Introduction
Acute lymphoblastic leukemia (ALL) is the most common diagnosis of childhood cancer. As a result of tremendous improvements in modern treatment, the five-year event-free survival is now approaching 90% in developed countries (Jeha et al., Reference Jeha, Pei, Choi, Cheng, Sandlund, Coustan-Smith, Campana, Inaba, Rubnitz, Ribeiro, Gruber, Raimondi, Khan, Yang, Mullighan, Downing, Evans, Relling and Pui2019; Toft et al., Reference Toft, Birgens, Abrahamsson, Griškevičius, Hallböök, Heyman, Klausen, Jónsson, Palk, Pruunsild, Quist-Paulsen, Vaitkeviciene, Vettenranta, Åsberg, Frandsen, Marquart, Madsen, Norén-Nyström and Schmiegelow2018). However, research suggests that a subgroup of survivors show neurocognitive sequelae many years into survivorship (Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013).
In childhood ALL survivors, neurocognitive sequelae have traditionally been attributed to cranial radiation therapy (Hardy et al., Reference Hardy, Krull, Wefel and Janelsins2018; Krull et al., Reference Krull, Hardy, Kahalley, Schuitema and Kesler2018). Cranial radiation therapy has been shown to impact the severity of neurocognitive impairments, with higher doses relating to higher severity rates (Zhou et al., Reference Zhou, Zhuang, Lin, Michelson and Zhang2020). To help preserve neurocognitive functions, the treatment has gradually been replaced by intrathecal chemotherapy. Cranial radiation therapy was first omitted from the treatment of standard risk ALL in the 1980s (Hudson et al., Reference Hudson, Neglia, Woods, Sandlund, Pui, Kun, Robison and Green2012; Schmiegelow et al., Reference Schmiegelow, Forestier, Hellebostad, Heyman, Kristinsson, Söderhäll and Taskinen2010; Toft et al., Reference Toft, Birgens, Abrahamsson, Griškevičius, Hallböök, Heyman, Klausen, Jónsson, Palk, Pruunsild, Quist-Paulsen, Vaitkeviciene, Vettenranta, Åsberg, Frandsen, Marquart, Madsen, Norén-Nyström and Schmiegelow2018). From the year of the 2000 and onward, increasingly more patients with high-risk disease have also been cured without cranial radiation therapy (Pui & Evans, Reference Pui and Evans2013). Although chemotherapeutic agents appear to have less severe effects on neurocognition (Cheung & Krull, Reference Cheung and Krull2015), adverse brain changes (e.g., white matter reduction) (Zhou et al., Reference Zhou, Zhuang, Lin, Michelson and Zhang2020), and neurocognitive sequelae (van der Plas, Modi, et al., Reference van der Plas, Modi, Li, Krull and Cheung2021) have been demonstrated in survivors of childhood ALL treated without cranial radiation therapy as well. Studies of long-term (min. five years post-diagnosis, Cheung & Krull, Reference Cheung and Krull2015) survivors in adulthood have documented mostly normal intellectual functions with specific impairments related to processing speed, attention, memory, and executive functions (Chiou et al., Reference Chiou, Lin, Liao and Yang2019; Edelmann et al., Reference Edelmann, Ogg, Scoggins, Brinkman, Sabin, Pui, Srivastava, Robison, Hudson and Krull2013; Elens et al., Reference Elens, Deprez, Danckaerts, Bijttebier, Labarque, Uyttebroeck, Van Gool, D’Hooge and Lemiere2017; Kanellopoulos et al., Reference Kanellopoulos, Andersson, Zeller, Tamnes, Fjell, Walhovd, Westlye, Fosså and Ruud2016; Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013). Executive functions are higher-level cognitive control processes, which contribute to the regulation of thoughts and goal-directed behavior (Friedman & Miyake, Reference Friedman and Miyake2017; Miyake & Friedman, Reference Miyake and Friedman2012), essential for adult daily-life and wellbeing (Friedman & Miyake, Reference Friedman and Miyake2017). However, a long period of follow-up time is needed to evaluate neurocognitive outcome in adulthood. As such, there are still few studies that have examined neurocognitive outcome associated with contemporary chemotherapy protocols in this population (Schmiegelow et al., Reference Schmiegelow, Forestier, Hellebostad, Heyman, Kristinsson, Söderhäll and Taskinen2010; Toft et al., Reference Toft, Birgens, Abrahamsson, Griškevičius, Hallböök, Heyman, Klausen, Jónsson, Palk, Pruunsild, Quist-Paulsen, Vaitkeviciene, Vettenranta, Åsberg, Frandsen, Marquart, Madsen, Norén-Nyström and Schmiegelow2018).
Most research has focused on treatment and disease factors in relation to neurocognitive outcome. It has previously been stated that treatment burden (Hardy et al., Reference Hardy, Krull, Wefel and Janelsins2018; Krull et al., Reference Krull, Hardy, Kahalley, Schuitema and Kesler2018), female sex (Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013; van der Plas, Qiu, et al., Reference van der Plas, Qiu, Nieman, Yasui, Liu, Dixon, Jacola, Kadan-Lottick, Weldon, Weil, Jacola, Gibson, Leisenring, Oeffinger, Hudson, Robison, Armstrong and Krull2021), and younger age at diagnosis (Jacola et al., Reference Jacola, Krull, Pui, Pei, Cheng, Reddick and Conklin2016; Sherief et al., Reference Sherief, Sanad, ElHaddad, Shebl, Abdelkhalek, Elsafy and Attia2018) increase the likelihood of neurocognitive sequelae. However, there is also a need to explore additional moderating factors, to facilitate the identification, rehabilitation, and prognosis of neurocognitive impairments (Zhou et al., Reference Zhou, Zhuang, Lin, Michelson and Zhang2020).
