Diaphragm paralysis is defined as "the presence of elevated hemi-diaphragm(s) on chest radiograph in conjunction with evidence of weak, immobile or paradoxical movement assessed by ultrasound or fluoroscopy" based on Society of Thoracic Surgeons (STS) Congenital Heart Surgery Database complication code specification. 1 The aetiology of diaphragm paralysis may be broadly classified into five categories: (i) traumatic, (ii) compression-related, (iii) inflammatory, (iv) neuropathic, and (v) idiopathic. The traumatic causes of diaphragm paralysis include open-heart surgery, lung transplantation, and other mediastinal procedures. Reference Qureshi2 Although unilateral diaphragm paralysis may be well tolerated in older children and adults; young children and infants are more prone to untoward effects of a failed diaphragm, since the intercostal muscles are not effective with regard to increasing the dimensions of the thoracic cavity during inspiration. Reference Stone, Brown, Canal and King3 The reported prevalence of diaphragm paralysis in children varies from 0.4 to 16% depending on the type of the study, age, diagnostic tools, and other factors. Reference Zhang, Wang, Li, Yang, Sheng and Yan4,Reference Guillemaud, El-Hakim, Richards and Chauhan5 Phrenic nerve injury and associated diaphragm paralysis may be a consequence of dissection, contusion, stretching, and thermal injury both in terms of hypothermia (i.e., topical cooling) and hyperthermia (i.e., electrocautery). The clinical presentation of diaphragm paralysis may vary from asymptomatic cases to respiratory distress, atelectasis, recurrent pulmonary infections, and inability in weaning from mechanical ventilation Reference Zhang, Wang, Li, Yang, Sheng and Yan4 . Plication of the diaphragm for diaphragm paralysis was first defined even a century ago, in 1923, by Morrison. Reference Morrison6 The data in literature with regard to the timing and indications of plicating the elevated diaphragm following diaphragm paralysis encountered after cardiac surgery are controversial. Reference Goldberg, Krauthammer and Ashkenazi7
Herein, we aimed to present our experience in a patient population who underwent plication of the diaphragm after paediatric cardiac surgery, especially focusing on the implications of diaphragm paralysis in patients with univentricular physiology.
Materials and methods
This was a retrospective and single-centre study which was approved by the local Ethics Committee (03/09/2022-022). The primary and secondary outcomes of this study were determined as: (i) diaphragmatic paralysis that may develop due to phrenic nerve injury after paediatric cardiac surgery, and (ii) analysing the results of patients who underwent plication of the diaphragm in order to reduce morbidity and hospital stay, respectively. A total of 1938 patients who had undergone congenital cardiac surgical procedures in our centre between January 2012 and January 2022 were reviewed retrospectively. The medical records of the 20 patients who underwent a total of 23 plication of the diaphragm procedures due to phrenic nerve injury or palsy were evaluated. The patients were selected based on aetiology and a combination of clinical manifestation and chest imaging characteristics. Asymptomatic cases with diaphragm paralysis were excluded from the study group. Informed consents were obtained from the participants of the study.
The highest incidence of diaphragm paralysis was encountered in systemic to pulmonary artery shunt patients (7 out of 152 patients, 4.6%). The second highest incidence of diaphragm paralysis was experienced in arterial switch operation (2 out of 53 patients, 3.7%). We encountered 4 patients with diaphragm paralysis in a total of 253 bidirectional cavopulmonary anastomosis (1.58%) and one patient with Fontan procedure out of 168 cases (0.59%).
Surgical technique
Our most important parameter for selecting the site to perform plication of the diaphragm (whether sternotomy or thoracotomy) was the position of the cardiac apex. Thoracotomy was the preferred method when the apex and diaphragm paralysis were at the same side. On the other hand, we performed plication of the diaphragm via sternotomy when the apex and diaphragm paralysis were at opposite sides. This preference was based on an idea of performing a safe procedure in terms of haemodynamic stability during the operation, in which we did not have to manipulate the heart chambers and the apex during the plication.
