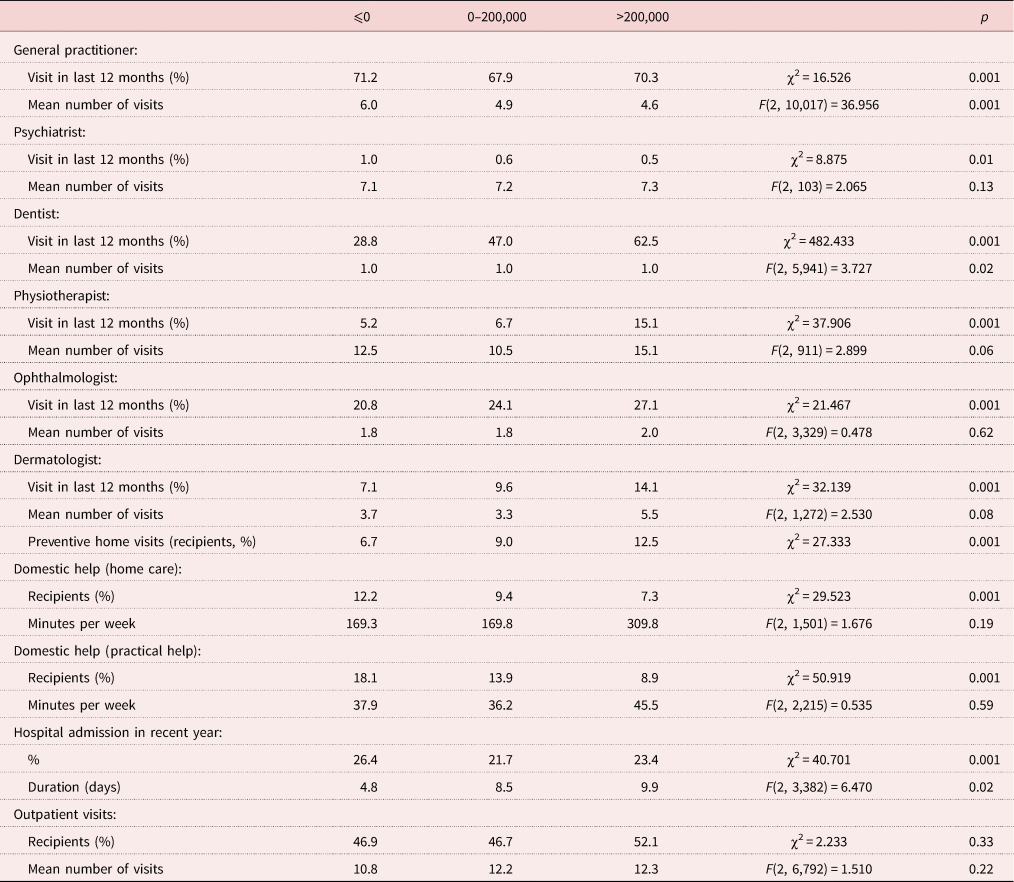
As shown in Table 8, living alone in rural municipalities is associated with a lower probability of using a range of specialised services (a psychiatrist, dentist, dermatologist and physiotherapist) and of being hospitalised. Though there are no differences in the probability of outpatient hospital visits, rural residents have fewer hospital visits per outpatient. Living in rural municipalities is also associated with a lower probability of receiving domestic practical help but with a longer duration of the help received. There are no differences in use of GP, preventive home visits and domestic home care.
Table 8. Health service utilisation by area of residence

Lower education among older men living alone is associated with a greater probability of using a GP, domestic help and preventive home visits but a lower probability of using a dentist, dermatologist, physiotherapist and psychiatrist (Table 9). There are no differences in the probability of hospital admissions and outpatient visits. Income shows almost the same pattern, though the results show that those with a low income use a psychiatrist more and an ophthalmologist and preventive home visits less (Table 10).
