The carotid artery is an alternative and reliable access for patients whose femoral artery cannot be used due to repetitive interventional procedures and surgical operations. Additionally, in certain patient populations, such as premature infants, the carotid arteries are primarily preferred because they are wider than the femoral artery and provide easier access to the intervention site. Reference Justino and Petit1 On the other hand, the neck being a difficult area in terms of compression, weakness of the surrounding connective tissue, individual and technical problems can cause rare but important complications. Pseudoaneurysm is one of these important complications, and with early diagnosis and good management, treatment can be provided without sequelae. Reference Webber, Jang, Gustavson and Olin2 In this paper, diagnosis and treatment of pseudoaneurysm in a patient who underwent interventional treatment via common carotid artery will be presented.
Case presentation
A 6-month-old girl was admitted to the hospital for evaluation for coarctation balloon angioplasty. In medical history, the patient was operated on due to aortopulmonary window, interrupted aortic arch, and aortic coarctation when she was 12 days old. Balloon angioplasty was performed for recoarctation 1 month later. Then, she underwent a second operation due to left phrenic nerve palsy. The patient was referred for evaluation due to recoarctation. On physical examination, she weighed 4.3 kg and revealed scars from previous surgeries around the left thoracotomy and left subcostal region. The femoral pulses were weak. A 2/6 systolic ejection murmur was heard in the interscapular region. On the echocardiogram, there were left ventricular hypertrophy and diastolic flow pattern in descending aorta. It was decided to perform a balloon coarctation angioplasty for the recurrence of the aortic coarctation. In the catheter laboratory, efforts to find access from femoral and axillary arteries were unsuccessful. Left common carotid artery access was performed by using an 18-gauge needle and 0.035-inch wire under ultrasound guidance, and a 4F sheath was inserted. Intravenous heparin 30 unit per kilogram was admitted. There were no complications during the procedure (Fig 1). The patient was discharged from the hospital one day after the procedure. After 10 days, the family noticed a prominent mass on the left side of the patient’s neck. The patient was called in for control. During the patient’s examination, a 2 × 2 cm pulsating mass on the left side of the neck, with no signs of infection on the skin, was noted (Fig 2). On ultrasound, a 2 × 2 cm pseudoaneurysm was detected adjacent to the left common carotid artery (Fig 3). To better assess the location. of the pseudoaneurysm, a CT angiography was performed. CT revealed a 3 × 3 cm pseudoaneurysm with a 3 mm connection with the left common carotid artery, located 2 cm below the bifurcation. Due to the pseudoaneurysm, the trachea and surrounding structures were noted to be shifted to the right side (Fig 4). The management was discussed with the department of interventional radiology. A stent graft was not suitable since the patient was an infant. Even the pseudoaneurysm neck was narrow, percutaneous thrombin injection still had a risk of distal emboli, and it was not possible to insert a filter into common carotid artery due to unattainable femoral access. With the department of cardiovascular surgery, it was decided upon to move forward with a surgical treatment plan. During the operation, considering the pseudoaneurysm sac’s growth direction, an incision was made lateral to the right sternocleidomastoid muscle. Sternocleidomastoid was excluded laterally, and the sac was partially exposed with a meticulous dissection. Proximal and distal parts of the carotid artery were identified and clamped after heparinisation. The pseudoaneurysm sac was excised, and the coagulum was removed. 1–2 mm needle hole on carotid artery was localised and closed with separated stitches (Fig 5). The clamps were removed, and the blood flow was re-established. The patient was extubated in the operating room and transferred to the paediatric ICU without any complications. The repeat ultrasound on the post-operative fourth day was normal, and the patient was discharged without any neurologic problems.
