Introduction
There is an increasing consumption of raw milk in many countries and increasing scientific evidence that raw milk can reduce asthma, allergies and atopic eczema [Reference Brick1, Reference Heckman2]. Furthermore, early life consumption of raw cow's milk has been shown to reduce the risk of manifest respiratory infections and fever by about 30% [Reference Loss3]. When raw farm milk is boiled, even farm children, who are the best protected group of children worldwide, showed increased incidence of asthma, hay fever and atopic diseases [Reference Loss4]. Mice studies show that heating milk at 80 °C for 10 min induced asthma, whereas mice that consumed unheated milk did not show any signs of asthma, and the destruction of heat-sensitive components such as alkaline phosphatase, and several whey proteins are involved [Reference Abbring5, Reference Abbring6]. A human proof-of-concept provocation pilot study in milk allergic children has further shown that milk processing (pasteurisation plus homogenisation) increases the allergenicity of cow's milk [Reference Abbring7]. It has been estimated that 334 million people world-wide are suffering from asthma that are reducing the quality of life, reducing health, increasing mortality and has a huge financial burden mainly due to productivity loss [8]. Global estimates show an increasing trend in the last 10 years (2007–2017) in both asthma and atopic dermatitis [9]. Furthermore, adult consumers perceive various health benefits when introducing raw milk or raw fermented milk into their diets [Reference Baars10, Reference Baars11].
Pasteurisation requirements for raw milk arose in the early 20th century when the hygienic quality of milk could not be assured, and tuberculosis and brucellosis were major public health threats. At the time, when urban populations were exploding, leading to either transport of pooled uncooled milk into the cities, or urban farms where swill feeding was common, milk-associated diseases were very common [Reference Atkins, Smith and Phillips12]. Pasteurisation plants were built, and many of the milk-associated outbreaks decreased. However, at that time there were several initiatives focusing on increased hygienic production of raw milk in the United States, United Kingdom and Denmark, but these disappeared over time [Reference Barnett, Smith and Phillips13]. Lady Eve Balfour, founder of the Organic Movement and Soil Association in the UK stated that ‘pasteurisation was a confession of failure. The aim should be to abandon the practice just as soon as the need for it – unhealthy cows and dirty methods – can be eliminated' [Reference Atkins, Smith and Phillips12]. Since raw milk for direct consumption has not been promoted or supported by regulatory food safety authorities over the last 70 years, there has been no training available for raw milk producers regarding systems for hygienic and safe raw milk productions. Therefore, most outbreaks associated with raw milk are associated with dairy farms that have not received specific training in hazard reduction and hygienic milking procedures. Several generations of farmers have now become used to the system where bulk tank milk is pasteurised, and there is no direct link between the producer and the consumers. Thereby sub-optimal hygienic practices have unfortunately over time become established. A recent survey in the UK indicated that pathogens and indicators of poor hygiene were present in almost half of the samples of raw milk intended for direct consumption and 25% of samples had non-acceptable indicator bacteria levels [Reference Willis14].
The current hazards associated with raw milk are mostly due to the faecal contamination of the milk with enteric bacteria such as Salmonella enterica, Campylobacter spp., verotoxin-producing Escherichia coli. Microbial hazards such as Listeria monocytogenes, Yersinia spp., Coxiella burnetii, Brucella spp. and Mycobacterium spp. can vary regionally and spatially [15]. Although national outbreak data can report these risks, the outbreak data are not a good source to quantify the risks. Data are incomplete as only a small percentage of all foodborne disease outbreaks are reported each year. In addition, raw milk-associated outbreaks are subject to a detection bias, because it is easier to trace an outbreak back to a niche commodity actively sought by few consumers (such as raw dairy products) than to commodities consumed by a large portion of the population such as pasteurised dairy products. This also leads to a reporting bias, since an investigation that leads to the detection of the source of the risk is much more likely to be reported and published. Another challenge with determining risks based upon reports from outbreaks is that outbreak investigations rarely estimate the denominator of an attack rate (including the number exposed, both ill and healthy). Furthermore, reliable data on levels of ingested pathogens in a certain food matrix causing and not causing illness or severe illness are crucial for estimating risk. A systematic review performed in 2008 by Massey University in New Zealand concluded that there were lacking well-defined studies to characterise the risks of raw milk using a meta-analysis [Reference Jaros, Cogger and French16]. After studying the hazards of raw milk, the European Food Safety Authority (EFSA) similarly concluded that that outbreak data are insufficient for risk evaluation [15].
