The World Health Organization (WHO) reports that at least 2.2 billion people worldwide suffer from a vision impairment or blindness, with the global need for eye care projected to increase dramatically in the coming decade. 1 At least 1 billion of these cases are preventable, and unsurprisingly, the burden of avoidable blindness is uneven, with 89% of vision impaired people living in low- and middle-income countries. 1 Vision loss poses a considerable challenge to health systems and economies, particularly when health systems are damaged.
Each year, hundreds of millions of people are affected by sudden-onset disasters and conflict that cause major human and material losses that can easily overwhelm local resources and health systems. 2–4 Following a sudden-onset disaster (eg, earthquake, tsunami, explosion), there can be sudden loss of health infrastructure, including hospitals. 5 Damage to health infrastructure severely affects health service delivery and can set back the development gains of a health system by years. Reference McMaster and Bamashmus6 Emergency Medical Teams are often invited to assist in providing initial direct clinical care following outbreaks and emergencies, and while they can play a vital role in supporting local health systems, their missions are usually temporary. 7,Reference Naor, Heyman and Bader8
There is a need to develop an intermediate system for the delivery of effective eye care, deployed following the initial emergency response and kept in place until the recovery of health infrastructure and strengthening of health systems in resource-scarce environments affected by sudden-onset disaster, complex humanitarian events, and conflict. This study proposes a design plan for a low-cost, reproducible mobile eye hospital that can be assembled and operated by minimal personnel and benefits from the high-efficiency systems developed by established surgical eye camps in resource-scarce environments.
Eye Camps
Eye camps are temporary screening and treatment facilities that provide eye care at the point of need, and are widely used in areas of the world where access to permanent ophthalmic services is limited. Reference Venkatesh, Muralikrishnan and Balent9–Reference Nayak, Kamath and Nayak14 Some countries rely heavily on the use of eye camps; in Nepal, populations in geographically inaccessible rural mountain areas rely on outreach camps for eye care services, whereas inhabitants of the flat Terai region benefit from hospital-based care. Reference Nowak and Grzybowski10,Reference Nowak15 In Yemen, even before escalation of conflict in 2015, the primary health-care facilities were not equipped to provide effective ophthalmic screening and treatment, resulting in the widespread use of eye camps to support these services. Reference McMaster and Bamashmus6,Reference Bamashmus and Al-Barrag12
Loss of vision from cataracts is most commonly caused by ageing, but it is also associated with eye injuries and infection, exacerbated by ultraviolet (UV) light exposure, smoking, and diabetes, all of which are significant problems in resource-poor settings. Cataracts are effectively treated by surgical removal and implantation of an intraocular lens (IOL). There are approximately 65.2 million cases of cataract causing moderate or severe vision impairment or blindness worldwide. 1 Establishing cataract treatment serves as a platform for developing other ophthalmic services and many eye camps focus on cost-effective cataract surgery. Between 2018 and 2019, teams from the Aravind Eye Care System in India screened more than 560,000 patients, performing almost 90,000 cataract operations in outreach camps. 16
Using standardized protocols and surgical techniques (ie, manual small incision cataract surgery), cataract eye camps can process a high volume of patients, achieving good postoperative visual outcomes with low rates of intraoperative and postoperative complications compared with local hospital standards. Reference Venkatesh, Muralikrishnan and Balent9,Reference Nowak and Grzybowski10,Reference Sangameswaran, Verma and Raghavan17,Reference Trivedy18 The Aravind model optimizes the efficiency of high-volume cataract services by striving to reduce costs, both to patients and of providers. Reference Ravilla and Ramasamy19 To reduce travel expenses for patients, these eye camps charter local bus services and ensure a quick turnover by performing all investigations during a single visit and offering an immediate appointment for surgery if indicated. By training mid-level ophthalmic personnel to undertake routine tasks, such as prepping and draping the eye, surgeons can maximize their operating time. Skilled surgeons can perform manual small incision cataract surgery in under 5 min, with some performing 80 procedures or more in a 6-h operating window without compromising the quality of patient outcomes. Reference Venkatesh, Muralikrishnan and Balent9,Reference Trivedy18
Although the incidence of operative complications in eye camps is generally low, the consequences for patients can be severe. Posterior capsule tears resulting in vitreous prolapse are the most common intraoperative complication. Reference Venkatesh, Muralikrishnan and Balent9,Reference Nowak and Grzybowski10,Reference Sangameswaran, Verma and Raghavan17,Reference Trivedy18 Because this complication may result in a poor visual outcome if the vitreous is not removed, it is important to ensure the availability of an automated vitrectomy machine. The most common postoperative complication following high-volume cataract surgery in eye camps is posterior capsular opacification, which can be easily treated with an yttrium-aluminum-garnet (YAG) laser. Reference Venkatesh, Muralikrishnan and Balent9,Reference Nowak and Grzybowski10,Reference Sangameswaran, Verma and Raghavan17,Reference Trivedy18 Surgical missions can be equipped with a portable YAG laser to treat this complication when patients return for follow-up months or years after surgery. Postoperative infections, which can destroy the eye, may present a few days after surgery, and the narrow window of opportunity to treat them with antibiotic injections can be missed if the teams have already departed.
