Minimally invasive cardiac surgery is practiced in the treatment of much of the cardiac pathology. These approaches have been developed to increase cosmetic gains without affecting clinical outcomes. Low mortality and morbidity in the repair of simple CHDs such as atrial septal defect, anomalous pulmonary venous return, and ventricular septal defect have made cosmetic gains also important in these operations. Reference Däbritz, Sachweh, Walter and Messmer1 Minimally invasive techniques, including total thoracoscopic approach, right anterolateral thoracotomy, and right vertical infraaxillary thoracotomy, are the main trends for atrial septal defect closure in order to avoid the characteristic long midline scar caused by the median sternotomy and to gain satisfactory cosmetic results. Reference Xu, Zhu, Wang, Huang and Zhao2
Right anterolateral thoracotomy has gained tremendous popularity over the past few years in patients with heart disease because of the combination of good aesthetic and functional results. Although the superiority of this approach in adult female patients is clear, some controversial data are currently present in the medical literature about the late results of this surgical approach in prepubertal girls, especially focusing on late breast development. Reference Vida, Tessari and Fabozzo3
Therefore, we examined the effects of anterolateral thoracotomy by our new approach to breast development in young female patients older than 8 years and under 14 years of age at the time of operation.
Materials and methods
200 patients underwent atrial septal defect repair through a median sternotomy and anterolateral thoracotomy between January 2010 and January 2018 at our institute. 114 of these patients are female. Atrial septal defect closure was performed in 55 female patients who were older than 8 years and younger than 14 years of age at the time of operation. Atrial septal defect repair was performed by anterolateral thoracotomy in 38 of the patients and by median sternotomy in 17 patients due to additional cardiac pathologies and based on surgeons’ decisions. Considering the fact that the thelarche for the female patients ranges between 9 and 13 years of age in population with an average age of 11–11.5, patient selection was made based on this criteria and particular attention was given to the patients for breast development between these ages. Reference De Silva4 Female patients aged 8–14 years who underwent atrial septal defect repair by thoracotomy or sternotomy were included in the study. Male patients, female patients younger than 8 years old, older than 14 years old, and patients who did not attend the outpatient clinic follow-up were excluded from the study.
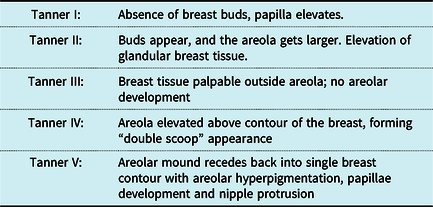
Patients who were operated between these dates categorised based on their ages and called for follow-up visits whom were 8–14 years of age at the time of the operation. These patients were called for routine post-operative follow-up visits on outpatient clinic at December 2020. During these visits, routine cardiac examination and breast examination were performed, complaints of patients were questioned, breast asymmetry were assessed, the sensory examination of the nipple and its surroundings were performed, also, pain and/or tenderness were evaluated by palpation, condition of the scar tissue, and the presence of keloid were evaluated prospectively. In addition, breast development of each patient examined was classified according to Tanner Breast Development Scale (Box 1).
Box 1. Tanner breast development scale
Three patients who underwent surgery by anterolateral thoracotomy excluded from the study since they did not show up for any follow-up visits.
In addition to that, breast sizes were evaluated subjectively by surgeons. Patients were referred to plastic surgery clinic in case in the presence of asymmetry between breast sizes.
During these controls, 52 patients conducted a subjective assessment of the operation with a 10-question questionnaire. This survey has been prepared by the authors in consideration of similar publications. Our questionnaire includes subjective evaluation of the appearance of scar tissue, the effect of scar tissue on patient psychology (lack of self-confidence, change in clothing selection, etc.), breast symmetry, and breast size.
The study protocol was approved by Ankara City Hospital Clinical Researches Ethics Committee (Ref No. E1-20-1409 Date:23/12/2020). A written informed consent was obtained from each patient/parent. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Breast development measurement techniques
The patients were examined as upper body naked. Measurements were made with the help of a ruler. In the first measurement, the measurement of the two nipples was made perpendicular to the nipple from the upper limit of the clavicle, and the symmetry of the nipples was evaluated. Breast size was evaluated by inspection, and patients were referred to the department of plastic surgery for further tests in case a notable difference in breast size was detected during the examination.