A prevalent (Hamre et al., Reference Hamre, Zeller, Kanellopoulos, Kiserud, Aakhus, Lund, Loge, Fosså and Ruud2013; van Deuren et al., Reference van Deuren, Penson, van Dulmen-den Broeder, Grootenhuis, van der Heiden-van der Loo, Bronkhorst, Blijlevens, Streefkerk, Teepen, Tissing, van der Pal, van den Heuvel-Eibrink, Versluys, Bresters, van Leeuwen, Ronckers, Kremer, Knoop and Loonen2022), distressing (Hamre et al., Reference Hamre, Zeller, Kanellopoulos, Kiserud, Aakhus, Lund, Loge, Fosså and Ruud2013; Kanellopoulos et al., Reference Kanellopoulos, Hamre, Dahl, Fosså and Ruud2013), and relatively persistent (Irestorm et al., Reference Irestorm, Steur, Kaspers, Van Eijkelenburg, Van der Sluis, Dors, Van den Bos, Tissing, Grootenhuis and Van Litsenburg2023; Zeller et al., Reference Zeller, Loge, Kanellopoulos, Hamre, Wyller and Ruud2014) symptom in survivors of childhood ALL is fatigue. Fatigue may be described as “a sense of tiredness and lack of energy, distinct from sadness and weakness” (Krupp et al., Reference Krupp, Alvarez, LaRocca and Scheinberg1988). Approximately ¼ of childhood ALL survivors report severe fatigue in adulthood (van Deuren et al., Reference van Deuren, Penson, van Dulmen-den Broeder, Grootenhuis, van der Heiden-van der Loo, Bronkhorst, Blijlevens, Streefkerk, Teepen, Tissing, van der Pal, van den Heuvel-Eibrink, Versluys, Bresters, van Leeuwen, Ronckers, Kremer, Knoop and Loonen2022). While several studies have demonstrated an association between fatigue and mental distress, research regarding the association with neurocognition is surprisingly limited (van Deuren et al., Reference van Deuren, Boonstra, van Dulmen-den Broeder, Blijlevens, Knoop and Loonen2020). Earlier research has revealed an association between fatigue and neurocognitive impairments (Clanton et al., Reference Clanton, Klosky, Li, Jain, Srivastava, Mulrooney, Zeltzer, Stovall, Robison and Krull2011), which may be explained by a lower mental capacity in fatigued individuals (Meeske et al., Reference Meeske, Siegel, Globe, Mack and Bernstein2005). However, this research is limited by self-report methodology only (Clanton et al., Reference Clanton, Klosky, Li, Jain, Srivastava, Mulrooney, Zeltzer, Stovall, Robison and Krull2011) and poorly specified neurocognitive domains (Meeske et al., Reference Meeske, Siegel, Globe, Mack and Bernstein2005; Rueegg et al., Reference Rueegg, Gianinazzi, Rischewski, Beck Popovic, von der Weid, Michel and Kuehni2013). In addition, one study on long-term adolescent survivors showed that females are especially vulnerable to the effects of fatigue on executive functions, processing speed, and attention (Cheung et al., Reference Cheung, Brinkman, Mulrooney, Mzayek, Liu, Banerjee, Panoskaltsis‐Mortari, Srivastava, Pui, Robison, Hudson and Krull2017). Still, little is known about this sex difference in adulthood.
Long-term survivors of ALL also report increased levels of tension headaches, migraines (Khan et al., Reference Khan, Hudson, Ledet, Morris, Pui, Howard, Krull, Hinds, Crom, Browne, Zhu, Rai, Srivastava and Ness2014), and back pain (Bowers et al., Reference Bowers, Griffith, Gargan, Cochran, Kleiber, Foxwell, Farrow-Gillespie, Orlino and Germann2012). Some survivors experience neuropathy (Kandula et al., Reference Kandula, Park, Cohn, Krishnan and Farrar2016), which can cause burning pain, numbness or hypersensitivity to touch. With the development of more effective cancer treatment for childhood ALL, there has been an increase in reports of cancer-related pain (Ness et al., Reference Ness, Hudson, Jones, Leisenring, Yasui, Chen, Stovall, Gibson, Green, Neglia, Henderson, Casillas, Ford, Effinger, Krull, Armstrong, Robison, Oeffinger and Nathan2017). This could possibly be due to more children with higher risk disease, being cured by more intensive treatments (e.g., >10 doses of intrathecal chemotherapy (Khan et al., Reference Khan, Hudson, Ledet, Morris, Pui, Howard, Krull, Hinds, Crom, Browne, Zhu, Rai, Srivastava and Ness2014)), in the more recent cohorts. As such, pain could be a particularly relevant factor in understanding neurocognitive sequelae following contemporary chemotherapy regimens. Due to the biological salience of pain (Moriarty et al., Reference Moriarty, McGuire and Finn2011), pain may occupy a significant amount of cognitive resources (e.g., attention) (Stone et al., Reference Stone, Karlson, Heathcote, Rosenberg and Palermo2018) and have a negative impact on neurocognitive performance (Moriarty et al., Reference Moriarty, McGuire and Finn2011). Consistent with this idea, emerging research shows that pain interference in long-term, adult survivors of childhood cancer has adverse effects on the performance of attention, executive functions, processing speed, and memory (Tonning Olsson et al., Reference Tonning Olsson, Alberts, Li, Ehrhardt, Mulrooney, Liu, Pappo, Bishop, Anghelescu, Srivastava, Robison, Hudson, Ness, Krull and Brinkman2021). However, the impact of pain interference on neurocognition in long-term survivors of childhood ALL specifically, remains to be examined (Stone et al., Reference Stone, Karlson, Heathcote, Rosenberg and Palermo2018).
The first aim of the current study was to map neurocognitive outcome in long-term survivors of childhood ALL, treated with chemotherapy, but without cranial radiation therapy. Both performance-based and self-report measures were used for this purpose. The second aim of this study was to examine factors associated with neurocognitive outcome in this population. We examined the impact of known risk factors (i.e., age at diagnosis, sex, and disease/treatment burden) on neurocognitive functioning. It was hypothesized that younger age at diagnosis, female sex, and more intensive treatment increased the risk of poor neurocognitive outcome. Furthermore, we explored the influence of pain interference and fatigue severity on neurocognitive functioning and whether females were more vulnerable to the effects of fatigue on neurocognition in adulthood. It was expected that fatigue and pain would negatively affect neurocognition.
