The prevention and management of invasive fungal infections is challenging due to the difficulty in establishing a definitive diagnosis, limited therapeutic options, potential for treatment-related adverse events, and high rates of morbidity and mortality. Reference Lestner, Versporten and Doerholt1,Reference Valerio, Rodriguez-Gonzalez and Munoz2 In children, antifungal use has dramatically increased and shifted to broader-spectrum agents. Reference Prasad, Coffin, Leckerman, Walsh and Zaoutis3,Reference Downes, Ellis, Lavigne, Bryan, Zaoutis and Fisher4 This increase is likely related to higher numbers of immunocompromised patients at risk of invasive fungal infections and the use of prophylactic and empiric antifungal therapy in this population. Reference Santiago-Garcia, Rincon-Lopez and Ponce Salas5,Reference Warris6 Also, significant variability exists in antifungal use across adult and pediatric hospitals, suggesting possible misuse or overuse. Reference Goldman, Ross and Lee7,Reference Stultz, Kohinke and Pakyz8 The inappropriate use of antifungals can lead to treatment failure, toxicities, increased costs, and the emergence of resistance. Reference Ananda-Rajah, Cheng and Morrissey9–Reference Shah, Yau and Lasco11 Antimicrobial stewardship is a widely established approach for monitoring and optimizing the use of antimicrobials; however, most stewardship efforts have focused on antibiotics and not antifungals. Reference Hersh, De Lurgio and Thurm12,Reference Kronman, Banerjee and Duchon13 Antifungals have many unique features: use in special populations (eg, immunocompromised patients, premature neonates), use for infections that are often difficult to microbiologically confirm, variable correlation between in vitro and in vivo activity, high cost, and requirement for therapeutic drug monitoring (TDM). Thus, the stewardship strategies employed for these agents may differ from those for antibiotics. We aimed to characterize the current state of antifungal stewardship among pediatric ASPs and the perception of ASPs regarding inappropriate antifungal use, antifungal stewardship, and antifungal resistance.
Methods
An electronic survey was developed based on published antimicrobial stewardship guidelines and specific antifungal stewardship interventions. Reference Barlam, Cosgrove and Abbo14–Reference Menichetti, Bertolino and Sozio17 An independent survey expert reviewed the readability and design of the questionnaire; subsequently, the survey was pilot tested among a group of antimicrobial stewardship physicians for relevance and content validity. The survey included 17 closed-ended questions exploring institutional antifungal stewardship practices and perceptions (Supplementary Fig. 1 online). The survey included questions about prospective audit and feedback (PAF) and preauthorization, since these are the core elements of antimicrobial stewardship described in the 2016 Infectious Diseases Society of America (IDSA) and the Society for Healthcare Epidemiology of America (SHEA) guidelines. Reference Barlam, Cosgrove and Abbo14 We also asked about other antifungal stewardship elements and interventions reported in the literature, including mandatory infectious diseases consultations for fungemia, antifungal TDM, publication of institutional antifungal susceptibility reports, and the use of fungal markers. Reference Hamdy, Zaoutis and Seo15–Reference Menichetti, Bertolino and Sozio17 Lastly, we included questions related to perceptions around inappropriate antifungal use, antifungal stewardship, and antifungal resistance. We used Likert-type scales, binary options, and multiple choice answers, as appropriate, to capture the perceptions around antifungal stewardship (Supplementary Fig. 1 online).
The survey was distributed electronically among pediatric ASPs of 74 hospitals participating in the multicenter Sharing Antimicrobial Reports for Pediatric Stewardship (SHARPS) Collaborative. A member of the antimicrobial stewardship team (physician or pharmacist) completed the survey at each institution. Data were collected from December 2018 through February 2019. Reminders were sent to nonrespondents at 2–3-week intervals during the data collection period. The first complete survey received was included in the study and duplicate or incomplete surveys from the same institution were excluded. Hospitals were deidentified prior to analysis.
We used descriptive statistics, including frequencies and proportions, to summarize the survey responses. We compared antifungal stewardship strategies and perceptions based on hospital type, hospital beds, and geographic region using the χ2 test. The statistical analysis was performed with JMP version 14.1 software (SAS Institute, Cary, NC). Informed consent was obtained from study participants. The study was approved by the Stanford University School of Medicine Institutional Review Board.
Results
We received 68 unique responses from 74 hospitals, for a response rate of 92%. We received surveys from 34 states and 2 international sites. The respondents included 37 pediatric infectious diseases physicians (54%) and 31 pharmacists (46%). Hospital characteristics of the participating pediatric ASPs are summarized in Table 1.