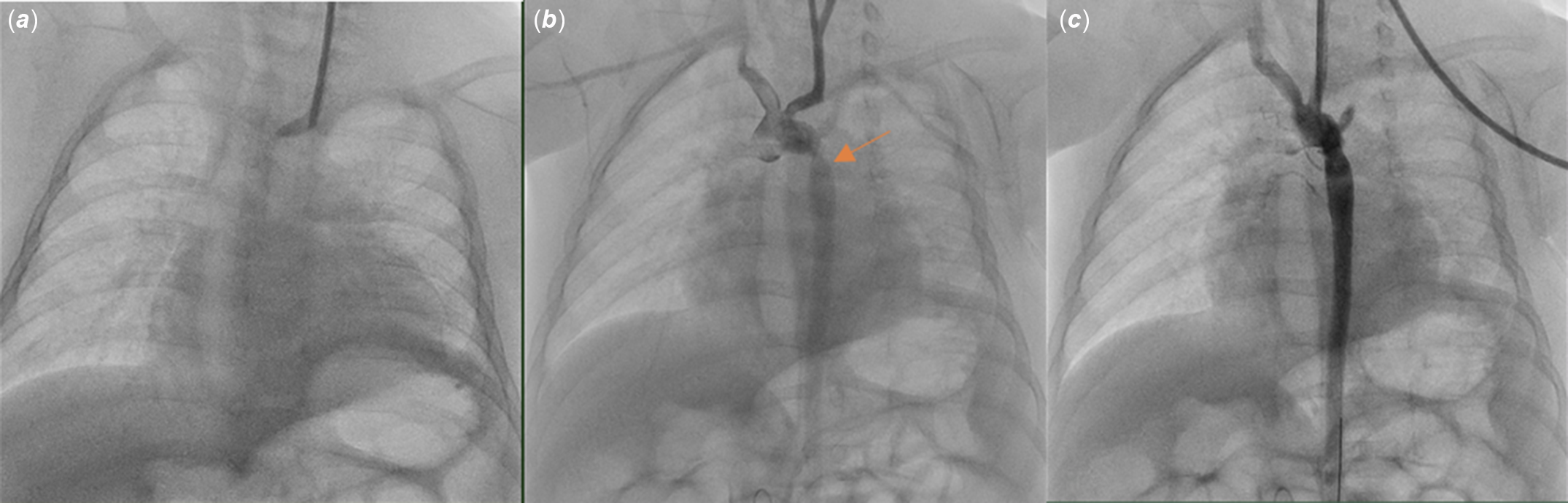
Figure 1. 4F sheath was placed in the left common carotid artery under ultrasound guidance in the catheterisation laboratory (A). The orange arrow indicates the region of severe coarctation in the descending aorta (B). Enlargement of the coarctation area after balloon angioplasty (C).

Figure 2. The swelling on the left anterior side of the neck is shown.
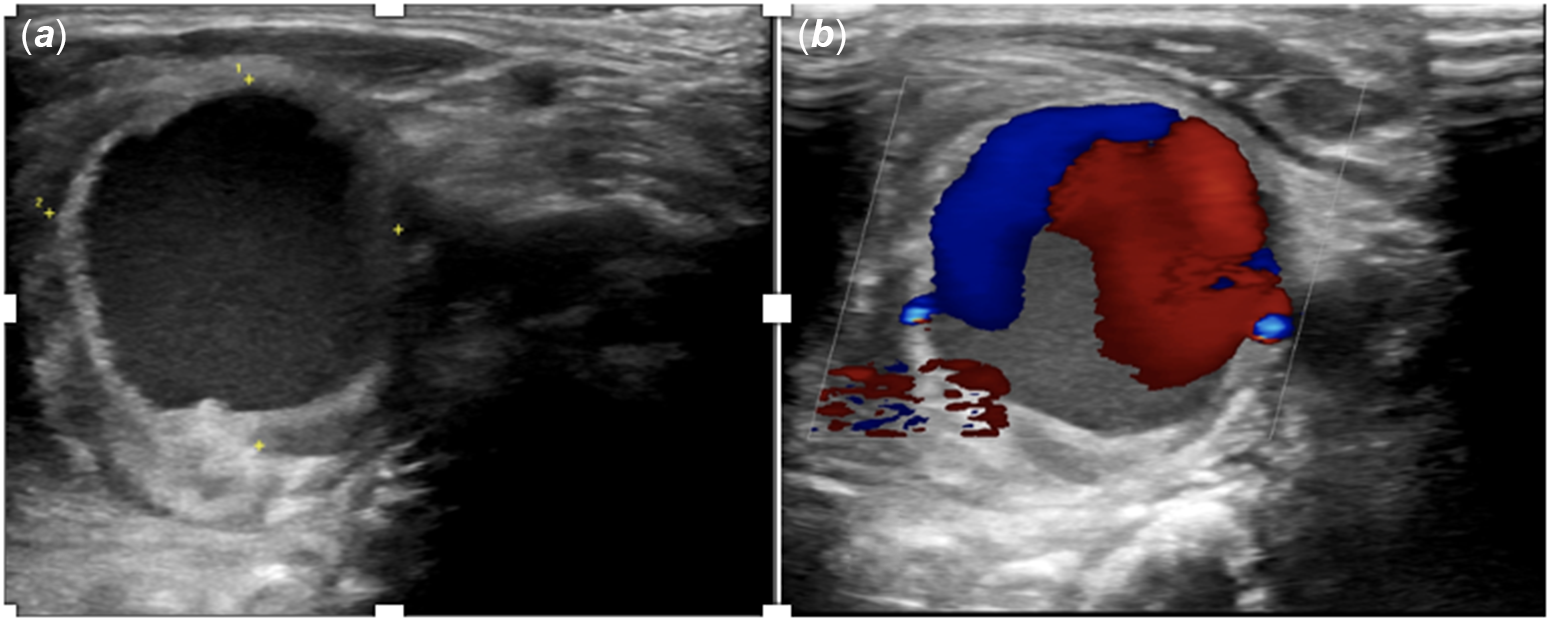
