Introduction
In recent decades, oral nutritional supplements (ONS) have become widely used in nutrition therapy for disease-related malnutrition within many medical disciplines, e.g. oncology, geriatrics and surgery, and for renal, lung and gastrointestinal conditions(Reference Volkert, Beck and Cederholm1–Reference Ikizler, Burrowes and Byham-Gray6). However, adherence (or compliance) to ONS treatment can be challenging(Reference Gosney7–Reference Skladany, Vnencakova and Laffers9), and there is a lack of understanding about how best to facilitate ONS consumption and avoid wastage(Reference Lester, Kleijn and Cornacchia10).
Adherence to therapy is defined by the World Health Organization (WHO) as ‘The extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider.’(11). Adherence to ONS can therefore be referred to as the behaviour of consuming ONS in relation to a recommendation or prescription. High adherence is crucial to achieving optimal treatment success(11–Reference Gast and Mathes13) and is associated with higher nutrition intake(Reference Hubbard, Elia and Holdoway14), better nutritional status(Reference López-Medina, López-Rodriguez and Estornell-Gualde15–Reference Kobayashi, Ishigure and Mochizuki18) and a decreased risk of hospitalisation(Reference Seguy, Hubert and Robert19). Yet, adherence to therapy presents a major challenge, both in general(11) and specifically in relation to ONS. Hence, knowing how different factors impact ONS consumption is essential to improve nutrition therapy effectiveness. Previous studies have highlighted a range of barriers and facilitators (factors that hinder or help) relevant for ONS consumption(Reference Harris, Payne and Morrison20,Reference Wan, Yuan and Xue21) and have focused on selected populations and settings(Reference Gosney7,Reference Grass, Bertrand and Schäfer8,Reference McMurdo, Price and Shields22,Reference Lidoriki, Schizas and Mylonas23) where adherence to ONS is problematic.
From earlier studies, it is evident that adherence to nutrition therapy with ONS has a multifaceted nature. Hubbard and colleagues’ 2012 milestone systematic review article summarised compliance to ONS across all healthcare disciplines (n = 46), focusing on ONS and patient-related factors(Reference Hubbard, Elia and Holdoway14). Wang et al.’s(Reference Wang, Yuan and Chen24) recent systematic review examined facilitating and hindering factors to ONS adherence in patients with cancer (n = 18), and Lester et al.(Reference Lester, Kleijn and Cornacchia10) reviewed the literature on factors that impact ONS intake in older adults. Each previous review focuses on quantitative studies, although Wang et al. included one qualitative study in their summary(Reference Wang, Yuan and Chen24). Qualitative studies add a patient perspective that highlights the variety and complexity of individuals’ experiences, which can help to explain quantitative results and guide the development of changes that the patients are able to implement(Reference Agius25). Comparing barriers and facilitators affecting different diagnostic groups, and investigating contextual as well as patient- and ONS-related factors, may also inform practice that supports patients with different needs and challenges. Extending previous reviews, a trans-diagnostic mixed-studies review on this topic, considering all medical conditions relevant for disease-related malnutrition, and including qualitative studies, would add important information clarifying factors affecting adherence to ONS therapy. Previous literature has indicated a large number of factors, so an organising framework is advisable to help sort and characterise the barriers and facilitators. Previous studies on medication adherence have used the WHO adherence dimensions(Reference Kardas, Lewek and Matyjaszczyk12,Reference Gast and Mathes13) , and those criteria have also been suggested to be used for ONS therapy specifically(Reference Liljeberg, Andersson and Blom Malmberg26).
Besides providing clinically important and cost-effective care to the patient, another challenge for healthcare is to provide sustainable care. ONS therapy seems to be cost-effective(Reference Elia, Normand and Laviano27,Reference Elia, Normand and Norman28) ; however, ready-made ONS requires manufacturing, logistics such as transport, storage space and commonly some sort of cooling system, thus contributing to greenhouse gas emissions. Hence, adherence to ONS is not only an important question for the individual patient and for healthcare, but also for society and the environment. Identification of barriers and facilitators to consuming ONS would guide and support clinical practice and future studies on how the healthcare system can manage nutrition therapy with ONS, with minimal waste, to achieve optimal results for patients.
The main objective of this review is to summarise the evidence regarding barriers and facilitators to adherence to and/or consumption of ONS among patients with disease-related malnutrition or at nutritional risk, using the WHO dimensions of adherence as the conceptual framework.
Methods
Study design
This systematic mixed-studies review investigates barriers and facilitators to adherence to ONS among patients with disease-related malnutrition or at nutritional risk. The protocol was registered in the PROSPERO database (CRD42021286200) in November 2021(29). The reporting of this review complies with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines(Reference Page, McKenzie and Bossuyt30). The whole review team held regular meetings during the review period (between September 2021 and March 2024) and took all major decisions on the review together. This review was performed from a realist epistemological position with focus on the reality of participants described by quantitative measures or reports of meanings and experiences in qualitative studies(Reference Patton31).
Search strategy
The search strategy was designed in collaboration with librarians from Uppsala University Library, Sweden using the Population Intervention Comparison Outcome (PICO) criteria (Table 1). Articles were included if they fulfilled the PICO criteria and were published in English between January 2000 and February 2022. The search was restricted to articles published from 2000 since a new regulation for Food for Special Medical Purposes was published in 1999(32). The following study types were accepted: randomised controlled trials (RCTs), non-RCTs, quantitative descriptive studies, mixed-methods and qualitative studies, e.g. interview and focus group studies. Exclusion criteria were the following: (i) context where impaired nutritional status was caused by lack of food/food insecurity concerns rather than a primary disease and (ii) literature reviews. Four databases were searched in March 2022; the Cochrane Central Register of Controlled Trials (CENTRAL), PUBMED, PsycINFO via Ovid, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (Appendix A). Search results were captured in Endnote X8, and duplicates were removed by a librarian. Since some duplicates remained, a second de-duplication round was made by the review team following the guidelines by Bramer et al.(Reference Bramer, Giustini and de Jonge33).
Table 1. Population, intervention, comparison and outcome (PICO) criteria
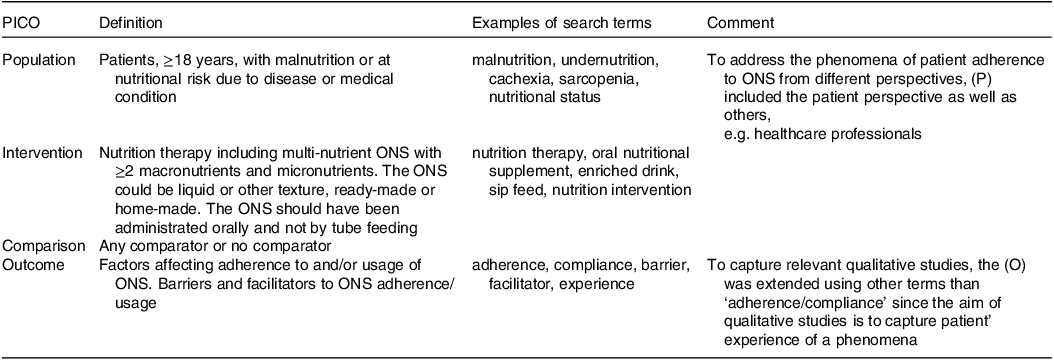
ONS, oral nutritional supplements.
Study selection
Study titles and abstracts were screened for eligibility independently by two researchers (E.L. and S.E.) using the Rayyan software(Reference Ouzzani, Hammady and Fedorowicz34). In a second step, all included articles from the screening process were read in full text by the same two researchers, to confirm inclusion or exclusion. RCTs were read in full text if more than one arm contained ONS (including placebo drinks), even if the outcome (O) was absent in the abstract. Studies comparing two or more different ONS could reveal important findings on barriers/facilitators to adherence even if this was not the primary aim of the study. Disagreements on screening results and final inclusion of articles were resolved by continuous consensus discussion.