Methods
Participants and procedures
The Cancer Registry of Norway identified all individuals diagnosed with ALL between 1980 and 2015 at age below 18 and minimum five years post-diagnosis, in the South-Eastern and Middle regions of Norway. Adults (>18 and <40 years) who were alive in 2020 and 2021, without relapse of ALL within the last five years, and treated at Oslo University Hospital or St. Olavs Hospital in Norway, were eligible to participate in the study. Individuals with a history of premorbid CNS disease or injury (e.g., cerebral palsy) were excluded. The study was part of a larger clinical trial (clinialtrials.gov: NCT04541056) where participants with executive functioning complaints were further invited to participate in cognitive rehabilitation. It was clearly stated that neurocognitive sequelae were not a prerequisite for participation in the present study. A total of 143 individuals received an invitation letter, with 57 individuals eventually participating (40% participation rate). The research was completed in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants and the study was approved by the Regional Committee for Medical Research Ethics in Central Norway (2018/1810). Three participants were excluded from analyses due to substance abuse and a sensory impairment. One was not included due to having received cranial radiation therapy. Thus, a total of 53 survivors (Mean age = 24.40, SD = 4.41, 51% females) are included in the current study (Table 1).
Table 1. Demographic characteristics of the sample (N = 53)
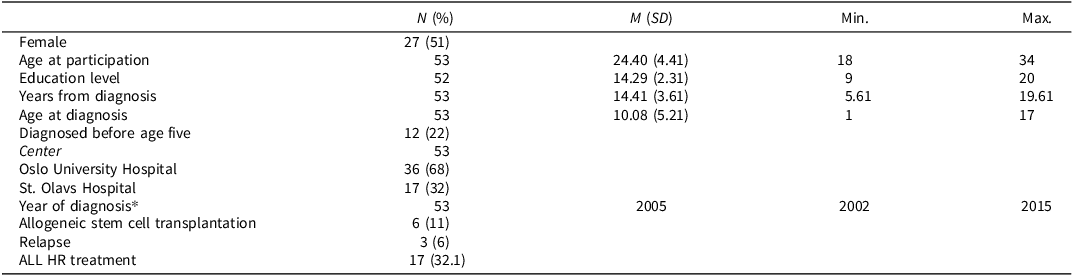
Note. M = mean, SD = standard deviation. Education level = years of education. *Median reported for year of cancer diagnosis. ALL = acute lymphoblastic leukemia, HR = high-risk.
Demographic and treatment characteristics were collected from a semi-structured interview, The Cancer Registry and the participants’ hospital records. From the latter, we collected information about diagnosis, date of diagnosis and treatment start, treatment protocols, stem cell transplantation, radiation therapy, and relapse. All participants had received ALL treatment according to a strict protocol, most frequently NOPHO ALL 2000 (Schmiegelow et al., Reference Schmiegelow, Forestier, Hellebostad, Heyman, Kristinsson, Söderhäll and Taskinen2010) (N = 35) and NOPHO ALL 2008 (Toft et al., Reference Toft, Birgens, Abrahamsson, Griškevičius, Hallböök, Heyman, Klausen, Jónsson, Palk, Pruunsild, Quist-Paulsen, Vaitkeviciene, Vettenranta, Åsberg, Frandsen, Marquart, Madsen, Norén-Nyström and Schmiegelow2018) (N = 13). Treatment duration for these protocols is 2–2.5 years from diagnosis (Schmiegelow et al., Reference Schmiegelow, Forestier, Hellebostad, Heyman, Kristinsson, Söderhäll and Taskinen2010). The remaining (N = 5) had received other treatment protocols (e.g., Hammersmith/modified Hammersmith) (Bersvendsen et al., Reference Bersvendsen, Kolstad, Blystad, Aurlien, Fosså, Kvaløy, Holte and Lauritzsen2014). The protocols stratified between a high-risk and a non-high-risk treatment approach based on biological factors associated with prognosis. The high-risk approaches had more intensive, more types, and higher cumulative doses of chemotherapy. Details and exact doses of chemotherapy are not collected in this study.
Participants took part in neurocognitive testing and completed self-report questionnaires. Neurocognitive testing took place in a dedicated room and lasted approximately four hours including short breaks. The order of testing was fixed. Survivors were offered the opportunity to participate over two subsequent days, and all survivors had a one-hour lunch break. Participants who were unable to attend physically (e.g., due to the Covid-19 pandemic), were asked to respond to self-report questionnaires only (N = 2). Various infection control measures (e.g., plexiglass, disinfection of material) were employed during testing.
Measures
Performance-based neurocognitive tests
The subtests Block design, Matrix reasoning, Similarities, and Vocabulary (scaled scores, M = 10, SD = 3) from the Wechsler Adult Intelligence Scale-IV (WAIS-IV) (Weschler, Reference Weschler2008) were used to calculate the general ability index (GAI, IQ scores, M = 100, SD = 15) as an estimation of intellectual functioning. In addition, the Digit span and Letter-number sequencing were used as measures of working memory capacity (Scaled scores, M = 10, SD = 3).
California Verbal Learning Test 2nd Edition (CVLT-II) was used to characterize auditory attention span, verbal learning and memory. List A, trial 1 (M = 0, SD = 3) was used to assess auditory attention span, the overall correct recall from list A 1-5 (M = 50, SD = 10) was used to assess verbal learning. Short-delay free recall and long-delay free recall (M = 0, SD = 3) were used to measure verbal memory.
Conner’s Continuous Performance Test 3rd Edition (CPT-3) (Conners, Reference Conners2014) was used to assess inhibitory control and focused attention (M = 50, SD = 10). Specifically, Commissions and detectability were employed as measures of inhibitory control and focused attention respectively. Scores were converted to T-scores (M = 50, SD = 10) and reversed so that higher scores reflect fewer commission errors and better performance.
The Trail Making Test (TMT) from the DKEFS (Delis et al., Reference Delis, Kaplan and Kramer2001) was used to measure cognitive set-shifting (condition 4). Here, the participant is asked to shift between number and letter sequencing. To assess processing speed, conditions 2 (number sequencing) and 3 (letter sequencing) were employed. Scores reflect completion time, and raw scores were converted to scaled scores (M = 10, SD = 3), where higher scores reflect better performance.