We preferred a modified technique of diaphragmatic plicating which does not require muscle resection. Reference Stone, Brown, Canal and King3,Reference Shoemaker, Palmer, Brown and King8–Reference Schwartz and Filler9 After visualising the elevated diaphragm, we began plication at the far most part of the diaphragm muscle with a 4/0 or 5/0 pledged enhanced polypropylene suture. The diaphragm was gently pulled, and the first U-suture was placed and stabilised with a tourniquet. This manoeuvre helped to fix the diaphragm at a lower level than the anatomic position, and the proceeding sutures were put more easily and closer to the costodiaphragmatic or pericardiodiaphragmatic recesses. At this point, the bites of the sutures should be taken with extreme care to avoid damage to the abdominal organs, vascular structures, and visible phrenic nerve fibres. All the sutures were tightly tied down; the thin and elevated flaccid diaphragmatic muscle was pleated forming a taut hemidiaphragm (Fig 1). In cases where a satisfactory hemi-diaphragmatic stabilisation was not achieved only with a longitudinal technique, the second layer of transverse U-sutures was also added in anteroposterior diameter in order to enhance plication of the diaphragm. This decision was made purely intraoperatively. Following longitudinal plication, in case islands of diaphragmatic tissue was left in between the squeezing polypropylene sutures, transverse sutures were added (Fig 2).
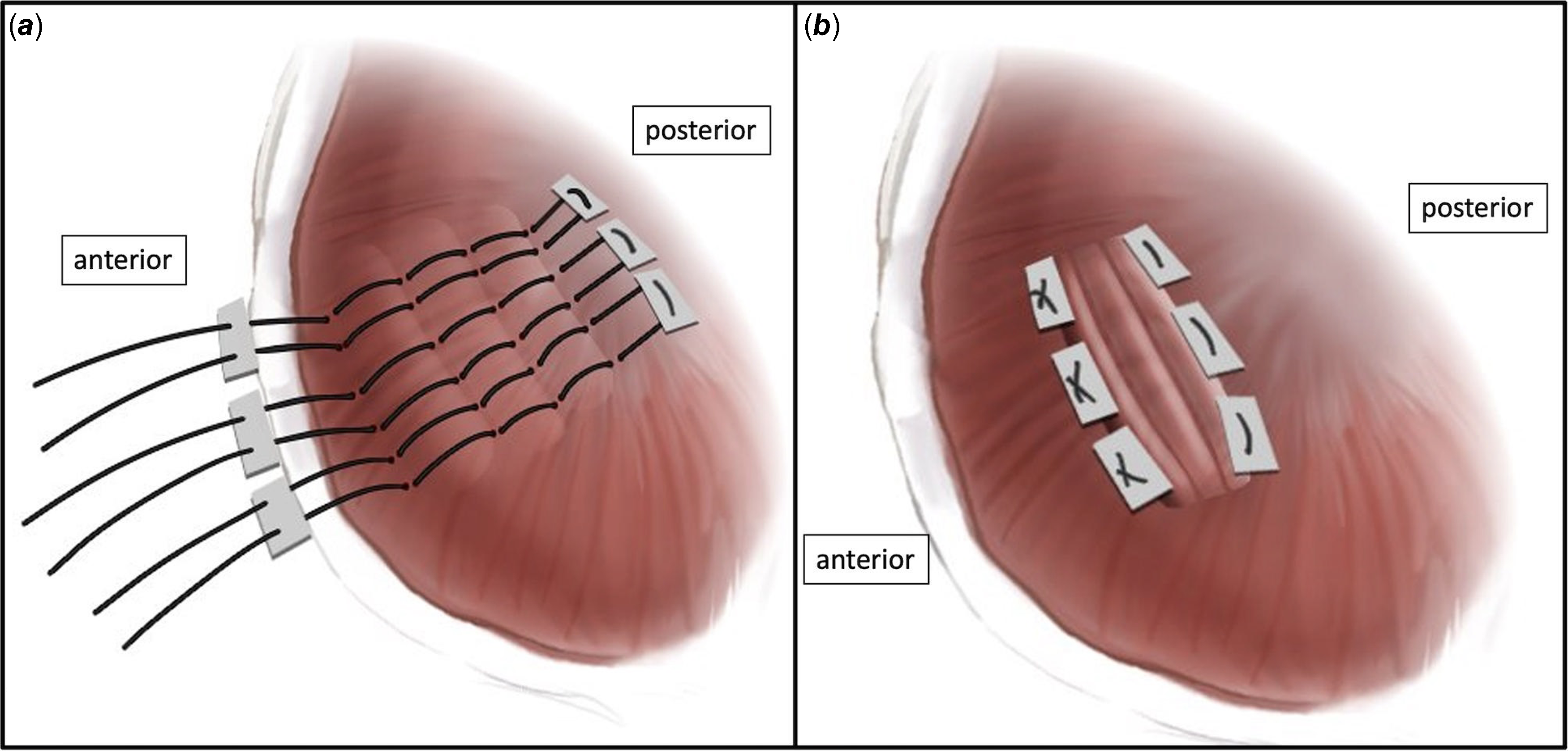
Figure 1. Transverse technique of diaphragm plication. The pledgeted sutures are placed ( a ) and tied ( b ) in anteroposterior direction.

