Among the enzymes detected in the blood, the troponin complex is considered as the gold standard for detection of cardiac injury and measurements of troponin levels have become part of the diagnosis in clinical settings. Reference Neves, Henriques-Coelho, Leite-Moreira and Areias1
Cardiac troponins complex are proteins that are unique to cardiac muscle and are detected in the blood in cases of cardiac damage. Elevated levels of troponin may result from reversible membrane damage or from cell death. Reference Coudrey2–Reference Wu, Apple, Gibler, Jesse, Warshaw and Valdes4 In the adult population with coronary artery disease, elevations in cardiac troponin I have been shown to be an effective prognostic variable in patients with myocardial infarction and predicts adverse short- and long-term prognosis. Reference Antman, Tanasijevic and Thompson5–Reference Christenson and Christenson7
In cases of myocarditis and myopericarditis, the quantitative levels of troponin vary widely with some of the patients showing mild elevations while others have a more significant rise with a factor of hundreds to thousands of the normal level. Reference Smith, Ladenson, Mason and Jaffe8,Reference Soongswang, Durongpisitkul and Nana9 It seems logical that severe elevations in troponin levels reflect more extensive cardiac involvement that will be related to higher morbidity and mortality, although to date no clear correlation has been described between quantitative measurements of troponin levels to disease course or prognosis. Moreover, studies that addressed this issue found contradicting results. Reference Al-Biltagi, Issa, Hagar, Abdel-Hafez and Aziz10–Reference Freixa, Sionis and Castel13
The aim of this study is to examine the correlation between quantitative levels of troponin I in children diagnosed with myocarditis and myopericarditis to indirect measures of severity as hospitalisation course, treatment during hospitalisation, recommendation at release from hospitalisation and to mortality.
Methods
Troponin I levels are routinely checked in our hospital for all patients with clinical signs of suspected myocarditis, myopericarditis and pericarditis since 2010. Troponin I is measured with a stat high sensitive troponin I kit, Arcitect system, using chemiluminescent microparticle immunoassay. Normal troponin I levels were defined as less than 0.028 ng/ml.
The study is a retrospective study, and all consecutive patients younger than age 30 years were admitted to Rambam Health Care Campus between 2010 and 2016 with the diagnosis of suspected acute myocarditis, myopericarditis and acute pericarditis. The study was approved by the local Helsinki committee.
Clinically suspected myocarditis was diagnosed by clinical criteria of the 2013 ESC task force criteria Reference Caforio, Marcolongo, Basso and Iliceto14 : i.e., in the presence of ≥1 of the following clinical presentation in the absence of coronary artery disease or pre-existing cardiovascular disease: acute chest pain, new onset or worsening heart failure, palpitation and/or arrhythmia and/or syncope and/or aborted sudden cardiac death or cardiogenic shock along with ≥1 of the following diagnostic criteria: new onset ECG changes, elevated cardiac biomarkers, new functional or structural abnormalities on cardiac imaging, or classical findings on CMR. In asymptomatic patients, two or more diagnostic criteria were required. Pericarditis was diagnosed by the presence of two or more of the following criteria: pleuro-pericarditis chest pain, pericardial friction rub on cardiac examination, electrocardiogram changes, or pericardial effusion. Myopericarditis was diagnosed when criteria for pericarditis were met along with one additional feature: elevated cardiac biomarkers, presumed new left ventricular systolic dysfunction on echocardiography or cardiac MRI, and myocardial inflammation by cardiac MRI. Reference Imazio15
Electronic charts of 118 patients were reviewed for demographics data, troponin I levels at admission to the hospital, and peak troponin I levels during the hospitalisation period. Six patients were disqualified from the study due to other significant systemic or cardiac diagnosis or if diagnosis did not meet the criteria above. Other information recorded was survival, length of hospitalisation in the ICU and in the cardiac or paediatric ward, cardiac supportive therapy that included: extracorporeal membrane oxygenation support, intravenous inotropic or Milrinone support, diuretics, ace inhibitors, beta blockers, or other oral cardiac support drug and if there was a recommendation for cardiac therapy on discharge from the hospital. Information was recorded and correlation between troponin I levels and the above variables was examined.
