No CrossRef data available.
Article contents
Alterations in brain myelination at early-stage schizophrenia detected by macromolecular proton fraction MRI
Published online by Cambridge University Press: 19 July 2023
Abstract
There is evidence that cerebral myelination is impaired in schizophrenia. The purpose of this study is to find the myelin content changes in the brain structures of patients with early-stage schizophrenia using the macromolecular proton fraction (MPF) method, and also to evaluate the differences in the myelination of these structures.
To measure MPF in the brain structures of schizophrenia patients
Forty-five subjects, 22 controls (10m+12f, 31.6±9.7 y.o.) and 23 schizophrenia patients (F20.0, 11m+12f, 31.5±5.1 y.o.). Philips Achieva dStream 3T MRI scanner, standard head coil. The magnetization transfer (TR=20 ms, TE=4.60 ms, FA=10°), T1-weighted (TR=20 ms, TE=4.60 ms, FA=20°) and PD-weighted (TR=20 ms, TE=4.60 ms, FA=4°) were acquired. The MPF maps were reconstructed using home-made software. In FSL, non-brain structures were removed and MPF maps were registered to a standard MNI152 1 mm atlas. Harvard Oxford Cortical and Subcortical atlases were used to select areas of interest. T-test was used in search for between-group differences.
A 3% decrease in myelination in schizophrenia was observed in whole cerebral cortex p = 0.03) and cerebral white matter (p=0.02). Trends to cortical demyelination were found: paracingular cortex (p=0.06), anterior (p=0.1) and posterior cingulate cortex (p=0.07). No myelination disorders were detected in the cerebellum.
Image:
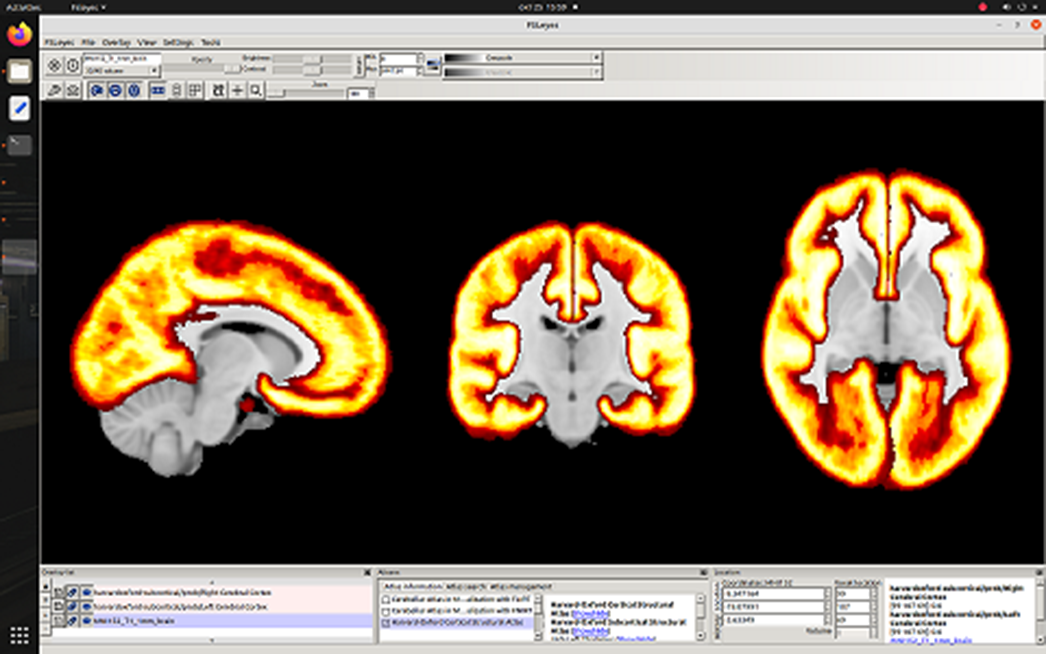
Image 2:
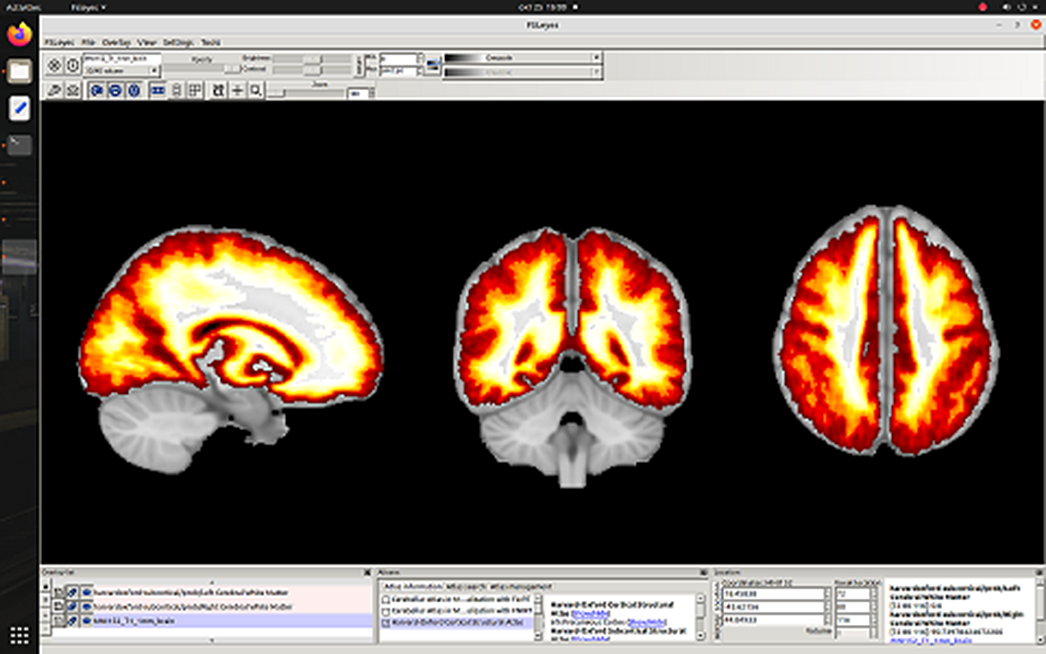
Image 3:
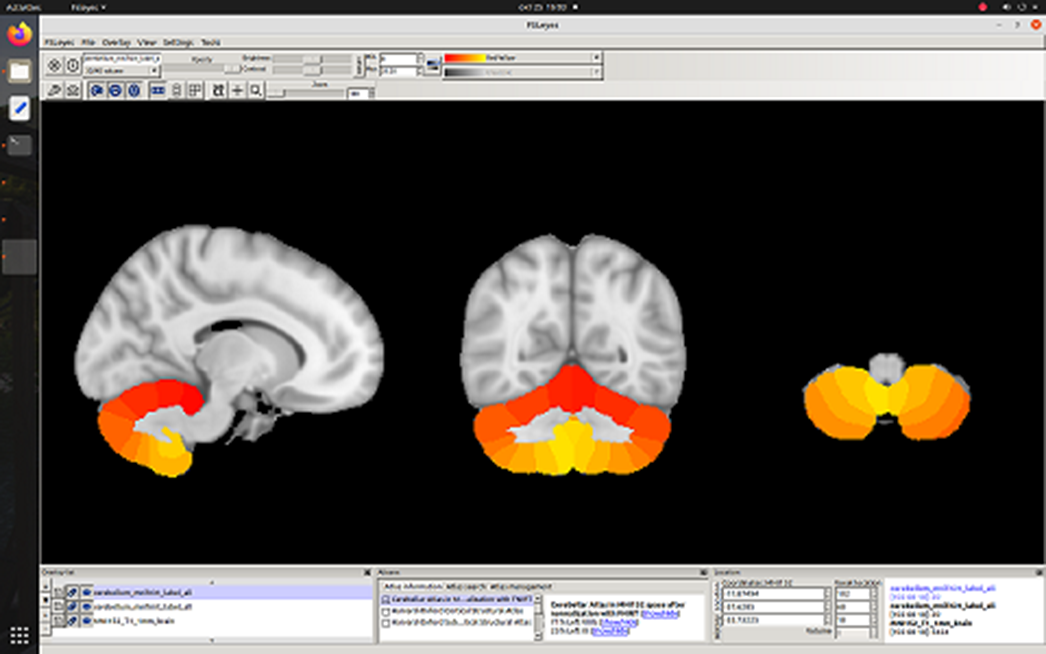
To our knowledge, the absence of cerebellar myelination disorders in patients at an early-stage schizophrenia is reported for the first time, while the observed decrease in cerebrum myelination in schizophrenia is consistent with the previous findings. The difference in myelination between cerebellum and cerebrum may help to characterize the dynamics of the pathological process and provide additional information for understanding the biological mechanisms of the development of schizophrenia.
Grant RSF 20-15-00299 (partially).
None Declared
- Type
- Abstract
- Information
- European Psychiatry , Volume 66 , Special Issue S1: Abstracts of the 31st European Congress of Psychiatry , March 2023 , pp. S134 - S135
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2023. Published by Cambridge University Press on behalf of the European Psychiatric Association





Comments
No Comments have been published for this article.