In common with eye camps, mobile eye units can be used to provide treatment in rural and remote areas. The level of equipment varies from basic instrumentation needed for ophthalmic examinations to on-board operating theaters, Reference Sangameswaran, Verma and Raghavan17,Reference Sharma, Chakrabarty and Pavan20–Reference Hautala, Hyytinen and Saarela22 they can be used to deliver eye care to remote locations and have shown their efficacy in disaster relief. Reference Yuki, Nakazawa and Kurosaka23 Whereas mobile eye units have deployed on aircraft, ships, and trains, this study addresses the need for clinical facilities transported by road vehicles for deployment on land in resource-scarce environments in low- and middle-income countries.
Mobile Eye Hospital
The WHO defines a field hospital as, “a mobile, self-contained, self-sufficient healthcare facility capable of rapid deployments and expansion or contraction to meet emergency requirement for a specified period of time”. 7 Field hospitals can be broadly split into 3 categories: flying, floating, and terrestrial. All have their own advantages and logistical challenges. Reference Bitterman and Zimmer24 An ideal field hospital is both mobile and modular, allowing easy transportation, quick assembly, and expansion if necessary. The WHO classifies emergency medical team field hospitals into type 2 and 3, with at least 20 and 40 inpatient beds, respectively. 25 In ophthalmology, the most common causes of vision loss can be successfully treated as outpatient procedures and within clinics, allowing for a unique use of space without the need for large numbers of inpatient beds.
Design
This study proposes a design plan for a mobile eye hospital using established commercially available structures, including an expandable shipping container and a rapid assembly field tent. 26–28 The emphasis is on providing comprehensive high-volume services without needing the logistical complexity of military operations. The design focuses on easy assembly, dismantling, and operation by minimal numbers of personnel (Figure 1). For transportation, a truck capable of delivering a standard 20-ft shipping container to the target location is the minimum requirement. Four hydraulic jacks unload the container onto the ground. Equipment packed into wheeled, ruggedized, waterproof, and dustproof boxes are unloaded from the container. The container walls expand, increasing the internal floorspace. A rapid-assembly field tent in man-portable bags is unpacked from a trailer, which contains a generator and portable environmental control unit (ECU) meeting the Centers for Disease Control and Prevention (CDC) air exchange standards. 28 The field tent is erected and connected to the container by an inflatable corridor (Figure 2).
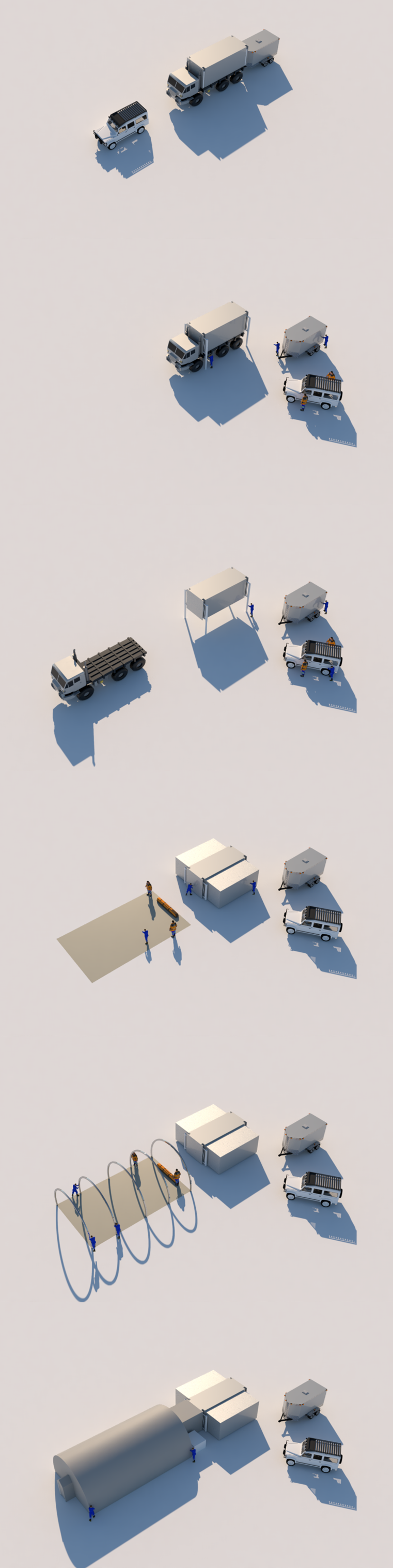
Figure 1. Deployment phases of a mobile eye hospital.
