Introduction
The prevalence of mental illness in nursing homes is high. It has been found that up to 91% of nursing home residents have coexisting psychiatric disorder (Tariot et al. Reference Taylor, Paton and Kapur1993). There is extensive use of psychotropic agents in nursing homes, despite warnings about side effects. A recent systematic review examining the prescribing practices in nursing homes revealed that Ireland has amongst the highest rates of antipsychotic drug use in Western Europe (Janus et al. Reference Inouye2016). Murphy & O’Keeffe (Reference Murphy and O’Keeffe2008) found that half of Irish nursing home residents prescribed regular antipsychotic medications were deemed to be receiving these agents inappropriately. The shared values, beliefs and behaviours within an organisation play an important role in medication prescribing (Shaw et al. Reference Shaw, McCormack and Hughes2016). Modification of the factors which influence the treatment culture within nursing homes may lead to a more person-centred approach to use of psychoactive medications. Evidence suggests that regular psychiatric liaison to nursing homes is of benefit. Provision of psychiatric input may impact upon diagnosis, management, identification of medication side effects and better staff understanding of behaviours (Goldman & Klugman, Reference Fossey, Ballard, Juszczak, James, Alder, Jacoby and Howard1990). Amongst nursing home staff there is a perceived need for a greater level of psychiatric involvement particularly in relation to non-pharmacological management techniques, staff support, and dealing with family conflict (Reichman et al. Reference Reichman, Coyne, Borson, Negron, Rovner, Pelchat, Sakauye, Katz, Cantillon and Hamer1998).
According to the Health Information and Quality Authority (HIQA) there is an onus on nursing homes to promote both the general physical and mental health of residents and to provide access to specialist healthcare services where appropriate. In terms of challenging behaviour, HIQA also advocates that ‘expert advice is sought where necessary on a behaviour management and activity plan before commencing psychotropic medication’ (HIQA, Reference Goldman and Klugman2009). Therefore, psychiatric referral and consultation is often a necessary aspect of patient care.
The aim of this study was to describe the behavioural and psychiatric problems found in nursing home psychiatric referrals in the Dublin South city area over two consecutive 12-month periods. We aimed to compare the reasons for referral with the final diagnosis on psychiatric assessment and to examine the prescribing practices in relation to antipsychotic medication. Furthermore, we aimed to assess how these factors would be affected following the introduction of a new clinical nurse specialist (CNS) whose role involved triaging referrals, ensuring patients underwent adequate medical investigation, assessing and monitoring patients and providing support to nursing home staff.
Methods
The St James’s Hospital psychogeriatric team provides an outreach service to patients residing in seven separate nursing homes in the Dublin South city area, with a total of 456 beds. We undertook two consecutive surveys of nursing home referrals to the psychiatry of old age service over a 2-year period.
Survey one retrospectively examined the referrals from 1 April 2014 until 31 March 2015. Towards the end of this period in January 2015 a new CNS was specifically appointed to manage the nursing homes. This was an ideal opportunity to assess how the new role would impact the referrals. Survey two included referrals received between 1 April 2015 and 31 March 2016.
Referrals were accepted directly from nursing homes either via general practitioner (GP) letter or a pre-formatted referral form. Subsequently, patients were clinically interviewed by the team consultant psychiatrist or senior registrar, in the nursing home setting. Diagnoses were made according to the International Classification of Diseases, 10th Revision (World Health Organization, 1992). Collateral information was obtained from family members and nursing staff. A management plan, briefly outlined in the patient’s medical record was developed. All cases were discussed at a weekly multidisciplinary team (MDT) meeting and a comprehensive written report was sent to the GP. Urgent management strategies were implemented immediately by the treating psychiatrist but routine management was left to the GP and nursing home staff.