Table 1. Hospital Characteristics of Surveyed Pediatric Antimicrobial Stewardship Programs

Note. ASP, antimicrobial stewardship.
Overall, 93% of ASPs (63 of 68) reported that they conduct 1 or more antifungal stewardship activities. Of the 68 respondent ASPs, 32 (47%) use both core stewardship strategies: PAF and preauthorization of antifungals. Also, 20 ASPs (30%) require preauthorization of antifungals alone, 11 (16%) perform PAF of antifungals alone, and 5 (7%) do not perform any antifungal stewardship activities.
Among pediatric ASPs, 43 of the 68 respondents (63%) perform PAF of antifungals and 52 (76%) require preauthorization of 1 or more antifungal agents. The characteristics of antifungal PAF and preauthorization are shown in Table 2. No differences in antifungal stewardship strategies were identified based on hospital type or hospital beds. For those who do not audit antifungals, the most common reasons for not performing PAF are insufficient time or resources (19 of 25, 76%) and minimal institutional antifungal use (6 of 25, 24%).
Table 2. Characteristics of Antifungal Stewardship Strategies Among Pediatric Antimicrobial Stewardship Programs
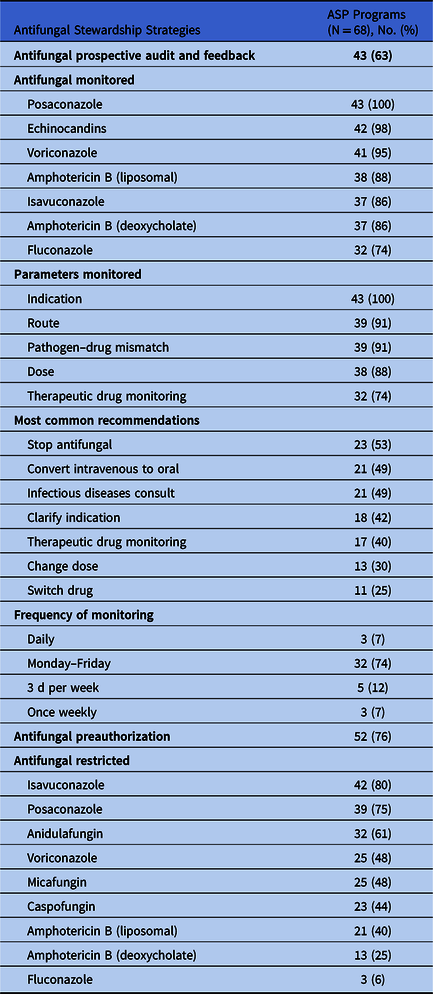
Note. ASP, antimicrobial stewardship.
At 58 of the 68 respondent hospitals (85%), TDM of antifungals is routinely performed, and 23 of these 58 programs (40%) have a pharmacokinetics program to assist with this effort. Of the 58 hospitals that reported antifungal TDM, all 58 (100%) perform TDM for voriconazole and 46 (79%) perform TDM for posaconazole. The target trough level reported for the treatment of suspected invasive fungal infections varied across institutions (Fig. 1). Among the responding hospitals, 10 (15%) reported that their hospital has a policy mandating pediatric infectious diseases consultation for patients with fungemia. Among hospitals without a mandatory consult policy, most reported that pediatric infectious diseases consultations occur with >75% of the cases of fungemia (67%, 39 of 58). Also, 53 of 68 institutions (79%) reported using noninvasive fungal markers when evaluating for invasive fungal infections. The most commonly used fungal markers among these institutions were serum aspergillus galactomannan (53 of 53, 100%) and (1,3)-β-D-glucan (41 of 53, 77%). Only 14 hospitals (20%) reported that they include antifungal susceptibilities as part of their institutional antibiogram.

Fig. 1. Voriconazole and posaconazole target therapeutic levels reported by pediatric antimicrobial stewardship programs.
A summary of the ASPs perceptions about antifungal use and resistance is shown in Figure 2, with additional details in Supplementary Table 1 (online). Compared to children’s hospitals within a hospital, ASPs from freestanding children’s hospitals are more likely to agree or strongly agree that antifungals are inappropriately used at their institutions (60% vs 34%, P = .03). Likewise, respondents from large-size hospitals (>300 beds) are more likely to agree or strongly agree that antifungals are inappropriately used at their institution than medium- and small-sized hospitals (67% vs 51% vs 25%, P = .02). The perception of inappropriate use did not differ based on the respondent’s role. ASPs in hospitals that reported antifungal susceptibilities were more likely to perceive antifungal resistance as problem at their institutions (64% vs 35%, P = .04). Only 25 ASPs (37%) reported feeling very confident in providing antifungal recommendations. Respondents reported that having clinical guidelines specific for antifungal use in children and better diagnostics would improve their level of confidence in making antifungal recommendations (46%, 31 of 68 and 37%, 25 of 68, respectively). Furthermore, respondents perceived hematology-oncology (32 of 68, 47%) and stem cell transplant (15 of 68, 22%) as the services most likely to benefit from antifungal stewardship interventions.