The data were processed in SPSS version 21. Descriptive statistics in terms of averages, standard deviation, percentages, and ranges were performed for all variables in the study. Troponin I value were divided into groups that were correlated with the different variables: length of intensive care and overall hospitalisation, need for drugs or extracorporeal membrane oxygenation support, and mortality. Kolmogorov–Smirnov test was performed to examine the normal distribution of the quantitative variables. In accordance with this test, parametric or a-parametric tests was performed. A difference between the groups of troponin I in the quantitative values was performed in the ANOVA or Kruskal−Wallis test. The difference between the troponin I groups in the category indices was performed according to the Pearson chi square test. A paired test to examine enzyme values at admission and peak levels was performed according to the paired t-test. P < 0.05 was considered statistically significant.
Results
Ninety-three patients were diagnosed with myocarditis or perimyocarditis (46 and 47, respectively). Nineteen had no evidence of myocardial involvement and were diagnosed with pericarditis. Patient information is presented in Table 1.
Table 1. Patient information. CtnI-cardiac troponin I, ECMO- extracorporeal membrane oxygenation.

Most patients were male. Only five (5%) were younger than 10 years. This group of patients had lower median peak troponin I levels, compared to 34 patients age 10–20 years (0.47 ng/ml [0.11–24.2] and 9.9 ng/ml [2.8–14.2] respectively, p = 0.2) and to 54 patients older than 20 years (2.1 ng/ml [0.09–6.8], p = 1).
Admission and peak troponin I levels by different parameters for myocarditis and myopericarditis groups was examined and are presented in Figs 1 and 2, respectively.

Fig. 1 Median admission cTn-I levels in myocarditis patients by different parameters. IV - intravenous, P > 0.05 for all categories.
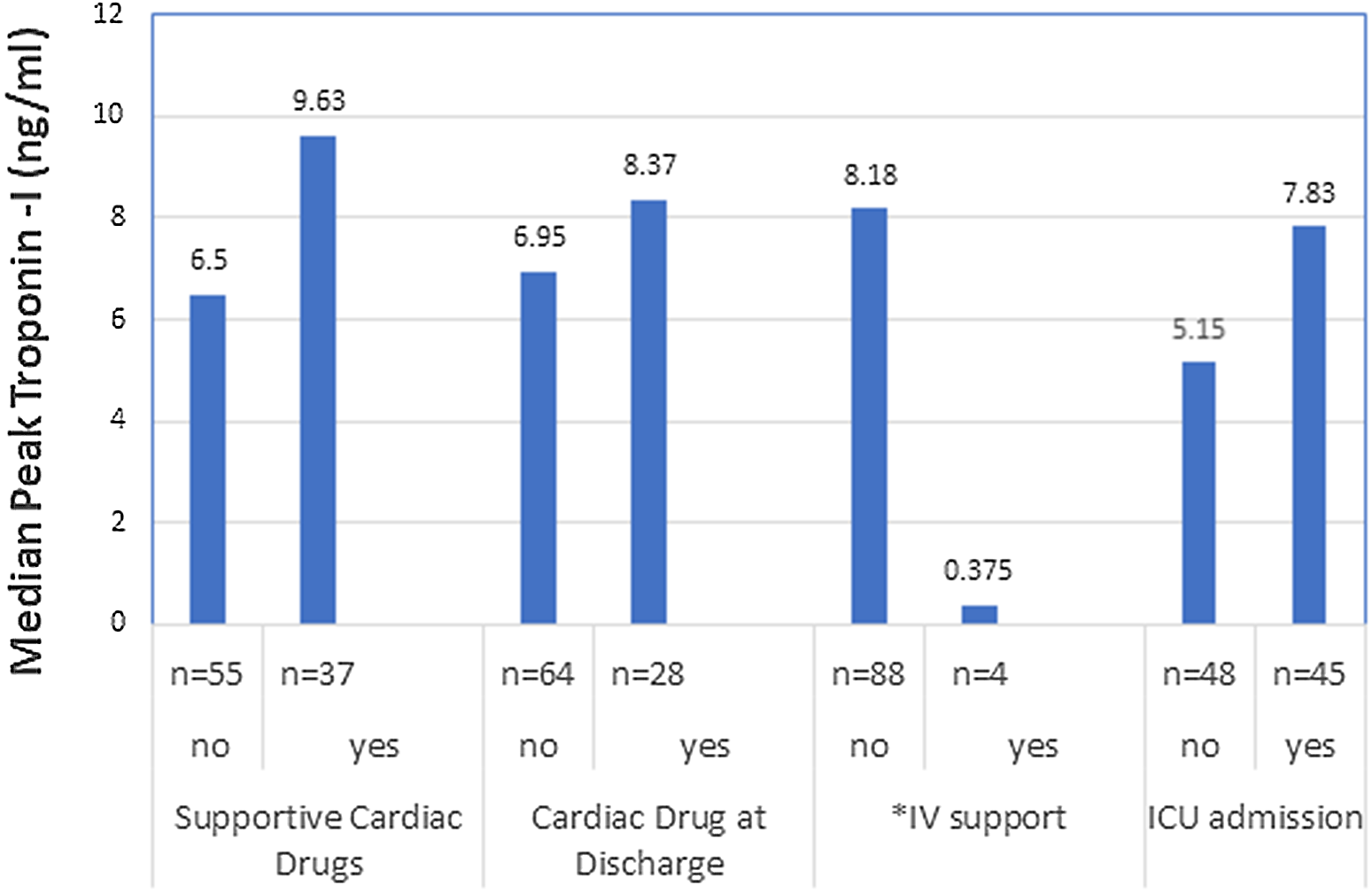