Upon assessment it often became apparent that many psychiatric referrals were in fact initiated by nursing staff rather than GPs and that patients had not first undergone adequate medical assessment and investigation. The role of the newly appointed CNS was to triage referrals and to ensure that patients had been seen by a GP prior to psychiatric assessment. It was also the duty of the CNS to undertake a preliminary review of the patient and assess the urgency of the referral. The CNS would then accompany the team psychiatrist during the initial patient assessment and provide ongoing follow-up where appropriate. This generally consisted of monitoring and evaluating the patient’s response to treatment and amending the care accordingly in conjunction with the treating psychiatrist and MDT. In addition, the CNS offered support to family and nursing home staff in the care of patients with psychiatric co-morbidity and provided ongoing psycho-education, particularly in relation to the non-pharmacological management of behavioural and psychological symptoms of dementia (BPSD). Finally, the CNS introduced a more stringent method of recording and tracking referrals by establishing a central register. This was used to log information on each patient referred including diagnosis and an up-to-date management plan.
We recorded the following details for each referral made during the study period: gender, age, source of referral (nursing home), reason for referral, psychotropic medication on referral, diagnosis on assessment and intervention. For survey one information was obtained from various sources including hospital files, GP correspondence and nursing home charts. For survey two, information was primarily drawn from the newly established central register.
Results
In total, 107 referrals were received for 98 individuals during the 2-year study period. More than two-thirds of these were female (69%; n = 74) with a median age of 83 years (range 63–96 years). For survey one, 58 psychiatric referrals were received for 52 individuals over a 12-month period. The majority were female (74%; n = 43) and had a median age of 82 years (range 71–98 years). The number of patients referred for psychiatric assessment during survey two was slightly less: 49 referrals were received for 46 individuals. Of these, 63% (n = 31) were females with a median age of 84 years (range 63–96 years). There were no statistically significant differences in relation to gender or age between those in survey one and those in survey two (p>0.05).
During survey one, the median number of referrals received from each of the seven nursing homes was five (range 3–19). A median number of three referrals (range 0–19) were received from each of the nursing homes during survey two.
The most common reason for referral during survey one was uncooperative/aggressive behaviour (22%; n = 13) (Table 1). For survey two, patients were most commonly referred for low mood (31%; n = 15) or agitation (29%; n = 14).
Table 1 Reasons for referral and diagnoses on assessment

BPSD, behavioural and psychological symptoms of dementia; LBD, Lewy body dementia.
During survey one, the majority of patients assessed were diagnosed with BPSD (41%; n = 24). This was also a prevalent diagnosis during survey two, affecting 27% (n = 13) of those referred. Both surveys one and two found that the most common type of BPSD reported was physical and/or verbal aggression (50%; n = 12 and 54%; n = 7, respectively).
On psychiatric assessment only 7% (n = 4) of patients were considered to be delirious during survey one. This rose to 31% (n = 15) the following year making it the most common diagnosis during survey two. Despite this, only two of the 15 delirious patients were actually referred with a diagnosis of delirium. The remaining 13 delirious patients were referred for the following reasons: agitation (39%; n = 5), psychotic symptoms (31%; n = 4), confusion (15%; n = 2), aggression (8%; n = 1) and low mood (8%; n = 1).
Rates of depressive disorder at the time of psychiatric assessment in our study were found to be 10% (n = 6) in survey one and 4% (n = 2) in survey two, with an overall prevalence of 7% (n = 8) across the 2-year study period.
In terms of prescribing practices, 20 patients were on antipsychotic medication at the time of referral during survey one (Fig. 1). Of these, the outcomes were documented for 16 patients: one had their antipsychotic stopped, three were switched to an alternative psychotropic medication (valproate or trazodone), four were switched to an alternative antipsychotic, while eight remained on their current antipsychotic. An additional two patients were also commenced on an antipsychotic during survey two. This resulted in an overall discontinuation rate of 13%. By survey two, the antipsychotic discontinuation rate had risen to 47% following psychiatric input, with the number of patients on antipsychotic medication falling from 15 to eight: six had their antipsychotic stopped, two were switched to an alternative psychotropic medication (trazodone), one was switched to an alternative antipsychotic and six remained on their current antipsychotic. Only one patient was commenced on an antipsychotic medication (quetiapine) in 2015 for management of BPSD.