Figure 3. Carotid Doppler ultrasound revealed a 20 x 20 mm pseudoaneurysm in the left common carotid artery (A). "Yin Yang" colour pattern is specific for the pseudoaneurysm (B).
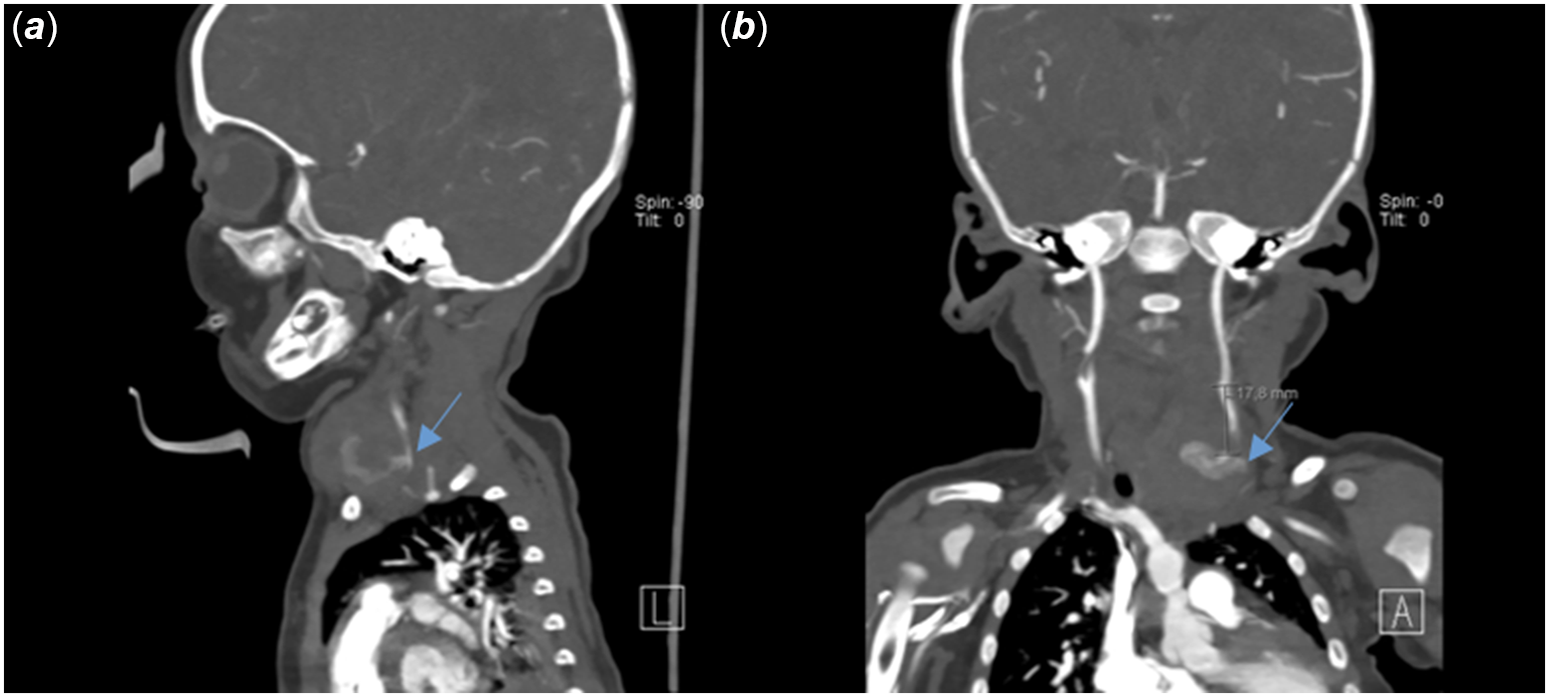
Figure 4. The sagittal section blue arrow shows the orifice of the pseudoaneurysm originating from the left common carotid artery (A). In the coronal section, it is observed that the pseudoaneurysm is approximately 2 cm below the bifurcation (B).
