1. Introduction
Recruitment and retention in psychiatry have been two issues of major concern in recent decades. While negative perception of psychiatry may discourage medical graduates from entering the field [Reference Farooq, Lydall, Malik, Ndetei, ISOSCCIP Group and Bhugra1,Reference Goldacre, Fazel, Smith and Lambert2], reports from doctors leaving psychiatry have indicated reasons such as high numbers of challenging patients, depressing work conditions, job stress and low morale among staff [Reference Lambert, Turner, Fazel and Goldacre3]. With shortage of qualified psychiatrists, most countries today cannot afford to lose trainees for reasons such as poor training conditions and development of work-related burnout. However, very little is known regarding burnout rates, or indeed factors influencing burnout syndrome among psychiatric trainees.
Work-related burnout syndrome is characterised by a triad of emotional exhaustion, cynicism, and low sense of professional efficacy [Reference Maslach, Jackson and Leiter4]. It has been associated with impaired patient care [Reference Demerouti, Bakker and Leiter5], reduced learning capacity [Reference Girard and Hickam6], stress-related health problems [Reference Maslach, Schaufeli and Leiter7], and broken personal relationships [Reference Shanafelt, Sloan and Habermann8]. Medical doctors experience higher rates of burnout syndrome than the general population [Reference Shanafelt, Boone and Tan9]. Persistent imbalance between demands and resources seems to be a crucial contributor to development of burnout. Training years, more than any other stage in physicians’ career, are characterised by this type of imbalance due to long and irregular work hours [Reference Martini, Arfken and Balon10] and high levels of responsibility combined with lack of professional experience [Reference Burnout, Firth-Cozens and Payne11]. Psychiatry itself adds several very specific stressors such as perceived stigma of this profession, demanding therapeutic relationships, personal threats from violent patients and patient suicide [Reference Rössler12].
The reported burnout rates among medical trainees vary from 27% to 75%, depending on specialty, country and methods [Reference Prins, Gazendam-Donofrio, Tubben, van der Heijden, van de Wiel and Hoekstra-Weebers13,Reference Thomas14]. A small number of studies explored this issue among psychiatric trainees. A national multi-specialty study from Netherlands included 242 psychiatric trainees [Reference Prins, Hoekstra-Weebers and Gazendam-Donofrio15]. Reported burnout rates of 23.2% were higher than for the whole sample (21%). This was the only extant study that analysed the role of psychiatric training conditions in this context. The authors reported that trainees who worked with chronically-ill patients were more emotionally exhausted than others. Similarly, an US study found that psychiatric trainees (n = 11) reported higher levels of emotional exhaustion than trainees from other specialties [Reference Afzal, Khan, Mulla, Akins, Ledger and Giordano16]. Martini et al. compared US trainees from eight different specialties and with a sample of 15 psychiatric trainees found that 40% met criteria for burnout, while the rate was 50% for the whole sample [Reference Martini, Arfken, Churchill and Balon17]. Several other studies included rather small subsamples of psychiatric trainees that were merged with trainees from other specialities, without reporting burnout rates or risk factors specifically for psychiatric trainees [18–Reference Zis, Anagnostopoulos and Sykioti21]. Studies in other disciplines indicated that occupational factors such as excessive workload, high degree of work-home interference, and perception of work as stressful, were strongly correlated with burnout syndrome [Reference Prins, Gazendam-Donofrio, Tubben, van der Heijden, van de Wiel and Hoekstra-Weebers13,Reference Thomas14]. Individual factors such as neuroticism and being unmarried were also found to be associated with burnout, but these associations were weak. Overall, there is a lack of evidence regarding burnout rates and factors influencing burnout among psychiatric trainees.
Thus, the aim of this study was to assess burnout rates among psychiatric trainees, and explore which individual, educational and work-related factors are associated with severe burnout.
2. Methods
The study was created by a group of European trainees involved as national representatives in the European Federation of Psychiatric Trainees and early career psychiatrists involved with the European Psychiatric Association. The driving force behind the study was a shared awareness of the impact of burnout on service provision, and of the challenges for retention and recruitment in psychiatry.