Data extraction and analysis
First, study characteristics were captured. Then, text segments outlining barriers/facilitators associated with/related to ONS adherence/compliance/consumption were extracted from included studies, verbatim. Text segments were included from the abstract, results, discussion and conclusion in each article. NVivo Plus 11 and NVivo 12 analysis software was used to aid data organisation and analysis. A sequential exploratory synthesis of quantitative and qualitative data on barriers and facilitators to adherence to ONS was conducted(Reference Pluye and Hong35). This design contains two phases: a qualitative phase followed by a quantitative phase. In the qualitative phase, a thematic synthesis was performed on text retrieved from all articles according to the process described by Thomas and Harden(Reference Thomas and Harden36). This involves three steps; (i) coding text, (ii) developing descriptive themes, which in this study consisted of barriers and facilitators, and finally (iii) generating analytical themes where we as reviewers interpreted the findings to go beyond the content of the original studies(Reference Thomas and Harden36). In the qualitative phase, text from both qualitative and quantitative studies was included(Reference Pluye and Hong35).
Two researchers (E.L. and S.E.) independently coded a random selection of articles (first round, n = 17, second round, n = 20). After a discussion and calibration (i.e. agreeing on how text segments should be coded line-by-line), the remaining dataset (n = 154) was randomly distributed between E.L. and S.E. and coded separately. Recurrent analysis meetings between E.L., S.E. and L.P. were held to organise the codes into groups of descriptive themes. The descriptive themes are in this review equivalent to the barriers/facilitators identified in the material and summarise the key content of codes on the same topic. The next step of the analysis process followed a deductive approach in which the descriptive themes were mapped to the five dimensions of adherence declared by WHO (see section ‘The WHO adherence dimensions as framework for mapping barriers/facilitators’ for description)(11,Reference Patton31) . As a final step, analytical themes were developed. Further discussions about the meaning of data, in light of the mapping process, resulted in additional adjustments of the themes.
Since the same study could describe many barriers/facilitators for ONS consumption, one study could contribute to multiple descriptive and analytical themes in the analysis. Also, in some studies, the ONS was part of a larger nutrition intervention. In these cases, the coded barrier/facilitator relates to the whole intervention, including ONS. The qualitative phase of the analysis process is exemplified in Appendix B.
In the quantitative phase, results from RCTs where adherence/compliance/consumption of ONS was a primary or secondary outcome were tabulated alongside findings about the effect of barriers or facilitators identified in the qualitative synthesis. The aim was to clarify which barriers/facilitators were supported with RCT evidence(Reference Pluye and Hong35). The number of articles with coded barriers/facilitators within each analytical theme was then calculated to give an overview of the number in total and across populations and settings. All articles were categorised according to patient population, since all coded barriers and facilitators relate to patient adherence/compliance/consumption of ONS even when expressed by healthcare professionals (which was the case in a small amount of the articles). Articles describing populations undergoing gastrointestinal surgery were categorised as ‘Malignancy’ even though a small proportion of the population might have had benign diseases. When the setting (inpatient, outpatient or mixed) was not clearly reported, assumptions were made by the review team on the basis of the disease and context described in the study.
Finally, the interpretation of the findings in phase 1 (qualitative phase) and 2 (quantitative phase) aimed to shed light on existing knowledge on ONS adherence and knowledge gaps in the field.
The WHO adherence dimensions as framework for mapping barriers/facilitators
In the analysis process, the barriers/facilitators identified were mapped to the five dimensions of adherence according to WHO. Those five dimensions are (i) patient, (ii) condition, (iii) social and economic, (iv) therapy and (v) healthcare team and system-related factors(11) and are further exemplified in a literature meta-review of systematic reviews by Kardas et al.(Reference Kardas, Lewek and Matyjaszczyk12). Patient-related factors include demographic factors such as age and sex but also factors related to health beliefs and knowledge(11,Reference Kardas, Lewek and Matyjaszczyk12) . Condition-related factors gather around treatment and disease-related components that may impact the patient in different ways, for example, symptom and disease severity, whereas social and economic factors include e.g. family and social support status and cost of medication. Therapy-related factors are, for example, treatment duration and complexity. The dimension of healthcare team and system-related factors is exemplified by e.g. routines related to follow-up, healthcare professionals’ knowledge and training, and patient–healthcare provider relationship. The five dimensions should not be seen as silo structures but rather as interacting constructs with no strict boundaries(11).
Risk-of-bias assessment
All included articles were critically assessed independently by two researchers (L.S. and M.S.J.) using the Mixed Methods Appraisal Tool (MMAT version 2018)(Reference Hong, Pluye and Fàbregues37). The MMAT was developed to assess the methodological quality of qualitative, quantitative and mixed-methods studies.
In accordance with the MMAT recommendations, the quality appraisal was reported using descriptive responses to each MMAT criteria(Reference Hong, Pluye and Fàbregues37) and by an overall score for each article. The overall score ranges from 0% (if no quality criteria are met) to 100% (if all five quality criteria are met). The two researchers held continuous consensus discussions to achieve mutual understanding where disagreements were resolved. All 171 articles were included in the review regardless of the MMAT result as they were deemed to contribute with useful information.
Results
Search results
In total, 29 360 articles were identified in the search. After removal of duplicates, 21 835 abstracts were screened. Of these, 507 articles were included to be read in full text, and finally, 171 articles were included in the review. Of the 336 articles excluded, the most common reasons for exclusion were ‘not suitable intervention’ (n = 109), e.g. a nutrition intervention that did not include ONS, ‘wrong publication/study type’ (n = 82) and ‘no barrier or facilitator reported’ (n = 60) (Figure 1). Due to the nature of this analysis, all 171 articles were treated as a single source of data even though some of the articles represented study participants from the same study.
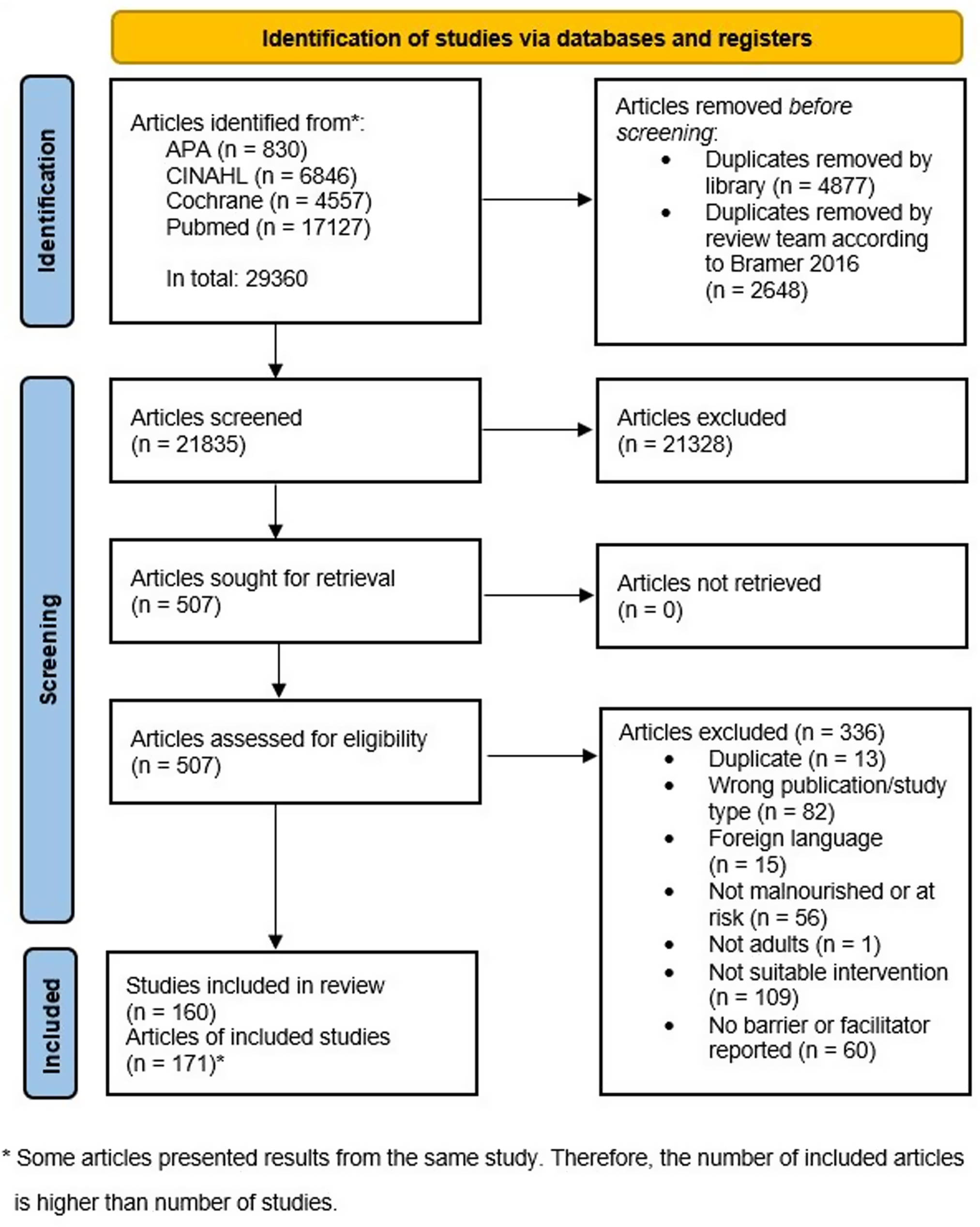
Figure 1. PRISMA flow diagram.