Fig. 2. Perceptions about antifungal use and stewardship among pediatric antimicrobial stewardship programs.
Discussion
Our survey revealed some of the antifungal stewardship practices and perceptions in a cohort of pediatric ASPs. Most pediatric ASPs have implemented some form of antifungal stewardship, and the strategies employed are highly variable across surveyed hospitals. Interestingly, although nearly half of respondents perceived inappropriate antifungal use as a problem at their hospital, many did not feel confident in providing antifungal recommendations. Specific stewardship strategies, including antifungal TDM and fungal susceptibility reporting, appear to be less common and may represent unique and important antifungal stewardship opportunities.
According to our survey results, the core antimicrobial stewardship strategies, PAF and preauthorization, have been expanded to include antifungals in most pediatric ASPs. Although these antifungal stewardship interventions have been shown to successfully reduce antifungal consumption in hospitalized patients, the best approach to antifungal stewardship remains unknown. Reference Santiago-Garcia, Rincon-Lopez and Ponce Salas5,Reference Menichetti, Bertolino and Sozio17–Reference Valerio, Munoz and Rodriguez20 This lack of comparative data has likely led to the very heterogenous and hospital-specific approaches illustrated in this study. Some studies have proposed that PAF and more intensive stewardship strategies like daily PAF in combination with preauthorization and formulary restriction, may be more effective in decreasing antibiotic utilization. Reference Stenehjem, Hersh and Buckel21,Reference Tamma, Avdic and Keenan22 Whether the same is true for antifungals is unknown. In our study, the use of preauthorization was more common than PAF, which is considered relatively labor intensive. Reference Barlam, Cosgrove and Abbo14 Similar to prior reports evaluating antibiotic stewardship strategies, respondents reported that the biggest barrier to implementing antifungal PAF was a lack of time and resources. Reference Hersh, Beekmann, Polgreen, Zaoutis and Newland23–Reference Newland, Gerber and Weissman25 The frequency of antifungal monitoring varied widely, with <10% of programs performing daily PAF. Whether the absence of daily PAF reflects a lack of sufficient resourcing or is a purposeful choice is uncertain; however, it may result in missed opportunities to intervene and improve antifungal prescribing. These findings highlight the importance of identifying effective antifungal stewardship interventions to better utilize and optimize current resources.
The characteristics of antifungal PAF and preauthorization varied across hospitals. For example, the survey detected differences in the types of antifungals monitored as part of PAF and restricted as part of preauthorization programs. Broad-spectrum triazoles, including voriconazole, posaconazole, and isavuconazole, were commonly targeted as part of antifungal stewardship efforts. ASPs may focus their efforts on these antifungals given the need for TDM, potential toxicities, and their higher costs. Reference Munoz and Bouza26,Reference Ross, Hersh, Kronman, Newland and Gerber27 However, fluconazole may represent an important antifungal stewardship target because it accounts for ~70% of antifungal prescriptions in children Reference Downes, Ellis, Lavigne, Bryan, Zaoutis and Fisher4 and has been associated with inappropriate prescribing in neonates and children. Reference Lestner, Versporten and Doerholt1,Reference Ferreras-Antolin, Irwin and Atra28
The TDM of azole medications is an important strategy to ensure the appropriate use of antifungals and mitigate adverse events. Reference Park, Kim and Kim29 Most institutions responding to this survey routinely monitor azole levels; however, TDM was the least commonly monitored parameter among ASPs performing PAF of antifungals, and only a few institutions reported having a pharmacokinetics program to assist with antifungal TDM. These findings suggest that most clinicians conduct TDM of antifungals without expert guidance from pharmacists or ASP team members, which may increase the risk for medication errors and suboptimal dosing. Antifungals can be particularly challenging to use in children given their unique pharmacokinetic and pharmacodynamic characteristics. For example, studies have shown that up to 50% of antifungals are inadequately dosed and that certain antifungals require multiple dose adjustments to achieve therapeutic levels. Reference Santiago-Garcia, Rincon-Lopez and Ponce Salas5,Reference Ferreras-Antolin, Irwin and Atra28,Reference Lachenmayr, Berking, Horns, Strobach, Ostermann and Berger30,Reference Soler-Palacin, Frick and Martin-Nalda31 Our study revealed variability in the target therapeutic levels reported across institutions, which suggests a lack of consensus in current practices and an important opportunity for standardization.