2.1 Study protocol
This is a cross-sectional, multicountry, online survey in which participants were sent e-mail invitations to participate in the study by entering data via an online questionnaire directly into an anonymised, encrypted, secure database. While planning the study, we explored available avenues to access trainees’ e-mail contacts. In the majority of countries (n = 15) all trainees were invited to participate in the study. If centralised database of trainees was not available, other options were considered. In 6 countries, we were able to invite all trainees from at least three training institutions. While choosing participating institutions, trainee organisations acted to balance geographical and educational characteristics to ensure the most representative sample within local limitations. Total number of trainees in each country and sampling method are listed in Table 1. An ethical approval was obtained in each country in line with best practice. The study was first piloted in Croatia and France in 2007/2008 [Reference Jovanovic, Beezhold, Andlauer, Rojnic Kuzman, Hanon and Schulze22], and subsequently implemented in other countries during 2009–2012. The only inclusion criterion was being a psychiatric trainee, defined as a fully qualified medical doctor enrolled in a nationally recognised specialist training program in psychiatry. All participants received two reminders within a one-month timeframe. Taking part in the study was voluntary.
Table 1 Sampling description with response rates, age, gender, weekly working hours and burnout syndrome rates in participants included in the study (n = 1980).

a Hierarchical Sample-Type Options: A: all trainees in the country; B: statistically rigorous randomised sample of all trainees in the country that controls for possible sources of bias; C: randomised sample consisting of a significant proportion of all trainees in the country but without clear controls for possible sources of bias; D: all trainees from more than one training institution in the country; E: trainees from more than one training institution in the country; F: all trainees from the largest training institution in the country.
b Number of participants who fully completed the MBI-GS and were included in the final analysis presented in this paper.
c Percentage of trainees who fully completed the MBI-GS out of all approached trainees in each country.
d MBI-GS subscales were abbreviated as follows: Emotional exhaustion (MBI-EX), Cynicism (MBI-CY) and Professional efficacy (MBI-PE).
e Severe burnout was determined as the result of the following logical operation: (MBI-EX > 2.20) and (MBI-CY > 2.00).
f The sample was taken from Flanders only.
g Two participants did not provide data on their age.
The main outcome was trainees’ burnout syndrome measured using the Maslach Burnout Inventory MBI-GS [Reference Maslach, Jackson and Leiter4]. The instrument consists of 16 items divided into three subscales: emotional exhaustion (MBI-EX), cynicism (MBI-CY), and professional efficacy (MBI-PE). All items use a frequency rating scale ranging from 0 (never) to 6 (daily). The MBI-GS cut-off scores for severe burnout are mean sum scores ≥ 2.20 on the MBI-EX and ≥ 2.00 on the MBI-CY, or ≤ 3.66 on the MBI-PE [Reference Maslach, Jackson and Leiter4,Reference Lasalvia, Bonetto and Bertani23]. To determine severe burnout cases as a dichotomous outcome, only the first two criteria were used as there is empirical evidence that exhaustion and cynicism constitute the core of burnout and are often used to distinguish clinically burned out from non-burned out subjects, whereas lack of professional efficacy seems to play a less prominent role [Reference Maslach, Schaufeli and Leiter7].
We also collected data on three groups of predictors – individual (age, gender, relationship status, having children, psychiatry as first career choice), educational (completed years of training, postgraduate education other than training), and work-related (weekly working hours, daily rest and weekly clinical supervision) characteristics. Relationship status was dichotomized into being single (comprising being single, divorced, separated, and widowed), and being in a relationship (married or in a relationship).
2.2 Statistical analysis
Burnout syndrome was explored across three dimensions (continuous variables) and as severe burnout (dichotomous variable). Descriptive statistics were used to report burnout rates and trainees’ general characteristics. Sensitivity analysis was performed to examine the possible impact of non-response on burnout rates. First, to gain some insight into relations between the studied variables, all predictors were compared between severe burnout and others using Chi2 and analyses of variance, depending on the type of data.
Secondly, due to inter-country variance (MBI-EX: 9.2%, MBI-PA: 16.1%, and MBI-CY: 5.0%), linear mixed models (provided by IBM SPSS Statistics 22 software) were used to predict MBI scores. A random-intercept model was used to account for the nesting (clustering) of residents within countries. Country was considered a level-2 variable, while the other variables were considered level-1 variables. A random-intercept model where all predictors were entered simultaneously in the regression equation as main effects only was compared to the null random-intercept model. Because the means of various predictors differed among the countries, we decided to centre all continuous predictors using group-mean centering [Reference Enders and Tofighi24]. The maximum likelihood method was used for estimating parameters. As residuals were not normally distributed for any of the studied criteria, the bias-corrected and accelerated bootstrap approach with 10,000 generated samples stratified by country was used for deriving 95% CIs for the estimated regression parameters.