The Color-Word Interference test (CWIT) from the Delis–Kaplan Executive Function System (DKEFS) was used to assess inhibition and cognitive set-shifting (Delis et al., Reference Delis, Kaplan and Kramer2001). Condition 3 was used for inhibition and condition 4 was employed as a measure of set-shifting. To assess processing speed, conditions 1 (color naming) and 2 (word reading) were used. Primary scores were computed for completion time, and raw scores were converted to scaled scores (M = 10, SD = 3), where higher scores reflect better performance.
A computer-based version of The Wisconsin Card Sorting Test (WCST-4) (Heaton & Staff, Reference Heaton and Staff1993) used to assess set-shifting and problem-solving capacity (Lezak et al., Reference Lezak, Howieson, Bigler and Tranel2012). T-scores (M = 50, SD = 10) were generated, with higher scores reflecting better performance.
Self-report questionnaires
Behavior Rating Inventory of Executive Functioning – Adult Version (BRIEF-A) (Gioia, Reference Gioia2000; Roth et al., Reference Roth, Gioia and Isquith2005) was used to assess the perception of daily-life executive functions. Participants report the frequency of daily-life executive functioning problems (e.g., I have trouble finding things, in my room, in my closet, on my desk) during the past six months on a scale from 1 (Never) to 3 (Often). The questionnaire provides the summary score Global Executive Composite (GEC) and the two index scores: the Behavioral Regulation Index (BRI) and the Metacognitive Index (MI). The BRI includes the subscales of Inhibit, Shift, Emotional control and Self-monitor and reflects the behavioral and emotional aspects of executive functions. The MI includes the subscales Initiate, Working Memory, Plan/Organize, Task Monitor and Organization of Materials and reflects the cognitive aspects of executive functions. Raw scores were converted to T-scores (M = 50, SD = 10), where higher scores indicate worse executive functions. The recommended clinical cutoff for this measure is T ≥ 65 (Roth et al., Reference Roth, Gioia and Isquith2005). Data from healthy Norwegian adults indicate that the normative mean in Norway is at least ½ SD below that of the U.S. normative mean (i.e., M = 45) (Løvstad et al., Reference Løvstad, Sigurdardottir, Andersson, Grane, Moberget, Stubberud and Solbakk2016), suggesting a clinical cutoff of T ≥ 60 might be more appropriate.
The Fatigue Severity Scale (FSS) was used to characterize fatigue (Krupp et al., Reference Krupp, LaRocca, Muir-Nash and Steinberg1989). Participants responded to statements about how fatigue interferes with certain activities, on a scale from 1 (strongly disagree) to 7 (strongly agree). FSS has been used to measure fatigue in multiple clinical populations (Lerdal, Reference Lerdal2021). High correlations between FSS and other measures of fatigue (e.g., r = −0.76 with the vitality scale from Short-Form-36) and excellent test–retest reliability have been reported (Gencay-Can & Can, Reference Gencay-Can and Can2012; Kleinman et al., Reference Kleinman, Zodet, Hakim, Aledort, Barker, Chan, Krupp and Revicki2000). Additionally, good psychometric properties have been demonstrated for the Norwegian version of FSS, with satisfactory reliability (i.e., internal consistency (Lerdal et al., Reference Lerdal, Wahl, Rustoen, Hanestad and Moum2005). Based on previous reports on the prevalence of fatigue in the Norwegian population, a FSS score ≥5 was interpreted as indicative of severe fatigue (Schanke et al., Reference Schanke, Stanghelle, Andersson, Opheim, Strom and Solbakk2002).
Patient reported outcome measure system (PROMIS) short form, version 1.1-Pain Interference was employed to evaluate pain interference in the participant’s life. The degree to which pain interferes with daily-life (i.e., family life, work, social activity) was reported on eight items, scaled from 1 (not at all) to five (very much). T-scores (M = 50, SD = 10) were calculated using the online scoring at www.assessmentcenter.net/ac_scoringservice. The Norwegian version has shown adequate reliability and validity, indicating that the measure is suitable for use in the Norwegian population (Rimehaug et al., Reference Rimehaug, Kaat, Nordvik, Klokkerud and Robinson2022).
Statistical analysis
Statistics were analyzed in SPSS 28 and STATA 17. Differences in age, age at diagnosis, follow-up time and sex between participants and non-participants were examined. A chi-square test of homogeneity, independent sample t test or Mann−Whitney U test was used for this purpose. One sample t tests or Wilcoxon signed-rank tests were performed to compare the sample neurocognitive performance and executive functioning complaints to the normative means or medians. Preliminary analyses were conducted to determine whether assumptions (i.e., normality and no outliers) were violated. Boxplots, histograms, QQ-plots, values of skewness and kurtosis, Shapiro–Wilk were inspected. If assumptions were violated, a non-parametric statistical test was employed (i.e., Wilcoxon signed-rank test). A significance value of p < 0.01 was used to partially control for multiple comparisons.
Furthermore, multiple linear regression analyses were performed to evaluate factors associated with neurocognitive outcome (i.e., performance and self-reported). Analyses to assess assumptions related to linearity, homoscedasticity, outliers, multicollinearity, and normality were conducted. Risk factors (age at diagnosis, sex, risk group), fatigue severity, and pain interference were entered as independent variables. Risk group was used as a measure of disease severity and treatment intensity. Participants were categorized into non-high-risk or high-risk based on risk stratification associated with their treatment protocols (e.g., NOPHO ALL 2000 and 2008) (Schmiegelow et al., Reference Schmiegelow, Forestier, Hellebostad, Heyman, Kristinsson, Söderhäll and Taskinen2010; Toft et al., Reference Toft, Birgens, Abrahamsson, Griškevičius, Hallböök, Heyman, Klausen, Jónsson, Palk, Pruunsild, Quist-Paulsen, Vaitkeviciene, Vettenranta, Åsberg, Frandsen, Marquart, Madsen, Norén-Nyström and Schmiegelow2018). In cases where participants had been treated with Hammersmith protocols (Bersvendsen et al., Reference Bersvendsen, Kolstad, Blystad, Aurlien, Fosså, Kvaløy, Holte and Lauritzsen2014), IntReALL protocols (von Stackelberg et al., Reference von Stackelberg, Bourquin, Zimmermann, Revesz, Attarbaschi, Ferster and Elhasid2022; von Stackelberg et al., Reference von Stackelberg, Qi, Saha, Locatelli, Moschandreas and Love2017), protocols for Philadelphia positive ALL (Biondi et al., Reference Biondi, Schrappe, De Lorenzo, Castor, Lucchini, Gandemer, Pieters, Stary, Escherich, Campbell, Li, Vora, Aricò, Röttgers, Saha and Valsecchi2012), and/or had a relapse or stem cell transplantation, they were categorized into the high-risk group. Age at diagnosis was calculated as the time from date of birth (month and year) to date of diagnosis (month and year). If date of the diagnosis was missing, the date of chemotherapy treatment start was used. For the regression analyses, age at diagnosis was dichotomized into under/over 10 years. Exploratory t tests comparing neurocognitive outcome between participants under/over five years at diagnosis were performed as well. To explore whether females were more vulnerable to the effects of fatigue on neurocognitive outcome, the interaction between sex and fatigue severity was analyzed. A significance value of p < 0.01 was used to partially control for multiple analyses.