Figure 2. Longitudinal technique of diaphragm plication. The pledgeted sutures are placed ( a ) and tied ( b ) in mediolateral direction.
Results
We encountered 20 patients (15 males and 5 females) with diaphragm paralysis out of the 1938 cases performed during the above-mentioned time period, and the overall incidence of diaphragm paralysis was 1% in our centre. Three of them had bilateral diaphragm paralysis. Fifteen diaphragmatic plications (66%) were performed via thoracotomy, whereas eight of them were performed via midline sternotomy (34%). We performed bilateral plication of the diaphragm for patients no. 3, 8, and 17 in the same session. These three patients’ paradoxical diaphragmatic motions did not improve in the follow-up period before plication of the diaphragm. Tracheostomy was not deemed mandatory in any of the cases in our patient population. Mean age and body weight were 18.2 ± 15.1 months (range 1–48 months) and 8.3 ± 3.7 kg (range 3–17 kg), respectively. Out of 20 patients with the diagnosis of diaphragm paralysis, 14 of them (70%) were operated with cardiopulmonary bypass and 6 of them were (30%) operated without cardiopulmonary bypass at the operation for underlying cardiac malformations. The period between the cardiac surgical procedure and the plication of the diaphragm was 18.7 ± 16.8 days (range 2–55 days) except for the patient no. 6 who had intraoperative phrenic nerve injury, and the decision of plication of the diaphragm was made at the same time with cardiac surgery. The demographic, operative, and post-operative data of the patients are summarised in Tables 1 and 2.
Table 1. Summary of the patients who underwent diaphragmatic plication after paediatric cardiac surgery.

BW: body weight; STS-EACTS: Society of Thoracic Surgeons-European Association of Cardiothoracic Surgery; DPL: diaphragmatic plication; TGA: transposition of the great arteries; ASD: atrial septal defect; VSD: ventricular septal defect; PDA: patent ductus arteriosus; DORV: double-outlet right ventricle; MV: mitral valve; LV: left ventricle; RV: right ventricle; PA: pulmonary atresia; IVS: intact ventricular septum; LV: left ventricle; TA: tricuspid atresia; TOF: tetralogy of Fallot; AV: atrioventricular; CAVSD: complete atrioventricular septal defect; APVS: absent pulmonary valve syndrome.
Table 2. Operative details of the patients.

DPL: diaphragmatic plication; ASO: arterial switch operation; VSD: ventricular septal defect; USG: ultrasonography; AP: anteroposterior; PAB: pulmonary artery banding; DORV: double-outlet right ventricle; PA: pulmonary artery; RMBTS: right modified Blalock–Taussig shunt; TOF: tetralogy of Fallot; coA: coarctation of the aorta.
Patients who had prolonged intubation with an unsuccessful weaning from mechanical ventilatory support or patients with respiratory distress after extubation were evaluated with anteroposterior chest radiograms and/or diaphragmatic ultrasonography and/or fluoroscopy. Diaphragmatic plication was extensively reserved for the symptomatic patients with diaphragm paralysis.
We encountered an unsuccessful attempt of weaning from mechanical ventilatory support and prolonged intubation in 11 of the cases (55%), whereas 8 of the patients (40%) were weaned form mechanical ventilation but had respiratory distress after extubation. Therefore, except for patient no. 6, all patients had at least one unsuccessful attempt of weaning from mechanical ventilatory support. In patient no. 6, who had a univentricular physiology, while preparing the superior vena cava and the pulmonary artery, a probable injury to ipsilateral phrenic nerve could not be ruled out, and a plication of the diaphragm was performed following the cavopulmonary anastomosis.
When the age groups of our patients were analysed, the incidence of diaphragm paralysis was 5% (n = 1) in neonates, 40% (n = 8) in infants, and 55% (n = 11) in children. Five (25%) of the patients had univentricular physiology, whereas 15 of them (75%) underwent biventricular repair. Eleven (55%) of the patients had a cyanotic and nine of them (45%) had acyanotic CHDs. We encountered right-sided diaphragm paralysis in nine (45%) and left-sided diaphragm paralysis in eight (40%) patients. Three of the patients (15%) had bilateral involvement (patient no. 3, 8, and 17), and bilateral plication of the diaphragm was performed with 2-, 12-, and 13-day intervals, respectively.
