Introduction
COVID-19 (2019 novel coronavirus) activity continues to cause a high disease burden and hospitals around the world remain vulnerable to ventilator scarcity. Reference Burke, Midgley and Dratch1,Reference Ranney, Griffeth and Jha2 Crisis based Standards of Care guidelines aim to maximize the number of lives saved by reallocating resources from those who will not benefit to those who will, and reducing potential bias and clinician moral distress resulting from ad hoc bedside rationing. 3 In the United States, 26 states have allocation guidelines and 15 use the Sequential Organ Failure Assessment (SOFA) score to triage patients. Reference Piscitello, Kapania and Miller4
SOFA scores predict mortality in hospitalized patients, Reference deGrooth, Geenen and Girbes5 and provide objective data to reduce the need for clinician judgment that may be prone to bias. It is unknown how efficiently they ration resources to patients who are most likely to survive. We use data from the peak of the spring 2020 surge of COVID-19 in New York City (the period with the highest disease burden) to model performance of a protocol adapted from New York State’s 2015 guidelines. 6 The protocol, as adapted from the 2015 guidelines, was not implemented and ventilators were not rationed at the study sites during the study period. This report estimates how well the adapted protocol would have predicted outcomes, had the protocol been implemented. The authors are unaware of other published literature that has modeled a ventilator rationing protocol using similar data.
Methods
This protocol was reviewed and approved by the Montefiore/Einstein Institutional Review Board (IRB# 2020-11324). This is a chart review of a representative random sample (205) of 20.5% of all intubated adult patients (1002) in 3 NYC hospitals between March 25, 2020, and April 29, 2020, regardless of etiology of respiratory failure. All 1002 patients were assigned an ordinal numerical value. A simple randomization program was used to obtain the study sample of 205 patients. The population of 1002 patients had an average age of 64 years. COVID positivity rate was 74%, of which 57% were male. The average age for the COVID negative fraction of the 205 patients (21%) was 63 years, of which 59% were male and 86% had ≥ 1 comorbidity. Average age for the COVID positive fraction of the 205 patients (79%) was 64 years, amongst whom 57% were male and 96% had ≥1 comorbidity. Adult patients with and without COVID-19 were included because the protocol would apply to all patients during a crisis.
SOFA scores were calculated using MDcalc (MdCalc, New York, USA) for the time of intubation: 48 hours and 120 hours post-intubation using the worst values available for the previous 24 hour period for 6 organ systems. These included the ratio of partial arterial pressure of oxygen to fraction of inspired oxygen, whether the patient required respiratory support, platelet count, Glasgow Coma Scale (GCS) value, bilirubin, mean arterial pressure or vasoactive agent requirements, and creatinine. The respiratory component in the conventional SOFA score is comprised of a ratio of 2 values (partial arterial pressure of oxygen and fraction of inspired oxygen) and 1 binary variable (whether on respiratory support). Reference Vincent, Moreno and Takala7 When combined, these 3 data inputs produced the single respiratory sub-score. Thus, the SOFA score calculations were still comprised of 6 sub-scores, as is conventionally done.
If all 205 patients from the sample survived to the 120-hour assessment, 615 SOFA scores would have been calculated, with 6 sub-scores each, resulting in a maximum possible 3690 sub-scores. However, as patients expired or were weaned, their SOFA scores were not calculated. A total of 502 SOFA scores were calculated, with 6 sub-scores each, resulting in 3012 total data points, of which 75 (2.5%) were missing. For patients intubated prior to arrival, the initial assessment was performed using the earliest available in-house data. If no data was available for a sub-score, the lowest possible sub-score value was used to avoid inappropriately assigning higher SOFA scores. GCS scores were assumed to be normal for 295 total sub-scores in sedated patients due to the inability to record accurate GCS scores in sedated patients. Reference Lambden, Laterre, Levy and Francois8
Our analysis was descriptive; we calculated mortality and the proportion of patients categorized into four groups based on the SOFA score guidelines: blue (ventilator should not be offered or should be removed), red (highest priority for ventilator), yellow (intermediate priority for ventilator) and green (weaned or ventilation not indicated) at each interval. Triage decisions based on SOFA score recalculation at different intervals allowed for simulation of how the SOFA score component of the triage guidelines would have performed in this cohort. Predictive accuracy of the other exclusion criteria included in the adapted triage guidelines was not studied.