Results
Demographic and treatment characteristics
A comparison of participants and eligible non-participants can be found in Supplementary Table 2. Median age at investigation was significantly higher in participating survivors than non-participants. Participants also had a higher age at diagnosis compared to non-participants treated at Oslo University Hospital.
Demographic and treatment characteristics of the sample are reported in Table 1. According to the semi-structured interview, none (N = 52, missing = 1) had received cognitive rehabilitation at the time of study participation. However, one participant used stimulant medication (i.e., Ritalin) and two had received rehabilitation directed at chronic fatigue.
Neurocognitive outcome
Survivors demonstrated significantly better general intellectual abilities, but significantly poorer auditory attention span (CVLT-II, list A trial 1), inhibitory control (CPT-3 commissions), and oral processing speed (CWIT color naming) compared to the normative mean (Table 2). Although shifting (cond. 4, TMT, cond. 4, CWIT, pers. response, WCST-4) was not significantly different from the normative mean, performance was significantly poorer than the normative mean when we controlled for processing speed (TMT, shifting vs. combined number letter sequencing). We examined these domains in greater detail to establish how many participants might be classified as having a neurocognitive impairment (i.e., score 1.5 SD below the normative mean). The number of participants showing an impairment was 12 (24%) for auditory attention span (CVLT-II, list A trial 1), 13 (26%) for inhibitory control (CPT-3, commissions), 14 (28%) for shifting (TMT, switching vs. combined number letter sequencing), and 18 (35%) for oral processing speed (CWIT color naming). On a group level, there were no impairments in working memory (WAIS-IV, digit span, letter-number sequencing), verbal learning and memory (CVLT-II, list A trial 1-5, short and long delay), problem-solving/set-shifting (WCST-4, pers. response, pers. errors), and visual processing speed (TMT number sequencing).
Table 2. Performance-based and self-reported neurocognitive outcome
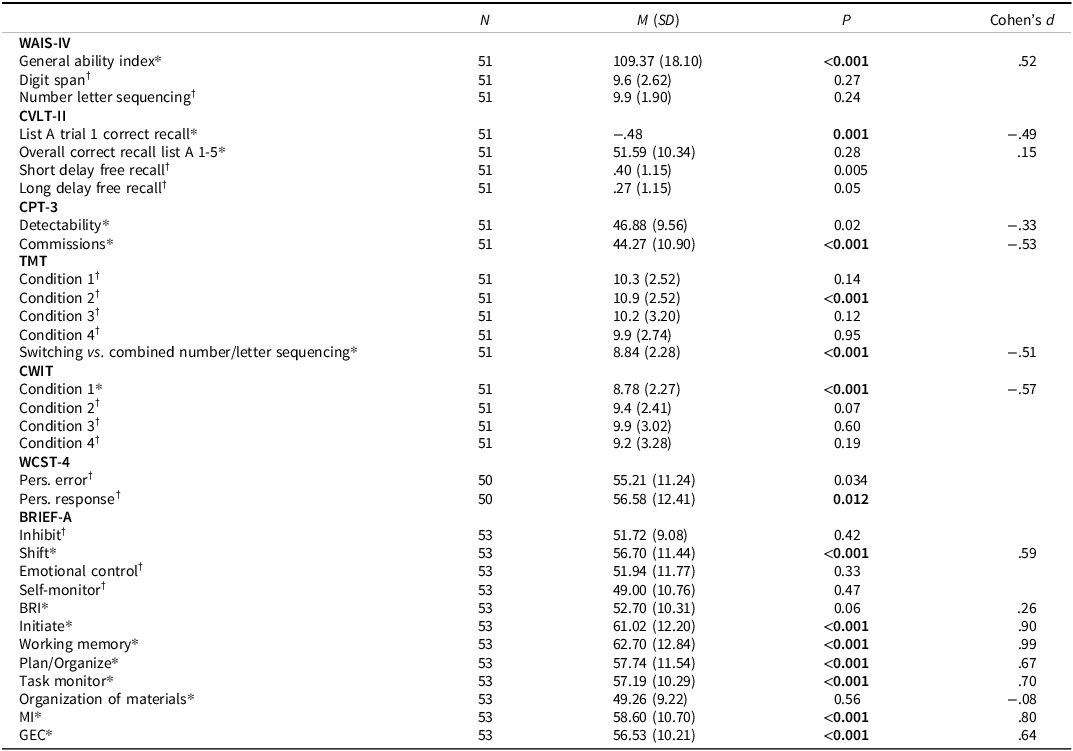
Note. M = mean, SD = standard deviation. WAIS-IV = Wechsler Adult Intelligence Scale-IV, CVLT-II = The California Verbal Learning Test-II, CPT-3 = Conners’ Continuous Performance Test-3, TMT = Trail Making Test, CWIT = Color-Word Interference Test, WCST-4 = Wisconsin Card Sorting Test-4, BRIEF-A = Behavior Rating Inventory of Executive Functioning- Adult Version, BRI = Behavior Regulation Index, MI = Metacognitive Index, GEC = Global Executive Composite.
*One sample t test.
†Wilcoxon signed-rank test. Higher scores indicate better performance, except for BRIEF-A where higher scores indicate increased symptom level. The U.S. normative mean was used as comparison for BRIEF-A.