Study characteristics
Of the articles included in the review (n = 171)(Reference Gosney7–Reference Skladany, Vnencakova and Laffers9,Reference Jobse, Liao and Bartram16–Reference Seguy, Hubert and Robert19,Reference Wan, Yuan and Xue21–Reference Lidoriki, Schizas and Mylonas23,Reference Liljeberg, Andersson and Blom Malmberg26,Reference Alberda, Alvadj-Korenic and Mayan38–Reference Cruz-Jentoft, Calvo and Durán197) , almost half were RCTs (n = 71, 42%) and one-fifth (n = 34, 20%) had a qualitative study design (Table 2, Appendix C). Forty articles (23%) were published from 2000 to 2009, n = 81 (47%) from 2010 to 2019 and n = 50 (29%) from 2020 to February 2022. The patient populations studied varied, with the largest groups being older adults (n = 60, 35 %) and patients with malignancy (n = 58, 34 %). Half of the articles described studies performed in outpatient settings (n = 91, 53%), and n = 25 (15%) articles represented healthcare professionals’ experiences or reports on adherence to ONS instead of patients’ experiences.
Table 2. Summary of study characteristics (n = 171)
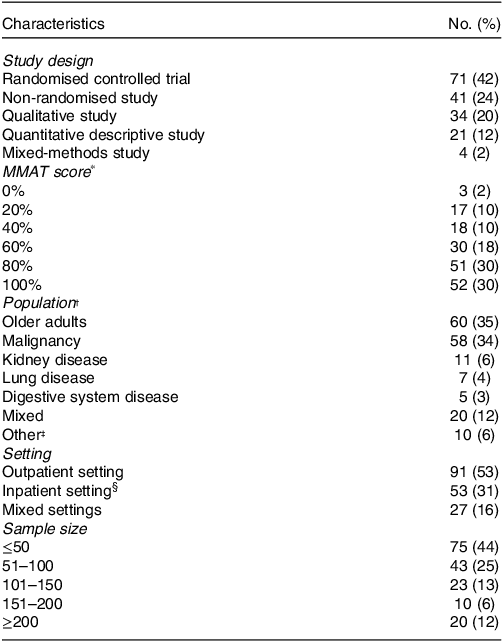
* Mixed Methods Appraisal Tool (MMAT version 2018).
† In n =19 studies, healthcare professionals were the study population, and n = 6 had a mixed study population (healthcare professionals and patients).
‡ For example, patients with wounds/pressure ulcers, patients undergoing orthopaedic treatment (without malignancy) and patients infected with HIV.
§ Inpatient setting, e.g. hospitals and nursing homes.
Risk of bias in included studies
The MMAT assessment outcomes revealed trends in research quality across various study designs, considering the number of included articles for each (Appendix D). The qualitative studies stood out with an average score of 88%, indicating their methodological robustness. The average score for RCTs was 58%, non-randomised studies 79%, quantitative descriptive studies 77% and mixed-methods studies 55%. The MMAT score varied between 0% and 100% in all the study designs, except for the non-randomised and mixed-methods study designs, where the MMAT score varied between 20% and 100%.
Sequential exploratory synthesis of qualitative and quantitative data of barriers and facilitators to adherence to ONS
During the qualitative phase of analysis, a final number of thirteen analytical themes and fifty-nine barriers and facilitators (descriptive themes) to ONS adherence/consumption were identified and categorised according to the five WHO dimensions of adherence (Figure 2). Figure 2 also shows the barriers/facilitators that have been addressed in an RCT with adherence as a primary or secondary outcome measure, which are the results from the quantitative phase.
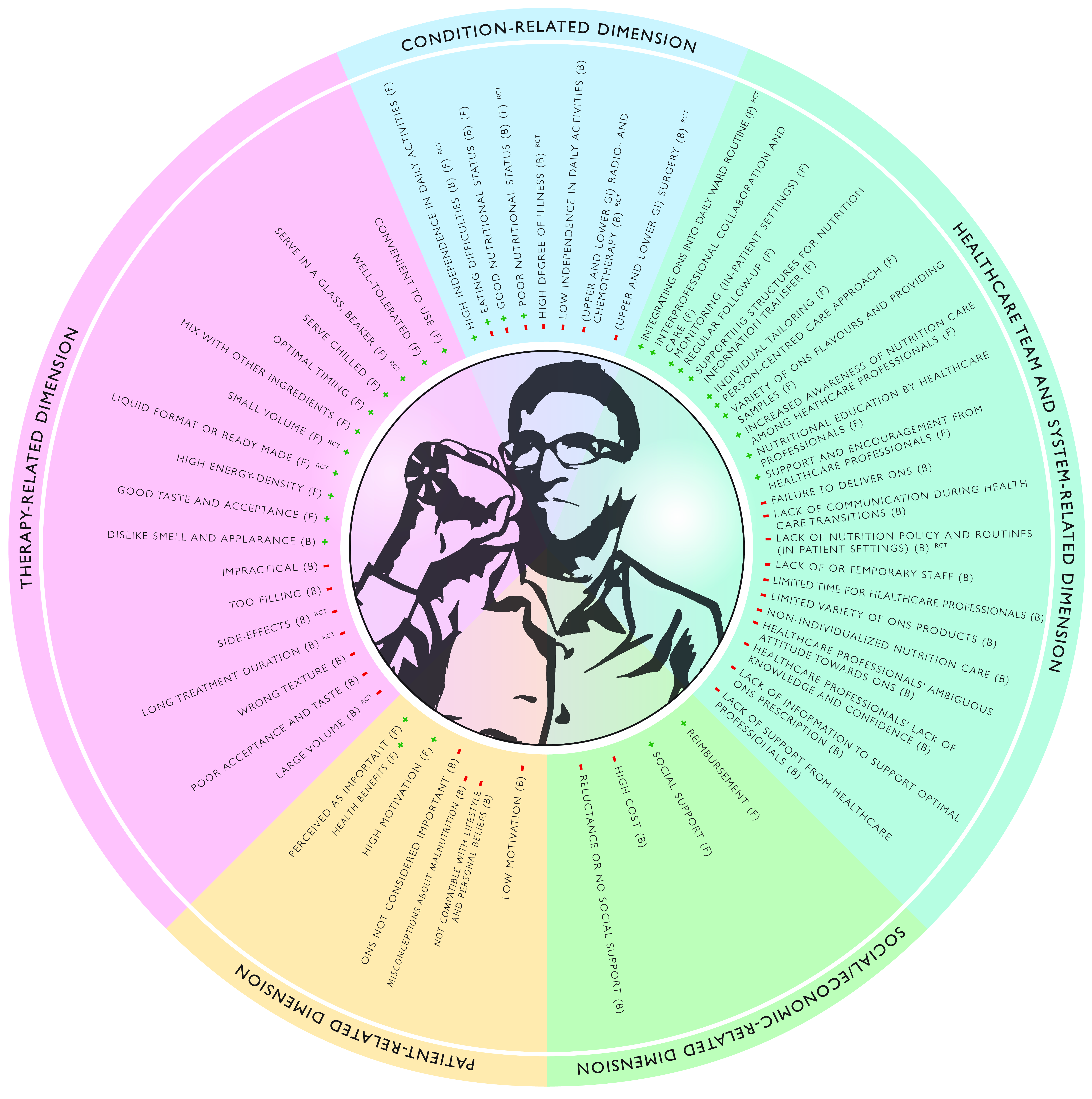
Figure 2. Five dimensions of adherence to oral nutritional supplements (ONS). Barriers and facilitators to adherence to ONS mapped against the five dimensions of adherence described by the World Health Organization (WHO). Each barrier (B) is highlighted with a red minus symbol and each facilitator (F) with a green plus symbol. Text in italics represents barriers/facilitators relating to an overarching barrier/facilitator. RCT in superscript shows barriers/facilitators that have been investigated in a randomised controlled trial. Illustration made by Byrå4 (https://byra4.se).