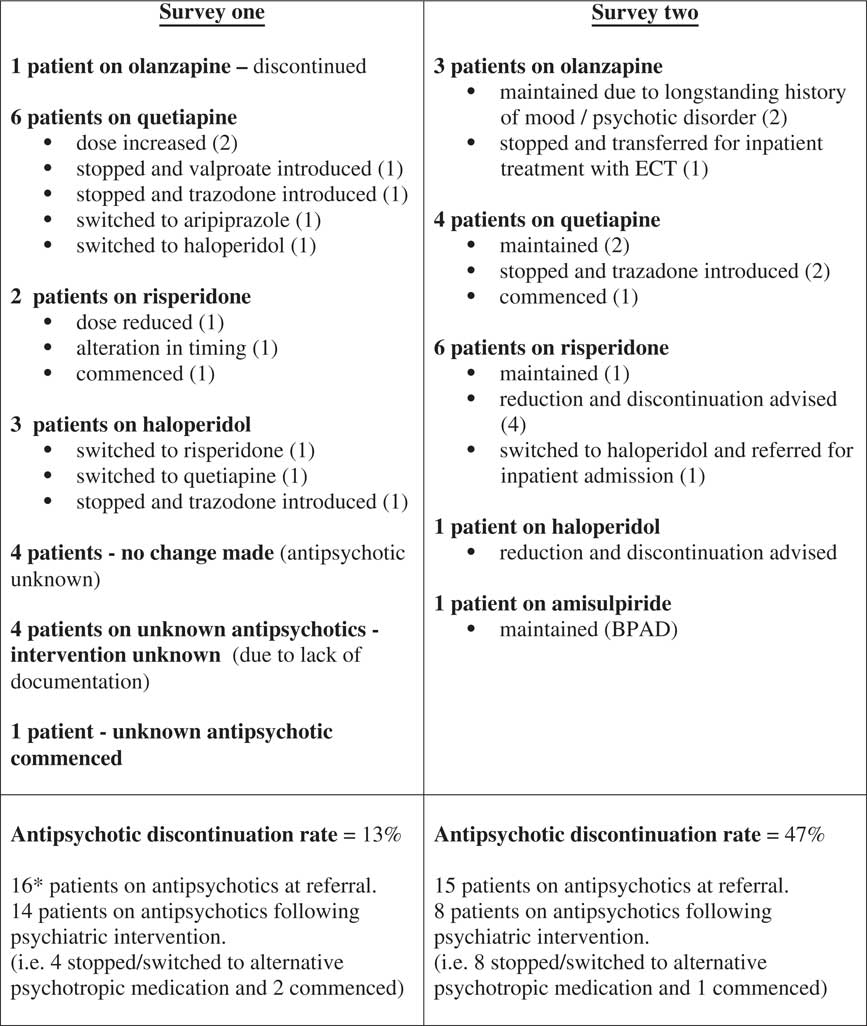
Fig. 1 Antipsychotic interventions. *An additional four patients on antipsychotics with unknown outcomes. ECT, electroconvulsive therapy.
Other patient interventions carried out over the 2-year study period, not related to the management of antipsychotic prescribing, are outlined in Table 2.
Table 2 Non-antipsychotic-related psychiatric interventions

BPSD, behavioural and psychological symptoms of dementia; ECT, electroconvulsive therapy.