Self-reported executive functioning complaints were significantly higher than the US normative mean for the summary scores MI and GEC. The subscales shift, initiate, working memory, plan/organize, and task monitor were all significantly higher than the normative mean. When we examined self-reported executive functioning complaints in greater detail, 16 (30%) and 11 (21%) scored above the U.S. clinical cutoff T ≥ 65 for the MI and GEC scales respectively. We examined the number of clinical cases based on the Norwegian cutoff of T ≥ 60 as well. This resulted in an even higher level of clinical cases with 25 (47%) in the MI domain and 19 (36%) in the GEC.
Risk factors and predictors of neurocognitive outcome
None of the domains identified as neurocognitive impairments were significantly associated with any of the risk factors, age at diagnosis (under/over 10 years), risk group (high-risk vs. non-high risk), and sex (Table 3). Exploratory t tests did not show significant differences between participants diagnosed before and after five years of age.
Table 3. Age at diagnosis, risk group and sex as risk factors for neurocognitive outcome

Note. For Sex: male was coded as 1, female as 0. CVLT-II = The California Verbal Learning Test 2nd edition, CPT-3 = Conners’ Continuous Performance Test-3, TMT = Trail Making Test, CWIT = Color-Word Interference Test, GEC = Global Executive Composite, BRIEF-A = Behavior Rating Inventory of Executive Functioning- Adult Version, MI = Metacognitive Index.
The descriptive statistics for fatigue severity and pain interference are reported in Table 4. Furthermore, multiple linear regression analyses showed that fatigue severity was significantly associated with both self-reported metacognitive and general executive functioning complaints (Table 5). However, no significant associations were found for auditory attention span, switching versus combined number letter sequencing, inhibitory control, and processing speed. Furthermore, there was no significant interaction between sex and fatigue for any of the above neurocognitive impairments (see Supplementary material, Table 1).
Table 4. Descriptive statistics of fatigue severity and pain interference

Note. M = mean, SD = standard deviation. FSS = Fatigue Severity Scale, PROMIS = patient reported outcome measure system- short form, version 1.1 pain interference, PROMIS - Pain interference reported as T-scores (M = 50, SD = 10), with impairment referring to scores 1 SD above the mean. FSS reported as raw scores, and impairment referring to FSS > 5.
Table 5. Fatigue severity and pain interference as predictors of neurocognitive outcome

Note. CVLT-II = The California Verbal Learning Test 2nd edition, FSS = Fatigue Severity Scale, PROMIS = patient reported outcome measure system- short form, version 1.1 pain interference, CPT-3 = Conners’ Continuous Performance Test-3, TMT = Trail Making Test, CWIT = Color-Word Interference Test, GEC = Global Executive Composite, BRIEF-A = Behavior Rating Inventory of Executive Functioning- Adult Version, MI = Metacognitive Index.
Discussion
The first aim of the current study was to examine neurocognitive outcome in long-term, adult survivors of childhood ALL, treated without cranial radiation therapy. The participants had received anticancer treatment in which cranial radiation therapy was omitted, thus including a fair number of survivors treated for high-risk ALL with intensive chemotherapy only (i.e., 30% of the sample). In line with prior work in this population (Elens et al., Reference Elens, Deprez, Danckaerts, Bijttebier, Labarque, Uyttebroeck, Van Gool, D’Hooge and Lemiere2017; Kanellopoulos et al., Reference Kanellopoulos, Andersson, Zeller, Tamnes, Fjell, Walhovd, Westlye, Fosså and Ruud2016; Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013), we report performance-based impairments within the executive functions, processing speed, and attention domains. Moreover, rates of executive functioning impairments (i.e., 26−28%) are very similar to that reported in an earlier Norwegian study (i.e., 31%) (Kanellopoulos et al., Reference Kanellopoulos, Andersson, Zeller, Tamnes, Fjell, Walhovd, Westlye, Fosså and Ruud2016). Over one decade after childhood ALL, we also report intact intellectual abilities compared to the normative mean. This is consistent with earlier research with shorter follow-up time (Conklin et al., Reference Conklin, Krull, Reddick, Pei, Cheng and Pui2012; Krull et al., Reference Krull, Cheung, Liu, Fellah, Reddick, Brinkman, Kimberg, Ogg, Srivastava, Pui, Robison and Hudson2016), thus indicating that impairments are confined to specific neurocognitive domains. However, unlike some previous research on long-term, adult survivors (Edelmann et al., Reference Edelmann, Ogg, Scoggins, Brinkman, Sabin, Pui, Srivastava, Robison, Hudson and Krull2013; Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013), we did not find evidence of learning and memory impairments. Our results were more consistent with a study in younger survivors of childhood ALL (Lofstad et al., Reference Lofstad, Reinfjell, Weider, Diseth and Hestad2019), showing compensating mechanisms in relation to learning. In the present study, the first trial of CVLT (auditory attention span) was below the normative mean, but verbal learning and memory were not. This might suggest that survivors with attention impairments were able to compensate and still achieve normal learning outcomes. Still, it should be noted that the current study sample is relatively young compared to some previous studies in which broader impairments have been reported (Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013). Research has documented signs of accelerated aging in adult survivors of childhood ALL (Ness et al., Reference Ness, Kirkland, Gramatges, Wang, Kundu, McCastlain, Li-Harms, Zhang, Tchkonia, Pluijm and Armstrong2018; Schuitema et al., Reference Schuitema, Alexander, Hudson, Krull and Edelstein2021). Consequently, memory impairments may first emerge later in adulthood for some survivors (at a mean age of 31.8 according to Phillips et al., Reference Phillips, Stratton, Williams, Ahles, Ness, Cohen, Edelstein, Yasui, Oeffinger, Chow, Howell, Robison, Armstrong, Leisenring and Krull2023).
