Penfield, the Royal Victoria Hospital, and the MNI
Wilder Penfield was born in Spokane, Washington in 1891. Reference Penfield1,Reference Feindel and Leblanc2 He matriculated at Princeton University and graduated in medicine from Johns Hopkins Medical College. Penfield was awarded a Rhodes Scholarship while at Princeton, which he took with Charles Sherrington at Oxford University. From this experience, Penfield learned the functionings of a Nobel caliber laboratory. In furtherance of his aspirations towards integrating basic research and neurosurgery, Penfield went to Madrid in 1924 to learn the silver and gold methods of staining neurons and glia from Pío del Río Hórtega. As Penfield mastered the intricacies of the metallic staining techniques, he and Río Hortega discovered that post-traumatic cortical scars are composed of reactive astrocytes, collagen fibrils, and a meshwork of newly created blood vessels that anastomose with the arteries of the surrounding cortex. Reference del Río Hortega P. Penfield3,Reference Leblanc4 Penfield thought that as the cortical scar contracted, it exerted traction on the surrounding arteries. This, in turn, caused focal vasoconstriction and ischemia, and triggered an epileptic seizure. Reference Leblanc5 The investigation of this hypothesis by Penfield and his research fellows set the surgical treatment of epilepsy on solid ground and shed light on the pathophysiology of the epileptogenic focus, the spread of epileptic seizures, and the role of the collateral circulation in cerebral ischemia. It introduced a generation of neurosurgeons to experimental neurosurgery, who then contributed to the emergence of neuroscience following the Second World War.
The Department of Neurology and Neurosurgery
Penfield was recruited to head McGill University’s Sub-department of Neurosurgery at the Royal Victoria Hospital (RVH) in 1928. Reference Leblanc6 An autonomous Department of Neurology and Neurosurgery was created at McGill in 1930, which relocated to the newly built MNI in 1934 (Figure 1). Reference Penfield7 The departmental structure allowed Penfield to set his own academic priorities and recruit according to those needs, independently of the Departments of Medicine and Surgery, while generous endowments shielded the MNI from austerity measures during the Great Depression.

Figure 1: Left. Penfield’s sketch of the Montreal Neurological Institute. The sketch is only an approximation of the final structure. Neurological offices and clinics were located on the first floor. The neurosurgical offices and examining rooms were on the fifth floor, in proximity to the two operating rooms. A covered bridge (RVH) spanned University Street to connect the MNI to the RVH. The sketch was not drawn by Penfield in New York City as the Biltmore Hotel letterhead would seem to indicate. Rather, it was drawn in Montreal using paper from the hotel that Penfield had at hand. Courtesy of the Osler Library of the History of Medicine, McGill University. Right. Aerial view of the Montreal Neurological Institute. The photograph was taken in 1934 and is included in the MNI’s Foundation Volume. Reference Penfield7 Montreal Neurological Institute Archives. All rights reserved.
The MNI’s faculty held full-time university appointments and had their offices, clinics, and laboratories within the Institute. This assured, Penfield wrote, “that those who are granted consulting rooms within the clinic shall place clinical research above the desire for private practice.” Reference Penfield7 The neurosurgical staff of the MNI consisted of Wilder Penfield, Chair of the Department and Director of the Institute, Penfield’s collaborator William Cone, Neurosurgeon-in-Chief and Head of clinical and experimental Neuropathology, and Arthur Elvidge, who had trained with Penfield and Cone. Reference Preul, Stratford, Bertrand and Feindel8,Reference Preul, Feindel, Dagi, Stratford and Bertrand9 They were joined by Collin Russel, Neurologist-in-Chief, Donald McEachern, neurologist and head of neurochemistry, Herbert Jasper in clinical electroencephalography and neurophysiology, Molly Harrower and Donald Hebb in neuropsychology, and Francis McNaughton, neurologist and head of neuroanatomy. Admission to the neurosurgical training program was predicated on an applicant’s willingness and ability to perform independent research in one of these laboratories. The requirement for research assured that all those who applied foresaw a future academic career (Table 1).
Table 1: North American trainees at the Montreal Neurological Institute 1934–1945

* AANS: American Association of Neurological Surgeons.
† ABNS: American Board of Neurological Surgery.
‡ WNS: Western neurosurgical Society.