Qualitative phase – identified barriers and facilitators to adherence to ONS
The following sections (‘Therapy-related dimension’ to ‘Patient-related dimension’) illustrate the thematic synthesis, which consists of analytical themes and the barriers (B) and facilitators (F) (descriptive themes), categorised according to the five dimensions of adherence according to WHO. Illustrative examples from the studies have been selected and described narratively.
Therapy-related dimension. ONS tolerance, a prerequisite for usage
The included studies provide a clear picture of ONS tolerance as a prerequisite for ONS consumption since side-effects (B) from consuming ONS such as nausea, vomiting, bloating, diarrhoea and stomach pain together with the feeling of ONS as too filling (B) were described as central barriers to adherence to ONS(Reference Wan, Yuan and Xue21,Reference Cameron, Kurrle and Uy64,Reference Laviano, Calder and Schols123,Reference Sjögren Forss, Nilsson and Borglin169) . On the other hand, absence of such symptoms and consuming ONS that were well tolerated (F) was frequently described as an important facilitator(Reference Olde Rikkert, Verhey and Blesa145,Reference Previtali, Fiore and Colombo153,Reference Dhuibhir, Collura and Walsh181) .
An ONS format with satisfactory product and sensory properties
Poor acceptance and taste (B), wrong texture (B) and dislike of the smell and appearance (B) of ONS were central barriers to consumption of ONS in a range of different study populations and settings. Negative sensory characteristics of ONS were, for example, described as excessive sweetness or ‘bland taste’ (Reference Doll-Shankaruk, Yau and Oelke80,Reference Enriquez-Fern, Chen and Klassen81,Reference Hertlein, Zeder-Göß and Fürst94,Reference Lambert, Potter and Lonergan120) . On the contrary, good taste and acceptance (F) was described as a facilitator to consumption and was commonly presented as one important explanation to patients’ high adherence rates(Reference Wan, Yuan and Xue21,Reference Ishiki, Iwase and Gyoda109,Reference Mayr, Kalde and Vogt132) . Liquid format or ready-made (F) ONS were in general described as facilitating ONS consumption(Reference Lammel Ricardi, Marcadenti and Perocchin de Souza121,Reference Liljeberg, Nydahl and Lövestam126) .
Another aspect of importance for adherence to ONS was the volume to be consumed. In many studies, a small volume (F) was expressed as facilitating intake(Reference Jukkola and MacLennan112,Reference van den Berg, Lindeboom and van der Zwet182,Reference Wengström, Wahren and Grodzinsky190) while a large volume (B) was described as a barrier(Reference Jeloka, Dharmatti and Jamdade111,Reference Olsson, Bergbom and Bosaeus146,Reference van den Berg, Lindeboom and van der Zwet182) . Sometimes this related to the total volume to be consumed in one day(Reference Hogan, Solomon and Carey98), but in most studies, it related to the volume to be consumed at one specific timepoint(Reference Jobse, Liao and Bartram16,Reference Jukkola and MacLennan112,Reference Roberts, Potter and McColl159) . A related finding was the identification of high energy density (F) as a facilitator to ONS consumption(Reference Hogan, Solomon and Carey98,Reference Lombard, Steijn and Schuur127,Reference Smith, Cawood and Walters170,Reference Stow, Ives and Smith176) .
ONS, a convenient solution with a few practical drawbacks
Finding the ONS convenient to use (F) was identified as a facilitator to adherence to ONS in many studies. For example, ONS was described as easy to take(Reference Brown, Fry and Cawood57), useful when one cannot eat(Reference Enriquez-Fern, Chen and Klassen81), and a therapy that places a low burden on the patient(Reference Myers141). On the other hand, some studies described ONS as impractical (B), which could hinder ONS consumption(Reference Browne, Kelly and Geraghty58,Reference Wong, Goh and Goh191) . For example, the collection and transport of ready-made liquid ONS was described as difficult for fragile populations(Reference Bojesen, Jørgensen and Grube52,Reference Browne, Kelly and Geraghty58,Reference Wong, Goh and Goh191) .
Finding the most suitable serving style of ONS at the right time
How the ONS are served to or by the patient, the timing of the serving and the duration of ONS usage seem to impact adherence. Adherence can be facilitated by the ONS being served chilled (F)(Reference Lambert, Potter and Lonergan120), served in a glass or breaker (F), especially for older adults(Reference Gosney7,Reference Allen, Methven and Gosney40,Reference Vikström, Grönstedt and Cederholm187) , or by mixing with other ingredients (F) such as coffee or flavouring agents(Reference Neo, Hong and Chan143,Reference Tanaka, Ueno and Yoshida178) .
Finding an optimal timing (F), e.g. in between meals, of ONS consumption was described as increasing adherence(Reference Roberts, Potter and McColl159). Also, the time since the ONS therapy started seemed to be of importance since a longer treatment duration (B) of ONS was pointed out as a barrier to adherence. Many studies identified a declining trend of ONS consumption with a longer duration among patients undergoing different types of cancer treatments such as gastrointestinal surgery or chemotherapy(Reference Wan, Yuan and Xue21,Reference Baldwin, Spiro and McGough42,Reference Imamura, Matsuyama and Nishikawa108,Reference Lambert, Potter and Lonergan120) .
Social economic-related dimension. Cost of ONS influences use: the importance of reimbursement
Needing to pay for ONS and high cost (B) were shown to be barriers to adherence. For example, a study on facilitators/barriers for nutrition risk in older adults found price to be a central issue(Reference Sadarangani, Johnson and Chong161), and similarly, the patients´ financial status was shown to affect patient compliance to ONS in a study with patients who underwent gastrectomy(Reference Wan, Yuan and Xue21). On the contrary, reimbursement (F), i.e. free of charge, or reduced-price prescriptions were shown to facilitate ONS consumption in many studies(Reference Breedveld-Peters and Reijven54,Reference Calegari, Barros and Veronese63,Reference Førli, Bjørtuft and Vatn85,Reference Hulsbæk, Laursen and Kristensen105,Reference Smith, Cawood and Walters170,Reference Wong, Goh and Goh191) . Studies from France(Reference Alberda, Alvadj-Korenic and Mayan38), Sweden(Reference Liljeberg, Nydahl and Lövestam126) and the UK(Reference Smith, Cawood and Walters170) specifically highlighted their system of reimbursement of ONS as important for ONS consumption and adherence.