Table 9. Health service utilisation by educational level
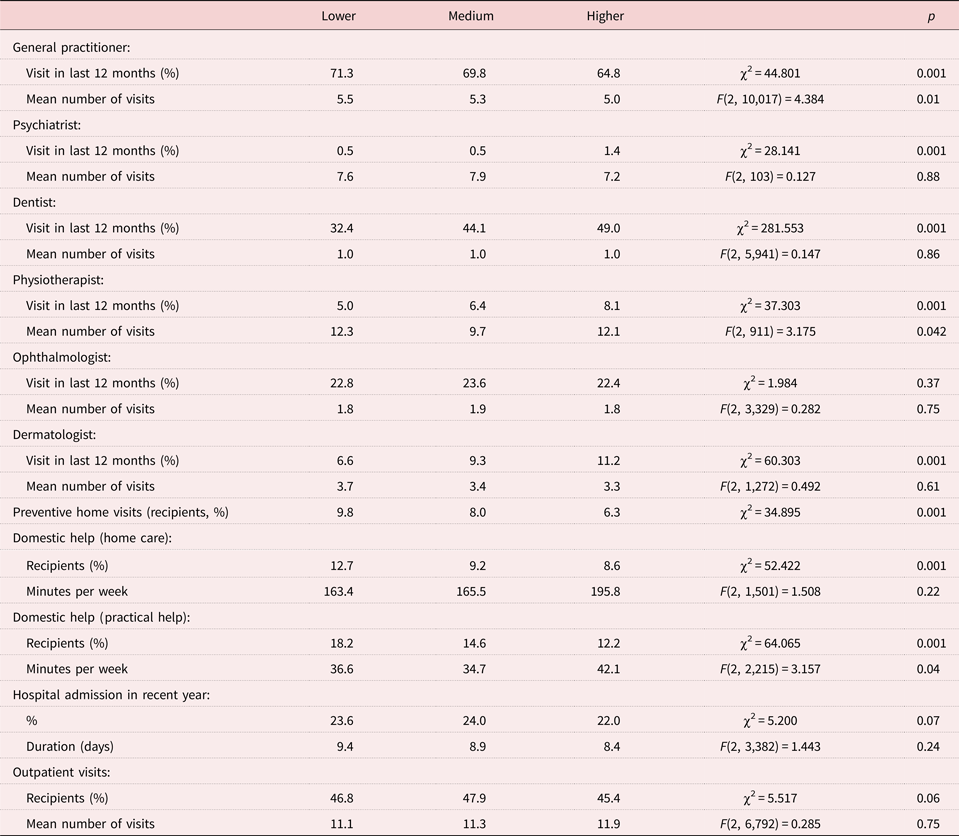
Table 10. Health service utilisation by income (kroner)
Discussion
Overall, the results add further weight to studies that consider older men living alone an at-risk group compared with older men living with others. This was the opinion of the preventive health-care professionals who visit the men in their homes, and it was reaffirmed by the men themselves through self-report data. The men reported poorer physical and mental health, more stress, less social contact and social support, and feeling more unwanted alone. These results are in line with those reported by other researchers (e.g. Kharicha et al., Reference Kharicha, Iliffe, Harari, Swift, Gillmann and Stuck2007) on the health-related downsides of living alone. In addition, the results point to a social gradient in health among older men living alone. We found socio-economic status, as indicated by educational level, to be thoroughly associated with lower health scores thereby attesting to the widespread literature on social inequities in health (e.g. Huisman et al., Reference Huisman, Kunst and Mackenbach2003; Mackenbach et al., Reference Mackenbach, Stirbu, Roskam, Schaap, Menvielle, Leinsalu and Kunst2008). On all self-report measures, individuals with no further education beyond primary education stand out negatively compared with other groups.
Though research shows that living alone in old age is associated with an increased use of GPs (Dreyer et al., Reference Dreyer, Steventon, Fisher and Deeny2018), older men living alone are often portrayed through a ‘vulnerability narrative’ that also implies a lack of agency (Leontowitsch et al., Reference Leontowitsch, Fooken and Oswald2019). This includes a lack of help-seeking behaviour which might be further accentuated by masculine norms (Courtenay, Reference Courtenay2000). We find that older men living alone actually do use their GP to a greater extent than men living with others. When differentiating between men living alone according to socio-economic factors, we see that men with less education and less income also make greater use of their GP. We were not able to control for the actual need to see a doctor, and there may therefore still be inequities concealed in the data. In another study, Terraneo (Reference Terraneo2015) controlled for this and found no differences in the use of GPs.
The men living alone and especially the men with a low educational level made lesser use of more specialised and often partly self-funded services such as dental care. This is consistent with other findings on the association between educational level and health-care utilisation (van Doorslaer et al., Reference van Doorslaer, Koolman and Jones2004, Reference van Doorslaer, Masseria and Koolman2006). They did, however, make greater use of free-of-charge outreach services such as preventive home visits and domestic help, particularly practical help. One interpretation of this might be that these men adapt to their situation by utilising the readily accessible parts of the welfare state in organising their existence, thereby ‘ageing in place’ and underlining the role of the welfare society and old-age policies when choosing to live alone (Reher and Requena, Reference Reher and Requena2018). This might add nuance to the picture of miserable single men, but matters of somatic and mental health remain.
A related finding is that, although the self-report data reveal an expected association of low socio-economic status with poorer health, the survey with preventive home visitors actually demarcates a group of economically well-off individuals in need of intervention. This group consists of 27.3 per cent of the men, and it highlights the need to look at different configurations of men living alone and not simply men with limited financial means. The well-off men might also be rendered invisible in advanced old age with the current emphasis on health inequities.