Results
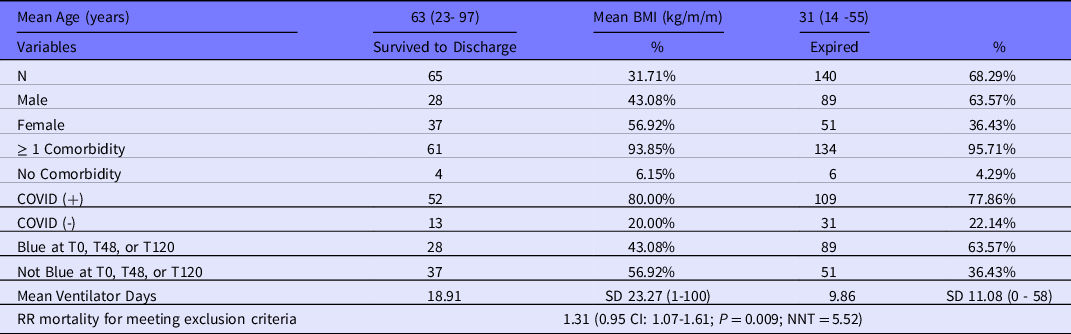
Approximately 20% of the sample was COVID-19 negative. Of 205 patients, 65 (32%, 95% CI 25-39%) survived to discharge. About 117 patients (57%, 95% CI 50-64%) were categorized as blue at 1 or more points in time and would have been candidates for exclusion from ventilation. Out of the 117 patients who were categorized as blue points, 28 (24%, 95% CI 17-33%) ultimately survived hospitalization. Patients who had ever been in the blue category had a higher mortality rate (76%) if compared with those who were never categorized blue (58%, P < 0.01). Of the 140 patients who died, 89 (63%) were categorized as blue during at least one time point (Table 1). The Figure does not only illustrate fluctuations in patient categorization over time, but also how SOFA at T120 discriminated better than at T48. All 16 blue-category patients at T0 had SOFA scores ≥ 11. Of the 95 blue-category patients at T48, 35 had SOFA scores ≥ 11 and 60 were categorized as blue due to lack of sufficient improvement in SOFA score. Out of 49 blue-category patients at T120, 29 had SOFA scores ≥ 11 and 20 were categorized as blue due to lack of sufficient improvement in SOFA score.
Table 1. Characteristics of study population
Limitations
The primary limitation of this study is that it is a retrospective descriptive single center study which limits generalizability. Another limitation was missing data for some SOFA scores. However, this limitation represents a real-world challenge which clinicians would face in implementation of an organ dysfunction score-based triage protocol during a public health crisis. Thus, these data reflect the conservative approach to managing such circumstances in practice. The sample size of 205 limits generalizability as well. The lack of detailed outcome analysis, such as the discharge dispositions for patients who were extubated, is another limitation.
Discussion
Ventilator triage protocols aim to maximize survival by redirecting ventilators from those who will die with or without them to patients who are more likely to survive with ventilator support. In this sample, more than 50% of the patients (57%) would have been categorized as blue and identified as candidates for ventilator removal over the first 120 hours following triage. Mortality was similar in red and yellow categories. However, more lives can be saved only if a ventilator is reallocated from a patient who will die despite ventilation to another patient who will survive with ventilation. The 28 patients who survived were assigned to blue category (43% of survivors) and would have likely died if ventilation was withdrawn. If all 117 ventilators from patients in the blue category were re-directed to prioritized patients with similar survival rate (41%), an estimated 48 patients would have survived compared to the 28 patients in the blue category. Real-life gains in survival would depend on the actual shortfall of ventilators, staff availability, and the rate at which new patients with respiratory failure presented. Improvements in the management of COVID-19 since the initial surge have also improved mortality. Thus, these data may not reflect what would happen in a different institution if there was a need for triage later in the pandemic. Though mortality was higher in this cohort than in other studies from similar geographic areas and time points, this investigation included only patients who required mechanical ventilation. Reference Filardo, Khan and Krawczyk9,Reference Keene, Shiloh and Eisen10
During the study period, the 3 NYC hospitals were able to avoid rationing by implementing resource augmentation measures such as alternative ventilator support and staffing strategies. The impact of these changes in care delivery processes on mortality is unknown. These data are consistent with other studies which have found poor SOFA score discriminant accuracy up to the time of intubation. Reference Raschke, Agarwal, Rangan, Heise and Curry11 However, these data also demonstrate limited SOFA score discriminant accuracy in mechanically ventilated patients at multiple assessment intervals during hospitalization.