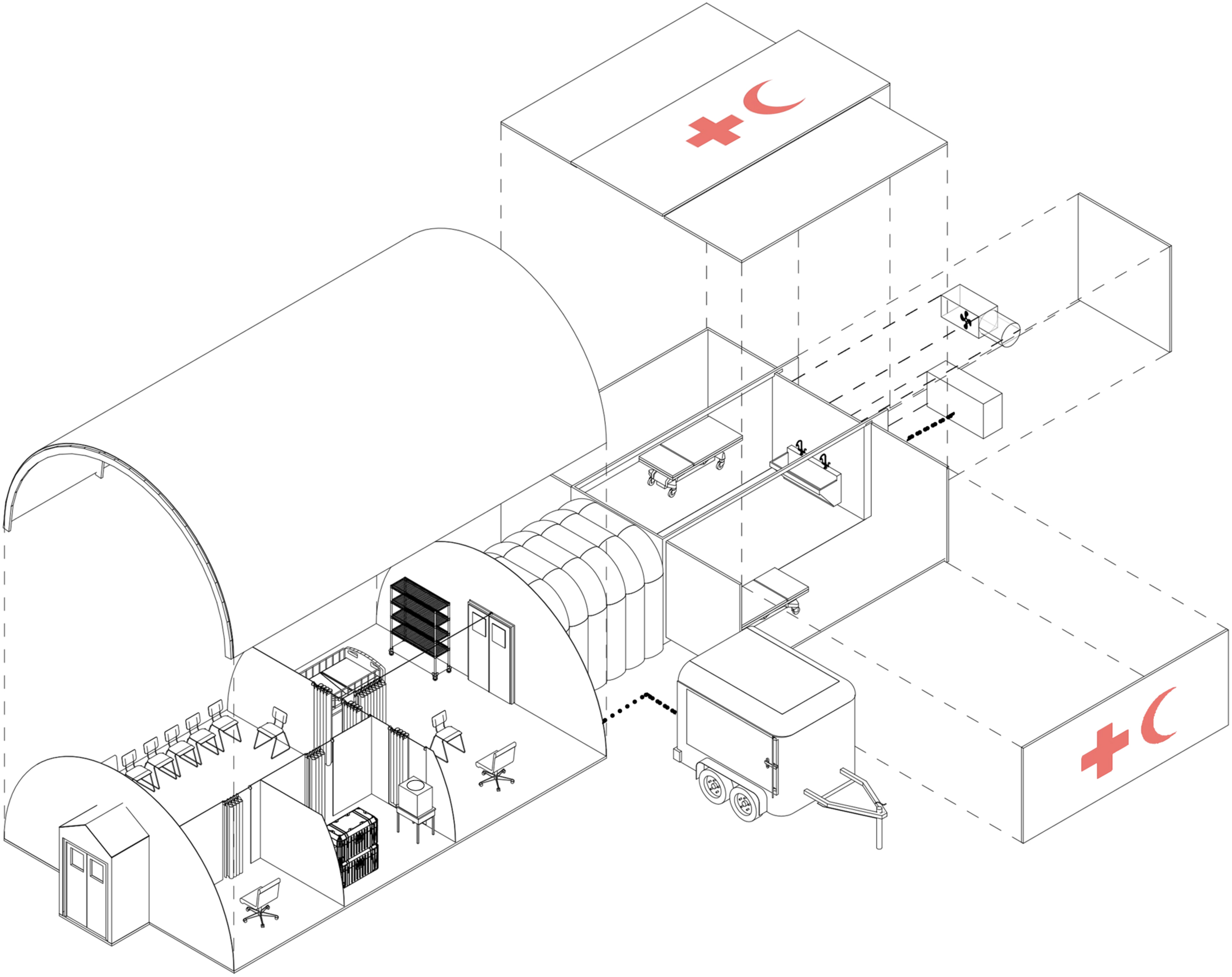
Figure 2. Mobile eye hospital. Axonometric projection including combination of layout for either clinic or surgery days.