Previous research into rural–urban differences has found a lesser degree of health-care and preventive health-care utilisation in rural areas (Casey et al., Reference Casey, Call and Klingner2001; Cohen et al., Reference Cohen, Manuel and Sanmartin2016). This picture is partly replicated in our register-based data, where we found that residents in rural areas used more specialised health-care services less frequently than their urban counterparts. One hypothesis might be that this is an indication of underlying differences in educational level and can thus be explained by our results on education, but this is contradicted by our self-report data. We did not find any significant physical or mental health differences between rural and urban residents nor any differences in the number of men with a high stress level. These results align with the finding that there are no differences in the use of GPs. While there might be inequities in the use of certain services, it does not seem warranted to point to social inequities in health and wellbeing in disfavour of rural residents. Another explanation might instead be that of cultural differences in rural and urban ways of life. It is a well-known phenomenon among GPs that these regions present different demands for health-care services. Yet it may also be a contributing factor that specialised services are simply not as readily available in rural municipalities (Hicks, Reference Hicks1990; Merwin et al., Reference Merwin, Snyder and Katz2006).
Furthermore, our results from the electronic survey with preventive home visitors showed that it was in rural areas that passing time was easier, and it was also in these areas that available health care and social services seemed of more relevance. One might expect more densely populated municipalities to offer a greater variety of health and social services and volunteer initiatives, but, if this is the case, they do not seem to reach these men. This might be partly explained by better social integration in rural areas, where higher degrees of social participation have been reported (Greiner et al., Reference Greiner, Li, Kawachi, Hunt and Ahluwalia2004). This is somewhat supported by our self-report data. Though urban residents reported slightly more perceived social support, there was a clear discrepancy between the groups regarding contact with friends and neighbours. Individuals in rural municipalities seemed more connected.
The results should also be seen in light of previous studies indicating greater health problems in urban areas (Nummela, Reference Nummela, Nyqvist and Forsman2015) and better psychological wellbeing for older men living outside the larger cities (Hansen and Greve, Reference Hansen and Greve2016). Though the corresponding differences in our study did not reach significant levels, these studies and our results regarding social relations paint a different picture than the prevailing image of depleted rural areas where people are left behind.
Social relations
At the beginning of this article, we distinguished between living alone, social isolation and loneliness. In our study, we found that living alone is associated with higher rates of loneliness, but we also noticed a need to nuance the vulnerability narrative.
The preventive home visitors identify loneliness and a lack of social participation as the biggest problems among men living alone. The men themselves also score higher on loneliness measures, though we should highlight that it is still a minority (13.4%) of men living alone that often feel unwanted alone. These findings might not be surprising since other studies have identified living alone as a risk factor for loneliness (Hansen and Slagsvold, Reference Hansen and Slagsvold2016).
The lonely widower is perhaps the most stereotypical image of the vulnerable older man, and widowers do stand out in our data. Despite widowers making up just 58.3 per cent of the population of men over 75 living alone (according to Denmark's Statistics databases), preventive home visitors described a widower in 70.5 per cent of their survey responses. Since the number of widowers rises substantially with age, and since we do not know the exact age distribution in our first study, their overrepresentation could be due to old age rather than widowhood itself. This result is, nevertheless, in line with other research suggesting that widowers in general have problems adjusting to solo living (Hansen and Greve, Reference Hansen and Greve2016).
In our data, this vulnerability seems limited to loneliness. There are no differences in the mental health or level of stress between widowers, divorcees and bachelors. There is a difference between groups on the measure of somatic health, but this puts divorcees more at risk. In our study, widowers report feeling more unwanted alone. Yet they are also more in contact with family and neighbours and have higher levels of perceived social support. This indicates that it is more of an emotional loneliness related to a specific person, their late wife, than a social loneliness (Weiss, Reference Weiss1973; Munk et al., Reference Munk, Smærup, Hansen, Beck, Højlund and Thomasen2016) and points to resources in their environment.
Men who had never married were less lonely, but they also had lower levels of perceived social support, and they were, indeed, in contact less with family, friends and neighbours (based on mean ranks of the groups: the percentage of divorcees with no contact at all to neighbours was actually higher, as seen in Table 4, perhaps because of their moving out of familiar surroundings following a divorce). One interpretation might be that – possibly lifelong – single lifestyles have made men who were never married more accustomed to a life with fewer social contacts (Tornstam, Reference Tornstam2011). They may therefore be more in need of social support interventions when trouble arise whereas widowers may also benefit from emotional support interventions. Divorcees might be a more heterogeneous group with some of these men warranting attention. This group shows worse average somatic health and the highest percentages of isolation from neighbours. In addition, in our first sub-study, men in this group were more often in need of financial help.