Since over 50% of all patients were categorized as blue during at least 1 assessment interval, clinical judgment may still be needed in reallocating ventilators and deciding which patients in the blue category to extubate first. This may re-introduce bias and exacerbate moral distress, both being issues that an effective ventilator triage protocol ought to address. 6
Adjustments to improve score discrimination may include assessing priority at a much later time in order to reflect the prolonged respiratory failure of patients with COVID-19. The difference in outcome prediction accuracy between T48 and T120, as depicted in Figure 1, highlights this. More specific scoring systems such as the 4C mortality score may improve performance compared with the SOFA score. Reference Knight, Ho and Pius12 Alternative triage strategies such as the first-come first-served, randomization, clinician judgement, and use of triage committees, all lack empirical efficacy data and have well described ethical shortcomings which would need to be creatively addressed. 3
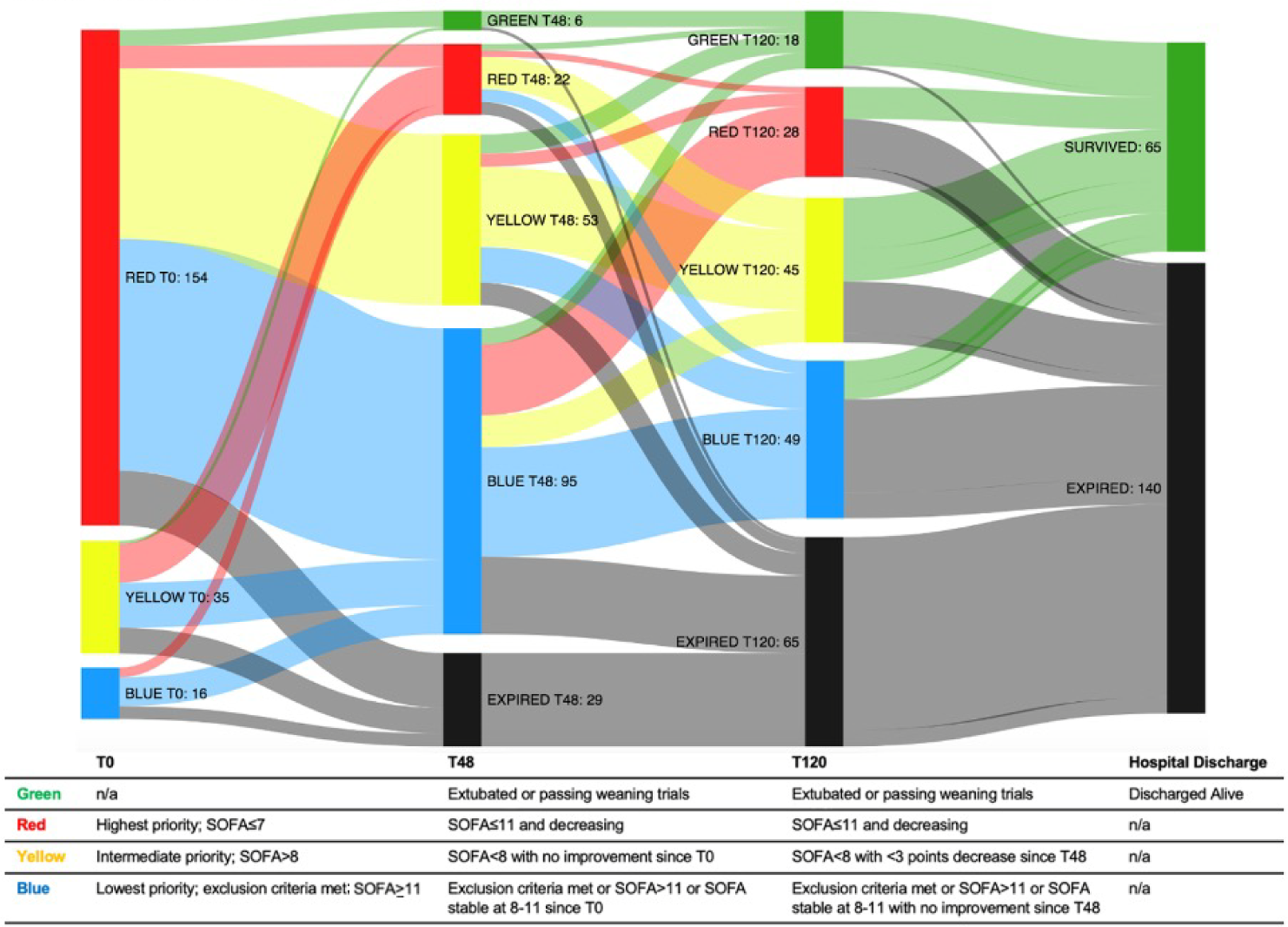
Figure 1. Fluctuations in SOFA color categorizations over time.
Our findings differ from a recent large retrospective cohort study which found that few patients were categorized in the New York State guideline blue category among more than 40000 ICU admissions in a national sample. Reference Wunsch, Hill and Bosch13 Our sample more closely reflects the acuity of pandemic conditions. However, both sets of findings demonstrate that existing guidelines poorly identify those who will not benefit from mechanical ventilation.
Conclusion
Currently, apart from excluding patients with overwhelming short-term likelihood of death, no known triage system has empiric evidence that it predicts mortality with sufficient accuracy to substantially increase population survival. The data from this preliminary study suggest that the SOFA score has a limited utility in triage, thus raising questions as to whether there is sufficient ethical justification to impose a life-ending decision on a subset of patients to offer potential benefit to a modest number of others.
Conflict(s) of interest
The authors have no conflicts of interest to disclose.
Funding statement
Elizabeth Chuang PhD received funding from the National Center for Advancing Translational Sciences Institutional Career Development Core KL2TR002558-03, through the Einstein-Montefiore Institute for Clinical and Translational Mentored Clinical/Translational Research Career Development Award.