Fig. 2 Median peak cTn-I levels in myocarditis patients by different parameters. IV - intravenous, *P < 0.05
Two patients needed extracorporeal membrane oxygenation support, and one patient died. There was a large range distribution of troponin I values between these patients (0.244–44.471 ng/ml). The small number of patients precludes statistical analysis.
Higher troponin I levels at admission in patients with myocarditis and myopericarditis were correlated with overall longer hospitalisation duration (p = 0.026, Pearson correlation: r −0.23). There was a tendency for longer hospitalisation duration in the cardiac or paediatric wards with higher median troponin at admission (p = 0.056, Pearson correlation r = 0.2) and higher peak troponin I levels correlated with longer hospitalisation times in the cardiac or paediatric wards (p = 0.03, Pearson correlation r = 0.3). The correlations are not strong but significant.
A group of 11 patients with extreme elevations of troponin I levels to above >20 ng/ml was compared to the group that had lower than 20 ng/ml troponin I (n-82); results are presented in Table 2.
Table 2. Comparison between patients with troponin I levels above and below 20 ng/ml.

Discussion
We present a group of patients hospitalised in a single tertiary hospital with acute myocarditis, myopericarditis and pericarditis over a 7-year period. Most patients had evidence of myocardial involvement and were diagnosed with either myocarditis or myopericarditis.
A higher percentage of patients were male, a finding that correlates with other studies. Reference Al-Biltagi, Issa, Hagar, Abdel-Hafez and Aziz10 Additionally, most of our patients were older than 10 years of age, which is also consistent with the literature. Reference Neves, Henriques-Coelho, Leite-Moreira and Areias1
There was a statistically significant increase in average and median troponin I levels during hospitalisation in 52% of our patients, which was usually seen within a day of admission. This finding shows that many of the patients present while the disease is still active.