The Montreal Neurological Institute
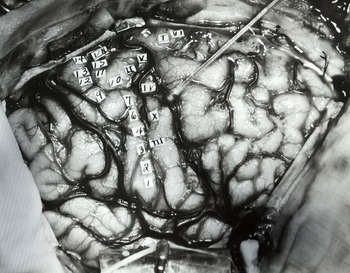
The MNI had two operating rooms. The bigger one had a glass-enclosed viewing gallery and a specially designed system for intraoperative photography (Figure 2). Pneumoencephalograms, ventriculograms, and angiograms Reference Elvidge10 were performed in the smaller one. Clinicians and the clinical facilities were proximate to the research laboratories, allowing easy interaction between clinicians and basic scientists. Thus, by its very physical structure, Reference Feindel and Leblanc2,Reference Adams11 the MNI was created to assure that neurosurgery would contribute to the emerging field of neuroscience. Penfield’s vison of research-based neurosurgical training attracted many like-minded individuals who would go on to advance academic neurosurgery in North America.

Figure 2: Photograph of the first operation performed at the Montreal Neurological Institute. The surgeon is Theodore Erickson. He is assisted by Donald Coburn. The scrub nurse is Cora McLeod. David Reeves is observing in the glass-enclosed gallery. A mirror attached to a movable boom is visible in upper left. The photographer was in a cubby under the gallery floor and could move the mirror automatically to reflect the operative field. The photographer then aimed his camera at the mirror to capture an image of the exposed cortex. Montreal Neurological Institute archives. All rights reserved.
Residency began with three 6-month rotations in neurology, neurosurgery, and the trauma service. This was followed by research in one of the MNI’s laboratories. Research fellows were encouraged to work towards a graduate degree. The completion of a research fellowship was a prerequisite to the final 2 years of training as a neurosurgical resident. Research by the first MNI fellows was directed toward the further characterization of the cortical scar that del Río Hórtega and Penfield had demonstrated in Madrid. This led to the discovery of the ischemic penumbra and of the epileptogenic zone, the importance of the corpus callosum in the spread of epileptic seizures, the pathological effects of cerebral vasospasm, and of the structure-function relationship of the brain.
The Cortical Scar and the Ischemic Penumbra
Joseph Evans was Penfield and Cone’s first resident and their third research fellow, after Ottiwell Jones from the University of California at San Francisco (UCSF), and Dorothy Russell from the London Hospital, United Kingdom. Evans accompanied Penfield and Cone from the RVH to the MNI at its opening and remained there until 1937 (Figure 3). He was immediately tasked with the study of post-traumatic epilepsy and its surgical treatment, for which he was awarded a MSc from McGill University. Reference Evans12 Evansʼ experiment consisted of producing cortical scars in one group of animals and uncomplicated surgical excisions of cortical tissue in another. Both groups were submitted to drugs known to produce epileptic seizures after sufficient time had passed to allow the maturation of the scars and cortical incisions. From the results of these experiments, Evans concluded “There can be no doubt that brain scars reduce the convulsant threshold, nor can there be doubt that surgically correct removal of cerebral tissue does not result in a lowering of the threshold.” Reference Evans12 These experiments led Evans to investigate the cortical scar’s role in a putative vascular reflex mechanism in focal epilepsy. To do so, he studied the effects of middle cerebral artery occlusion on the collateral circulation in the border zone between infarcted tissue and normal cortex. Reference Evans13,Reference Evans and McEachern14 He discovered that what we now refer to as the ischemic penumbra is a dynamic area in which the effects of ischemia can be mitigated by increased collateral flow. Working with Donald McEachern, Evans suggested that a therapeutic effect in cerebral ischemia could be achieved by “increasing the availability of the oxygen supply by a) heightening the oxygen content of the blood, b) by increasing the rate of oxygen dissociation, or c) by opening up more rapidly and perhaps to a greater degree, the available collateral channels.” Reference Evans and McEachern14 The latter, he suggested, could be achieved by mitigating the effects of cerebral edema on perfusion in the border zone “by the use of salt and glucose solutions and perhaps by lyophile sera,” and by performing a decompressive craniectomy. More than three decades would elapse before the penumbra was recognized as a therapeutic target in stroke and that a large craniectomy could mitigate its effects. Nonetheless, Evans had immediately applicable advice for his neurosurgical colleagues, as he highlighted “the extreme importance in surgical procedures of treating blood vessels, large and small, with the utmost respect.” Reference Evans13

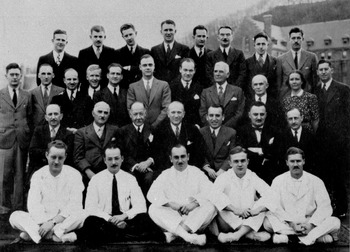
Figure 3: MNI group photo, 1936. Font row: starting at second from the left are Edwin Boldrey, Donald Reeves, Robert Pudenz, and Isadore Tarlov. Second row: Wilder Penfield (fourth), William Cone (fifth). Third row: Exum Walker (first), Joseph Evans (second), Arthur Elvidge (third). Top row: Theodore Erickson (third). Montreal Neurological Institute archives. All rights reserved.