Despite the inadequacy of the outbreak data, public policy and risk management is often based on outbreaks. A 12-year longitudinal analysis using a recent analysis of outbreak data in relation to raw milk consumption indicates that outbreak rates in the USA have declined from 2010 to 2016, while legalisation and consumption increased [Reference Whitehead and Lake17]. This was, according to the authors, attributed to the increased awareness and attention to milk hygiene and safety in production in North America. There are dedicated raw milk producers that have become highly qualified and methodical in the production of hygienically produced safe raw milk and organisations are developing to assist raw milk producers.
The European Union legislation has laid down basic microbiological criteria for general raw milk production that involves no detection of common pathogens in defined sample quantities, standard plate counts (SPC) <50 000/ml and coliform counts <100/ml [18, 19]. There are indications that the hygienic indicator bacteria levels set may be insufficient to be protective from microbiological hazards, as was demonstrated in a survey of raw milk-associated outbreaks in the UK, where the SPC limits were not associated with the presence of pathogens [Reference Willis14].
There are numerous foods that present a microbial hazard to consumers, and food production systems using good manufacturing practices (GMP) and hazard analysis critical control points (HACCP) have been developed. These food safety systems have been applied on raw milk dairies. These practices include biosecurity, herd health management, hygienic milking routines, closed mechanical milking systems, rapid cooling, cold chains, refrigeration and quality controls. There are an increasing number of producers that develop on-farm microbiological testing programmes for their raw milk, where the raw milk is only sold when acceptable results of the hygienic monitors are fulfilled. Furthermore, there are several disease control programmes that apply on national or industry levels that focus on reducing the spread of potential zoonotic agents such as Mycobacterium spp., Brucella spp., S. enterica, Campylobacter spp. These programmes involve testing to determine farm-level disease status, biosecurity measures and trade restrictions in case of disease agent findings on the farms. HACCP-based systems combined with GMP have been implemented in virtually all agricultural and food processing sectors worldwide as the basis for producing safe food. Hygienic production, harvesting and storage techniques have become obligatory standards for many products, including those intended for possible raw consumption such as meat, eggs, fruits, vegetables and nuts. The only food commodity that is still subject to an obligatory pasteurisation requirement in many countries is raw milk, despite evidence that raw milk can be safe using the same food safety principles. It has therefore been recommended that ‘studies of the role of on-farm food safety programs to promote the further reduction of unpasteurised milk outbreaks should be initiated, to investigate the efficacy of such risk management tools' [Reference Whitehead and Lake17]. The aim of this paper is to present the components and results from industry-initiated programmes and one federal programme to assure a high level of safety of raw milk for direct consumption. Some further developments and initiatives in Europe are briefly discussed.
Vorzugsmilch (Germany) – the preferred milk
German Vorzugsmilch (VZM) (bevorzugen means ‘to prefer’) is a federally regulated raw milk intended for direct consumption that has been produced as such since the 1930s [20]. It is subjected to high requirements as regards milking hygiene, handling, packaging and transport. Farms that produce VZM are initially inspected and approved by the federal veterinary services. The VZM programme previously made it possible to deliver raw milk to retirement homes, schools and hospitals. Since the EHEC crisis in 1989, raw milk sales to these institutions was prohibited, and many VZM farmers stopped, despite that there were no EHEC cases linked to VZM or raw milk in Germany when this prohibition was introduced. In 2018, around only 1100 tonnes raw milk is sold by 13 VZM farms in Germany and most of these farmers combine the labelling of raw milk with the organic labelling.
There are monthly farm visits by the local veterinary health service where cow health is controlled, single cow milk samples are taken and one bottle of fresh VZM is taken for laboratory control. The milk control is based on hygienic handling (SPC, coliform counts), udder health (somatic cell count, Staphylococcus aureus) and zoonotic risks (Campylobacter spp., enterohemorrhagic E. coli/verotoxin producing E. coli (EHEC/VTEC), L. monocytogenes and Salmonella spp.). Based on local conditions additional zoonotic pathogens, such as Mycobacterium bovis in alpine regions where wildlife tuberculosis may be present, may be controlled by the inspecting veterinarian. The standards for the sales of VZM are strict and the Government reduced the limit values for hygiene parameters in 2007. The laboratory microbial control system is based on warning values (m) and upper limit values (M) [21]. Exceeding the upper limit M will immediately ban raw milk delivery and recall milk sold or delivered. Only after the implementation of operational corrective measures and follow-up examinations within the acceptable range can raw milk sales restart. The strict test criteria for VZM and the necessary follow-up examinations usually result in quick elimination of errors and deficiencies.
