Mitral annular disjunction (MAD) is a fibrous separation between the attachment of the mitral valve posterior leaflet hinge and basal left ventricular myocardium. Reference Toh, Mori and Izawa1 Mitral annular disjunction is often seen with mitral regurgitation in myxomatous mitral valve disease and mitral valve prolapse (upwards of 50.8 and 32.6%, respectively). Reference Bennett, Thamman and Griffiths2 It has been reported in patients with ventricular tachyarrhythmia and sudden cardiac arrest. Reference Dejgaard, Skjølsvik and Lie3 Inferolateral mitral annular disjunction can be readily identified on an echocardiographic parasternal long-axis view. Reference Bennett, Thamman and Griffiths2
A 17-year-old female with previously diagnosed mitral valve prolapse with moderate mitral regurgitation who presented with 5 days of fever, petechiae and Staphylococcus aureus bacteremia. While being treated for infective endocarditis, she acutely decompensated with respiratory distress and hypotension. Emergent echocardiography showed new concern for perforation of the posterior leaflet and mitral annular disjunction, which was not previously recognised (Fig. 1, Video 1). A three-dimensional echocardiogram demonstrated a 15-mm X 8-mm perforation in P1 and P2 (Fig. 2a–b, Video 2). Given haemodynamic instability in the setting of Staphylococcus aureus endocarditis and the new finding of mitral valve perforation, Reference Otto, Nishimura and Bonow4 surgical intervention was indicated. The defect measured 12–15 mm in diameter in P1–P2 scallop of the mitral valve consistent with findings from the 2-dimensional and 3-dimensional echocardiogram (Fig 2c–d). The damaged posterior leaflet was excised, and the defect was repaired using an autologous pericardial patch. Pathology examination of the excised leaflet showed a fibropurulent plaque with abundant fibrin and neutrophils consistent with infective endocarditis. Tissue culture resulted methicillin-sensitive Staphylococcus aureus, matching her blood cultures. The patient had an uneventful postoperative recovery, completed the course of antibiotics, and had mild mitral regurgitation at discharge. She has been followed up over the last two years with no evidence of ventricular arrhythmia. However, she unfortunately had recurrent regurgitation at the perforation possibly due to active inflammation at the time of her initial surgery. She is scheduled for repair in the coming months at the time of writing this manuscript.