Evans’ studies led to a doctoral degree, but that was not the limit of his research, as he learned the power of the clinicopathological method. With Penfield, he published a paper Reference Penfield and Evans15 on the cognitive effects – most notably apathy and lack of initiative – of large frontal resections in humans, that is considered a milestone in neurophysiology, observations that Donald Hebb later elaborated upon. This led Hebb to comment during his Hughlings Jackson Lecture at the MNI, “I must publicly record my indebtedness to the Fellows of 1937 and 1938, who, having found someone who knew less than they did, proceeded to take my education vigorously in hand.”
Joseph Evans left the MNI in 1937 for the University of Cincinnati, where he established a working relationship with Frank Mayfield at Cincinnati’s Good Samaritan Hospital. Although Mayfield had no university appointment, Evans invited him to join in founding that University’s first neurosurgery training program. 16
The Epileptogenic Zone
A vascular reflex requires the participation of perivascular nerves, and this was the subject of Storer Humphreysʼ thesis. Humphreys came to the MNI in 1937 and studied the innervation of blood vessels of normal cortex and those of the epileptic focus. He observed that, compared to normal cortex, perivascular nerves appeared to be more numerous and arranged in what appeared to be plexuses in the epileptic focus and its border zone. Given this arrangement, Humphreys concluded “that a mechanism has anatomically been demonstrated to justify the possibility of vasospastic elements in the epileptic seizure.” Reference Humphreys17 Furthermore, the cytological changes observed in the border zone were compatible with hypoxemia, which Humphreys equated with the abnormal innervation of its blood vessels. He concluded from these observations that there is a cytologically and vascularly defined zone between an epileptogenic lesion and the normal cortex surrounding it, and that, although the lesion itself is electrographically silent, “the edge of the lesion gives rise at times to spikes and often to delta waves…. [this zone is] active in the sense of continuing to produce periodic seizures…. [T]he border zone between normal and abnormal tissue is the nidus of the epileptic attack.” This was the first description of what was later referred to as the epileptogenic zone.
Humphreys had discovered that regardless of the etiology of the epileptic lesions, all had similar vascular and cytologic changes within the epileptogenic zone. Reference Penfield and Humphreys18 Humphreysʼ thesis is also noteworthy for its description of microgyria, which is now recognized as a common cause of focal epileptic seizures. Reference Leblanc19
William Bridgers, who came to the MNI in 1940, further characterized changes in the epileptogenic zone as consisting of “circumscribed foci of neuronal destruction … [u]sually accompanying these foci were glial nuclei which were increased in number compared to those in the surrounding cortex.” Reference Bridger20 Walther Spielmeyer had previously described neuronal loss and gliosis in the hippocampi and cerebellums of persons suffering from chronic epileptic seizures, which he ascribed to chronic ischemia. Similarly, Bridgers proposed that the changes that he had observed were in keeping with Penfield’s hypothesis that local cortical ischemia plays a role in initiating or propagating epileptic seizures. Reference Leblanc5 Penfield later discovered that hippocampal neuronal loss and gliosis, a pathophysiological process to which he referred as incisural sclerosis, is the substrate of psychomotor epilepsy. Reference Leblanc4
Cerebral Vasospasm
Francis Echlin was born in Ottawa, Canada, and graduated from McGill Medical School in 1931. He then studied at the College de France in Paris and the Physiological Laboratory of Cambridge University, coming to the MNI in 1937 (Figure 4) where he investigated cerebral vasospasm and cortical ischemia in the context of epileptogenesis. Reference Echlin21,Reference Echlin22 Echlin exposed the cerebral hemispheres in cats and induced vasospasm by mechanically stimulating arteries along a gyrus, while an assistant injected gentian violet intravenously. Echlin observed that “the brain rapidly turned a deep blue except in the area where the blood vessels had been constricted. This area remained white. Coronal sections of the brain showed that ischemia had been almost complete through the entire depth of the cortex in a large portion of the area stimulated.” Echlin thus demonstrated that prolonged vasospasm results in cerebral infarction, an observation that was not appreciated until vasospasm following subarachnoid hemorrhage was recognized as a significant cause of disability and death in the early 1950s. Reference Ecker and Riemenschneider23

Figure 4: Group photograph of the MNI, 1937. The house staff are in white. The attending staff and research fellows are in day suits. Front row: Robert Pudenz (fourth). Second row: Wilder Penfield (fourth), William Cone (fifth). Third row: Donald Hebb (fourth). Molly Harrower (tenth), Arthur Elvidge (eleventh). Top row: Guy Odom (first), Edwin Boldrey (second). Theodore Erickson (fourth), Storer Humphreys (seventh), Francis Echlin (eighth). Montreal Neurological Institute archives. All rights reserved.