Curtains can be attached to the aluminum frame of the field tent, splitting the interior into defined areas. The field tent and container both contain an easy to clean nonslip vinyl floor, with an option for a sub-flooring system on uneven ground. To ensure the operating area remains sterile, a positive pressure airflow system and air handling unit with high-efficiency particulate air (HEPA) and UV germicidal filtration system is incorporated into a plant room within the shipping container. 29–31 Entry to the operating area is by means of a twin air curtain to isolate the sterile environment. The plant room also contains a small back-up generator should the main generator fail, ensuring that at a minimum, operating microscopes, sterilizers, and lights remain working. The main generator and heating, ventilation, and air conditioning (HVAC) unit are neatly housed within the trailer, supplying electricity and temperature control to the field tent and shipping container. If local power is available, voltage regulators are indicated.
Adaptability
The internal area can be easily reorganized dependent on the mission requirements. During clinic days, where there is a need to screen a large number of patients, the field tent can be organized into 3 exam rooms with the operating area re-purposed to handle minor operations and the option to black out a single room for laser treatment (eg, pan-retinal photocoagulation for the treatment of diabetic retinopathy) (Figure 3). At a minimum, examination equipment should include visual acuity charts, a portable slit lamp, indirect ophthalmoscope, tonometer, fundus lenses, compact A/B ultrasound scanner, autorefractor, sphygmomanometer, and expendable supplies such as eye drops and reagent for estimating urine sugar. Additional equipment that may be considered include a portable optical coherence tomography (OCT) scanner for detailed imaging for the ocular fundus, and an automated visual field tester. Many patients will require refractive correction and missions should be equipped with ample supplies of spectacles. The addition of a tabletop automatic lens edger may also be considered. In addition to a satellite Internet connection, it is important to include a way of storing electronic medical data (eg, secure laptop), both to keep an accurate record of patients and also to make it easier to transfer records back to local health authorities.
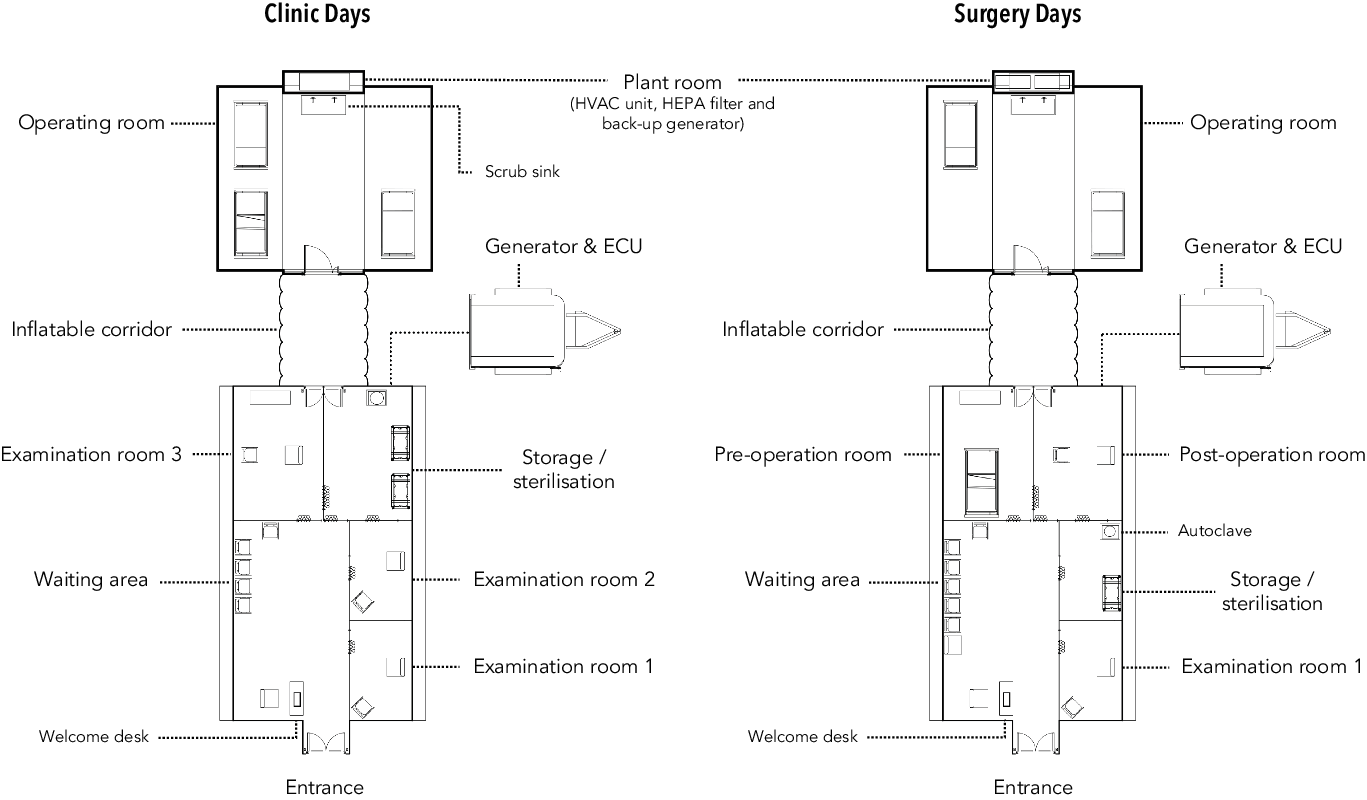
Figure 3. Floor plan of optional layouts for a mobile eye hospital. Heating, ventilation, and air conditioning (HVAC); high-efficiency particulate air (HEPA); environmental control unit (ECU).
The internal area can also be organized for high-volume surgery (Figure 3). When running a surgical day for the treatment of cataracts the internal structure may include: a waiting area where an ophthalmic assistant can perform an initial assessment; an exam room for detailed assessment including biometry to calculate appropriate IOL strength; a preoperative area where the patient can be prepared (eg, administration of dilating drops, local anesthetic); an operating area with scrub basin, 2 beds, operating microscope, surgical instruments, consumables, and an automated vitrectomy machine on standby; a postoperative area adjacent to the preoperative area (separated by a privacy curtain) where the patient can have any additional surgical dressings applied and receive appropriate information on drop regimen and further management before discharge; and a storage and sterilization room, including a tabletop autoclave for surgical instruments. The storage room should also include disinfectant, with the operating room space thoroughly cleaned at the beginning and end of each day.