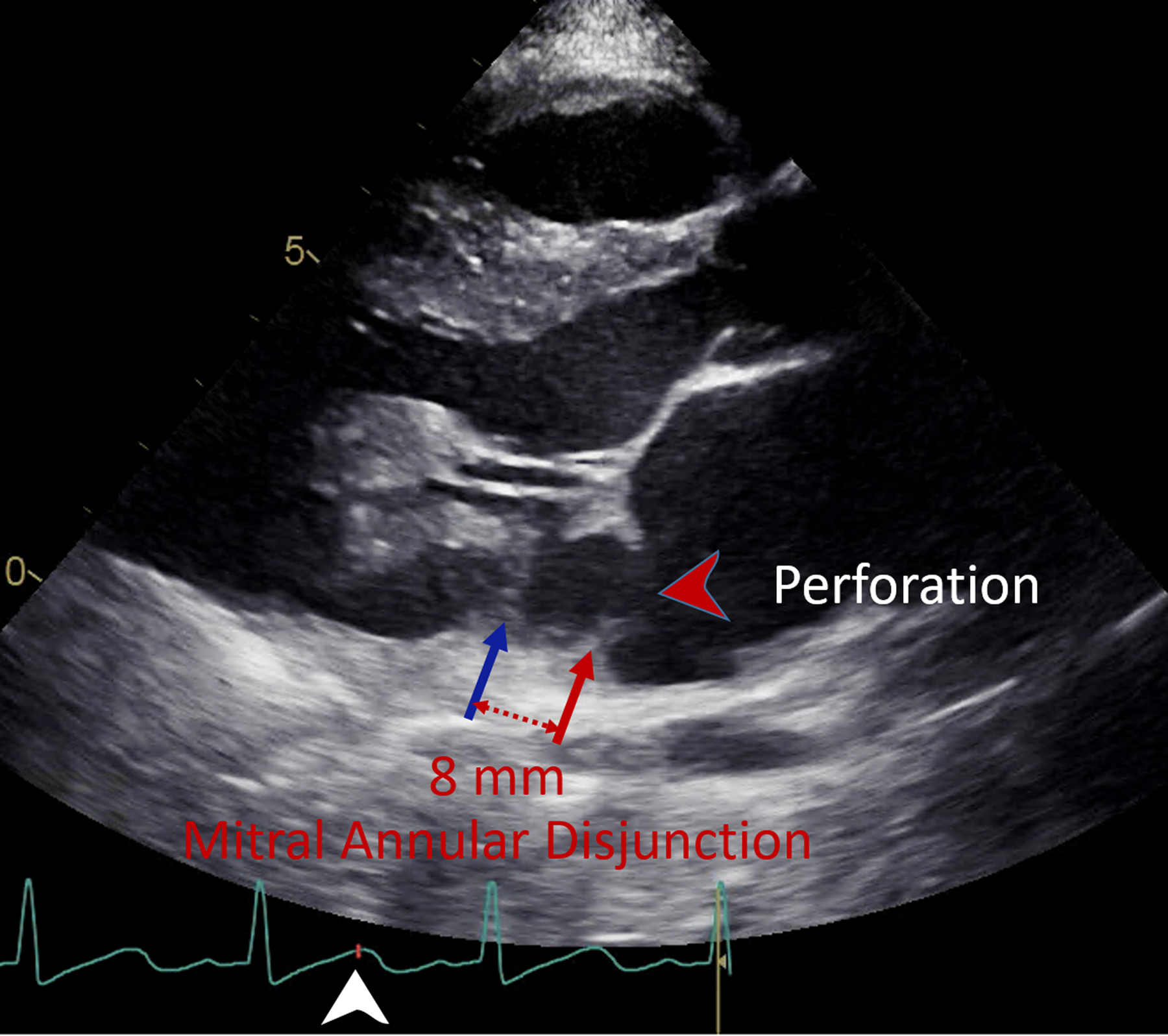
Figure 1. Parasternal long-axis view of mitral annular disjunction and perforation of the posterior leaflet near the disjunction. Mitral annular disjunction is defined as the fibrous separation between the attachment of posterior leaflet (red arrow) and basal left ventricular myocardium (blue arrow) measured at end systole (white arrowhead). A perforation in the posterior leaflet is suspected (red arrowhead).

Figure 2. Three-dimensional echocardiographic image and surgical inspection of the perforated posterior mitral valve leaflet. ( a , b ) Three-dimensional echocardiographic images with and without colour mapping of a large perforation in the P1–P2 scallops (arrowheads). ( c , d ) Surgical view and diagram of the mitral valve from a left atrial view demonstrating a 15 X 8 mm perforation (arrowheads) between P1 and P2 scallop of the posterior leaflet. AL = anterolateral commissure, AoV = aortic valve, P1, P2, P3 = scallops of the posterior mitral valve leaflet, PM = posteromedial commissure.
Mitral annular disjunction is associated with an area of fibrous thin wall exposing to the high-pressured left ventricle. Reference Toh, Mori and Izawa1 This is a rare case of mitral valve perforation near the area of disjunction. Awareness of mitral annular disjunction allowed for the diagnosis to be recognised, although much remains to be learned about mitral annular disjunction in the paediatric population. Three-dimensional echocardiography provided helpful information to explain for clinical deterioration and surgical planning, which aided in the successful management of this patient.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951123002615.
Acknowledgements
The authors appreciate Dr. Michiaki Imamura for the image of the mitral valve from surgical inspection and Ms. Kaitlin Doan for her assistance in editing the videos.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
None.