Echlin left the MNI for the Bellevue and Lenox Hill Hospitals of New York University in 1939, where he joined former MNI fellows Thomas Hoen and Isadore Tarlov, Reference Feindel and Leblanc2,Reference Leblanc6 and where he developed experimental models of acute and chronic cerebral vasospasm. Reference Echlin24,Reference Echlin25 His models gave great impetus to the experimental study of cerebral vasospasm, most notably by his fellow MNI alumni Guy Odom (Duke University), Eric Peterson and Richard Leblanc (University of Ottawa and MNI), and Bryce Weir (Universities of Alberta and Chicago). Reference Feindel and Leblanc2
The Structure-Function Relationship of the Brain
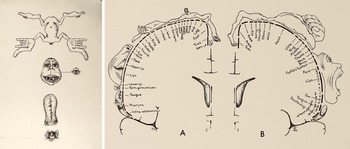
Edwin Boldrey came to the MNI in 1936 after his internship and residency in surgery at the Montreal General Hospital. He was exposed to neurosurgery through Arthur Elvidge, who was the neurosurgical consultant there, and met Penfield when he attended meetings of the Montreal Neurological Society. Although he had been offered a neurosurgical residency with Percival Bailey at the University of Chicago, Boldrey decided to train with Penfield at the MNI, a decision of momentous importance to neurobiology, as Boldrey produced what is perhaps the most influential thesis to have originated at the MNI. Entitled “A Report of Electrical Stimulation of 105 Human Cerebral Cortices,” Reference Boldrey26 it details the points from which responses were obtained during the electrocortical stimulation of the cortex (Figure 5). Each stimulation point, representing a specific function such as sensation or movement of the face and limbs, was transcribed onto a brain map. Penfield and Boldrey published these maps, in which the first version of the homunculus appeared, in Brain in 1937 Reference Penfield and Boldrey27–Reference Leblanc and Preul29 (Figure 6). A more elegant homunculus, looking effortlessly draped across the hemispheres of the brain, achieved iconic status with the publication of Penfield and Rasmussen’s Cerebral Cortex of Man. Reference Penfield and Rasmussen30 Boldrey later joined Howard Naffziger and Ottiwell Jones, Penfield’s first research fellow, Reference Feindel and Leblanc2 at UCSF, where he studied cerebrovascular disease and brain tumors.

Figure 5: Operative photograph of case FS, operated upon in 1935, and included in Boldrey’s 1936 thesis and in Penfield and Boldrey’s 1937 Brain paper. The patient had right hemisphere focal motor seizures beginning with turning of the head and eyes to the left and involving the left leg. The right hemisphere is exposed. Arabic numerals indicate areas where sensory responses were produced by electrocortical stimulation, and Roman numerals reflect motor responses. Penfield observed that the region immediately in front of the precentral gyrus superiorly was indurated and atrophic. The operation was performed before electrocorticography was available. Stimulation at “I” produced motion of the foot as in an attack and stimulation at “V” produced what the patient felt in the left leg during an attack. Stimulation at “X (pointer)” adjacent to the frontal eye field, produced what Penfield described in his operative note as “a slight convulsive seizure consisting of clonic movements of conjugate deviation of the eyes.” Penfield resected “an area of brain about 5 cms. in length and from 3–4 cm. in width situated immediately in front of the precentral gyrus and extending down the falx to a depth of about 3–4 cm. along the falx.” Histopathological examination revealed a cerebral cicatrix. Montreal Neurological Institute archives. All rights reserved.

