Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Domen, Jos
2018.
Minimally Invasive Transplantation of Primary Human Hepatocyte Inserts that Facilitate Vascularization.
Transplantation,
Vol. 102,
Issue. 9,
p.
1413.
Hauptmann, Nicole
Lian, Qilin
Ludolph, Johanna
Rothe, Holger
Hildebrand, Gerhard
and
Liefeith, Klaus
2019.
Biomimetic Designer Scaffolds Made of D,L-Lactide-ɛ-Caprolactone Polymers by 2-Photon Polymerization.
Tissue Engineering Part B: Reviews,
Vol. 25,
Issue. 3,
p.
167.
Lin, Dawn S Y
Guo, Feng
and
Zhang, Boyang
2019.
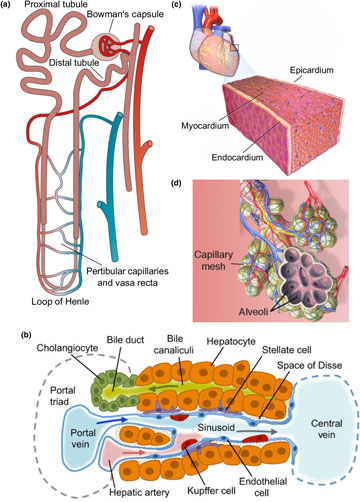
Modeling organ-specific vasculature with organ-on-a-chip devices.
Nanotechnology,
Vol. 30,
Issue. 2,
p.
024002.
Cui, Xiaolin
Li, Jun
Hartanto, Yusak
Durham, Mitchell
Tang, Junnan
Zhang, Hu
Hooper, Gary
Lim, Khoon
and
Woodfield, Tim
2020.
Advances in Extrusion 3D Bioprinting: A Focus on Multicomponent Hydrogel‐Based Bioinks.
Advanced Healthcare Materials,
Vol. 9,
Issue. 15,
Xie, Mengying
Wang, Zhiyi
Wan, Xinlong
Weng, Jie
Tu, Mengyun
Mei, Jin
Wang, Zhibin
Du, Xiaohong
Wang, Liangxing
and
Chen, Chan
2020.
Crosslinking effects of branched PEG on decellularized lungs of rats for tissue engineering.
Journal of Biomaterials Applications,
Vol. 34,
Issue. 7,
p.
965.
Yeleswarapu, Sriya
Chameettachal, Shibu
Kumar Bera, Ashis
and
Pati, Falguni
2020.
Xenotransplantation - Comprehensive Study.
Barbon, Silvia
Stocco, Elena
Dalzoppo, Daniele
Todros, Silvia
Canale, Antonio
Boscolo-Berto, Rafael
Pavan, Piero
Macchi, Veronica
Grandi, Claudio
De Caro, Raffaele
and
Porzionato, Andrea
2020.
Halogen-Mediated Partial Oxidation of Polyvinyl Alcohol for Tissue Engineering Purposes.
International Journal of Molecular Sciences,
Vol. 21,
Issue. 3,
p.
801.
Ghosal, Krishanu
Bhattacharjee, Upama
and
Sarkar, Kishor
2020.
Facile green synthesis of bioresorbable polyester from soybean oil and recycled plastic waste for osteochondral tissue regeneration.
European Polymer Journal,
Vol. 122,
Issue. ,
p.
109338.
Vardar, Elif
2020.
Biomaterials for Organ and Tissue Regeneration.
p.
441.
Sohn, Sogu
Buskirk, Maxwell Van
Buckenmeyer, Michael J.
Londono, Ricardo
and
Faulk, Denver
2020.
Whole Organ Engineering: Approaches, Challenges, and Future Directions.
Applied Sciences,
Vol. 10,
Issue. 12,
p.
4277.
Zakeri, Nima
Mirdamadi, Elnaz Sadat
Kalhori, Dianoosh
and
Solati‐Hashjin, Mehran
2020.
Signaling molecules orchestrating liver regenerative medicine.
Journal of Tissue Engineering and Regenerative Medicine,
Vol. 14,
Issue. 12,
p.
1715.
Aljabali, Alaa A. A.
Seetan, Khaled I.
Alshaer, Walhan
Abu-El-Rub, Ejlal
Obeid, Mohammad A.
Kamal, Dua
and
Tambuwala, Murtaza M.
2021.
Advances in Application of Stem Cells: From Bench to Clinics.
Vol. 69,
Issue. ,
p.
269.
Indurkar, Abhishek
Pandit, Ashish
Jain, Ratnesh
and
Dandekar, Prajakta
2021.
Plant based cross-linkers for tissue engineering applications.
Journal of Biomaterials Applications,
Vol. 36,
Issue. 1,
p.
76.
Pennarossa, Georgia
Arcuri, Sharon
De Iorio, Teresina
Gandolfi, Fulvio
and
Brevini, Tiziana A. L.
2021.
Current Advances in 3D Tissue and Organ Reconstruction.
International Journal of Molecular Sciences,
Vol. 22,
Issue. 2,
p.
830.
Prasathkumar, Murugan
and
Sadhasivam, Subramaniam
2021.
Chitosan/Hyaluronic acid/Alginate and an assorted polymers loaded with honey, plant, and marine compounds for progressive wound healing—Know-how.
International Journal of Biological Macromolecules,
Vol. 186,
Issue. ,
p.
656.
Wihadmadyatami, Hevi
and
Kusindarta, Dwi Liliek
2021.
Polysaccharides of Microbial Origin.
p.
1.
Wang, Mian
Li, Wanlu
Tang, Guosheng
Garciamendez‐Mijares, Carlos Ezio
and
Zhang, Yu Shrike
2021.
Engineering (Bio)Materials through Shrinkage and Expansion.
Advanced Healthcare Materials,
Vol. 10,
Issue. 14,
Ding, Aixiang
Jeon, Oju
Tang, Rui
Lee, Yu Bin
Lee, Sang Jin
and
Alsberg, Eben
2021.
Cell‐Laden Multiple‐Step and Reversible 4D Hydrogel Actuators to Mimic Dynamic Tissue Morphogenesis.
Advanced Science,
Vol. 8,
Issue. 9,
Jang, Jinah
Choi, Ji Young
Mahadik, Bhushan
and
Fisher, John P.
2021.
3D printing technologies forin vitrovaccine testing platforms and vaccine delivery systems against infectious diseases.
Essays in Biochemistry,
Vol. 65,
Issue. 3,
p.
519.
Qavi, Imtiaz
and
Tan, George Z.
2021.
Near-field electrospinning polycaprolactone microfibers to mimic arteriole-capillary–venule structure.
Progress in Biomaterials,
Vol. 10,
Issue. 3,
p.
223.