Personnel and Logistics
Assembly of the mobile eye hospital requires minimal personnel, with the majority of assembly managed by a single person and only 4 people needed to erect the field tent. Additionally, a small team of well-trained ophthalmologists, ophthalmic assistants and nurses can operate the hospital. It should be noted that as the majority of cataract operations (and other ophthalmic procedures) are performed under local anesthetic, it may be unnecessary to include an anesthetist in the team. Instead, ophthalmologists must be trained in basic and advanced life support with guidance from intensive care specialists and anesthetists to identify warning signs and understand acute management of emergencies, including resuscitation. The operating room should be equipped with essential emergency equipment, including airway and breathing equipment, intravenous and intraosseous access, and essential medicines including intravenous fluids and antibiotics.
In a disaster area, it is crucial that a foreign field hospital does not pose a burden on an already struggling health system and should attempt to be as self-sufficient as possible, including provision of food, water, security, and medical waste disposal. Sending a preliminary needs assessment team to a location can greatly enhance the logistic preparation by contracting vehicles, locating water, food, accommodation, and liaising with local translators and security forces. Reference Naor, Heyman and Bader8 If water is not locally available, it may be necessary to include a water treatment unit or water storage (eg, bladder) that can be transported to the site by means of the truck following the unloading and deployment phase.
Conclusions
Following a sudden-onset disaster, complex humanitarian event, or conflict in a resource-scarce environment, there is a need to provide a semi-permanent service between the initial emergency response and the reestablishment of local health service delivery. This study proposes a mobile eye hospital with high mobility and modularity that can be assembled and operated with a minimal crew and easily expanded if needed. The mobile eye hospital provides capability for screening and treating the most common causes of vision loss and may be a useful investment for local governments suffering damaged health systems during the medium-term recovery phase. The design may also be used to complement current eye health provision in resource-scarce environments, offering a mobile surgical solution to reach patients in more rural and inaccessible areas. It may also be used by charitable nongovernmental organizations (NGOs) during an initial emergency response to provide immediate eye care, with the option to either deploy to another location or remain in-country and help with the transition back to local governance as infrastructure and human resources are rebuilt.
Acknowledgment
We thank Benjamin Bryan, former Royal Navy Officer and architecture student, for the design and production of the figures.
Conflicts of Interest
The author has no conflicts of interest to declare.







