Background
Staphylococcus aureus (staph) bacteremia holds substantial clinical significance and represents a public health concern, being a leading cause of both community-acquired and hospital-acquired bacteremia. Reference Rhee, Aroutcheva, Hota, Weinstein and Popovich1,Reference El Atrouni, Knoll, Lahr, Eckel-Passow, Sia and Baddour2 Staph bacteremia has a mortality rate up to 30% and often requires prolonged antimicrobial therapy. Reference Chong, Moon, Bang, Park, Park and Kim3,Reference Chang, MacDonald, Peacock, Musher, Triplett and Mylotte4 Methicillin-resistant S. aureus (MRSA) is recognized as an enduring threat and has been classified as a high-priority pathogen by the World Health Organization. Reference Tacconelli, Carrara, Savoldi, Harbarth, Mendelson and Monnet5 However, the incidence of methicillin-susceptible S. aureus (MSSA) and MRSA bacteremia has shown temporal fluctuations, with varying trends observed across different geographic regions. Reference Kourtis, Hatfield, Baggs, Mu, See and Epson6–Reference Hindy, Quintero-Martinez, Lee, Scott, Gerberi and Mahmood10 Earlier research suggests that MRSA tends to lead to additional infections rather than replacing those caused by MSSA, and trends in MRSA and MSSA may diverge based on infection site and population characteristics. Reference Kourtis, Hatfield, Baggs, Mu, See and Epson6,Reference Mostofsky, Lipsitch and Regev-Yochay11–Reference Klein, Mojica, Jiang, Cosgrove, Septimus, Morgan and Laxminarayan13
Between 2005 and 2018, data extracted from the European Antimicrobial Resistance Surveillance Network revealed a statistically significant upswing in the incidence of staph bacteremia within the European Union and European Economic Area (EU/EEA). Reference Gagliotti, Hogberg, Billstrom, Eckmanns, Giske and Heuer9 Notably, this surge primarily stemmed from an increase in MSSA bacteremia cases, while the incidence and proportions of MRSA bacteremia diminished throughout the same timeframe within the EU/EEA.
Conversely, in the United States, analysis of electronic health records from over 400 acute-care hospitals, in conjunction with population-based surveillance data from the Centers for Disease Control (CDC) and Prevention’s Emerging Infections Program (EIP), showed a national reduction in MRSA bacteremia in healthcare settings, averaging approximately 17% annually between 2005 and 2012. Reference Kourtis, Hatfield, Baggs, Mu, See and Epson6 Nonetheless, a noteworthy deceleration in these reductions was observed from 2012 to 2017, raising concerns. Reference Kourtis, Hatfield, Baggs, Mu, See and Epson6 The same author also noted that hospital-onset (HO) MSSA bacteremia remained relatively stable, while community-onset (CO) MSSA bacteremia infections showed a slight increase from 2012 to 2017. Another study in the United States reported a sharp decline in staph infections, including bloodstream and non-bloodstream infections, from 2005 to 2017 in U.S. Department of Veterans Affairs medical centers, with most reductions attributed to decreases in MRSA infections. Reference Jones, Jernigan, Evans, Roselle, Hatfield and Samore14 Moreover, a population-based study in Minnesota examining the incidence of monomicrobial staph bacteremia between 2006 and 2020 demonstrated that there was no apparent temporal trend over 15 years with a stable incidence. Reference Hindy, Quintero-Martinez, Lahr, Palraj, Go and Fida15 While some studies have examined the trend of staph bacteremia, research on the trends in CO and HO staph bacteremia is limited, especially in the United States. This research gap may become increasingly clinically relevant with the forthcoming launch of volunteer reporting of Hospital Onset Bacteremia & Fungemia (HOB) events by the CDC/National Healthcare Safety Network (NHSN) in the United States. 16
Our primary objective is to elucidate trends in staph bacteremia incidence, categorized by methicillin susceptibility (MRSA versus MSSA) and onset designation (CO vs. HO), in the United States. Additionally, we assess patient demographics, characteristics, mortality, length of stay (LOS), and costs among patients with staph bacteremia and compare them to those without staph bacteremia.