Seven of our patients (35%) had re-sternotomy. The mean time period after the cardiac surgical procedure and plication of the diaphragm was 18.77 ± 16.86 days (range 2–55 days). We had nine cases (45%) with an STS/EACTS Risk Score of 4.
All of the patients had undergone successful extubation on the first attempt after plication of the diaphragm, and any re-intubation was not necessary. In our clinical practise, we take a chest X-ray at continuous positive airway pressure mode of the mechanical ventilator immediately before extubation in cases where a diaphragm paralysis is suspected. An elevated diaphragm was considered as an indirect sign of possible phrenic nerve damage, and further evaluation was scheduled, most commonly with ultrasonography.
Extubation times and ICU stay after plication of the diaphragm were 2.1 ± 1.2 days (range 1–5 days) and 6.6 ± 3.6 days (range 3–15 days), respectively. The follow-up period was 4.3 ± 2.6 years (range 1–9 years). We did not encounter any mortality in this patient population.
Discussion
Twenty-three successful plication of the diaphragm were performed in 20 patients with a diagnosis of diaphragm paralysis out of a total of 1938 operations performed in our centre. The primary and secondary end points of our study were to determine diaphragm paralysis due to phrenic nerve injury after paediatric cardiac surgery and to analyse the results of plication of the diaphragm in order to reduce morbidity and hospital stay, respectively.
Diaphragmatic paralysis after congenital cardiac surgery is an important factor affecting the respiratory functions of the patient. Although there is a wide variation across the centres (0.3–12.8%), a recent multicentre review reported an incidence of 1.16% (126 centres, 191.463 patients). Reference Fraser, Ravekes and Thibault10 The incidence of diaphragm paralysis in neonates, infants, and children are 2.19%, 1.22%, and 0.55%, respectively. The risk is reported to be maximum in patients undergoing Norwood procedure (3.7%), truncus arteriosus repair (3.4%), and arterial switch operation (3.2%) in this multicenter study. Reference Fraser, Ravekes and Thibault10 Nevertheless, underdiagnosis is speculated to be encountered when routine screening for diaphragm paralysis is not scheduled. Reference Tantawy, Imam, Shawky and Salah11 On the other hand, in cases with bilateral diaphragm paralysis, false-negative results may be obtained on chest X-ray, since the contralateral diaphragm could not be considered as a reference point in order to check for the level of the suspected side. The incidence of diaphragm paralysis requiring plication of the diaphragm in our patient population is 1.03% that is comparable with large series. Depending on our clinical experience, we recommend to check the diaphragmatic mobility in every patient at the first transthoracic echocardiography following extubation at ICU, regardless of the respiratory status in order to be aware of the asymptomatic cases.
Several factors have been emphasised in order to clarify the aetiology in patients with diaphragm paralysis encountered after cardiac surgery. Reoperations are under more risk due to adhesions and altered anatomical relationship of the mediastinal structures. Reference Saygılı, Mercan and Bitir12 Seven out of 20 (35%) cases of our patient population were reoperations. Intraoperative administration of topical cold and systemic hypothermia, efforts to divide/clip the previous systemic-to-pulmonary artery shunts during complete repair of cyanotic heart defects, harvesting pericardium, dissecting or excising thymus, cannulation of superior vena cava, and damage due to electrocautery may all lead to phrenic nerve damage. Reference Saygılı, Mercan and Bitir12 We recommend not to administer topical ice slush into the pericardial sac routinely besides mild to moderate hypothermia depending on the type of surgical procedure and underlying CHD. In patient no.6, damage to the paraphrenic fatty tissue could not be ruled out during left superior vena cava to left pulmonary artery anastomosis (i.e., left-sided Glenn procedure); therefore, we performed plication of the diaphragm after the cavopulmonary anastomosis before closing the sternum. We generally do not use electrocautery during preparation for cavopulmonary anastomosis, and haemostatic clips are safe alternatives in order to dissect vena cava without significant bleeding. Another idea may be using the monopolar electrocautery in "cut" mode rather than "coagulate" mode, since the traditional unipolar devices may heat the tissues even lead up to 300°C. Reference Massarweh, Cosgriff and Slakey13