The significant role of family and friends
Social support (F), especially for vulnerable patients, was highlighted as an important facilitator for ONS adherence. For example, staying at home or with relatives resulted in significantly higher energy intake from ONS and regular food compared with staying at a hotel during radiotherapy for head and neck cancer(Reference Hopanci Bicakli, Ozkaya Akagunduz and Meseri Dalak17). Reluctance or no social support (B) were described as a barrier to ONS adherence. Reluctance could be seen when patients and family showed lack of understanding of the importance of dietary support(Reference Ginzburg, Shmilovitz and Monastyrsky88) or when relatives were putting too much pressure on the patient to eat and take ONS, which could lead to a decreased intake rather than the opposite(Reference Holst, Rasmussen and Laursen100). Having limited social support was described as a barrier to ONS consumption(Reference Wan, Yuan and Xue21,Reference Hashizume, Tanaka and Fukahori91,Reference Wong, Goh and Goh191) , especially for patients needing help at home, e.g. older adults or patients with dementia.
Healthcare team and system-related dimension. Healthcare professionals’ knowledge on malnutrition and its therapy
Some studies described how healthcare professionals’ lack of knowledge and confidence (B) created a barrier to ONS consumption. This was expressed as lack of basic nutritional knowledge, ONS information and/or training(Reference Breedveld-Peters and Reijven54,Reference Brindisi, Noacco and Boudaoud Hansal56,Reference Lambert, Potter and Lonergan120) . In addition, healthcare professionals’ ambiguous attitude towards ONS (B) was highlighted as being a barrier to ONS adherence. For example, some healthcare professionals were not convinced that patients needed them(Reference Jobse, Liao and Bartram16,Reference Brindisi, Noacco and Boudaoud Hansal56,Reference Vikström, Grönstedt and Cederholm187) , and as discussed by Brindisi and colleagues(Reference Brindisi, Noacco and Boudaoud Hansal56), an ambiguous attitude by healthcare professionals may result in a mixed or unclear message about ONS to the patients, which will affect adherence. There were also studies describing that an increased awareness of nutrition care among healthcare professionals (F) would facilitate ONS adherence, for example, by clarifying ONS status among healthcare professionals(Reference Brindisi, Noacco and Boudaoud Hansal56) and giving the healthcare team the right mindset about nutrition(Reference Vikström, Grönstedt and Cederholm187).
Information and support increase patient motivation and capability
Nutritional education by healthcare professionals (F) was highlighted as a factor facilitating ONS consumption by increasing patients’ knowledge(Reference Grass, Bertrand and Schäfer8,Reference Hashizume, Tanaka and Fukahori91) , self-management skills(Reference Puranen, Pitkala and Suominen154,Reference Qin, Xu and Tian155) , motivation and capability(Reference Hogan, Solomon and Carey98,Reference Liljeberg, Nydahl and Lövestam126) . Nutritional education included information on ONS in relation to general food intake through dietary counselling by a dietitian(Reference Liljeberg, Andersson and Blom Malmberg26), reasons for using ONS(Reference Citty, Kamel and Garvan69), instructions on how to take ONS and how to deal with intolerance(Reference Qin, Xu and Tian155), and also to give ONS the same status as a medicine(Reference Liljeberg, Nydahl and Lövestam126,Reference Roberts, Potter and McColl159) . Besides nutritional education, support and encouragement from healthcare professionals (F) was found to be an important facilitator for ONS consumption. This was described in terms of both focusing on emotional support such as having an ‘encouraging and empathic attitude’ (Reference Vikström, Grönstedt and Cederholm187), and practical support such as solving issues with ONS delivery(Reference Liljeberg, Nydahl and Lövestam126). On the contrary, lack of support from healthcare professionals (B) and lack of information to support optimal ONS prescription (B) were highlighted as barriers to ONS adherence. For example, limited support from healthcare professionals was shown to have a negative effect on ONS consumption for inpatients(Reference Jobse, Liao and Bartram16,Reference Lambert, Potter and Lonergan120,Reference Stange, Bartram and Liao172) . Also, lack of information on ONS prescription was described to make the patients feel uncertain about when to take ONS and the daily target intake, leading to poorer adherence(Reference Brindisi, Noacco and Boudaoud Hansal56,Reference Qin, Xu and Tian155,Reference Reynolds, Castro and Geraghty158) .
Continuity of (ONS) care is supported by well-functioning organisational routines and structures
Well-functioning routines and structures within the organisation were shown to be of importance to support proper ONS management and, further, adherence to ONS. One barrier described in relation to this was lack of nutrition policy and routines (in-patient settings) (B) which can be exemplified by the existence of a diversity (or lack) of nutritional care policies(Reference Breedveld-Peters and Reijven54) or by staff not serving the ONS at ward(Reference Beck, Damkjaer and Tetens47,Reference Citty, Kamel and Garvan69) . Another barrier, lack of communication during healthcare transitions (B), points out problems related to poor communication about nutritional care between institutions, such as the hospital and the community(Reference Ginzburg, Shmilovitz and Monastyrsky88,Reference Reynolds, Castro and Geraghty158) . Other barriers related to organisational routines and structures were limited time for healthcare professionals (B) and lack of or temporary staff (B). These factors were described as leading to down-prioritising nutrition-related tasks and not being able to support nutritional intake(Reference Beck, Damkjaer and Tetens47,Reference Breedveld-Peters and Reijven54,Reference Holst and Rasmussen101,Reference Lambert, Potter and Lonergan119,Reference Vikström, Grönstedt and Cederholm187) . Failure to deliver ONS (B) was also highlighted as problematic, including failures both within institutions and directly to the patient’s home(Reference Breedveld-Peters and Reijven54,Reference Breedveld-Peters, Reijven and Wyers55) .
One facilitator related to organisational routines and structure was to integrate ONS into daily ward routine (F), such as serving ONS during medications rounds or adding ONS to the medical administration record(Reference Citty, Bjarnadottir and Marlowe68,Reference Gillis, Martin and Gill87,Reference Jukkola and MacLennan112,Reference Roberts, Potter and McColl159,Reference van den Berg, Lindeboom and van der Zwet182) . This concept is sometimes referred to as the ‘nutrition as medication’ (NAM) programme(Reference Jukkola and MacLennan112) or ‘Medication pass nutritional supplement program’ (MEDpass programme)(Reference Campbell, Webb and Vivanti65). Another facilitator was supporting structures for nutrition information transfer (F). To ensure continuity of nutritional care, proper nutrition information transfer was highlighted as imperative(Reference Breedveld-Peters and Reijven54,Reference Kraft, van den Berg and Kraft117) , and it has further been proposed that unit leaders should create conditions for continuity(Reference Vikström, Grönstedt and Cederholm187). The importance of regular follow-up (F), for example, by phone, face-to-face meetings or home visits, and monitoring (in-patient settings) (F) were highlighted as important facilitators for ONS adherence in many studies(Reference Boisselier, Kaminsky and Thézenas51,Reference Breedveld-Peters and Reijven54,Reference Breedveld-Peters, Reijven and Wyers55,Reference Caglar, Fedje and Dimmitt61,Reference Daud, Tubie and Adams73,Reference Puranen, Pitkala and Suominen154,Reference Wall, McCombie and Mulder188,Reference Xie, Chen and Xu193) . To increase ONS adherence, studies also highlighted the importance of a joint effort from different healthcare professionals, that is, emphasised the need of interprofessional collaboration and care (F). The purpose of this is to guarantee adequate communication(Reference Breedveld-Peters and Reijven54,Reference Lambert, Potter and Lonergan120) , align practices and standardise the information on ONS given to the patient(Reference Brindisi, Noacco and Boudaoud Hansal56).