Next, a generalized linear mixed model was used to examine how different predictors were associated with severe burnout. Subjects were grouped within countries and the same predictors as in predicting the MBI scale scores were entered simultaneously in the model with random-intercepts.
A binary logistic regression model (with binomial probability distribution and logit link function specified) was used with Satterthwaite's approximation for determining degrees of freedom and robust estimation of covariances. A 5% alpha error rate was used as the limit of statistical significance for each predictor.
3. Results
3.1 Subjects
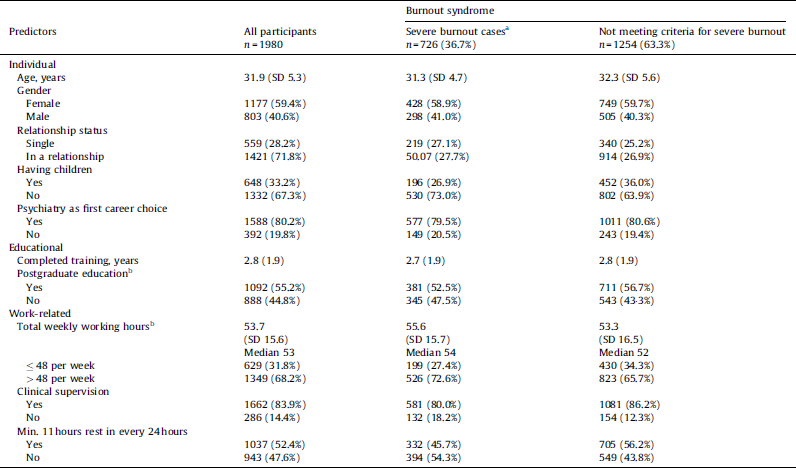
Out of 7468 trainees who received an e-mail invitation to participate, 2698 (36.1%) partially responded and 1980 trainees (26%) fully completed the main outcome measure (MBI-GS). Thus, a total of 1980 trainees from 22 countries were included in the final analysis presented in this paper. Please see the Flow diagram (Fig. 1). Trainees’ individual, educational and work profile is given in Table 2. On average, participants had started psychiatry training at the age of 28.5. At the time of study they had completed 2.8 years of training and were 32 years of age. Half of the sample was engaged in some form of postgraduate education outside official psychiatry training curriculum (n = 1092, 55.2%) such as having a master's degree (n = 525), being a master's degree student (n = 27), having a PhD (n = 82), being a PhD student (n = 117), or having completed/being in psychotherapy training (n = 439). For the vast majority, psychiatry was the first career choice (n = 1588, 80.2%) and this decision was made mostly after medical school (n = 947, 59.6%). Participants reported an average of 53.7 working hours per week divided between the workplace (mean 48.1, SD 14.3) and doing work assignments at home (mean 5.9, SD 7.1). The majority of the sample (n = 1349, 68.2%) was working more than 48 hours per week on average. Regular weekly clinical supervision was available to 1666 (83.9%) trainees, ranging from one hour (n = 722, 36.9%) to five hours per week (n = 110, 5.6%). A total of 286 trainees (14.4%) reported not having any supervision for their clinical work. It was also found that majority were able to get rest breaks such as eleven hours of continuous rest a day (n = 1037, 52.4%), a day off each week (n = 1638, 82.7%), and a 20 minutes rest break every six hours (n = 1297, 65.5%).

Fig. 1 Flow diagram.
Table 2 Individual, educational and work-related predictors among all study participants (n = 1980) and severe burnout cases (n = 726, 36.7%).

a Severe burnout was a dichotomous outcome, defined as mean sum scores ≥ 2.20 on the emotional exhaustion (MBI-EX) and ≥ 2.00 on the cynicism (MBI-CY).
b Total weekly working hours are sum of time spent doing work assignments at one's workplace (mean 48.1, SD 14.3) and at home (mean 5.9, SD 7.1). Two participants did not provide data on their weekly working hours.
3.2 Burnout syndrome
Table 1 shows mean scores on all three MBI-GS subscales for each country. When compared to standard values provided in the MBI-GS manual [Reference Maslach, Jackson and Leiter4], the overall level of burnout was moderate across all three dimensions. The number of trainees scoring above cut-off values on emotional exhaustion was 1167 (58.9%), on cynicism 892 (45.1%) and below cut-off on professional efficacy 414 (20.2%). The number of severe burnout cases was 726 (36.7%). The prevalence ranged from 15% in Bosnia and Herzegovina to 60% in South Africa. Internal consistency of the three subscales was good, Cronbach's alpha for MBI-EX was 0.89, for MBI-CY 0.81, and for MBI-PE 0.82.