Surgical techniques
Anterolateral thoracotomy with the new approach was the surgical technique we used in patients. If we look at what is different from standard anterolateral thoracotomy, patients were placed on the operation table in the supine position with the right shoulder placed at a 45° angle. The skin incision was made at the sixth intercostal space in patients whose breast development has not yet started and in patients at Tanner 1–2–3 stage; and made 1 cm below the breast contour in patients at Tanner 4–5 stage. In other words, in patients whose breast development has not started, the skin incision is made approximately 2–3 cm lower than standard thoracotomy patients and the risk of damage to the breast tissue is reduced. In patients whose breast development has started, the incision is made 1 cm below breast groove, reducing the risk of damaging the breast tissue and keeping the scar tissue under the developing breast.
The incision was performed starting from the nipple level and making a 5–7 cm continuation towards the posterior. Tissues under the pectoralis major muscle were dissected as mammary gland tissue was not intervened. The thorax cavity was entered through the third or fourth intercostal space by the subpectoral method like standard anterolateral thoracotomy. In order to provide easier access to the heart relative to the diaphragm level, third or fourth costa excised from costochondral joint level. The skin incision length was 5 ± 1 cm in patients. The pericardium was opened 1–2 cm above the phrenic nerve while preserving the phrenic nerve and was fixed with sling sutures. A simple retraction suture was placed in the right atrial appendage and a better exposition was achieved for exposure of the ascending aorta. Arterial cannulation was performed with a straight-guided aortic cannula (arterial ecmo cannula). Single lumen venous cannula to the superior vena cava, L-shaped curved venous cannula was placed to the inferior vena cava (Pictures 1 and 2). Antegrade Del Nido cardioplegia (10cc / kg) was used in all patients. Atrial septal defect closure was performed via primer closure or patchplasty.Reference Tasoglu, Avci and Koca5 In study group, there was no patient who was converted to median sternotomy due to insufficient exposure, difficulty in central cannulation, etc. during the operation.
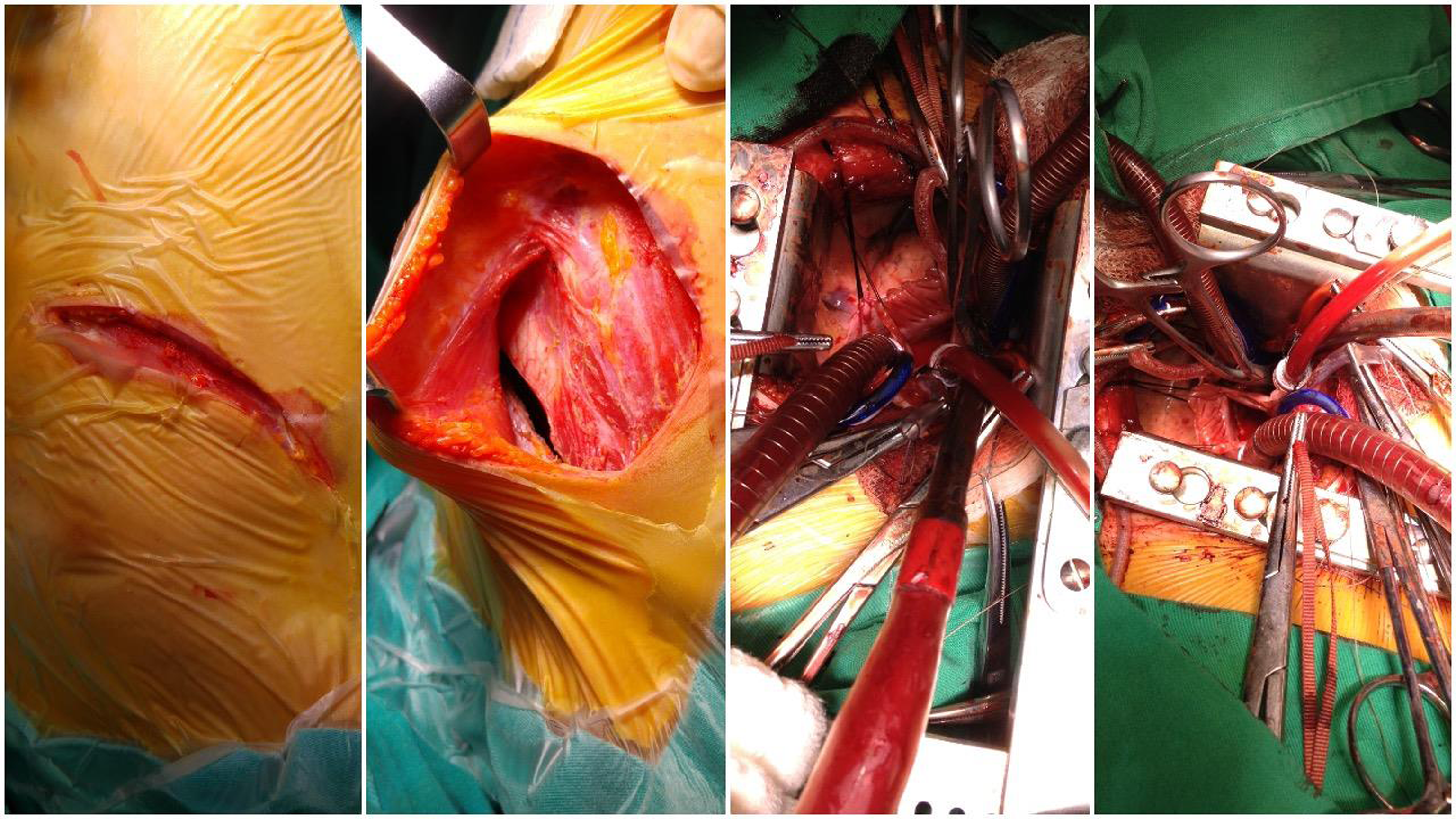
Picture 1 Intraoperative images of inframammarian incision, intercostal exposure with visible retraction, and bicaval cannulation of ASD closure (permission has been obtained from families).
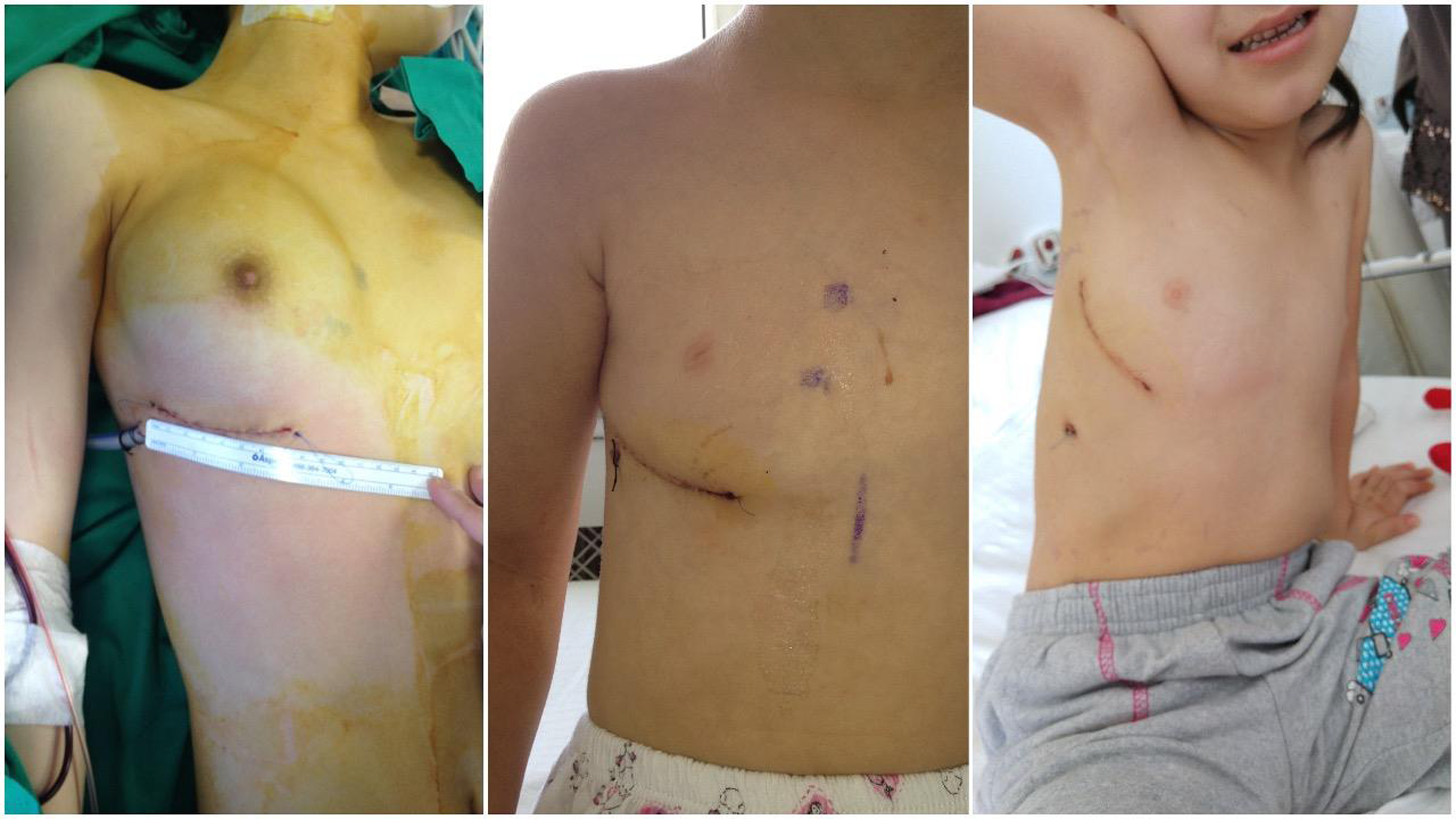
Picture 2 Post-operative photos of right anterolateral thoracotomy skin closure with pleasant cosmetic results (permission has been obtained from families).