Discussion
As noted in previous studies (Loebel et al. Reference Loebel, Borson, Hyde, Donaldson, Van Tuinen, Rabbitt and Boyko1991; Callegari et al. Reference Callegari, Menchetti, Croci, Beraldo, Costantini and Baranzini2006), our survey found that reasons for referral are not always reliable predictors of diagnoses. Patients do not always undergo adequate physical investigation prior to psychiatric referral. Following the introduction of a new CNS, detection rates of delirium increased significantly. This might be explained by more rigorous screening of referrals and by the increased likelihood that GPs would be requested to preform medical investigations in order to out rule physical illness. A large proportion of patients (31%) were found to be suffering from an underlying delirium during survey two requiring medical rather than psychiatric intervention. Conversely, there was a decrease in the diagnosis of BPSD which fell from 41% in survey one to 27% in survey two. These shifts may reflect actual changes in the prevalence’s of delirium and dementia with BPSD between the surveys. However, they also highlight the difficulty of disentangling the two diagnoses due to overlapping neuropsychiatric symptoms. Diagnosing delirium superimposed on a pre-existing dementia can be especially challenging because signs of delirium might be mistaken for the fluctuation of cognitive function, or psychological symptoms of patients with dementia. To further complicate the situation a proportion of people will have dementia that is not recognised, as well as the possibility of a persisting delirium. According to the National Institute for Health and Care Excellence (2010) guidelines, ‘if there is difficulty distinguishing between the diagnoses of delirium, dementia or delirium superimposed on dementia, treat for delirium first’. Delirium frequently goes unrecognised and untreated in nursing homes. Previous studies have noted that detection of delirium is lower in older patients with comorbid dementia (Inouye, 1998; Meagher & Trzepacz, Reference Meagher and Trzepacz2000; Mittal et al. Reference Mittal, Majithia, Kennedy and Rhudy2006). In long-term care, prevalence of delirium has been reported to range between 1.4% and 70.3%, depending on diagnostic criteria and on the number of individuals with dementia (de Lange et al. Reference Kramer, Allgaier, Fejtkova, Mergl and Hegerl2013). The risk of delirium is particularly high for people with dementia, who are over the age of 85 years, or who are living in a care facility (de Lange et al. Reference Kramer, Allgaier, Fejtkova, Mergl and Hegerl2013).
Depression also commonly affects nursing home residents (Tiong et al. Reference Tiong, Yap, Huat Koh, Phoon Fong and Luo2013) with rates three to five times higher than in elderly populations living in the community (Blazer, Reference Blazer2003). Average prevalence’s for nursing home patients are 43.9% for depressive symptoms, 25.7% for minor depression and 15.5% for major depression (Jongenelis et al. Reference Janus, van Manen, IJzerman and Zuidema2003). Our study found that low mood was a common reason for psychiatric referral with 21% of patients being referred with depressive symptomatology over a 2-year period. However, only 7% of patients were actually diagnosed with a depressive disorder following psychiatric assessment. This would indicate, in accordance with previous studies, that depression is often underestimated in the elderly (Teresi et al. Reference Teresi, Abrams, Holmes, Ramirez and Eimicke2001; Leo et al. Reference Leo, Sherry, DiMartino and Karuza2002; Callegari et al. Reference Callegari, Menchetti, Croci, Beraldo, Costantini and Baranzini2006; Kramer et al. Reference Jongenelis, Pot, Eisses, Beekman, Kluiter, van Tilburg and Ribbe2009). In our study, only a small proportion of patients were diagnosed with a depressive disorder suggesting that many depressed residents were not correctly identified or referred for psychiatric assessment and intervention. Nursing home residents are more likely to be psychiatrically referred for disruptive behaviours than depressive symptoms (Leo et al. Reference Leo, Sherry, DiMartino and Karuza2002). The elderly suffering from depression may not draw the attention of nursing home staff if they are not causing disturbance to the residential community.