Although several series report different incidences of diaphragm paralysis among various cardiac pathologies, effects of diaphragm paralysis in patients undergoing univentricular palliation may lead to unfavourable outcomes. Reference Fraser, Ravekes and Thibault10 In patients with univentricular physiology, the right ventricular driving force of the pulmonary blood flow is lacking; hence, the intrathoracic negative pressure generated by a normally functioning diaphragm gains importance. On the other hand, this deprivation in the pulmonary circulation leading to an impaired endothelial function and nitric oxide release reduced vascular recruitment and impaired lung growth, and all leads to progressive elevation in pulmonary vascular resistance (PVR). Reference Henaine, Vergnat and Bacha14,Reference Gewillig, Brown and Heying15 The increase in PVR is an important factor that jeopardises the late outcome of patients undergoing univentricular palliation. Reference Kreutzer, Kreutzer and Kreutzer16
Probably, one particular subset of patients with diaphragm paralysis after paediatric cardiac surgery consists of univentricular type of palliation including each stage ending up with Fontan completion. The patients generally have more than one sternal entry and venous cannulation attempts at neighbourhood of phrenic nerve, and diaphragm paralysis in these patients leads to restrictive ventilatory impairment. Reference Komori, Hoashi and Shimada17 The impaired respiratory physiology with diaphragm paralysis leads to suboptimal Fontan circulation with regard to prolonged pleural effusion, longer hospitalisation, and accumulation of ascites. Reference Ovroutski, Meskishvili and Stiller18,Reference Amin, McElhinney and Strawn19 In fact, these findings are not surprising, since inspiration augments systemic venous flow more significantly than in normal humans. Reference Ovroutski, Meskishvili and Stiller18 Nevertheless, Hsia and colleagues documented that even diaphragm paralysis dose not completely resolve normal subdiaphragmatic venous haemodynamics in patients with Fontan circulation, since a plicated diaphragm inspiration-derived hepatic venous flow is suppressed and portal venous system loses its physiological expiratory augmentation. Reference Hsia, Khambadkone, Bradley and de Leval20 The upstream congestion and downstream limited flow, in fact, is prone to fail even in an optimal Fontan, since the constructed neo-circulation is a palliative one rather than being physiological. Reference Rychik21 Stevenson demonstrated that in patients with univentricular circulation, a normal respiratory function has important contribution to pulmonary branch flow distribution; however, in patients with diaphragm paralysis, the loss of diaphragm function is associated with reduced pulmonary flow on the affected side and increased flow on the normal side; hence, a redistribution of pulmonary flow is encountered. Reference Stevenson22 In our patient series, we encountered five patients with diaphragm paralysis undergoing univentricular palliation. All of these cases were reoperations except patient no.6. In our limited experience, we strongly recommend close follow-up of the diaphragmatic function in patients with univentricular palliation, either with recent onset respiratory distress, suspicion of an elevated diaphragm on chest X-ray, or reduced diaphragmatic muscle movements drawing attention at transthoracic echocardiography. Moreover, we recommend plication of the diaphragm before the final stage (i.e., Fontan completion) of univentricular palliation whenever a diaphragm paralysis is encountered in order to perform this stage at optimum haemodynamic and respiratory conditions. Nevertheless, since even after plication of the paralytic diaphragm in a Fontan patient, findings similar with a failing univentricular circulation may be observed; therefore, in such patients, preventing the diaphragm paralysis is much more important rather than trying to “sink the lifted.” Reference Podgaetz, Diaz and Andrade23
The most debated topic with regard to management of diaphragm paralysis in terms of plication is whom and when to intervene. Firstly, the primary aim of plication of the diaphragm is to treat dyspnoea; hence, the ultimate indication for operative intervention should better be discussed in a symptomatic patient. Reference Podgaetz, Diaz and Andrade23 Symptomatic relief following plication of the diaphragm may also be related to an increase in forced expiratory volume (FEV1), improvement in tidal volumes, and decrease in respiratory rate. Reference Welvaart, Jak and Veerdonk24 However, these symptoms like respiratory distress, persistent atelectasis, paradoxical breathing (i.e., Hoover’s sign; indrawing of the intercostal muscles during inspiration), or inability to be weaned from mechanical ventilatory support may be sought more aggressively in patients with univentricular physiology in order to perform plication of the diaphragm earlier. Reference Talwar, Agarwala, Mittal, Choudhary and Airan25 Talwar and colleagues recommend a broad guideline in order to define the indications for plication of the diaphragm in children with diaphragm paralysis after open-heart surgery as: (i) age under 6 months, (ii) respiratory distress, (iii) tachypnoea, (iv) oxygen dependency, (v) carbon dioxide retention, (vi) inability to wean from ventilator, and (vii) children with cavopulmonary shunts with the intention to prevent increase in PVR. Reference Talwar, Agarwala, Mittal, Choudhary and Airan25