Concluding remarks and implications
Our study has revealed that paying particular attention to older men living alone is warranted, and it has highlighted necessary foci for interventions. According to preventive home visitors, older men living alone pose a challenge to the health-care system since they are hard to connect to and need further specialised health and social care, particularly regarding social participation. These men self-report their health and wellbeing as worse than co-habiting men and use certain, primarily specialised, health services to a lesser extent. They do, however, make greater use of free health care such as the GP, home care and preventive home visits. They do not all have the same needs: socio-economic status is associated with low scores on all health measures, being widowed is associated with loneliness, and living in the cities is associated with difficulties utilising social services and possibly with being less socially integrated.
Key to future social and health-care initiatives might be an alertness to the fact that men living alone, in particular men with little education, do utilise certain health-care services more than their counterparts – those services that are readily accessible and free of charge. GPs are usually found within close distance of most people, and home care services and preventive home visits are outreach services. It may, therefore, prove vital to use and further develop these readily accessible services as vessels to combat health inequities (Frausing et al., Reference Frausing, Smærup, Maibom and Munk2020). In support of this, older people living alone who receive home care are hospitalised half as much and for half as long as those who do not receive home care (Deloitte, 2013). This difference is greater than when comparing co-habiting recipients and non-recipients.
A relevant question in this regard might be when and to whom preventive home visits should be offered. A change of law in 2020 means that older persons receive a preventive home visit at 75 but then only again at 82, after which they receive visits on an annual basis (Danish Health Authority, 2020). The focus on living alone has now led to an additional visit to persons living alone in the year they turn 70. In addition, municipalities must offer preventive home visits ‘as needed’ for individuals between 65 and 81 who are at particular risk of reduced social, physical or psychological functioning. What this means is not fully developed. Our results can orient policy makers and practitioners towards older men living alone and help them differentiate among them. Developing the home visit service to suit the needs of men is a difficult endeavour. Previous research has shown that only older women benefit from increased training of the home visitors (Vass et al., Reference Vass, Avlund, Kvist, Hendriksen, Andersen and Keiding2004). Future work on this service should take the particular situations of widowers, divorcees and bachelors as well as urban versus rural residents, respectively, into consideration. We recommend qualitative research on older men's use of GPs and preventive home visits to illuminate relevant processes. Finally, policy makers should take note of the differential use of often partly self-funded specialists and address barriers to equal access.
Strengths and limitations
This study has a number of strengths. By relying on both the men's subjective evaluations of their own health, objective measures for their health-care utilisation and the professional view of the preventive home visitors, we provide a multifaceted presentation of the health and needs of older men living alone. Many studies of health-care utilisation have relied on survey data or self-reported utilisation (Dreyer et al., Reference Dreyer, Steventon, Fisher and Deeny2018). We use register-based data, which is not subject to selection bias and avoids the difficulties associated with men's possible under-reporting of health-care utilisation. We should also emphasise that, in our first sub-study, we gain insight into the lives of individuals otherwise deemed invisible to the health-care system, namely older men who live alone and do not receive home care services.
There are, however, some limitations to the study. Previous research has indicated that men may be less likely to seek help for or admit to health problems (Courtenay, Reference Courtenay2000; Yousaf et al., Reference Yousaf, Grunfeld and Hunter2015), which may include an unwillingness to report their loneliness on a survey (Nicolaisen and Thorsen, Reference Nicolaisen and Thorsen2014; de Jong-Gierveld et al., Reference de Jong-Gierveld, Tilburg, Dykstra, Vangelisti and Perlman2018). It is therefore possible that our data on, for example, health and loneliness may be somewhat optimistic. However, since we mainly focus on the relative positions of different groups of men, we do not expect this to influence our main results.
Our first and second studies might be susceptible to selection bias. We might have data on the more resourceful respondents. We also acknowledge that the estimates of the preventive home visitors might be subject to a possible recollection bias. However, our aim was to acquire these professionals’ impressions, which will inevitably involve a degree of subjectivity, and we tried to counter a possible generalisation bias by restricting their evaluation to the most recent man they visited.
Acknowledgements
The authors wish to thank the preventive home visitors for their participation.
Author contributions
The authors all declare to have contributed to the research project and article.
Financial support
This work was supported by the EGV Foundation and the Velux Foundation. The Danish National Health Survey 2013 was funded by The Capital Region, Region Zealand, The South Denmark Region, The Central Denmark Region, The North Denmark Region, The Ministry of Health and the National Institute of Public Health, University of Southern Denmark.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
Approval for this project was granted by the Danish Data Protection Agency (J.nr. 2015-41-3795). No further ethical approval was required.