Figure 6: Left. The 1937 homunculus does not distinguish sensory from motor functions. It illustrates the responses obtained from what was widely referred to at the time as the sensorimotor region, comprised of the ascending frontal and parietal gyri. The anatomical orientation is from the Sylvian fissure inferiorly to the interhemispheric fissure superiorly. The figurine is represented in four detached segments. The size of each segment represents the relative cortical representation of the area represented. The lower segment represents the nasopharynx and uvula. The second segment represents movements of the tongue, in which the base is inferior and the tip superior. The representation of the face is not inverted, as are the other aspects of the figurine. The areas devoted to the opposable thumbs, necessary for grasping tools, and to the tongue and lips, necessary for speech, are disproportionally large, as befits their importance in human evolution. Right. The 1950 sensory (A) and motor (B) homunculi. Courtesy of the Osler Library of the History of Medicine, McGill University.
Cortical Transection and Callosotomy
Theodore Charles Erickson had trained in neurosurgery with Charles Frazier and Francis Grant at the University of Pennsylvania before coming to the MNI in 1933, where he studied the spread of epileptic seizures in animals. Reference Erickson31 Erickson caused a focal motor seizure after identifying the precentral gyrus by electrocortical stimulation, and, using electrocorticography, he followed the epileptic activity as it marched along the motor strip. Erickson observed that transection of the precentral gyrus distal to the epileptic focus arrested the spread of the seizure, and that sectioning the corpus callosum prevented the seizure from spreading to the opposite hemisphere. From these experiments, he concluded that, “my observations on the spread of the epileptic discharge from one cerebral hemisphere to the other prove definitely that this spread occurs largely or entirely via the corpus callosum.” Erickson presented his results to the Montreal Neurological Society in December 1938 and to the American Psychiatric Association in May 1939. They were published in March 1940. Reference Erickson32 Van Wagenen and Herren published their experience with callosotomy for the treatment of epileptic seizures in October 1940, Reference Van Wagenen and Herren33 but their paper is devoid of references, so whether they knew of Erickson’s work remains an open question. However, as Joseph Vogel concluded, “One might assume that Erickson’s animal experiments at the Montreal Neurological Institute were known to Van Wagenen since the neuroscience community was quite small in those days.” Reference Bogen, Reeves and Roberts34
Erickson devoted much of his time at the MNI to writing Epilepsy and Cerebral Localization with Wilder Penfield, Reference Penfield and Erickson35 the most comprehensive work on the investigation and treatment of epilepsy and cortical localization published in the first half of the 20th century. The book is also noteworthy for a section on the psychological evaluation of persons with epilepsy by Molly Harrower, who preceded Brenda Milner as Head of Neuropsychology at the MNI. Erickson left the MNI for the University of Wisconsin in 1941, where he recruited Clinton Woolsey, the noted neurophysiologist. Erickson and Woolsey subsequently made significant contributions to the understanding of the detailed somatotopic relationship of the pre- and post-central gyri, the supplementary motor area, and the second sensory region.
Wartime Research
Canada’s entry into the Second World War in September 1939 had a profound effect on research activities at the MNI. Reference Feindel and Leblanc2 Rather than pursuing graduate degrees, the residents and fellows engaged in war research, to which the MNI could apply a critical mass of talent and resources. Reference Penfield36
Two research fellows stand out: William Feindel and Robert Pudenz.
William Feindel, like Penfield a Rhodes Scholar, was born in Bridgewater, Nova Scotia, and came to McGill in 1942. While still a medical student, he was introduced to Miguel Prados who had worked with del Río Hortega in Madrid and to whom Penfield had given refuge from the Spanish Civil War. Prados, Strowger, and Feindel were the first to show the therapeutic effect of corticosteroids on experimentally induced cerebral edema. Reference Prados M.Strowger and Feindel37,Reference Prados M.Strowger and Feindel38 Feindel later founded the Department of Neurosciences at the University of Saskatoon, Canada, but returned to the MNI in 1959 as Full Professor of Neurology and Neurosurgery. He was appointed the MNI’s third Director in 1972. Reference Feindel and Leblanc2
Other Canadian residents and fellows were engaged in war-related research, including Claude Bertrand, who came to the Institute in 1941 and studied nerve repair with Herbert Jasper. Also a Rhodes Scholar–he was at Oxford with Feindel–he was subsequently appointed Professor and Head of Neurosurgery at the University of Montreal where he studied the physiology of the thalamus with Herbert Jasper. He achieved international recognition for his work in functional and stereotactic neurosurgery. Eric Peterson, who came to the MNI from McGill, worked on high-altitude air evacuation with Jasper, Cone, and Murray Bornstein Reference Jasper, Peterson and Bornstein39,Reference Peterson, Kent and Cone40 (Figure 7). Bornstein became a prominent neuroscientist specializing in demyelinating diseases.