Methods
Study design and population
We conducted an epidemiological study, evaluating the microbiological data among adult patients, aged 18 years or older, who were admitted to any of the 267 acute-care hospitals assessed in the BD Insights and Research Database (Becton Dickinson, Franklin Lakes, NJ) during the period spanning from October 1, 2015, to February 28, 2020. The hospital demographic distribution of 267 acute-care hospitals is shown in Supplemental Table 1a. This database incorporates electronically recorded laboratory results, pharmacy records, patient demographics, administrative data, as well as admission, discharge, and transfer data. Reference Kaye, Gupta, Mulgirigama, Joshi, Scangarella-Oman and Yu17–Reference Yu, Ye, Edwards, Gupta, Benin, Ai and Dantes19
As claims data were available for a subset of facilities (41 out of the 267 acute-care hospitals), we conducted a retrospective cohort study limited to those hospitals to assess mortality rates, length of hospital stays, and associated costs. The hospital demographic distribution of 41 acute-care hospitals is shown in Supplemental Table 1b. Additionally, we conducted a case-control study comparing individuals with and without staph bacteremia to investigate differences in LOS, mortality, 30-day readmission, and total cost. This study received approval as a limited retrospective dataset for epidemiological analyses and was granted an exemption from the requirement for consent by the New England/WCG Institutional Review Board and Human Subjects Research Committee (Wellesley, MA). The study was executed in strict accordance with the regulatory standards set forth by the Health Insurance Portability and Accountability Act.
Outcomes and definitions
In our analyses, we considered the day of admission as “day 1.” An HO MSSA and HO MRSA was defined as the first positive blood culture with MSSA or MRSA, which begins on day 4 or later of the hospital stay, consistent with the HOB definition planned by the NHSN at the time of writing. CO MSSA and CO MRSA were defined as a first positive blood culture with a MSSA or MRSA as defined by the CDC within the first 3 days of hospital admission. Reference Yu, Ye, Edwards, Gupta, Benin, Ai and Dantes19 The control group was defined as inpatient admissions with at least one blood specimen collection but without any positive staph bacteremia identified. Therefore, the control group included those with negative blood cultures and those with positive blood cultures for bacteria other than Staphylococcus aureus.
Variables assessed include age, gender, year of diagnosis, payor class, presence of intensive care (ICU) admission, LOS in the ICU, Acute Laboratory Risk of Mortality Score (ALaRMS, an EHR-derived comorbidity measure), Reference Tabak, Sun, Nunez and Johannes20 total LOS in the hospital, payor type, readmission within 30 days, and in-hospital mortality, and hospital-level variables (hospital staffed bed size, hospital teaching status, hospital urbanicity, hospital region (CDC geographics census division [9 divisions]). 21 We noted whether patients with staph bacteremia had any of the following six infectious disease diagnoses commonly associated with staph bacteremia: central line-associated bloodstream infection, infective endocarditis, musculoskeletal infections, phlebitis and thrombophlebitis, pneumonia, and skin and soft tissue infection. Reference Inagaki, Weinberg and Kaul22 The International Classification of Diseases, 10th Revision (ICD-10 codes) were employed to identify these six diagnoses (please refer to Supplemental Table 2 for code details). Rural vs. urban patient residence was determined using Rural Urban Commuting Area codes linked to ZIP codes. 23
Statistical analysis
For the epidemiological study, we plotted the incidence of CO staph bacteremia stratified by methicillin susceptibility over time. The incidence of CO MSSA/MRSA was computed by dividing the number of CO MSSA/MRSA admissions by the total count of inpatient admissions, multiplied by 1000. As the risk of HO bacteremia may vary with the duration of patient admission, we also produced separate plots for HO MSSA/MRSA. The incidence of HO MSSA/MRSA was determined by dividing the number of HO MSSA/MRSA admissions by the total patient days at risk, multiplied by 1000. If admissions included CO MRSA/MSSA cases, the patient days at risk were excluded from the denominator of HO MRSA/MSSA. Patient days at risk were defined as the number of days from the commencement of admission to the occurrence of the event, excluding days following the fulfillment of one of the infection criteria. To assess the trend in the incidence rates for total MSSA, total MRSA, CO MSSA, HO MSSA, CO MRSA, and HO MRSA, we employed the generalized estimating equations technique using the Poisson distribution. To quantify the change in the incidence over time, we used Poisson regression models to estimate the incidence rate ratio with 2015 quarter 4 as the reference.
For the retrospective study, we summarized patient characteristics, hospital characteristics, diagnoses potentially linked to staph bacteremia, and clinical outcome, including mortality rates, LOS, total cost, and 30-day readmission based on methicillin susceptibility and onset location (CO versus HO), employing the subset data. For the case-control study, we fit multivariable regression models to identify whether there was any difference in mortality, LOS, total cost, and 30-day readmission between those with and without staph bacteremia. The control group comprised individuals who had at least one blood culture but tested negative for staph bacteremia. We used Poisson regression for modeling LOS, gamma regression for total cost, and binomial regression for mortality and 30-day readmission. The models were adjusted for age, sex, ALaRMS, Reference Tabak, Sun, Nunez and Johannes20 payor, number of staffed beds, hospital teaching status, and hospital urbanicity. All analyses were carried out using R software version 4.1.2 software (R Foundation for Statistical Computing, Vienna, Austria) with R Studio (Boston, MA).