Patients that were admitted to ICU, received oral cardiac drugs, or were discharged with recommendation to take oral drugs had higher median troponin levels but this finding was not statistically significant, possibly due to the small sample group. Additionally, there were 11 patients with extreme elevations of troponin I to above 20 ng/ml, an elevation of >700 times the normal value. Of these patients, most were admitted to the ICU but compared to the rest of the patients with lower troponin levels, this group had similar characteristics and hospital course as patients with much lower peak troponin I values.
Results in the literature trying to relate troponin levels to morbidity and prognosis are inconsistent with contradicting results, and most studies constitute a small number of patients. Freiaxa et al. found that normal level or minimal elevation of troponin was associated with worse in-hospital and midterm prognosis. They suggested that patients with higher troponin levels are at an earlier stage of disease with more acute inflammation and better potential for recovery. Reference Freixa, Sionis and Castel13 Sachdeva found that an elevated initial and peak troponin >1 ng/ml was actually associated with a good outcome in paediatric myocarditis. Reference Sachdeva, Song, Dham, Heath and DeBiasi12 On the contrary, a study by Al-Bilagi et al. compared 25 children with fulminant myocarditis to 45 cases of acute myocarditis and found that significantly elevated troponin levels in patients with fulminant myocarditis were related to decreased survival and concluded that cardiac troponin levels can predict short-term prognosis. Reference Al-Biltagi, Issa, Hagar, Abdel-Hafez and Aziz10
In our series, two patients required extracorporeal membrane oxygenation support (2%) and one patient died (1%) which precludes statistical evaluation due to the small number of patients; however, these patients had a wide range of troponin levels comparable to other patients with a more benign course. A few studies in adults and children tried to identify factors associated with extracorporeal membrane oxygenation use and mortality in myocarditis patients. A study from Taiwan Reference Han-Ping, Mao-Jen, Wen-Chieh, Kang-His and Chun-Yu16 included 60 paediatric patients with acute myocarditis showed a tendency for patients with initial troponin levels above 14.2 ng/ml to require extracorporeal membrane oxygenation support (10 patients). A study from China Reference Duo, Ruo-Chi, Wen-Hui and Han-Bin17 included 403 adults diagnosed with myocarditis found that troponin T levels above 50 μg/l was an independent risk factor for mortality. Finally, Butto et al. Reference Buttu, Rossano and Nandi18 analysed data from paediatric health information for 149 paediatric patients with myocarditis. Abnormal troponin levels (I or T) in the first 72 hours was found to be associated with the use of extracorporeal membrane oxygenation but not with mortality.
We found that higher median troponin levels at admission correlated with longer overall hospitalisation and that median peak troponin correlated with longer hospitalisation at cardiac/pediatric ward. There was also a tendency for higher median troponin levels for patients admitted to ICU. These correlations may imply on disease severity, but the fact that the small number of patients that required intravenous cardiac drug support actually had significantly lower median peak troponin levels does not support this, and it seems more likely that high levels of troponin influenced doctors’ decisions regarding ICU admission and delaying discharge.
In summary, we found a correlation between troponin I quantitative levels and longer hospitalisations time. However, the correlation found in our dataset is not strong, and further studies are needed to verify this result. A small number of patients that required intravenous cardiac drug support were found to have lower median peak troponin levels, but we could not correlate quantitative levels of troponin I with other parameters related to the severity of disease.
Study limitations
Our study is limited by the small sample and in that it is a retrospective study with possible bias that may be present. Additionally, we have only reviewed the patient’s hospitalisation chart, and we do not know if they received a different diagnosis later on. Furthermore, due to our wide age range, our patients were treated both in the paediatric departments and ICU and cardiac ward and ICU, which may have different treatment protocols. As in other studies, the number of patients that required extracorporeal membrane oxygenation support or died was too small to draw conclusions.