Approximately 20–50% of patients in institutional care receive antipsychotic drugs (McGrath & Jackson, Reference McGrath and Jackson1996; Fossey et al. Reference de Lange, Verhaak and van der Meer2006). The adverse effects of these drugs include an increased risk of stroke, confusion, sedation, postural hypotension, extra-pyramidal effects and anti-muscarinic effects (BMJ Group, 2007). Therefore, it is important to have a clearly defined indication for prescribing psychotropic medication in elderly patients. Training and support of nursing home staff can result in reduced antipsychotic prescribing in patients, without worsening behavioural symptoms (Fossey et al. Reference de Lange, Verhaak and van der Meer2006). The results of our study revealed that withdrawal of psychotropic medication is possible in many instances. During survey two, 47% of antipsychotics were successfully discontinued with no concomitant objective clinical evidence of a deterioration in patient mental state. In a few cases, patients were switched from an antipsychotic to an alternative psychotropic medication (such as an antidepressant or a mood stabiliser) with less robust evidence of efficacy in BPSD and the potential for a range of different side effects (Taylor et al. Reference Tariot, Podgorski, Blazina and Leibovici2015).
The appointment of a new CNS in January 2015 resulted in differing referral and assessment pathways in surveys one and two. A central register for recording and tracking nursing home referrals was also introduced. However, this did not come into effect until several months after the CNS’s start date. For this reason, there was a lapse of several months between the CNS commencing and survey two commencing. The two study periods ran from April until March of consecutive years. We allowed for a ‘settling-in’ period in an attempt to evaluate the true impact of the CNS’s role on the service. The effect of the improved method for logging referrals via a central register is evident in the results of our study. We encountered difficulties accessing patient details prior to April 2015 due to poor record keeping. This is reflected in the missing data apparent in survey one, with an unknown reason for referral in 19% of cases (n = 11), and an unknown diagnosis on assessment in 16% of cases (n = 9). There was also no documentation of psychiatric interventions and outcomes for four of the 20 patients receiving antipsychotic medication at the time of referral in survey one. However, this was not an issue in survey two as patient information was easily accessed from the central register.
Over the 2-year study period, there was significant variation in the number of referrals received from each of the seven nursing homes. During survey two, for example, some nursing homes referred no patients while one nursing home referred as many as 19 patients. This could be due to differences in bed numbers with some nursing homes accommodating more residents than others. In addition, some nursing homes may have had a greater proportion of individuals with psychiatric illness. However, the variation in numbers of patients referred for psychiatric assessment could also be an indication of differing levels of staff education and confidence in managing mental illness; GPs have different thresholds for requesting psychiatric support and intervention.
Conclusions
Our study demonstrated that following the introduction of a new CNS recognition of delirium increased, with 31% of referred patients being diagnosed with delirium following psychiatric assessment. Delirium is often undetected and untreated in nursing homes. Residents presenting with psychiatric symptoms need to undergo routine bloods and urinalysis prior to psychiatric referral. Based on the study findings a new and more detailed nursing home referral form was drafted incorporating a specific delirium screening tool, the 4A’s Test (Bellelli et al. Reference Bellelli, Morandi, Davis, Mazzola, Turco, Gentile, Ryan, Cash, Guerini, Torpilliesi, Del Santo, Trabucchi, Annoni and MacLullich2014).
Depression is also underestimated in the elderly. Over a 2-year period, we found that only a small proportion of referred patients (7%) were diagnosed with depression. Staff training in relation to the recognition of depressive symptoms is important, particularly as, within the nursing home environment, depressed individuals may be overshadowed by residents who are more behaviourally disturbed and overtly disruptive.
In our study, the discontinuation rate of antipsychotic medication increased from 13% in survey one to 47% in survey two. Ongoing monitoring of antipsychotic prescribing and careful re-evaluation of the need for antipsychotic medication is important to reduce unnecessary drug use. Promoting and educating nursing home staff around the non-pharmacological management of BPSD is an essential role of the psychogeriatric team.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
L.W. has no conflicts of interest to declare. C.P. has no conflicts of interest to declare. R.O. has no conflicts of interest to declare. B.L. has no conflicts of interest to declare.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that ethical approval for publication of this service evaluation study was not required by their local Ethics Committee.