The operation was performed via median sternotomy in the control group. Primer or patch closure of atrial septal defect and/or anomalous pulmonary venous return repair was performed through aorto-bicaval cannulation with antegrade Del Nido cardioplegia.
Statistical analysis
Continuous data are presented as mean ± SD, median (Min–Max) and categorical data are presented as percentage and number. The data were checked for normality using the Kolmogorov−Smirnov test. Median scores of the parameters of the study and control groups were compared using the Mann–Whitney U-test. The chi-squared test was used to examine the relation between the groups and the categorical variables. Statistical analysis was performed using SPSS for Windows version 23.0 software (SPSS Inc., Chicago, IL, USA). The level of significance was set at p < 0.05.
Results
Fifty-two patients participated in the study. All patients were examined during the routine outpatient clinic visits and a 10-question questionnaire was administered at the time of the examination.
As seen Table 1, the age at the time of the study of the control group (median = 18.00) was higher than the study group (median = 13.00) (p < 0.001). Follow-up time by month for the control group (median = 119.00) was significantly higher than the study group (median = 63.00) (p < 0.001). The control group obtained higher median values (Median = 4.00) than the study group (Median = 3.00) on Tanner stages at the time of the examination (p = 0.003). In our clinic, patients were operated mainly with median sternotomy between 2010 and 2015, but with increasing experience after 2015, they were operated mainly with anterolateral thoracotomy. For this reason, the average age of the control group patients during the study is higher than the study group and their follow-up period is long. There is a difference between the Tanner stages of the patients in the control group, since the operation date is older and the follow-up periods are longer. However, when we look at the ages and Tanner stages of both groups during the operation, there is no difference between the two groups.
Table 1. Comparison of continuous parameters among the study and control group.
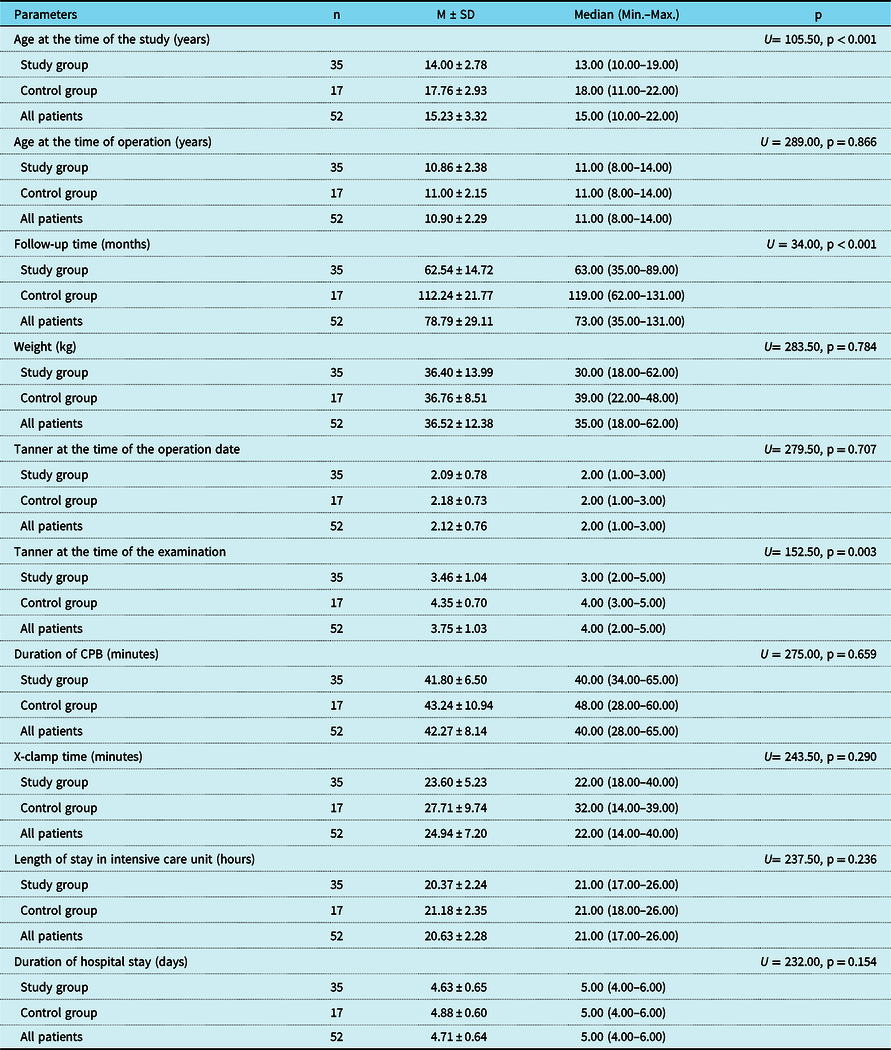
When we analysed the other variables in Table 1, no statistically significant difference was found between the groups (p > 0.05).
The comparison of the patients in the control and study groups is shown in Figure 1.
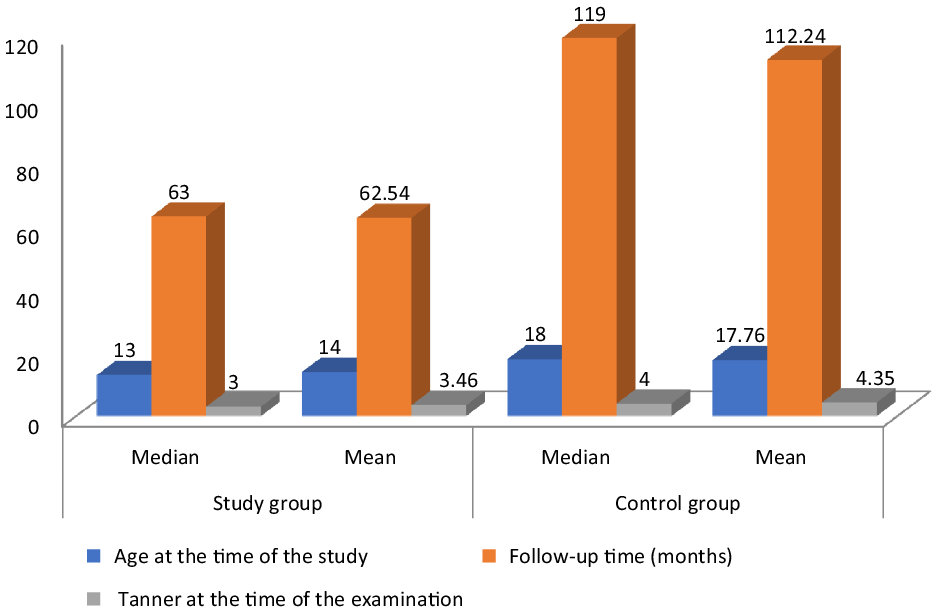
Figure 1. Comparison of follow- up time by months, age at the time of operation, and Tanner stage at the time of examination parameters among study and control groups.