The bacteriological results from 1172 milk samples from 15 farms were collected in the period 2001–2015 and were analysed (Table 1, Fig. 1a and b). The results of pathogen testing of food samples are published yearly by the German Federal Institute for Risk Assessment (BfR) [22]. The annual data from of analysis for the major milk zoonotic pathogens in milk from 2001 to 2015 of VZM dairies, samples of raw milk taken at the creameries, samples taken on conventional dairy farms from the bulk tank and samples of pasteurised milk from shops were reviewed (Table 2). As can be noted from Table 2, the VZM dairies have lower prevalence of pathogens than raw milk collected in creameries and from bulk tanks on other dairy farms. Bulk tank milk samples from these VZM farms for zoonotic bacteria detection are not significantly different from the samples of pasteurised milk, except for L. monocytogenes (tested with stratified analysis and Fisher's exact tests). These results show that hygiene management at VZM farms reaches a zoonotic risk level comparable to pasteurised milk. It should be noted that pasteurised milk, which has undergone a heat treatment to achieve at least a 5 log 10 reduction of Coxiella burnetii (according to the Codex Alimentarius Code of Hygienic Practice for Milk), is not guaranteeing eliminations of pathogens (such as S. enterica, L. monocytogenes, verotoxin-producing E. coli and Yersinia enterocolitica). Thus, it may not be reasonable to expect 100% safety in raw milk when even pasteurised milk is not 100% safe [Reference Whitehead and Lake17]. The yearbooks of BfR describe the food-related outbreaks in Germany. Data could be extracted from 2006 to 2017 and during these years there were 7120 foodborne outbreaks, of which 6.4% (457 outbreaks) were related to all types of milk products. In this period, only one recall of VZM occurred when school children got sick in campylobacteriosis following a visit to a VZM farm in the State Hesse.
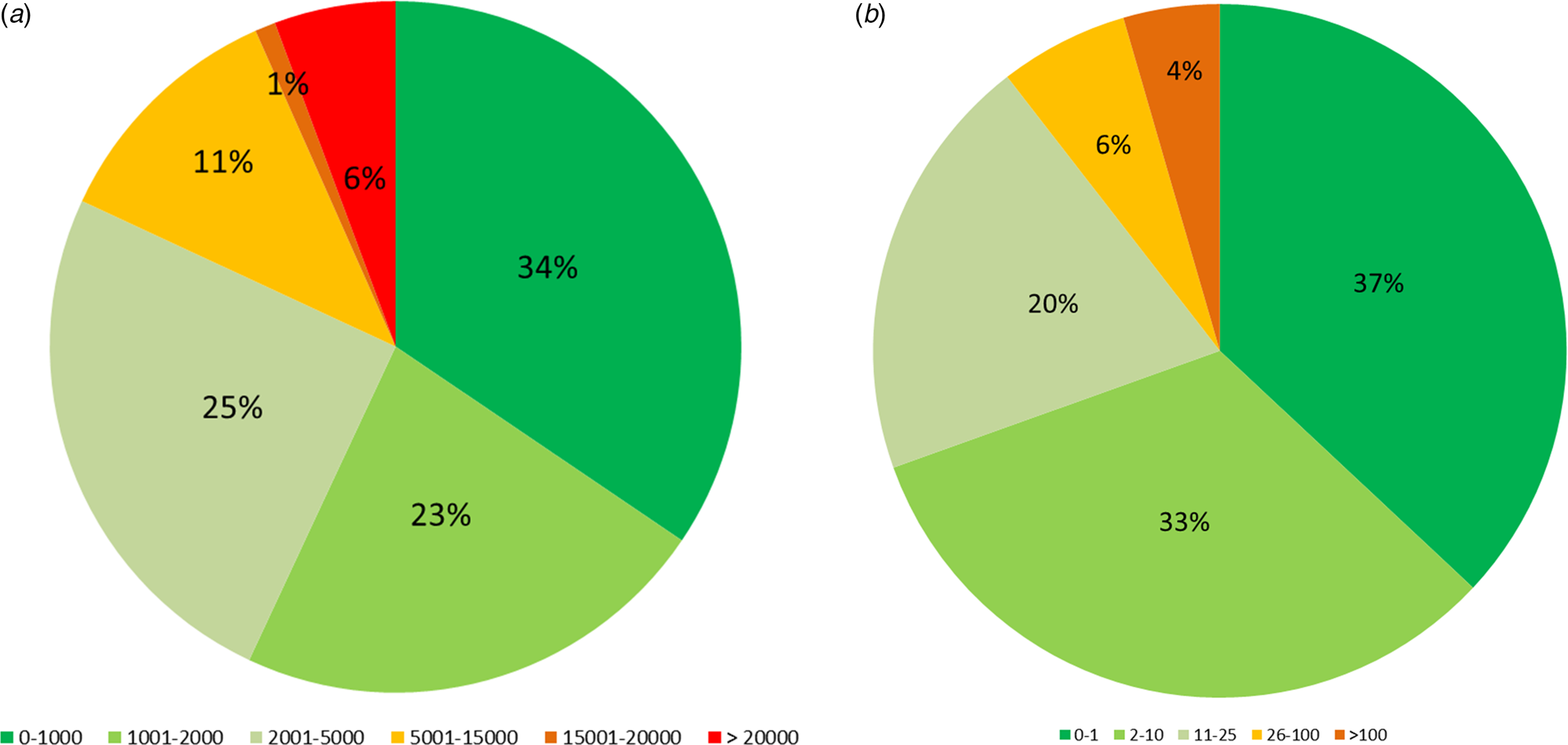
Fig. 1. Results from 15 VZM dairies for monthly indicator bacteria samples analysed in 2001–2015: SPC (a) and coliform counts (b) per ml milk.
Table 1. Results from the monthly control data from VZM dairies in Germany, Raw Milk Institute listed dairies in North America and British Colombia herdshare dairies in Canada

a The coliform limits were reduced in 2007.
b The SPC limits were reduced 2007.
Table 2. The major zoonotic enteric bacteria found in routine milk samples performed by Robert Koch Institute (2001–2015) of VZM, raw milk at creameries, bulk tank milk on conventional dairies and pasteurised milk

a Pos. = the number of positive samples; N = the total number of samples analysed.
b Verotoxin. E. coli = verotoxin-producing Escherichia coli.
The Raw Milk Institute (USA) – an industry-initiated programme