3.3 Non-response bias
There are several ways to address non-response bias [Reference Johnson and Wislar25]. Firstly, countries with response rate above 50% of all trainees in the country (i.e. Bosnia and Herzegovina, Croatia, Estonia, and Slovenia) were compared to the rest of the sample. No statistically significant difference was found in emotional exhaustion [mean 2.6, SD 1.4 vs. mean 2.5, SD 1.4, F(1) = 0.333, P = 0.467], cynicism [mean 1.9, SD 1.2 vs. mean 2.1, SD 1.4, F(1) = 2.43, P = 0.119] or rates of severe burnout [49/127 vs. 677/1763, Chi2(1) = 0.002, P = 0.96]. However, trainees in these countries scored significantly higher on professional efficacy [mean 4.7, SD 0.9 vs. mean 4.5, SD 1.1, F(1) = 8.118, P ≤ 0.001]. Associations between predictors and severe burnout were all replicated with the exception of weekly working hours [mean 53.8, SD 16.1 vs. mean 50.6, SD 14.7, F(1) = 2.55, P = 0.111]. Secondly, we assumed that partial responders are likely to resemble non-responders. When compared to full responders, partial respondents (n = 718) did not differ in socio-demographic characteristics or the reported weekly working hours (see flow diagram). Thirdly, we searched for national data to compare basic socio-demographic characteristics of responders vs. all psychiatric trainees within the country. Data on trainees’ age and gender were available from UK, Hong Kong, Croatia, Latvia, Estonia and Belgium. No difference in gender distribution was found. In terms of age, the UK sample in our study differed from the UK national sample. The proportion of younger trainees (less than 34 years) was higher in our study than in the national sample (575/811 vs. 1317/1984).
3.4 The role of individual, educational and work-related characteristics
To explore the role of these predictors on emotional exhaustion, cynicism and professional efficacy and at the same time control for the differences in burnout rates between countries, a hierarchical linear model was created and results are shown in Table 3. The models were statistically significant [MBI-EX Chi2(10) = 133.9, P < 0.001; MBI-CY Chi2(10) = 119.5, P < 0.001; MBI-PE Chi2(10) = 65.7, P < 0.001]. A higher level of emotional exhaustion was statistically significantly associated with longer working hours, lack of clinical supervision and less than 11 hours of daily rest. Cynicism was statistically significantly higher in younger participants and in participants without children, male trainees, those who stated that psychiatry was not their first career choice, and those who had no clinical supervision. Professional efficacy was statistically significantly lower in those without postgraduate education.
Table 3 Linear mixed models for predicting scores on the three Maslach Burnout Inventory (MBI-GS)a scales among all study participants (n = 1978)b.

a Maslach Burnout Inventory (MBI-GS) consists of 16 items divided into three subscales: emotional exhaustion (MBI-EX), cynicism (MBI-CY), and professional efficacy (MBI-PE). In our analysis, the three outcome variables were treated as continuous and ranged from 0 to 6.
b As two participants had some missing data, the analyses were performed on 1978 cases.
c Predictor variables were dichotomous (gender, not in a relationship, not having children, psychiatry was not first career choice, no postgraduate education, not enough daily rest, and no clinical supervision) or continuous (age, completed years of training, and working hours). All predictors were entered simultaneously in the model. Please note that for dichotomous predictors the value of the coefficient shows the difference in the outcome variable between the tested and the reference group (e.g., Not in a relationship represented the tested group compared to the reference group that was composed of participants who were in a relationship) when all other variables are held constant. In continuous variables, the value of the coefficient shows the amount of change in the outcome variable for every one-year increase in age and completed years of training, or for every one-hour increase in working hours when all other variables are held constant.
d Ninety-five percent CI for parameter estimates were obtained with the bias-corrected and accelerated bootstrap.
To explore the influence of these predictors on severe burnout, we created a generalized linear model and results are shown in Table 4. The probability for the presence of severe burnout was positively related to younger age (for every one-year increase, the odds ratio of severe burnout decreased for 17%), not having children (the odds ratio of severe burnout was increased by 44% compared to the odds ratio in participants having children), and not choosing psychiatry as the first career choice (the odds ratio of severe burnout was 21% higher than in the participants who chose psychiatry as the first career choice). Not being enrolled in or not having completed postgraduate education was of borderline statistical significance. All work-related characteristics showed significant association even when controlled for country differences and individual and educational predictors. The odds ratio of severe burnout was higher with more weekly working hours (it increased by 9% with every additional hour), not having clinical supervision (it was 63% higher than in the group receiving supervision), and not having regular 11 hours rest in every 24 hours (the odds ratio of severe burnout was 38% higher for those who did not have regular rest compared to those who did have it). The relationship between severe burnout and working hours remained positively significant even when only working hours at the workplace where taken into account (without hours spent doing assignments at home).