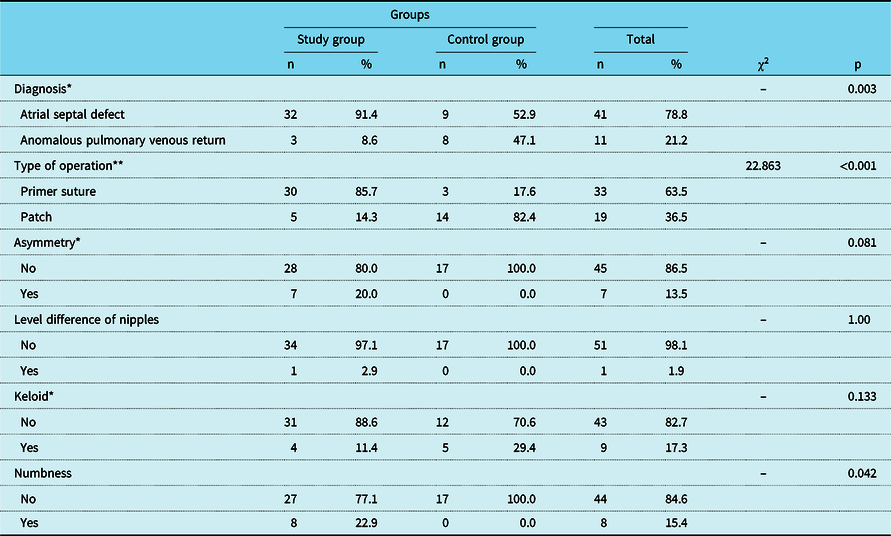
The relation between groups and type of the diagnosis was significant (p = 0.003). The percentage of atrial septal defect in the study group (91.4%) was higher than the control group (52.9%). Similarly, the percentage of primer suture in the study group (85.7%) was higher than the control group (17.6%) χ2 = 22.863, p < 0.001. Lastly, the percentage of the numbness in the study group was 22.9% whereas the percentage of the numbness in the control group was 0.0%. The difference in percentage is significant p = 0.042 (Table 2). However, there was no significant relationship between the other variables and groups in Table 2 (p > 0.05).
Table 2. Comparison of categorical parameters among the study and control group.
* Fisher’s exact test.
** Chi-square test.
In the study group, mean age was 10.86 ± 2.38. Which is corresponding to the normal age range for breast development in the Turkish population. In this group, out of 35 patients who were examined, 7 were stage 2 (20%) according to Tanner Breast Development Scale, 12 were (34.2%) stage 3, and 9 were stage 4 (25.7%). In the control group, out of 17 patient who was examined, 2 were stage 3 (11.8%) according to Tanner Breast Development Scale, 7 were (41.2%) stage 4, and 8 were stage 5 (47%).
Based on the measurement method, bilateral nipple distance according to upper limit of clavicle were same in all of the patient in study groups (100%). Those were evaluated as symmetrical. Three patients in study group (8.6%) had breast size differences. These patients were referred to plastic surgery for breast examination. Upon examination, plastic surgeons did not plan immediate intervention and followed up the patients, and as rest of the patients had no breast size differences (91.4%). In the control group, two patients had breast size differences and it was also reported in normal physiological limits following detailed examinations by plastic surgeons.
Post-operative neurological complications, mediastinitis, and surgical site infection were not seen in both groups. Three patients had pleural effusion regressed with treatment (two patients in study group, one patient in control group) and two patients had pericardial effusion (both in control group). Right internal mammary artery injury was not seen in the patients.
Electrocardiogram were normal in all patients. No block, arrhythmia, and tachycardia were found in the electrocardiogram documentation. All patients were in sinus rhythm. Echocardiography showed no haemodynamically significant residual atrial septal defect in both groups.
When we examined the answers to the survey questions;
The answer given by the patients of study group to the question of “how would you describe your scar” was excellent in 30 patients (85.7%) and good in 5 patients (14.3%). This has showed that the surgical method satisfies all patients cosmetically. The overall satisfaction rate for the cosmetic results of right anterolateral thoracotomy was 100%. In the control group, only seven patients answered this question as excellent or good and less than half of the patients (41.1%) found this surgical method satisfactory. The overall satisfaction rate for the cosmetic results of median sternotomy was 41.1%.
The percentage of those who said no to the question “Do you experience lack of self-confidence related your scar?” in the study group (100.00%) was significantly higher than the control group (52.9%), p < 0.001.
The percentage of those who said no to the question “Have you changed your clothes choice depending on your scar?” in the study group (100.0%) was significantly higher than the control group (70.6%) p = 0.002.
The percentage of those who said yes to the question “Would you like to be operated with the same approach if you will have surgery again?” in the study group (100.0%) was significantly higher than the control group (41.2%) p = 0.002.
The answer given by the patients to the question of “Did the postoperative pain last longer than 2 months?” was no in 28 (80.00%) patients in the study group, however this rate in the control group was (n = 2, 11.8%). This difference is significant p < 0.001.
The answers given by the patients to other survey questions are given in Table 3.
Table 3. Frequencies and percentages of survey questions among the study and control group.

a χ2 = 21.827.
* Fisher’s exact test.