Finding the right approach for the individual
Having a person-centred care approach (F) by, for example, discussing different options within the nutrition intervention(Reference Collins, Tucker and Walton70,Reference Hestevik, Molin and Debesay95) or giving patients freedom to choose for themselves and take an active part of the nutrition care(Reference Kraft, van den Berg and Kraft117,Reference Liljeberg, Nydahl and Lövestam126) was shown to facilitate ONS consumption. In line with a person-centred care approach, individual tailoring (F) such as adapting the advice and amount to individual needs and preferences, was shown to be an important facilitator for ONS adherence(Reference Beck, Kjær and Hansen45,Reference Breedveld-Peters and Reijven54–Reference Brindisi, Noacco and Boudaoud Hansal56,Reference Liljeberg, Nydahl and Lövestam126) . To enable individual tailoring, a variety of ONS flavours and providing samples (F) was shown to be of importance to find products that meet patient’s taste preferences and to allow for variation(Reference Liljeberg, Andersson and Blom Malmberg26,Reference Dewey and Dean79,Reference Liljeberg, Nydahl and Lövestam126,Reference Smith, Cawood and Walters170) . On the contrary, limited variety of ONS products (B) was shown to be a barrier to ONS adherence. Here, the prescription could be limited due to ONS brands and flavours available(Reference Dewey and Dean79). Also, non-individualised nutrition care (B) such as receiving generic suggestions about ONS and food adaptations(Reference Alberda, Alvadj-Korenic and Mayan38) and lack of considerations for individual needs was described as hindering adherence to nutrition care (including ONS)(Reference Hestevik, Molin and Debesay96).
Condition-related dimension. Contradictive consequences of a worse health status on ONS use
A high degree of illness (B) and/or low independence in daily activities (B) were in many studies described as barriers to adherence to ONS. A high degree of illness could relate to a worsened disease status(Reference Steiner, Barton and Singh173), not feeling well(Reference Citty, Kamel and Garvan69) or being depressed(Reference Jobse, Liao and Bartram16), and was described as impacting ONS consumption negatively. The significance of low independence in daily activities for the consumption of ONS was mainly described in studies on populations with older adults. Several of those articles described a lower adherence to ONS among patients who were dependent on others(Reference Wengström, Wahren and Grodzinsky190), were immobile(Reference Jobse, Liao and Bartram16) or had poor memory(Reference Xie, Chen and Xu193). On the other hand, a high independence in daily activities (F) was connected to a higher adherence(Reference Jobse, Liao and Bartram16,Reference Wengström, Wahren and Grodzinsky190) .
A diverse picture was identified of the consequences of a good (B/F) or poor (B/F) nutritional status on adherence to ONS. In some studies, patients with a better nutritional status were more compliant to ONS than those with a poorer nutritional status(Reference Bauer, Capra and Battistutta43,Reference Hogan, Solomon and Carey98) , while the trend was the opposite in other studies(Reference Jobse, Liao and Bartram16,Reference Wan, Yuan and Xue21) .
Conflicting findings were also shown for eating difficulties (B/F). A great share of studies across many medical disciplines and settings suggests that adherence to ONS was lower among patients experiencing eating difficulties such as early satiety(Reference van der Meij, Langius and Smit183), lack of appetite or thirst(Reference Hertlein, Zeder-Göß and Fürst94,Reference Jukkola and MacLennan112) , nausea/vomiting(Reference Citty, Kamel and Garvan69,Reference Roberts, Potter and McColl159) or swallowing difficulties(Reference Sandmæl, Bye and Solheim139). However, in some studies, adherence was described as higher with a higher burden of eating difficulties such as chewing difficulties(Reference Jobse, Liao and Bartram16,Reference Ginzburg, Shmilovitz and Monastyrsky88) and a large number of nutrition impact symptoms, e.g. feeling full, dry mouth, loss of appetite or taste changes(Reference Enriquez-Fern, Chen and Klassen81).
Treatments of the disease reduce ONS use
Several studies, mainly in populations with upper or lower gastrointestinal cancer, showed that consequences from (upper and lower GI) radio- and chemotherapy (B) and (upper and lower GI) surgery (B) affect ONS consumption negatively. For example, several studies on different cancer populations show that ONS consumption tends to be higher before than after surgery(Reference Hanai, Terada and Hirakawa90,Reference Hertlein, Zeder-Göß and Fürst94,Reference Short, Atkinson and Ness168) .
Patient-related dimension. Having implications for ONS consumption
Adherence to an ONS prescription was described as being dependent on whether patients had high motivation (F) and whether consuming ONS was perceived as important (F). For example, for patients, the perceived importance of consuming ONS seemed to be higher when healthcare professionals presented ONS as medicine(Reference Lambert, Potter and Lonergan119,Reference Roberts, Potter and McColl159) or when a doctor recommended their patient to use ONS(Reference Dedeyne, Dewinter and Lovik77). Experiencing health benefits (F) from ONS was also suggested to be of great importance for consumption. This could be seen in studies highlighting reasons for patients taking ONS, for example, to provide the body with proteins and vitamins to ‘catch up’(Reference Gillis, Martin and Gill87), to improve body condition and to be strong before surgery(Reference Hogan, Solomon and Carey98), or for community-dwelling older adults to prolong their independence(Reference den Uijl, Kremer and Jager78).
In contrast, ONS not considered important (B) by patients and low motivation (B) to consume ONS were identified as influential barriers and were suggested as potential explanations for low adherence among the whole or a part of the studied population in several studies(Reference Grass, Bertrand and Schäfer8,Reference Hertlein, Zeder-Göß and Fürst94,Reference Kraft, van den Berg and Kraft117,Reference Patursson, Møller and Muhic149,Reference Qin, Xu and Tian155,Reference Short, Atkinson and Ness168) . Furthermore, when patients had misconceptions about malnutrition (B) and its treatment or when ONS were not compatible with patient’s lifestyle or personal beliefs (B), ONS was not considered important (B) and adherence to treatment was lower. One example of a misconception about disease-related malnutrition was when patients considered weight loss to be positive despite having disease-related malnutrition(Reference Jobse, Liao and Bartram16,Reference Hazzard, Haughton and Fish92,Reference Stange, Bartram and Liao172) . Another barrier to ONS intake was when the usage of those products was not compatible with patient’s lifestyle or personal beliefs(Reference Alberda, Alvadj-Korenic and Mayan38,Reference Enriquez-Fern, Chen and Klassen81,Reference van der Meij, Langius and Smit183,Reference Zhang, Zhu and Zhang196) . Also, cultural aspects, such as believing that tonics (drugs used in traditional Chinese medicine) or herbal products were more effective than ONS, were aspects highlighted in studies as factors that could impact ONS consumption negatively(Reference Wan, Yuan and Xue21,Reference Huang, Piao and Cao102) .
Quantitative phase – barriers and facilitators supported by quantitative data
In total, the effect of thirteen out of fifty-nine identified barriers and facilitators in the qualitative phase had been investigated in RCTs with adherence/compliance/consumption as primary or secondary outcome measure (Table 3). Poor nutritional status (B, F), (upper and lower GI) surgery (B) and side-effects (B) were the most frequent barriers/facilitators supported by RCT evidence. In Table 4, all analytical themes within each WHO dimension are presented with tabulated information on the number of articles supporting each specific theme. Two analytical themes ‘An ONS format with satisfactory product and sensory properties’ and ‘ONS tolerance, a prerequisite for usage’ (therapy-related dimension) were supported by the highest number of individual articles (n = 95 and n = 86, respectively).