Interestingly, the largest effect sizes related to neurocognitive outcome were found for self-reported executive functioning complaints (Cohens d = 0.59−0.99). Compared with data from healthy adults from a Norwegian study (Løvstad et al., Reference Løvstad, Sigurdardottir, Andersson, Grane, Moberget, Stubberud and Solbakk2016), 36−47% of the sample was in the clinical range, with working memory, planning, organization, and task-monitoring being most prominent. Although healthy controls in research may not be representative of the general population, this contrasts with earlier research in long-term, adult survivors showing much lower rates (i.e., 10−16%) of executive functioning complaints (Leclerc et al., Reference Leclerc, Lippé, Bertout, Chapados, Boulet‐Craig, Drouin, Krajinovic, Laverdière, Michon, Robaey, Rondeau, Sinnett and Sultan2020; Tamnes et al., Reference Tamnes, Zeller, Amlien, Kanellopoulos, Andersson, Due‐Tønnessen, Ruud, Walhovd and Fjell2015). Impaired insight or long-term adaptation has previously been suggested to characterize long-term survivors in adulthood (Kanellopoulos et al., Reference Kanellopoulos, Andersson, Zeller, Tamnes, Fjell, Walhovd, Westlye, Fosså and Ruud2016; Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013). However, our study differs from these former studies in important ways. One earlier study (Leclerc et al., Reference Leclerc, Lippé, Bertout, Chapados, Boulet‐Craig, Drouin, Krajinovic, Laverdière, Michon, Robaey, Rondeau, Sinnett and Sultan2020) included survivors mostly treated with cranial radiation therapy. For various reasons (e.g., lower insight), this subgroup of survivors may report fewer executive functioning problems in daily life than those treated with more contemporary chemotherapy protocols. Another earlier study, conducted in Norway (Tamnes et al., Reference Tamnes, Zeller, Amlien, Kanellopoulos, Andersson, Due‐Tønnessen, Ruud, Walhovd and Fjell2015), did not take data from healthy Norwegian adults into account. As such, executive functioning complaints might have been underestimated. Until now, research on rehabilitation for childhood cancer survivors has focused almost exclusively on children (Benzing et al., Reference Benzing, Spitzhüttl, Siegwart, Schmid, Grotzer, Heinks, Roebers, Steinlin, Leibundgut, Schmidt and Everts2020; Conklin et al., Reference Conklin, Ogg, Ashford, Scoggins, Zou, Clark, Martin-Elbahesh, Hardy, Merchant, Jeha, Huang and Zhang2015). However, the high level of executive functioning complaints reported in the present study underscores the need for executive functions rehabilitation in adult survivors as well. Since young adulthood is accompanied by increasing expectations and demands, rehabilitation directed at daily-life executive functions (Egset et al., Reference Egset, Weider, Stubberud, Hjemdal, Ruud, Hjort, Eilertsen, Sund, Røkke and Reinfjell2021) may be especially relevant for this population.
In disagreement with our hypothesis (Fellah et al., Reference Fellah, Cheung, Scoggins, Zou, Sabin, Pui, Robison, Hudson, Ogg and Krull2019; Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013), participants treated with high-risk ALL protocols did not demonstrate poorer neurocognitive outcome compared to those with a non-high-risk treatment. Additionally, we did not find support for the hypothesis stating female sex as a risk factor for poor neurocognitive outcome. Previous research has identified female sex and treatment burden as risk factors for neurocognitive sequelae in adulthood (Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013; van der Plas, Qiu, et al., Reference van der Plas, Qiu, Nieman, Yasui, Liu, Dixon, Jacola, Kadan-Lottick, Weldon, Weil, Jacola, Gibson, Leisenring, Oeffinger, Hudson, Robison, Armstrong and Krull2021). Still, these studies were conducted with much larger samples than ours (Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013; van der Plas, Qiu, et al., Reference van der Plas, Qiu, Nieman, Yasui, Liu, Dixon, Jacola, Kadan-Lottick, Weldon, Weil, Jacola, Gibson, Leisenring, Oeffinger, Hudson, Robison, Armstrong and Krull2021). Thus, any potential effects may not have been large enough to be detected in the current sample size. In addition, associations have typically been established with specific chemotherapeutic agents (e.g., methotrexate, Phillips et al., Reference Phillips, Stratton, Williams, Ahles, Ness, Cohen, Edelstein, Yasui, Oeffinger, Chow, Howell, Robison, Armstrong, Leisenring and Krull2023), which were not investigated in this study. Furthermore, since the mean age at diagnosis in this study was 10 years, we compared neurocognitive outcome above and below this age. Previous studies in younger survivors have shown that being diagnosed before age five is a neurocognitive risk factor (Conklin et al., Reference Conklin, Krull, Reddick, Pei, Cheng and Pui2012; Jacola et al., Reference Jacola, Krull, Pui, Pei, Cheng, Reddick and Conklin2016; Sherief et al., Reference Sherief, Sanad, ElHaddad, Shebl, Abdelkhalek, Elsafy and Attia2018). Still, none of the comparisons between groups showed significant differences in neurocognitive outcome in the current study. However, relatively few had been treated before the age of five, which may have impacted the results. Importantly, other factors may become more influential as survivors progress into young adulthood. This is why we also examined the impact of fatigue severity and pain interference on neurocognitive outcome.
Fatigue severity was the present study’s most significant predictor of neurocognitive outcome. In agreement with our expectation, more severe fatigue was associated with poorer neurocognitive outcomes (i.e., executive functioning complaints). Survivors with severe fatigue were more likely to report difficulties with the regulation of thoughts and goal-directed behavior in adult daily-life. This is in accordance with earlier studies showing a relationship between fatigue and neurocognitive impairments (e.g., having received special education services) (Meeske et al., Reference Meeske, Siegel, Globe, Mack and Bernstein2005; Rueegg et al., Reference Rueegg, Gianinazzi, Rischewski, Beck Popovic, von der Weid, Michel and Kuehni2013). The association between fatigue and executive functions may have implications for rehabilitation. As both fatigue and executive functions are potentially modifiable, future research should explore whether specific interventions (e.g., cognitive, and physical rehabilitation) could have a favorable impact on both outcomes in this population.