** Chi-square test.
Discussion
Median sternotomy has been considered the most universal method for most cardiac procedures but has some disadvantages such as unsatisfactory cosmetic results. Also sternal dehiscence, sternal wound infections, and mediastinitis are complications which may become fatal. In spite of this, especially in patients with mild congenital defects, a permanent scar on the incision zone leads to a lifetime remembered condition which causes displeasure and psychological distress, especially in young female patients. Therefore, a successful and low-risk approach may be preferred instead of median sternotomy. Reference Vida, Tessari and Fabozzo3,Reference Bleiziffer, Schreiber and Burgkart6
Different approaches to treat CHDs in the paediatric population have been tested for years. The main objective of a surgeon is to provide adequate exposure, a safe vascular access for initiating cardiopulmonary bypass, effective myocardial protection, and ability to perform effective de-airing after the procedure. In our clinical experience of 35 patients operated with right anterolateral thoracotomy, we did not encounter intraoperative mortality, neurological deficit, or other complications. All of these findings indicate that this technique is as safe and effective procedure as median sternotomy.
In the early 1970s, right anterolateral thoracotomy was used as a safe alternative to median sternotomy. In the literature, most authors seem to like the cosmetic advantage of right anterolateral thoracotomy. Reference Vida, Tessari and Fabozzo3,Reference De Silva4 It is because the scar can be easily hidden if the patient is clothed and is not visible under the breast. Reference Däbritz, Sachweh, Walter and Messmer1 The patient’s preference in this regard is quite important. In our study group, all patients (100%) described the cosmetic result as excellent or good. Contrary to this result, 41.1% of patients in the control group gave this answers. In the light of these rates, it is obvious that there is a dissatisfaction in the control group.
Another issue is potential phrenic nerve injury after right anterolateral thoracotomy. While our group and Däbritz et al Reference Däbritz, Sachweh, Walter and Messmer1 could not find any risk on this matter (87 patients), Helps et al found an increased risk for phrenic nerve injury. Reference Dietl, Torres and Favaloro7 Other risk factors for phrenic nerve injury are direct damage, use of cautery nearby to the nerve, excessive thymus dissection, location of the pericardial sling sutures, sternal tension, internal jugular vein cannulation, and topical cooling. Reference Bleiziffer, Schreiber and Burgkart6 In our study, there was no patient with phrenic nerve injury after the examination of the chest radiographs in post-operative period.
Dietl et al Reference Dietl, Torres and Favaloro7 preferred subpectoral approach rather than transpectoral approach to prevent breast asymmetry after right anterolateral thoracotomy. The short follow-up period in these patients was considered as a limitation. Likewise, the follow-up period in the Tiete et al study was approximately 9 months and was a short period for evaluation. Reference Tiete, Sachweh, Kozlik-Feldmann, Netz, Reichart and Daebritz8 The average follow-up period in our study group is 62.54 months and follow-up period in all groups are 78.79 months. This follow-up period is quite long compared to the literature.
During this period, no breast asymmetry or insufficiency in breast development was found in any patient outside of the physiological limit during the follow-up. In another study conducted by Bleiziffer et al, breast development in the anterolateral thoracotomy group was found significantly deficient compared to the median sternotomy group in the long-term follow-up. Reference Bleiziffer, Schreiber and Burgkart6 Likewise, in the study of Işık et al, anterolateral thoracotomy-related breast development retardation was detected. Reference Isik, Ayik, Akyuz, Daylan and Atay9 On the other hand, in the series of Xu et al, breast asymmetry was found to be lower in the right anterolateral thoracotomy group, contrary to the literature Reference Xu, Zhu, Wang, Huang and Zhao2 complementary with our study as thoracotomy found not to have negative impact on breast development. Contrary to the literature, our study did not find any evidence that anterior thoracotomy adversely affected breast development.
When the question of what may be the negative causes of late breast development is examined; infant cadaver dissections showed that the distribution of the breast bud was at least 1.5 cm periphery of the nipple and areola complex. These findings showed that dissection in this region would harm future developing breast tissue. Reference Cherup, Siewers and Futrell10 In the study where Lou et al compared three surgical methods, it was emphasised that right submammary thoracotomy should be avoided in young female patients due to its potential to damage to the breast tissue and chest wall muscles, especially when applied at younger ages, the incision should be made as far away from the breast tissue as possible to avoid development insufficiency of the tissue in future breast development. Reference Luo Z.R.Chen and Yu11 The point where we agree on with this study is; We made the skin incision at least 4–5 cm (approximately sixth intercostal space) below the nipple and aimed to minimise the damage to the breast tissue. We strongly suggest the location of the incision in the submammary region needs to be very low under the right nipple (above the fifth-sixth intercostal space). Also, we believe that short skin incisions and limited muscle plane dissection prevent negative outcomes.