The Raw Milk Institute is a non-profit corporation founded in California in 2011, initiated by the raw milk industry [23]. The need for an organisation to teach farmers how to produce safe raw milk was triggered by regular raw milk-associated zoonotic disease outbreaks reported. The mission of the institute is to teach farmers how to produce safe raw milk and create a system of listing farmers that had complied with the institute's safe production system and standards in order to provide consumers with a safe raw milk source. Due to the varying structure, size and goals of raw milk producers, the institute developed a system, where every farm interested in raw milk quality and safety, after guidance and information, develop their own risk analysis and management system, with guidance and approval of the institute. Biosecurity and management systems were set up to reduce the introduction of potentially zoonotic agents onto the farm and to reduce the spread of zoonotic agents within the farm. The institute emphasised the importance of hygienic milking systems, and farms have developed their standard operating procedures in milking, chilling and bottling to reduce the risk of faecal contamination during milking and rapid cooling of the milk to reduce the bacterial growth. Many producers are small herd-share farmers or family farmers, and this made it financially difficult to require expensive pathogen testing on a regular basis. A system of at least monthly control of milk bacterial indicators (coliform bacteria and total aerobic plate count or SPC) in accredited laboratories was set up to monitor the general hygienic milking practices.
Several farmers have gone beyond the minimum requirements and perform more frequent controls of hygiene indicators and regular pathogen testing of the milk. Some farmers have developed ‘Test-and-Hold’ milk controls, where the milk is checked daily for coliform bacteria and SPC in their own bench-top laboratories using Petri film plates developed for many food industry internal control systems. In these ‘Test-and-Hold’ systems the milk is not sold prior to having checked that the hygienic indicator bacteria are within desired control ranges. Benchmark values for the indicator bacteria are far below the current European Union minimum levels. The current benchmark values for raw milk samples are that coliform counts should be ⩽10 (similar to VZM) and SPC should be ⩽5000 (lower than VZM). RAWMI-listed farmers consistently achieve coliform counts that are lower than the requirements for post-pasteurised milk [Reference Marshall24], and extremely low SPC. There are 18 listed RAWMI farms (of which 14 are currently active) with an average annual production of 6900 tons of milk and the farm average coliform counts are 2.9 cfu/ml, and SPC of 1693 cfu/ml milk (Table 1). To date only 4% of monthly samples exceed the benchmark value of 10 coliforms/ml and 4% exceed the benchmark of SPC >5000 cfu/ml (Fig. 2a and b). All coliform results are well below the EU standards of coliforms ⩽100 cfu/ml and 96% are at or below the U.S. standard of coliforms ⩽10 cfu/ml for post-pasteurised milk [Reference Marshall24]. Furthermore the SPC of RAWMI listed dairies are well below the limits for pasteurised milk at 20 000 cfu/ml [Reference Alvarez, Clark, Drake and Bodyfelt25]. The RAWMI programme has inspired many other non-listed raw milk producers to adopt a similar production and hygiene approach [Reference Whitehead and Lake17].