Table 3. Randomised controlled trials (RCTs) investigating barriers or facilitators to oral nutritional supplements (ONS)
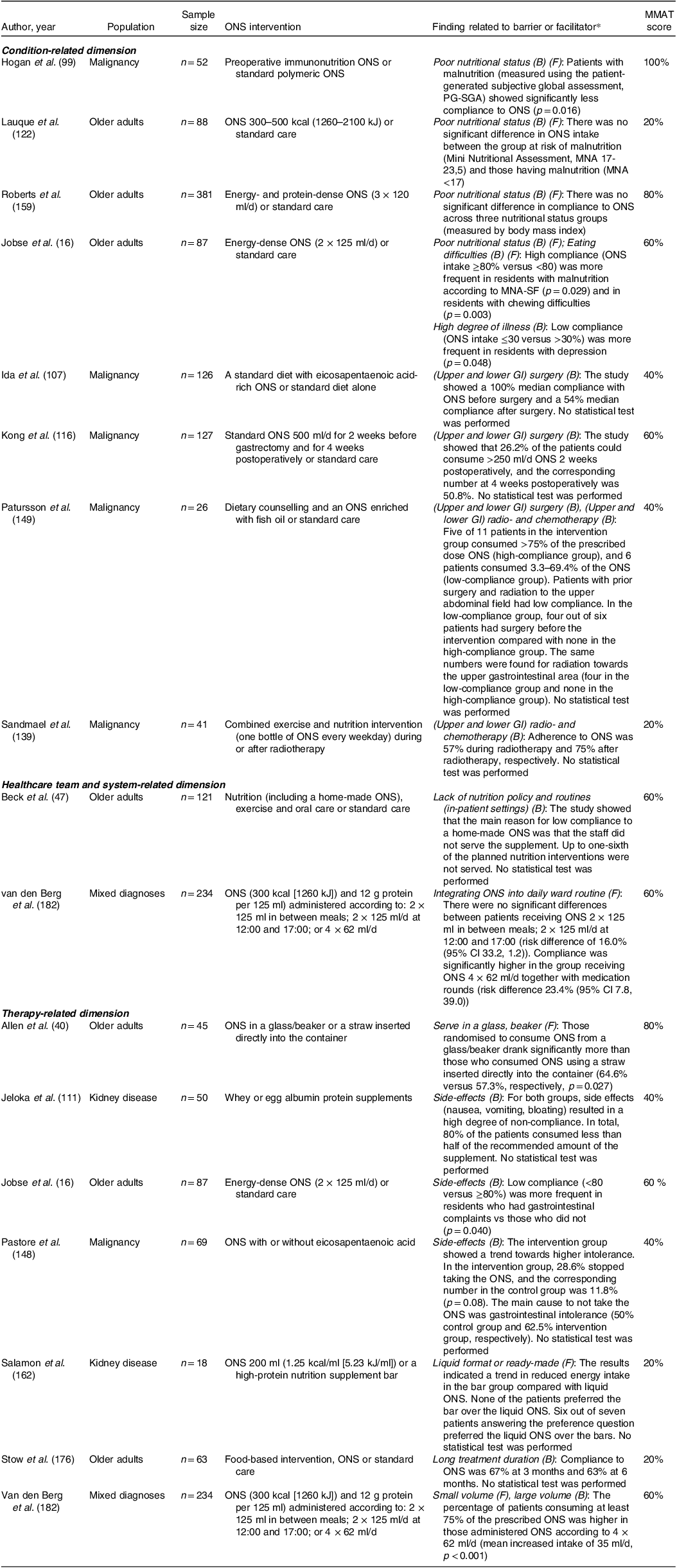
* No barriers/facilitators within the patient-related or social/economic-related dimension were supported by RCTs.
Table 4. Number of publications supporting the analytical themes, in total and divided by population and setting within each World Health Organization (WHO) dimension of adherence
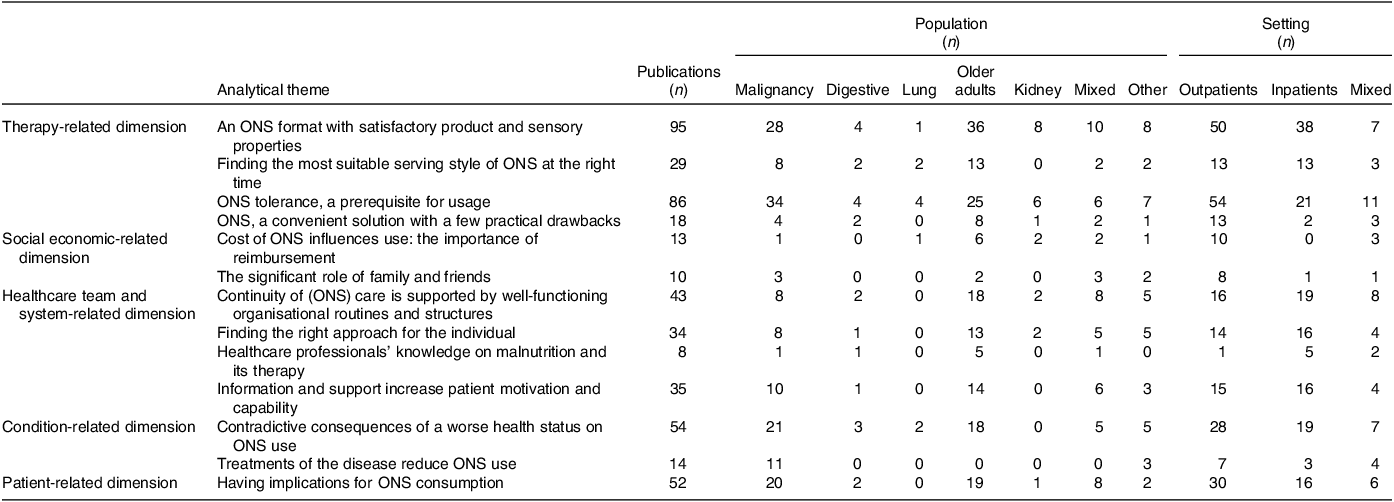
ONS, oral nutritional supplements.
Discussion
Our review on barriers and facilitators to adherence to ONS makes an important contribution to earlier reviews on this topic(Reference Lester, Kleijn and Cornacchia10,Reference Hubbard, Elia and Holdoway14,Reference Wang, Yuan and Chen24) as it presents a trans-diagnostic mixed-studies summary with potential to inform and guide clinical practice and healthcare professionals in their daily work when meeting patients with disease-related malnutrition or at nutritional risk needing ONS. Identified barriers and facilitators to ONS consumption were mapped to all five WHO dimensions of adherence(11), showing its complexity and multifaceted nature and that a diverse range of factors need to be considered when using this nutrition therapy approach to patients.
The majority of the barriers and facilitators identified belong to the therapy-related and the healthcare team and system-related dimensions, and are also modifiable in their nature. For example, the volume to be consumed, when and at what temperature to serve ONS and whether to mix them with other ingredients are therapy-related factors that have been recurrently identified as important for consumption and adherence(Reference Stratton and Elia198,Reference Gandy199) . Such factors have also been seen as solutions to counteract therapy-related hindering factors such as poor acceptance and side-effects. In addition, we also found many facilitators with great potential within the healthcare team and system-related dimension such as having a person-centred approach, tailoring the ONS prescription to individual needs and providing suitable monitoring and follow-up. This highlights the importance of having the whole healthcare system, from top to bottom, address and work towards solving issues related to ONS adherence. For example, it was shown that the lack of nutritional care policies may hamper the implementation of nutrition interventions with ONS(Reference Breedveld-Peters and Reijven54) and that nutrition information transfer between the hospital and the community may constitute a barrier to ONS adherence(Reference Ginzburg, Shmilovitz and Monastyrsky88,Reference Reynolds, Castro and Geraghty158) . In addition, direct contact with the healthcare profession, education and having a person who gives support and encouragement were shown to be of importance, as supported by previous research on medication adherence(Reference Taibanguay, Chaiamnuay and Asavatanabodee200,Reference Levy, Huang and Huang201) . Similarly to our review, Levy et al.(Reference Levy, Huang and Huang201) mapped factors for medication adherence in patients with coronary heart disease to the five dimensions of the WHO adherence model. They highlight the need for a ‘Learning healthcare system’, to create feedback systems to better understand the conditions that generate non-adherence and how to best counteract them. This would create reflective institutions that learn, refine and improve in response to patient behaviour. From the results of our review, it is easy to understand that tackling a single barrier will fail to combat non-adherence to ONS. This is in line with previous advocates for multifaceted interventions to tackle medication non-adherence(Reference Kardas, Lewek and Matyjaszczyk12) and calls for a move away from blaming patients for this very complex behaviour change challenge(11). Instead, non-adherence to ONS should be addressed using a holistic approach, not just focusing on the physiological aspects but also being aware of a person’s psychological, social and spiritual needs(Reference Huljev and Pandak202).