As it’s well known, breast asymmetry can be seen in healthy population as well. Loughry et al measured breast volumes in 598 female patients by using stereophotogrammetry. In 70% of the patients, the volume difference between the two breasts was found less than 20%. In these volume differences, often the right breast was found to be relatively smaller. Based on this, a generalisation may be made that a volume difference less than 20% may be accepted as normal and the right breast is generally the smaller breast. Reference Loughry, Sheffer and Price12 In our study, only three patients had a smaller right breast than the other, based on the examination findings of plastic surgeons these size difference and the volume difference was reported as physiological. As the right breast tends to be physiologically smaller, it is not certain to attribute this size difference in our study due to the right anterolateral thoracotomy approach. Our findings provide a new perspective on the use of anterolateral thoracotomy in the prepubertal period. Our technique does not adversely affect the development of the right breast. Contrary to the findings in the literature, the effect of the technique on the development of right breast is not more than the difference occurred in the physiological development of the right breast. In addition to this, the questionnaire answers show that patients would still want to be operated via Right Anterolateral Thoracotomy if they have to undergone surgery again. This outcome suggests that cosmetic results of the surgical approaches should also be taken into consideration.
Accordingly, Grinda et al Reference Grinda, Folliguet, Dervanian, Lïc, Legault and Neveux13 and Bauver et al Reference Bauer, Alexi-Meskishvilli and Nakic14 consider Right Anterolateral Thoracotomy to be more appropriate for female patients who have completed breast development and whose breast groove is apparent. Even though this approach is partially correct; the risk of adversely affecting breast development is minimised by making the skin incision more underneath as in our study and by entering the thoracic cavity from fourth intercostal space. In such type of operational method, surgical technique and safety are not adversely endangered in any way. In the study of Tasoglu et al, special attention was given to female patients between the ages of 9 and 13 as the pubertal age of females ranges around this gap. Also, it is indicated that, after surgery, no growth retardation on the breast which related to the surgical technique was found. Reference Tasoglu, Avci and Koca5 Additionally, in another study of Tasoglu et al, 27 patients who had mini skin incision for atrial septal defect closure recovered without adverse events and were satisfied with the cosmetic healing of the operation. Reference Taşoğlu, Sert and Demir15
The axillary region represents an interesting surgical access to the thoracic cavity due to particular anatomical properties: The skin is flexible, the muscles are relatively sparse and can therefore be spared, it is far away from breast tissue in girls, and the resulting scar is hidden under the resting arm. Right axillary access is proven to provide sufficient exposure of the right atrium and right heart structures. Reference Heinisch, Wildbolz and Beck16–Reference Yaliniz, Topcuoglu and Gocen18 Since this area is in far proximity to the breast tissue, we have been performing atrial septal defect cases with vertical right axillar mini thoracotomy since 2018. Although the surgeon is moved away from the heart in thoracotomy with the right axillary incision, this distance does not create a disadvantage in surgery as experience improves. In this study, we demonstrate the safety and efficacy of Right Anterolateral Thoracotomy with limited skin incision in the surgical repair of an atrial septal defect. Our experience confirms that this technique, when compared with median sternotomy, offers satisfactory cosmetic results and affords good and symmetric breast development, good surgical exposure, and a satisfactory recovery. There was no compromise in the technical repair and conversion to a full sternotomy can be done at any time during the procedure. Despite the small number of nonrandomised patients, we believe that this type of procedure with a limited skin incision does not compromise exposure of the great vessels and should be favoured over other approaches.
Conclusion
Based on our results, we consider that our procedure is safe and effective with improved cosmetic results compared to median sternotomy which also confers many advantages such as less trauma, less pain, faster recovery, and shorter hospital stay. This study presents one of the largest series of paediatric patients for whom atrial septal defect closure via right anterolateral thoracotomy by central cannulation was performed. However, further studies are required to confirm these findings.
Limitations
Since the questionnaire used in the study is a questionnaire created by the researchers by scanning similar publications, it is a subjective assessment. This creates limitations for this study.
Acknowledgements
The primary author would like to acknowledge the following: Research Asistant Cem Soylu, for statistical analysis.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
The authors have no actual or potential conflict of interest in relation to this presentation.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees (Ankara City Hospital Clinical Researches Ethics Committee. Ref No. E1-20-1409 Date:23/12/2020).