Fig. 2a. Results from 18 dairies listed by the Raw Milk Institute for monthly indicator bacteria samples analysed in 2012–2019: SPC (a) and coliform counts (b) per ml milk.
British Columbia Herdshare Association
In Canada there is a complete prohibition for sale of raw milk for direct consumption. Herdshares are also prohibited but still exist in several areas of Canada. Herdshares are contractual arrangement between farmers and shareholders in the herd, where the shareholder is able to obtain raw milk and other products from the farmer proportionate to the shareholder's interest in the herd. The British Columbia Herdshare Association is a legally-incorporated non-profit society that has been developing on farm food safety plans [26]. There are 10 producers that have been part of the programme. Samples of raw milk are regularly collected by the farmer and sent to an accredited laboratory (MB Laboratories in Sidney) for analysis of hygiene indicators and major pathogenic bacteria. The results have been collected and shared on their website [26]. The results indicate a similar level of hygiene to the RAWMI listed dairies with 93% of all samples with milk coliform counts of 10 cfu/ml or less, and 92% of all SPC were below 5000 cfu/ml (Table 1). All samples tested negative for the four main pathogenic bacteria (VTEC, Salmonella spp., Campylobacter spp. and L. monocytogenes) associated with raw milk (Table 1). These herdshares are hoping that their track record of microbial safety can help to alleviate the Canadian ban on herd shares.
Other raw milk movements in Europe
In the UK there has been an increase in fluid raw milk producers. The UK authorities were concerned, as this led to an increased number of raw milk-associated disease outbreaks in the country [Reference Willis14]. This has led to the establishment of a new organisation called the Raw Milk Producers Association (RMPA) in 2019 [27]. This organisation has as goal to assist dairy farmers to produce and sell safe raw milk, and the RMPA has been working closely together with the UK food safety authorities to assure the safety of raw milk and a good relationship between producers, inspectors and regulators. The organisation has already performed whole day workshops (with the authors of this paper and FSA inspectors), and prepared newsletters including important information regarding potential hazards and mitigation measures.
Safety components of existing raw milk production systems
High quality safe raw milk is directly linked to healthy animals and extreme attention to hygiene. Good farmer's training and support programmes are very important in order to assist the dairy producer to understand the various risks in milk production and the measures needed to mitigate the risks. Such raw milk training programmes performed by undersigned authors have led to improvement of the milk quality and management around milking hygiene. Bacteria in raw milk comes from a few main sources; udder, teat canal, skin, manure, environment, milking equipment, pipelines, tanks and bottles. The bacterial contaminants of these sources differ and require targeted control strategies. Actions to reduce the likelihood of contamination of raw milk are essential and must be practiced daily to assure the consistent safety of the product. Biosecurity is a very important part of safe raw milk as it can reduce the introduction of potential zoonotic pathogens into the farm and prevent the spread of potential pathogens that might be present on the farm. Biosecurity can also reduce the introduction and spread within the farm of animal pathogens that can reduce the immunity of the animals and increase the likelihood that the animals will shed potential zoonotic pathogens. Feed management and environment management need to assure that the animals are subjected to minimal stress and that the husbandry and feed ensures that all the needs of the animals are met in order to assure stress-free healthy producing dairy cows. Feed and water should not be microbially contaminated. A very good system of verification of practices with documentation and review is necessary to quickly identify potential weak areas in production that can be a risk to consumers.