Table 4 Generalized linear mixed model for predicting severe burnouta among all study participants (n = 1978)b.

a Severe burnout was a dichotomous outcome, defined as mean sum scores ≥ 2.20 on the emotional exhaustion (MBI-EX) and ≥ 2.00 on the cynicism (MBI-CY).
b As two participants had some missing data, the analyses were performed on 1978 cases.
c Predictor variables were dichotomous (gender, not in a relationship, not having children, psychiatry was not first career choice, no postgraduate education, not enough daily rest, and no clinical supervision) or continuous (age, completed years of training, and working hours). All predictors were entered simultaneously in the model. Please note that for dichotomous predictors the value of the coefficient shows the difference in the outcome variable between the tested and the reference group (e.g., Not in a relationship represented the tested group compared to the reference group that was composed of participants who were in a relationship) when all other variables are held constant. In continuous variables, the value of the coefficient shows the amount of change in the outcome variable for every one-year increase in age and completed years of training, or for every one-hour increase in working hours when all other variables are held constant.
4. Discussion
Key findings:
besides national variations, 36.7% of psychiatric trainees met criteria for severe burnout syndrome;
the risk was increased by several individual factors such as not opting for psychiatry as a first career choice, not having children and younger age. Educational characteristics such as years spent in training and other postgraduate education were not statistically significantly associated with severe burnout;
even after adjusting for these individual differences, country differences in burnout rates, and years in training, three work-related factors remained positively associated with severe burnout: long working hours, lack of clinical supervision, and not having regular time to rest.
Burnout syndrome rates among psychiatric trainees in most countries included in the study were substantial and double that in the general population [Reference Lindblom, Linton, Fedeli and Bryngelsson26]. However, they seemed to be in line or lower than among other medical trainees [Reference Prins, Hoekstra-Weebers and Gazendam-Donofrio15] or fully qualified psychiatrists [Reference Shanafelt, Boone and Tan9,Reference Lasalvia, Bonetto and Bertani23]. This rather optimistic finding might be beneficial for the image of psychiatry and potentially attract medical graduates considering this career. When analysing trainees’ individual and educational characteristics, we found that years of completed training were not protective from severe burnout. Postgraduate education other than core psychiatric training (such as a master's degree, PhD or psychotherapy training) was of borderline protective value. Notably, trainees with additional postgraduate education did report more feelings of professional efficacy, which might be one of factors that is preventing them from developing burnout syndrome. For example, it might be expected that for many trainees psychotherapy training would entail personal therapy. Although we were not able to explore this specific point in our sample as data was not available, it might be worth exploring it in future research because personal therapy could be expected to be a key factor in supporting trainees and mitigating burnout. We have also found that having children, but not relationship status, decreased the risk for severe burnout. This finding was previously reported for medical trainees [Reference Collier, McCue, Markus and Smith27] and might indicate a protective role of parenthood, possibly through its contribution to healthier work-life balance.
Most importantly, even after adjusting for these individual differences, country differences in burnout rates, and years in training – three work-related factors remained positively associated with severe burnout. These were long working hours, lack of clinical supervision, and not having regular time to rest. The effect of working hour limitations has been studied extensively and it was found that trainees who reported working more than 80 hours had higher rates of burnout (69.2%) compared with 38.5% after the time restriction [Reference Martini, Arfken and Balon10]. In our sample long working hours increased the risk for high emotional exhaustion and severe burnout even when only hours at the workplace where taken into account (without hours spent on work assignments at home).
This is the first study to show the negative influence of lack of supervision, and the impact of working in a field where this is not the trainees’ first career choice, on developing severe burnout. Supervision has been often considered as a unique learning experience for psychiatric trainees. It offers an effective platform for trainees to reflect on their practice, and supports development of competence and professional identity [Reference Falender and Shafranske28]. In the light of the known importance of clinical supervision, it is surprising that almost 15% of trainees did not receive regular weekly supervision (or did not perceive it as such). Despite several reports which have highlighted problems over structure and content of supervision [29–Reference Viswanath, Chandra and Chaturvedi31], the topic lacks systematic research and remains a largely under researched area. The impact of not choosing psychiatry as first career choice (in 19.8% trainees) on developing severe burnout could be related to the lack of interest and motivation to persevere with training, and endure its more demanding aspects. This finding needs to be discussed in the light of recruitment challenges in psychiatry [Reference Katschnig32]. With current unfilled training posts, it remains likely that trainees who fail to attain a training post in a preferred discipline will be recruited into psychiatry training presenting both challenges and opportunities for trainees and training systems.