Results
During the study period, we observed a total of 9,202,650 admissions across 267 acute-care hospitals. The incidence of total MSSA remained relatively stable and showed a significant increase, rising from 2.43 per 1,000 admissions in the fourth quarter of 2015 to 2.87 per 1,000 admissions in the first quarter of 2020 (rate ratio: 1.18, 95% CI (1.09, 1.29), 2020 Q1 versus 2015 Q4). The CO MSSA showed similar patterns as total MSSA. (P for trend <0.0006; see Figure 1; Supplemental Table 3). The incidence of CO MRSA exhibited a steady increase, rising from 1.84 per 1,000 admissions in the fourth quarter of 2015 to 2.16 per 1,000 admissions in the first quarter of 2020 (P for trend < 0.0001, Figure 1). The incidence of total MRSA followed similar patterns as CO MRSA. However, the incidence of HO MSSA and HO MRSA remained relatively stable (P for trend was 0.3 and 0.4, respectively, Figure 2).

Figure 1. Trends of total and community-onset staph bacteremia (per 1,000 admissions) among 267 hospitals in the United States from 2015 to 2020. MSSA, methicillin-susceptible Staphylococcus aureus; MRSA, methicillin-resistant Staphylococcus aureus; CO, community-onset. P for trend: Total MSSA, <0.0006; CO MSSA, <0.0006; Total MRSA, < 0.0001; CO MRSA, < 0.0001.

Figure 2. Trends of hospital-onset staph bacteremia (per 1,000 patient days at risk) among 267 hospitals in the United States from 2015 to 2020. MSSA, methicillin-susceptible Staphylococcus aureus; MRSA, methicillin-resistant Staphylococcus aureus; HO, hospital-onset. P for trend: HO MSSA, 0.3; HO MRSA: 0.4.
During the same study period, data from the subset (41 acute-care hospitals) revealed a total of 645,315 admissions (Table 1). Within this subset, we recorded a total of 3,730 cases of staph bacteremia, with 2,066 (55.4%) classified as MSSA and 1,664 (44.6%) as MRSA. Among the 2,066 cases of MSSA, 1,829 (88.5%) were categorized as community-onset (CO) and 237 (11.5%) as hospital-onset (HO). Of the 1,664 cases of MRSA, 1,477 (88.8%) were CO, and 187 (11.2%) were HO. Among the six pre-defined infectious diseases potentially associated with staph bacteremia, the most frequent infectious disease diagnosis was skin and soft tissue infection for both MRSA and MSSA (27.3% in the MRSA group and 25.7% in the MSSA group, respectively), followed by musculoskeletal infection (26.6% and 24.9%). The mean LOS in days was 12.4 in the CO MRSA group, 24.8 in the HO MRSA group, 10.2 in the CO MSSA group, and 19.0 in the HO MSSA group. In-hospital mortality rates were 10.8% in the CO MRSA group, 25.1% in the HO MRSA group, 7.5% in the CO MSSA group, and 19.8% in the HO MSSA group. The total median costs were $20,300 in the CO MRSA group and $41,700 in the HO MRSA group, $17,300 in the CO MSSA group, and $33,400 in the HO MSSA group. The characteristics and clinical outcomes of the control group are shown in Table 1.
Table 1. Patient demographics, characteristics, and staph bacteremia-associated clinical outcomes from 41 acute-care hospitals in the United States between 2015 and 2022

Note: MSSA, methicillin-susceptible Staphylococcus aureus; MRSA, methicillin-resistant Staphylococcus aureus; CO, community-onset; HO, hospital-onset; ALaRMs Score, Acute Laboratory Risk of Mortality Score; LOS, length of stay (days).
The model estimated and association between staph bacteremia and LOS, mortality, readmission, and total cost, stratified by methicillin susceptibility and onset of location, is summarized in Table 2. Compared to those without staph bacteremia, LOS was significantly longer in the CO MRSA group (10.0 days vs. 6.6 days in the control group, p < 0.0001) and in the HO MRSA group (17.9 days vs. 6.6 days, p < 0.001). Mortality was significantly higher in the CO MRSA group (4.0% vs. 2.9%, p < 0.001) and in the HO MRSA group (12.3% vs 2.9%, p < 0.0001) compared to the control group. Readmission was more common in the HO MRSA group (14% vs. 10%, p = 0.036) but similar in the CO MRSA group (10% vs 10%, p = 0.7105) compared to the control group. Total cost was significantly higher in the CO MRSA group ($24,437 vs. $15,261, p < 0.0001) and HO MRSA group ($45,444 vs. $15,261 p < 0.0001) compared to those without staph bacteremia. A similar trend was observed in the CO MSSA and HO MSSA groups compared to the control group, except for readmission; readmission was similar to those without MSSA.