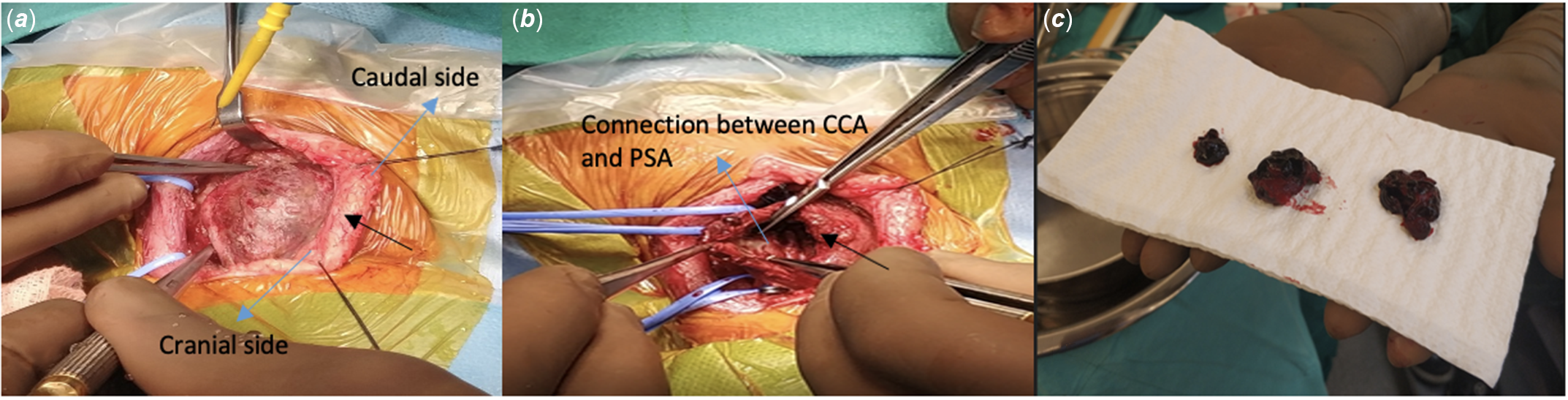
Figure 5. (A) Large pseudoaneurysm is seen (Black arrow). (B) The appearance of the pseudoaneurysm after evacuation and its connection with the common carotid artery is seen (Blue arrow). (C) Hematoma draining through the pseudoaneurysm. (CCA: Common carotid artery, PSA: Pseudoaneurysm).