Many of the survey respondents reported a lack of confidence in making antifungal recommendations. This important finding could be related to the limited diagnostic information available to guide antifungal stewardship recommendations. Indeed, almost 40% of the respondents in our survey reported that having better diagnostics would improve their level of confidence in making antifungal recommendations. The absence of microbiological data may limit the ability of ASPs to identify opportunities for discontinuation or de-escalation of antifungals and contribute to prolonged courses of prophylactic or empiric antifungals. Previous surveys have shown that de-escalation of broad-spectrum antibiotic therapy on the basis of culture results is one of the most common antibiotic stewardship interventions. Reference Hersh, Beekmann, Polgreen, Zaoutis and Newland23 In contrast, our study found that the recommendation to switch antifungals (ie, de-escalate therapy) was one of the least commonly reported interventions. As a surrogate for culture data, the use of noninvasive fungal markers was common among the surveyed hospitals. Prior studies have evaluated the use of noninvasive fungal markers for the surveillance of invasive fungal infection in stem cell transplant patients in an effort to shift from a prophylactic to a preemptive approach and decrease potentially unnecessary antifungal exposure. Reference Cordonnier, Pautas and Maury32–Reference Morrissey, Chen and Sorrell34 Further studies exploring the safety and utility of these tests as part of antifungal stewardship interventions in the pediatric population are warranted.
Inappropriate and unnecessary antifungal use was considered a problem by most pediatric ASPs in this study. Oncology and stem cell transplant were reported as the services that would benefit the most from antifungal stewardship, likely because of the disproportionally higher antifungal utilization described in this population. Reference Goldman, Ross and Lee7 Also, most ASPs in this cohort identified antifungal resistance as a national problem, and to a lesser extent, an institutional problem. This perception may be due to the recent emergence of multidrug-resistant Candida auris outbreaks in hospitals across the United States. Reference Forsberg, Woodworth and Walters35 Most of these cases have been reported in adults; therefore, respondents of this study may consider issues of antifungal resistance as a national, rather than local, problem. Only 20% of the hospitals reported antifungal susceptibilities as part of the institutional antibiogram, and ASPs in these hospitals were more likely to perceive antifungal resistance as a problem at their institution. Possibly, therefore, resistant fungal organisms are underreported or ASP team members are not aware of institutional antifungal susceptibility trends. The emergence of antifungal resistance has been increasingly recognized, and understanding the local epidemiology is essential to developing institutional guidelines for antifungal prophylaxis and the empiric treatment of fungal infections.
Our study has several limitations. First, these results may not be generalizable to all pediatric hospitals. Although our response rate was high, we only surveyed ASPs participating in the SHARPS Collaborative, in which members are actively involved in identifying best practices for the use of antimicrobials. Therefore, we may be overestimating the extent to which antifungal stewardship practices are occurring. However, we were able to capture responses from both freestanding children’s hospitals and children’s hospitals within a larger adult hospital. In addition, ASPs from all 4 geographic regions in the United States and 2 international sites in Europe were represented in our cohort. Another limitation is that some of the responses may have been influenced by the respondent’s familiarity with their institution’s resources and practices and may represent perception rather than fact. Finally, we did not evaluate the effectiveness of different antifungal stewardship interventions, which should be further explored in future studies.
Although implementing antifungal stewardship has challenges, it has the potential to decrease unnecessary and suboptimal antifungal use, to reduce toxicities associated with inappropriate antifungal use, and to prevent the emergence of antifungal resistance. Currently, PAF and preauthorization are the main strategies used by pediatric ASPs to perform antifungal stewardship. Future studies should evaluate the effectiveness and clinical impact of such interventions. Optimization of antifungal dosing and TDM via ASPs represent key components of antifungal stewardship in pediatrics. Thus, future antifungal stewardship efforts should focus not only on reducing unnecessary use but also on improving the quality of antifungal prescribing.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.306
Acknowledgments
The authors wish to thank Dr. Bonnie Halpern-Felsher for her input during the development of the electronic survey.
Financial support
This project was supported by the Stanford Maternal and Child Health Research Institute.
Conflicts of interest
The authors have no financial conflict of interest relevant to this article.