Figure 7: MNI. War time researchers. Herbert Jasper, Canadian Army, Robert Pudenz, United States Navy, and Eric Peterson, Royal Canadian Air Force, in uniform during World War Two. Montreal Neurological Institute archives. All rights reserved.
American residents and fellows also contributed to the Canadian war effort before the United States entered the war in December 1941. Chief among them was Robert Pudenz, who came to the MNI in 1936. Pudenz studied the use of thrombin as an anticoagulant in neurosurgical procedures, the role of sulfonamides in the treatment of head wounds and meningitis, and the use of biological tissues and artificial membranes as potential dural substitutes. Reference Pudenz41 Most noteworthy, however, was his development of the tantalum plate, which became the standard material for cranioplasty. Reference Pudenz42
Pudenz devised the first valved shunt system for hydrocephalus, Reference Pudenz, Russell, Hurd and Shelden43 a condition that Penfield had encouraged him to study: “During my residency training in Montreal,” he wrote, “one of my teachers, Wilder Penfield, remarked that any neurosurgeon ‘worth his salt’ would, at some time in his career, confront the problems of hydrocephalus and seek better methods of medical and surgical management.” Reference Pudenz44 Penfield undoubtedly had Arne Torkildsen in mind when he said this. Torkildsen, one of Penfield’s early research fellows, studied the anatomy of the ventricular subsystem while at the MNI, and later developed the revolutionary ventriculo-cisternal shunt (Torkildsen’s shunt), Reference Leblanc4 which Penfield routinely performed during Pudenz’s residency. Reference Penfield45
Theodor Rasmussen and Edgar Lotspeich studied blackout in pilots. After a period as Head of Neurosurgery at the University of Chicago following the war, Rasmussen returned to the MNI and succeeded Penfield as its Director in 1960. Reference Feindel46 Lotspeich and Frank Mayfield established a joint neurosurgical practice in 1947, a precursor to the Mayfield Clinic. Guy Odom worked with Pudenz on biological and artificial membranes as dural substitutes. Odom founded the neurosurgical training program at Duke University, similar in structure and emphasis to the MNI’s, Reference Odom47 where he continued Echlin’s work on vasospasm.
The Resident’s Life
Like Edwin Boldrey, Arthur Ward had initially applied to train in neurosurgery with Percival Bailey at the University of Illinois, but, to his surprise, Bailey told him, “I suggest that you go up to Montreal with my friend Wilder Penfield. In fact, I called him up and I think that you should apply to him, and you will be accepted.” Reference Ojemann48 (Figure 8). Ward had studied neurophysiology at Yale before coming to the MNI, so his time at the Institute was mostly on the clinical service, of which he left a vivid account:

Figure 8: Bailey and Ward at the MNI. Percival Bailey (sitting, fourth from left) gave the Ninth Hughlings Jackson Lecture on the “Cortical Organization of the Chimpanzee’s Brain” at the MNI on 22 May 1944. Front row, sitting left to right: A Ward, ES Lotspeich, Penfield, Bailey, K Stern, EW Peterson, A Eldvidge. Standing in the second row are F McNaughton (Neurologist-in-chief, MNI), W Hall, WH Bridgers, unidentified, unidentified, W Pepper, TS Bennett. In the back are GK Morton, W Feindel, unidentified, P Robb (later Neurologist-in-chief, MNI), and C Bertrand. Montreal Neurological Institute archives. All rights reserved.