The second most debated parameter in literature is the timing of plication of the diaphragm, which is the definitive surgical option in patients with symptomatic diaphragm paralysis. Some authors recommend plication of the diaphragm whenever the diagnosis of diaphragm paralysis is confirmed, while others recommend a waiting period of 1 to 6 weeks in anticipation of potential spontaneous recovery. Reference Stone, Brown, Canal and King3,Reference Zhang, Wang, Li, Yang, Sheng and Yan4,Reference Ricoy, Rodríguez-Núñez, Álvarez-Dobaño, Toubes, Riveiro and Valdés26 Georgiev and colleagues retrospectively analysed two strategies for surgical plication: one with plication of the diaphragm after multiple extubation attempts and other with a more aggressive early plication of the diaphragm. Reference Georgiev, Konstantinov and Latcheva27 Their limited data with plication of the diaphragm revealed that an aggressive strategy with early plication was not associated with decreased morbidity in terms of reintubation rate, ventilation time, and ICU stay; however, they excluded the newborns and only approximately 20% of their patients had univentricular physiology. Reference Georgiev, Konstantinov and Latcheva27 At this point, there is conflicting data about long-term function of the paralysed diaphragm and the possibility of spontaneous recovery. A prospective analysis of diaphragm paralysis in patients after cardiac surgery was reported by Yemisci and colleagues with the primary end point of preventing unnecessary plication of the diaphragm. They evaluated the electrophysiological phrenic nerve latencies and action potential amplitudes before and after congenital cardiac surgery in 59 patients. They concluded that prolonged phrenic nerve latencies and decreased diaphragmatic action potential amplitudes were common in the post-operative period, most of which were transient and clinically insignificant. Reference Yemisci, Cosar, Karatas, Aslamaci and Tokel28 Baker et al. analysed the quantitative return of diaphragm function over time after plication of the diaphragm which may probably be related to non-permanent nature of the thermal or stretch injury. Moreover, due to the high incidence of diaphragmatic function recovery (94%) in their study group, exploration of the phrenic nerve at the time of plication of the diaphragm was not recommended in order to prevent further injury. Reference Baker, Boulom and Reemtsen29 In selected cases, minimally invasive endoscopic plication may be an alternative for plication of the diaphragm even in infants. Reference Fujishiro, Ishimaru and Sugiyama30
Tracheostomy has been advised in some reports in patients whose phrenic nerve recoveries were significantly prolonged; however, tracheostomy may also be associated with increased mortality. Reference Bhaskar, Lone, Sallehuddin, John, Bhat and Rahmath31,Reference Cotts, Hirsch, Thorne and Gajarski32 We did not have to perform tracheostomy in any of our patients. Bhaskar and colleagues recommend tracheostomy for bilateral diaphragm paralysis in patients who have not recovered after 3 months of conservative management or in those with recurrent lung infections. Reference Bhaskar, Lone, Sallehuddin, John, Bhat and Rahmath31
Although not encountered frequently, diaphragm paralysis following phrenic nerve palsy is a significant complication following congenital cardiac surgery. Documentation of a possible dysfunction of the diaphragm should be a routine part of the post-operative echocardiography, especially in patients under the age of 1 year and in patients who will eventually undergo the consecutive stages of univentricular palliation. Our results are encouraging in terms of clinical improvement in patients with diaphragm paralysis who underwent surgical plication.
Limitations
The limitations of our study include low number of patients, as well as lacking post-operative long-term follow-up studies aiming to document recovery of the diaphragmatic muscle after plication of the diaphragm. Further prospective studies in order to compare plicated and non-plicated patients with diaphragm paralysis may help to provide further insight with regard to recovery of diaphragm function over time.
Acknowledgements
The authors would like to thank Sabri Cagri Sezgin for illustrations of the surgical technique.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of interest
None.
Ethical standarts
The authors assert that all procedures contributing to this work comply with the ethical standards of the Helsinki Declaration of 1975, as revised in 2008.