Table 2. Association between MRSA/MSSA with length of stay, mortality, 30-day readmission, and total cost
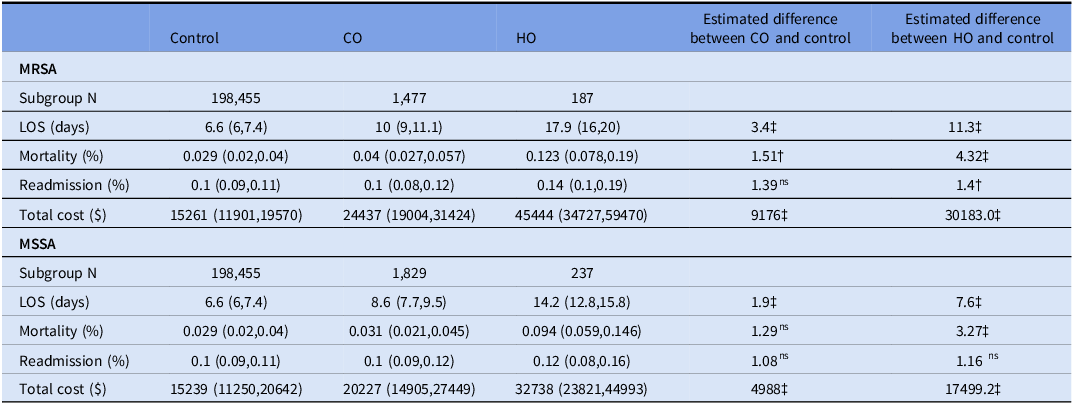
ns , not statistically significant; †, <0.05; ‡<0.0001.
Note. MSSA, methicillin-susceptible Staphylococcus aureus; MRSA, methicillin-resistant Staphylococcus aureus; CO, community-onset; HO, hospital-onset; LOS, length of stay (days); ICU, intensive care unit. Full model: Outcomes ∼ MRSA/MSSA (CO/HO) and adjusted for year (2015–2017 vs. 2018–2019), sex, age, ever ICU status, ALaRMs score, bed size, teaching hospital status, urbanicity, and region.
Discussion
This study revealed an increase in the incidence of MSSA and MRSA bacteremia between 2015 and 2020 across 267 acute-care hospitals in the United States. The primary driver behind this increase was CO bacteremia for both MSSA and MRSA. While HO MRSA demonstrated a decreasing trend from 2015 to 2018, as previously observed in similar studies, its incidence appeared to rebound in 2019 and 2020. Data obtained from a subset of 41 acute-care hospitals further highlighted that the most frequent infectious disease diagnosis associated with staph bacteremia was skin and soft tissue infection for patients with both MRSA and MSSA, followed by musculoskeletal infection. Compared to the control group, mortality, LOS, and total cost were all higher in those with staph bacteremia, regardless of methicillin susceptibility or onset location.
Staph bacteremia incidence is likely to vary based on the timing and locations of conducted studies, the risk factors prevalent in the studied population, and the infection control practices adopted in healthcare facilities. Reference Hindy, Quintero-Martinez, Lee, Scott, Gerberi and Mahmood10 NHSN at the CDC systematically gathers healthcare-associated infection (HAI) data from a wide array of healthcare facilities in the United States. 24 Nevertheless, the HAI report from NHSN exclusively covers CO and HO MRSA and does not encompass CO MSSA or HO MSSA. Although there are some efforts by EIP initiatives, with seven selected sites in the United States submitting data on invasive MSSA infections, including bacteremia, the true incidence and trend of staph bacteremia (both MSSA and MRSA) in the United States remain understudied.