Discussion and conclusions
There is a global interest in raw milk that is many times coupled to more traditional forms of food production, a closeness to the producer, a minimally processed food and to the health benefits of raw milk and products thereof. Many consumers are concerned about both production animal health and human health. They are also interested in the nutrition and hazards associated with the food choices they make. Since consumers cannot evaluate the safety of raw milk based on the organoleptic qualities (taste, look and smell), they must trust the food safety procedures of the farmer and any other processor or retailer involved. Consumers need to be able to source raw milk from farmers that have adopted a high level of good animal husbandry practices and manufacturing practices that can reduce potential food safety hazards to very low levels. A strict testing system regarding bacteriological quality of raw milk including indicator bacteria and potential pathogen testing can verify production system safety. However, the testing without a good raw milk hygiene system is not a guarantee for safety of raw milk. There have been several risk assessments performed in Italy where the microbial quality of the raw milk in vending machines has been monitored, and these have indicated higher health risks from these vending machines than what may be expected from the systems described in this paper [Reference Giacometti28–Reference Giacometti30]. This safety of raw milk is assured through the farm biosecurity, the good husbandry practices, GMP, distribution systems and ultimately consumer handling. The Farmhouse and Artisan Cheese and Dairy Producers network in Europe has been increasing their focus on raw drinking milk. Eldrimner, Sweden's resource centre for artisan food is likewise working hard to enable small producers to market raw milk and products thereof. The European College of Veterinary Public Health (ECVPH) has also recognised that it needs to deal with the current raw milk market, since the modern-day consumer fights hard for the rights to seek out nutritious raw foods. The ECVPH had a keynote half a day presentation at their annual meeting in Perugia, Italy in 2018, which provided a good discussion on the safety and benefits of raw milk.
Today's food safety approaches can not only include minimal risks from foodborne pathogens, but it must also embrace immunological or microbiome diversity benefits of food commodities when determining hygienic safety management approaches. This approach has been deemed appropriate in many other sectors of food production, where ‘new metrics, such as performance objectives that are linked to human health outcomes, should be utilised throughout the food chain to help define risk and identify ways to reduce adverse effects on public health' [Reference Mead31]. This overview has shown that various practices and systems to assist dairy producers to create a safe food commodity are present that are using similar food safety approaches that have been successfully used for other foods. The programmes described indicates that good biosecurity, animal management, hygienic milking techniques, quick cooling and thereafter a good cold chain can provide hygienic and safe raw milk, similarly to other raw foods. Furthermore, regular microbiological controls of the raw milk can continually evaluate the systems. Safe and hygienic raw milk can be accomplished in various dairy farm systems ranging from small family cow systems to very large dairies with state-of-the-art equipment.
The World Health Organisation has laid down the components of a healthy diet including sufficiency of nutrients and energy, with nutrient-dense food of high quality with minimal processing or additives and that are safe to consume [32]. The concept of zero risks from potential pathogens in raw milk need to be weighed against the benefits from raw milk to reduce the rise in allergies and other chronic conditions. Many published papers are not aware of the increasing evidence of the raw milk benefits, and only warn for the risk of general raw milk consumption. However, the consumption of raw milk should be based on systems described in this paper, where risk has been strongly reduced, and the balance of risks and benefits should be based on recent literature.
Despite that many published papers describe that risks exceed benefits for raw milk, none have conducted a well-designed analysis that well quantifies the risks. Furthermore, no papers have previously described the risks associated with dedicated raw milk production systems using the hygienic production systems described in this paper. The benefits have furthermore been disregarded and discredited by many food safety experts that do not fully grasp the hazards of an unhealthy diet as well as the potential microbial hazards.
Risk benefit analysis is needed where risks and benefits are measured according to the same health metrics such as disability-adjusted life years (DALYs) or quality-adjusted life years (QALYs) [33]. DALYs sum years of life lost due to premature mortality and years lived in disability/disease whereas a QALY is the arithmetic product of life expectancy combined with a measure of the quality of life-years remaining. These measures do not fully capture socio-economic consequences and emotional or mental health impacts, but they do attempt to quantify the impact of many non-communicable diseases that may be associated with nutritional choices, such as raw milk. It would be of value to differentiate production systems for raw milk in future risk analysis and risk-benefit analysis, as there are increasing number of producers that have received special training in safe and hygienic raw milk production. Consumers of today are placing increasing emphasis on freedom of choice as regards their food, as regards animal welfare, ethics, production systems and origin and processing. Regulatory systems need to continue to work together with the food production industry including artisanal production and the consumers to provide a safe and nutritious food supply.
In conclusion, this paper has described systems that have been developed to reduce potential microbial zoonotic hazards of raw milk. Microbial sampling from these systems indicates that raw milk can be produced with a high level of hygiene and safety.
Acknowledgements
The authors wish to thank contributing farmers and organizations for providing data.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None. TB is an advisor of the German Vorzugsmilch producers.