A strength of our study was the examination of fatigue in relation to neurocognitive performance in addition to self-reports. Still, no associations with performance-based measures were found. The adaptation of the testing schedule to accommodate participants with severe fatigue could have masked some of the effects of fatigue on test performance. It should also be noted that the current study only measured fatigue at one timepoint. Although severe fatigue in long-term survivorship can be an indication of chronic fatigue, the association between executive functions and fatigue over time (i.e., chronic fatigue) was not specifically examined. Furthermore, neurocognition in females was no more affected by fatigue than that of males. It is possible that sex differences previously detected by Cheung et al. (Reference Cheung, Brinkman, Mulrooney, Mzayek, Liu, Banerjee, Panoskaltsis‐Mortari, Srivastava, Pui, Robison, Hudson and Krull2017) are more salient in adolescence, in which females can be particularly vulnerable (Pfeifer & Allen, Reference Pfeifer and Allen2021). Still, our results are consistent with several other studies in the childhood cancer literature, that have reported similar levels of fatigue among males and females (Frederick et al., Reference Frederick, Kenney, Vrooman and Recklitis2016; Irestorm et al., Reference Irestorm, Steur, Kaspers, Van Eijkelenburg, Van der Sluis, Dors, Van den Bos, Tissing, Grootenhuis and Van Litsenburg2023; Zeller et al., Reference Zeller, Loge, Kanellopoulos, Hamre, Wyller and Ruud2014).
Somewhat surprisingly, we found no associations between neurocognitive sequelae and pain interference. However, existing research suggests that interference of pain is more frequent in survivors of soft-tissue sarcomas, non-Hodgkins lymphoma, Ewing sarcoma and/or osteosarcoma, and in those above the age of 30 years (Tonning Olsson et al., Reference Tonning Olsson, Alberts, Li, Ehrhardt, Mulrooney, Liu, Pappo, Bishop, Anghelescu, Srivastava, Robison, Hudson, Ness, Krull and Brinkman2021). Thus, the impact of pain interference on neurocognition may be less evident in long-term survivors of childhood ALL, in young adulthood. Recent research (Partanen et al., Reference Partanen, Alberts, Conklin, Krull, Pui, Anghelescu and Jacola2022), in younger survivors of childhood ALL, has, however, demonstrated associations between neuropathic pain and neurocognition. These specific associations warrant further study in long-term, adult survivors.
Strengths and limitations
This study is limited by a cross-sectional design. Pretreatment neurocognitive testing was not performed, which prevents any comparison to baseline performance. Thus, it is possible that other factors unrelated to disease and treatment have influenced the neurocognitive outcome of the studied sample. Another limitation of the current study is that it did not include a control group, which limits the conclusions that can be drawn regarding the neurocognitive outcome measures. This pertains especially to outcomes where Norwegian normative data was not available. Still, all neurocognitive measures used are standardized, and participants were compared with age-adjusted normative data, frequently used in Norwegian clinical practice.
The data reported in this manuscript was collected during the Covid-19 pandemic. Although recruitment continued until after the Norwegian society officially was back to normal everyday life, the data collection process was likely affected by the pandemic. The response rate was not optimal (overall 40% response rate). Although age at diagnosis was not available for all eligible non-participants, results suggested that participants were older at diagnosis (median = 12.00) compared to non-participants. Scandinavian children with leukemia are most frequently diagnosed at ages 1−5 years (National Quality Registry for Childhood Cancer, 2022), with a median of five years for those diagnosed with ALL before age 16 (Gustafsson et al., Reference Gustafsson, Kogner and Heyman2013). Hence, a possible selection bias should be kept in mind when interpreting the results. A younger age at diagnosis has been associated with more neurocognitive sequelae (Sherief et al., Reference Sherief, Sanad, ElHaddad, Shebl, Abdelkhalek, Elsafy and Attia2018). As such, the higher age at diagnosis in the current sample might influence the results in the direction of false negative findings. At the same time, the present study may also have attracted more individuals with neurocognitive complaints due to the inherent focus on neurocognitive sequelae (i.e., due to the associated clinical trial of cognitive rehabilitation). Furthermore, while the current sample was small compared to previous reports in long-term, adult survivors (Kanellopoulos et al., Reference Kanellopoulos, Andersson, Zeller, Tamnes, Fjell, Walhovd, Westlye, Fosså and Ruud2016; Krull et al., Reference Krull, Brinkman, Li, Armstrong, Ness, Srivastava, Gurney, Kimberg, Krasin, Pui, Robison and Hudson2013), our study is unique in presenting long-term adult survivors treated with Nordic protocols in which cranial radiation therapy was largely or totally omitted (Schmiegelow et al., Reference Schmiegelow, Forestier, Hellebostad, Heyman, Kristinsson, Söderhäll and Taskinen2010; Toft et al., Reference Toft, Birgens, Abrahamsson, Griškevičius, Hallböök, Heyman, Klausen, Jónsson, Palk, Pruunsild, Quist-Paulsen, Vaitkeviciene, Vettenranta, Åsberg, Frandsen, Marquart, Madsen, Norén-Nyström and Schmiegelow2018). The inclusion of participants from two of Norway’s largest pediatric hospitals (St Olavs Hospital and Oslo University Hospital), should also be considered a strength of the study, covering >60 % of the Norwegian childhood cancer population.
Conclusion
Long-term adult survivors of childhood ALL, treated without cranial radiation therapy demonstrate intact intellectual capacity and discrete neurocognitive impairments. However, continued neurocognitive follow-up of this group of survivors later in adulthood will be an important task for future research. Executive functions complaints in the metacognitive domain (i.e., working memory, planning, organization, task-monitoring) were frequently reported, which might indicate a need for rehabilitation programs targeting real-life functioning. The only significant predictor of neurocognitive impairment was fatigue severity, irrespective of survivor sex. The association between fatigue and executive functioning complaints may have implications for rehabilitation.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1355617724000080.
Acknowledgments
This study was funded by the Norwegian Cancer Society, with grant number 201842. Data were stored and managed on the TSD (Tjeneste for Sensitive Data) facilities, owned by the University of Oslo. The authors would like to thank Elna Hamilton Larsen and Katrine Aass Underhaug for assisting with medical journal extraction at Oslo University Hospital. The authors would also like to thank Magnhild Eitrem Røkke and Lisbet Moen for contributing to data collection in Trondheim and Synne Stadheim Øiestad, Henriette Hofsøy and Mari Arnesen for data collection in Oslo.
Competing interests
The authors have no conflicts of interest to declare.