Well, as chief resident, the day started at usually about quarter to seven or six thirty in the morning, when the night supervisor … would call the chief resident and essentially give him a verbal, make verbal rounds with him, on every patient in the house in both neurology and neurosurgery. Then after that I would rush down to one of the wards where they would bring a tray of breakfast to me on the ward, and I would have my breakfast and then rush off to the operating room. Weʼd spend at least the whole morning [there and] a fair amount of the afternoon. And then in the afternoon, there were diagnostic procedures to be done … some clinics … and then in the evenings there was rounds, dressings, and I guess the day usually ended up about, well if we were lucky, by one oʼclock in the morning, occasionally a little later than that if there was surgery or something going. Reference Ojemann48
Arthur Ward founded the Department of Neurosurgery at the University of Washington and structured its residency program to incorporate basic research, most notably in electrophysiology and epilepsy surgery. Just as importantly, “Arthur learned from Penfield the importance of always remaining a gentleman, even in the most trying circumstances.” Reference Ojeman49
Neurosurgery in North America 1934–1945
Edward Archibald, who had been performing neurosurgery at McGill University since 1906, and who was a founding member of the Society of Neurological Surgeons, had great insight into the state of neurosurgery in North America. Reference Zehri, Belykh, Zhao, Leblanc and Preul50 He wrote Penfield in August 1927, as he was attempting to recruit him to McGill:
I am quite determined that you shall come here. If you do I expect that ten years from now the Hub of surgical neurology, in this continent, will be transferred from Boston to Montreal. There is nobody in Boston who can fill Cushing’s shoes, and I shall expect at the very least that for the eastern half of the continent you will dispute the honors of the game with [Walter] Dandy [in Baltimore], with [Francis Clark] Grant [in Philadelphia] following as an indifferent third. Not one of them all, that I know of, is doing any fundamental work in histology, and scarcely anybody in physiology or experimental surgery. With your training along those lines, you will repeat Cushing’s career and do better than he did along the experimental line. Reference Feindel and Leblanc2
Archibald had been correct. A decade after his letter was penned, no other neurosurgical training program had departmental status, and all had to compete with other Divisions within a Department of Surgery for residency positions and resources. Most had only a single resident at a time, who trained in operative neurosurgery without exposure to research. This was the case at the University of Philadelphia under Charles Frazier and Francis Grant, at the Mayo Clinic under Alfred Adson, at the University of Southern California under Carl Rand, at Yale University under William German, and at UCSF under Howard Naffziger. The same was true for neurosurgery at the Peter Bent Brigham Hospital of Harvard University after Cushing’s retirement in 1932. Neurosurgery at the Massachusetts General Hospital didnʼt have a neurosurgical service until 1939. Ernest Sachs, at Washington University (St. Louis), trained only 20 neurosurgeons between 1921 and 1946. Johns Hopkins University didnʼt have a neurosurgery training program until 1941, and Dandy trained only eight neurosurgeons in his 28-year career there. Reference Sherman, Kretzer and Tamargo51 The New York Neurological Institute of Columbia University, under Charles Elsberg, Byron Stookey, and Tracy Putnam, was so plagued by internecine squabbles that it was irrelevant to neurosurgical research. Reference Solomon52 The same was true at the University of Toronto, where Kenneth McKenzie trained three residents from his arrival there as attending neurosurgeon in 1924 to the end of the Second World War, and with whom his relationships were so strained as to preclude civil discourse. Reference Morley53,Reference Weir54
The University of Chicago’s neurosurgery program under Percival Bailey warrants special mention. Bailey trained in neurosurgery with Harvey Cushing and remained at Harvard until he was recruited to the University of Chicago in 1928, the same year that Penfield came to McGill. Bailey had hoped to create a Department of Neuroscience in Chicago, as Penfield did in Montreal, but his efforts were thwarted by the governance of the University and Medical School, Reference Bucy55 a situation that was diametrically opposite to Penfield’s at McGill. Nonetheless, Bailey was able to train two of the last century’s most prominent academic neurosurgeons, Paul Bucy and Earl Walker. Dejected, Bailey left the University of Chicago in 1939 and was replaced, in succession, by MNI trainees Theodor Rasmussen, Joseph Evans, Sean Mullan, and Bryce Weir. Reference Feindel and Leblanc2
A Keynote Address
Harvey Cushing gave a keynote address during the MNI’s foundation ceremonies, in which he highlighted the significance of Penfield’s achievement, stating, “So we may well expect that under the widely trained and many-sided director of this new Institute neurology will receive a new impetus. Rest assured that here not only will the story of neurology’s great past be cherished but that a new significant chapter will be added to it.” Reference Penfield7 On that fall day in Montreal, Cushing foresaw the future of academic neurosurgery in North America.
Conflict of Interest
None.
Statement of Authorship
I am the sole author and responsible for all aspects of the manuscript.