This present study shows a significant increase in CO MSSA and CO MRSA between 2015 and 2020, with no significant changes observed in HO MSSA and HO MRSA. A similar trend has been observed in Europe. Reference Renggli, Gasser, Buetti and Kronenberg25 No observed increase in HO MSSA and MRSA bacteremia might be attributed to various infection control efforts, including improvements in preventing device- and procedure-associated infections, enhanced hand hygiene and environmental cleaning, admission screening with nasal swabs, and targeted ICU chlorhexidine-based decolonization practices. Reference Popovich, Aureden, Ham, Harris, Hessels and Huang26,Reference Lee, Bartsch, Wong, McKinnell, Cui and Cao27 However, most of these efforts have primarily focused on MRSA in hospital settings. Therefore, new guidance may be needed for high-risk outpatients, such as those with peripherally inserted central catheters, ports, pacemakers, implantable cardioverter-defibrillators, hemodialysis catheters, and prosthetic joint replacement. Reference Souli, Ruffin, Choi, Park, Gao and Lent28,Reference Rha, See, Dunham, Kutty, Moccia and Apata29 Additionally, the ongoing opioid epidemic is likely contributing to the increased CO staph bacteremia. Reference Quagliarello, Cespedes, Miller, Toro, Vavagiakis, Klein and Lowy30 Although a recent study revealed that post-discharge MRSA decolonization with chlorhexidine and mupirocin led to a 30% lower risk of MRSA infection than education alone, Reference Huang, Singh, McKinnell, Park, Gombosev and Eells31 there is currently no widely implemented approach for S. aureus carriers in outpatient settings, except for the recommendation of peri-operative decolonization and decolonization for individuals with recurrent staph infections. Reference Bebko, Green and Awad32
While the in-hospital mortality rate among those with staph bacteremia is high compared to controls, it is important to note that other delineations of bacteremia also exhibit disproportionate costs, LOS, and mortality outcomes. Reference Yu, Jung and Characteristics33,Reference Diekema, Hsueh, Mendes, Pfaller, Rolston, Sader and Jones34 Notably, mortality was higher in HO bacteremia, reaching 24.1% for MRSA and 19.8% for MSSA compared to CO bacteremia. Our study confirmed that the incidence of HO staph bacteremia did not continuously decrease. A recent study across 123 Veterans Affairs (VA) healthcare systems, examining all hospital-acquired infections due to MRSA (including HO MRSA bacteremia), also indicated an increased incidence of MRSA infection. Reference Evans, Simbartl, McCauley, Flarida, Jones and Harris35 Consequently, HO staph bacteremia should remain a focus for public agencies, necessitating ongoing active surveillance and mitigation efforts.
This study has several limitations. First, we only used the results of the first blood culture to classify CO vs. HO bacteremia. Some patients developed HO bacteremia after being admitted with CO bacteremia but were categorized as having CO bacteremia in the present study. This could potentially lead to misclassification bias and an underestimation of HO bacteremia. However, only 1.1% of our cohort had subsequent positive cultures. Second, the necessary data for the retrospective cohort study were not available for all patients across 267 hospitals, so we used a subset of data from 41 hospitals, which could potentially introduce selection bias. Additionally, results may not be generalizable to the entire US population. Third, as is the case with any research relying on administrative data, we had to depend on the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) coding for identifying six clinical diagnoses. Therefore, local coding practices could influence the accuracy of diagnostic coding, and bias cannot be ruled out. However, we used microbiological data to identify the population with true staph bacteremia. Fourth, the presence of orthopedic or cardiac prosthetic devices in the context of staph bacteremia increases the risk of relapsed infection. Although we included patients who presented with infections involving prosthetic devices, whether those devices were removed during treatment could not be determined. Moreover, we did not have access to information on the antibiotics used for treating staph bacteremia or whether source control was achieved when the source was identified. Fifth, due to the nonrandomized nature of the study, residual confounding in the outcome analyses cannot be ruled out. Sixth, we did not investigate which staph bacteremia was associated with intravenous drug use. Seventh, we did not have information regarding the infection control measures (e.g., contact precautions, admission screening) implemented by each hospital. Last, it is important to note that our study did not cover the period when the COVID-19 pandemic emerged in the United States, and trends might have changed in 2020.
In conclusion, the incidence of CO MSSA and CO MRSA increased between 2015 and 2020 across 267 acute-care hospitals in the United States, while HO MSSA and MRSA remained stable. In comparison to those without staph bacteremia, LOS, mortality, and total cost were higher in individuals with staph bacteremia, irrespective of methicillin susceptibility or onset location. In light of a potential HOB metric as proposed by the CDC, antibiograms produced at the hospital level may want to consider demarcating CO and HO resistance trends given that empirical and pre-op prophylaxis antimicrobial choices by clinicians and antimicrobial stewardship teams are often predicated on antibiogram information. Irrespective of a mandatory reporting requirement, the outcomes we describe may warrant further studies on the merits of tracking trends of both MRSA and MSSA and how to operationalize locally relevant resistance patterns into antimicrobial stewardship and infection prevention workflows.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ash.2024.402
Acknowledgment
None.
Financial support
None.
Competing interests
No disclosure; KY, MJ, CI are employees of Becton Dickinson and Company, a medical technology company.