Discussion
In patients who have previously undergone interventional procedures and cardiac surgeries, the traditional femoral approach is not always possible, and different vascular accesses are required. Carotid, axillary, brachial, and radial arteries can be used when necessary for vascular access. Azzolina et al. proved in the late 1960s that cardiac catheterisation in infants and young children could be performed using the common carotid artery. Reference Azzolina, Eufrate and Allella3 In the neonatal period, the axillary artery is wider than the femoral artery, providing easier access to pathology, and not affecting the extremity circulation compared to the femoral artery. Previously, access was gained with the cut-down technique, but nowadays, ultrasound-guided carotid access is performed. Reference Ligon, Kim, Vincent, Bauser-Heaton, Ooi and Petit4 In this presented case, the procedure was performed in a timely manner under ultrasound guidance since an access could not be obtained from the femoral arteries. In a study evaluating vascular complications in children undergoing catheterisation, Roushdy et al. reported that large sheath size, young age, and low body weight increase the risk of complications. The most common complications reported in this study were temporary loss of pulse (%17.6), bleeding (%3), subcutaneous haematoma (%2), vessel tear (%0.2), and vein thrombosis (%0.2). Reference Roushdy, Abdelmonem and El Fiky5 In a study conducted by Justino et al., 42 children who had undergone an interventional cardiac catheterisation procedure through the common carotid were evaluated; a pseudoaneurysm formation was reported only in a single patient. Reference Justino and Petit1 In our study, we evaluated the ductus stent implantation in newborns with a ductus-dependent pulmonary circulation. Arterial access was gained via the common carotid artery in 14 patients, and no patient developed a pseudoaneurysm. Reference Onalan, Odemis and Saygi6 Pseudoaneurysm develops after damage to the arterial wall, with a permanent connection between the artery and the cavity formed outside the vessel. It differs from true aneurysm by not participating in the formation of the three layers of the arterial wall. Reference Gulla, Chaudhary, Sahoo and Sachdev7
Pseudoaneurysm is a very rare complication and is mostly caused by not applying enough compression following interventional procedures. Reference Katzenschlager, Ugurluoglu and Ahmadi8 It may result in life-threatening complications due to rapid bleeding and airway compression. After the sheath removal, pressure was applied to the area for 10 minutes and there was no evidence of swelling in the procedural area the next day. The patient’s family stated that they noticed the swelling on the left side of the infant’s neck 10 days later and that there was no previous noticeable difference. In our study protocol, Doppler ultrasound is not routinely planned for every patient following the procedure. Further, patients with no pulse, who develop pain or swelling that are inappropriate with their clinical picture, are evaluated with an ultrasound before their discharge. Routine post-procedure ultrasound may be beneficial in early detection of pseudoaneurysms, especially in newborns and infants. Ultrasonography is a cost-effective, non-invasive, accessible, and effective imaging tool in the diagnosis of pseudoaneurysm. It guides the diagnosis with its high sensitivity and specificity. CT provides a better understanding of the anatomy and the relationship of the pseudoaneurysm with the surrounding structures. The size of the pseudoaneurysm neck and imaging from different axes are guiding the treatment plan. For imaging, conventional angiography is the gold standard. Despite the invasive nature of the procedure, it is preferred more in patients who are only being considered for simultaneous treatment. Reference Sarioglu, Capar and Belet9 After identifying the pseudoaneurysm with ultrasound with Doppler in our patient, the structure, location, and relationship of the aneurysm with other tissues were clearly demonstrated with CT. The first choice of treatment in patients with pseudoaneurysms detected earlier is ultrasound-guided compression and percutaneous thrombin injection. If these procedures fail, interventional procedures including coil embolisation, vascular plugs, and stent deployment options are mostly sought for. Reference Zhong, Islim, Sundararajan, Tahir, Goddard and Patel10 In patients for whom interventional treatment options are not deemed possible, a surgical approach can be an option to successfully eliminate the pseudoaneurysm in a way that ensures vascular continuity. In this case, ultrasound-guided compression was not considered because of the patient’s late presentation, the possibility of embolism, and airway compression associated with the pseudoaneurysm.
Conclusion
Carotid pseudoaneurysms are seen rarely following an interventional procedure in infants and children. This potentially fatal complication can be avoided and treated early by ensuring adequate compression, close follow-up, and utilising different imaging modalities. When planning a catheter procedure for small infants with previous interventional or surgical procedures, the appropriate preparations and precautions must be performed prior to, during, and after the procedure to avoid vascular access complications.
Acknowledgements
We thank Dr. Ömer Özden and Dr. Murat Tanyıldız for the management of the case after the post-operative process.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.