The study has both strengths and limitations. This is the largest study on training conditions and burnout syndrome among psychiatric trainees to date. In most countries included in the study no previous information on training conditions from the trainees’ perspective or trainee burnout is available. We hope this report will serve as a starting point for discussions regarding training and working conditions in individual countries and indeed in national organisations and at local and international policy levels. Although similar in response rate to extant data from other studies utilising online surveys, response rate varied across participating countries (range 17.8–65.6%; overall 26%). However, a sensitivity analysis revealed that the prevalence of severe burnout and associations with studied predictors did not statistically significantly differ between countries with response rates of more or less than 50%, which strengthens the representativeness of our results. We note that further evaluation of non-response bias indicated that UK subsample in our study is younger than the UK national sample of trainees in the same year when data was collected. Perhaps given the younger age of UK participants, this may indicate a response bias in our finding that younger trainees are at higher risk for severe burnout. Although several other studies also found younger age as a risk factor [Reference Maslach, Schaufeli and Leiter7], it remains unclear whether younger trainees are indeed more affected or maybe more likely to participate in similar research. In light of recent findings that burnout might be more strongly associated with generic than with job-related factors [Reference Bianch, Boffy and Laurent33], it might be expected parameters such as global stress, economic stability or global life satisfaction play significant role in trainees’ burnout. Lastly, countries included in the study differ in cultural, educational and organisational backgrounds. We were not able to explore in detail how different historic and cultural backgrounds, work ethos, health care settings, political settings and economic inequality for both trainees and patients might impact upon the prevalence of burnout rates, although we are aware that the impact might be both positive and negative. Extant research shows that burnout is a global phenomenon that can, to some extent, go beyond intercultural differences [Reference Schaufeli, Leiter and Maslach34]. We did explore further differences between training systems in countries included in the study and thus determined that duration of training and rotations were rather similar across countries, exceptions being Belarus and Russia with significantly shorter duration of training (1 and 2 years, respectively). Since data collection most countries did not reform their training curricula, while several countries slightly modified duration of non-psychiatric rotations (Czech Republic, Denmark and Hungary). In two countries curriculum has recently been prolonged from 4 to 5 years (Croatia and Bosnia and Herzegovina).
5. Conclusions
Working conditions influence burnout rates, even if other influential factors (such as personal and educational characteristics) are controlled for, so interventions such as limited working hours and regular supervision could represent a way of reducing severe burnout. Since previous research identified that job stress and low morale are associated with worse patient care and low retainment, we contend that these interventions may improve patient care and may increase retention rates in psychiatry. Clearly, these results only represent a part of a complex picture, which is not yet fully understood or detailed. The study was created using principles of model building methodology to provide basic understanding of associations between individual, educational and training characteristics, and severe burnout among psychiatric trainees. Future studies are needed to expand our knowledge in this area. Ideally, future studies could use individual domain data as continuous variables to further evaluate the relationship between severe burnout, supervision and career choice, and other potential contributing factors. They can also be expected to provide additional evidence regarding potentially resilience-promoting factors such as age, professional experience, psychotherapy training, generic factors, and work engagement. We hope this study provides a foundation for future work to benefit psychiatry, trainees, and ultimately psychiatric patients.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgements
We would like to thank Professor Stefan Priebe, Dr Amit Malik, Professor Andrea Fiorillo, Dr Adriana Mihai, Dr Olga Kazakova, Dr João Gama Marques, Dr Cecile Hanon, Dr Ulrike Weisz, Dr Goran Racetovic, Dr Teelia Rolko, Dr Mia Soendergaard, Dr Marija Rusaka, members of the European Federation of Psychiatric Trainees (EFPT) and the European Psychiaytric Association–European Early Career Psychiatrists (EPA–EECP).
We would like to thank the Royal College of Psychiatrists in the UK, the Hong Kong College of Psychiatrists, and the Croatian Institute of Public Health for their help in aquiring socio-demographic data of psychiatric trainees.Funding: none.









Comments
No Comments have been published for this article.