Within the social and economic-related dimension and the condition-related dimension, barriers and facilitators presented are typically non-modifiable from a healthcare professional point of view. For example, it is hard to affect the patient’s degree of illness, therapy received (e.g. surgery) or occurrence of eating difficulties, at least within a short time frame. It can also be hard to influence whether a patient receives social support from family or friends. However, even if not supported by a RCT in our review, social support has been identified as a predictor of better self-care adherence in patients with heart failure(Reference Meraz, McGee and Caldwell203) and as having a positive impact on adherence to therapy among patients with a range of chronic physical diseases in an overview of systematic reviews(Reference Gast and Mathes13). Together, those findings can support healthcare professionals to ask the patient for permission to involve possible family members and/or friends in the discussions on nutrition interventions such as ONS prescriptions or to encourage patients to share information that they are given to family members.
Even though the patient-related dimension has received the most focus in the previous adherence literature(11) the number of barriers/facilitators in the patient-related dimension was quite scarce. The present review showed how patient motivation and perceived importance were factors highly relevant to understanding adherence to ONS from the patient’s perspective. However, no RCTs focused on those barriers/facilitators and very few of the articles have measured the interrelated concepts of motivation or perceived importance of ONS use in a quantitative investigation or by using a theory or model, e.g. a behavioural change theory such as the health belief model(Reference Rosenstock204), as the starting point or explanation companion.
Finally, we would like to illustrate how the findings from this review can be used to interpret studies on adherence to ONS. Clinical trials included in this review found beneficial effects on adherence by serving ONS as medicines, in small volumes at ward during medication rounds (also named the NAM/MEDpass programme)(Reference Jukkola and MacLennan112,Reference van den Berg, Lindeboom and van der Zwet182) . The question of whether this approach leads to better compliance, better nutritional intake, higher body weight or higher hand grip strength was recently investigated in a systematic review including ten trials and confirms the positive effect of the NAM/MEDpass programme on compliance (but not on the other outcome measures)(Reference Krebs, Uhlmann and Stanga205). The results of our review contribute with a potential explanation on how different facilitators and barriers to ONS adherence inter-operate within this NAM/MEDpass intervention. First, small/non-large ONS volume (therapy-related dimension) is likely beneficial. Second, the integration of scheduled ONS rounds into daily ward routines, the close monitoring of ONS intake, and support and encouragement from healthcare professionals (healthcare team and system-related dimension) probably matter. Finally, viewing the ONS as medication might increase a patients’ perceived importance of taking them (patient-related dimension) and consequently lead to higher adherence.
Recommendations for future studies
Even though as many as 171 articles were included in this review, very few of the included RCTs investigated ways to overcome barriers and incorporate facilitators to ONS adherence as the primary research question. It is evident that future experimental studies investigating the effect of different approaches to increase adherence to ONS are greatly needed. Similarly, the lack of long-term good-quality studies was the main conclusion in a Cochrane review on interventions to enhance adherence to dietary advice for preventing and managing chronic diseases published in 2013(Reference Desroches, Lapointe and Ratté206). The field of adherence to medical nutrition therapy seems to be longing for more high-quality research to be published.
Strengths and limitations
A major strength of the present review is its extensive nature as it presents data from a total of 171 articles, with the initial screening of 21 835 titles/abstracts. This review is also the first to have a trans-diagnostic perspective, which we believe is important to fully understand the complexity related to ONS adherence. Another strength is the inclusion of studies using a qualitative study design, allowing for the patient’ perspective to be properly investigated. Study inclusion, data extraction, analysis and risk-of-bias assessment were carried out independently by two researchers. However, due to the comprehensive data collection, during the phases of coding text and analysis, the articles were evenly distributed between two researchers. This approach was supported by continuous discussions and consensus meetings within the review team.
Drawbacks of the WHO adherence dimensions
When conducting this review, a few drawbacks became evident when using the WHO adherence model to understand adherence to ONS. For example, there are overlaps between the dimensions, which the WHO authors also acknowledge in their report(11). A text sequence about the consequences of gastrointestinal surgery on ONS side-effects and eating difficulties could be coded to both the condition-related dimension and therapy-related dimension. It is easy to conclude that a higher burden of pre-existing eating difficulties (e.g. vomiting, nausea, low appetite) and a larger number of side-effects (e.g. nausea, feeling full, diarrhoea) from drinking the ONS brings you closer to the reason of why adherence is lower rather than being related to the surgery per se. Consequently, the WHO model does not aid in explaining the relationship between the dimensions as a behavioural change theoretical framework might, such as the Socio-ecological model by Bronfenbrenner(Reference Bronfenbrenner207) or the Behaviour Change Wheel by Michie et al.(Reference Michie, Van Stralen and West208). However, using such frameworks/models would require considerable resources to analyse the number of studies included in the present review, and would not allow for the broad scope that this review aimed to have.
Another question to raise concerning the WHO model is how one should distinguish between the therapy dimension and the healthcare team and system-related dimension. The presumptions of the model are that the therapy which can be defined as a ‘pill’ or the ‘ONS’ is separated from the actions of the healthcare team. However, ONS therapy is considered to be a multifactorial nutrition intervention that also is dependent upon a good relationship between the patient and prescriber and to include behaviour change strategies(Reference Liljeberg, Nydahl and Lövestam126,Reference Liljeberg209) . The same probably applies to the typical medication intervention where the relationship with the doctor and other healthcare professionals is central.
One argument for the use of the WHO model despite evident drawbacks is that it allows for the inclusion of barriers and facilitators at micro and macro levels such as going from the disease status of individual patients – to healthcare professional’s knowledge about malnutrition – and further to nutrition policies and economic and political systems. Our standpoint from using the WHO model to understand ONS adherence is that the model should be seen as a way of categorising different aspects related to adherence to therapy rather than a theoretically founded framework that tries to explain the actual phenomenon of adherence. It is also important to not see the different dimensions of the model as fixed but instead as interacting constructs with no strict boundaries. Hence, using the WHO adherence model was helpful to make sense of/understand the multidimensional aspects of ONS adherence, though we need to know more about how these dimensions interact.
Conclusion
This is the first systematic review with a trans-diagnostic mixed-studies design that has investigated barriers and facilitators to adherence to ONS among patients with disease-related malnutrition or at nutritional risk. Barriers/facilitators were found within each of the five dimensions of the WHO model of adherence, with a heavy weighting towards the therapy-related and healthcare team and system-related dimensions. Very few of the included RCTs investigated barriers and facilitators to ONS adherence as the primary research question, which calls for experimental studies investigating the effect of different approaches to increase adherence to ONS. Given the complexity and multifaceted nature of ONS adherence, non-adherence to ONS should be addressed using a holistic approach and being aware of each patient’s various needs. Only by learning from patients as first-hand users of ONS and how they interact with the barriers/facilitators present throughout the trajectory of care can we fully understand the factors affecting adherence to ONS consumption.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0954422424000192.
Acknowledgements
We would like to thank the librarians at Uppsala University Library, Sweden, who helped us with the search strategy and the final search. We would also like to thank Jesper Persson, Graphic Designer at Byrå4, who helped us design the figure showing barriers and facilitators to ONS adherence mapped in relation to the five dimensions of adherence described by WHO.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
Liljeberg was the first author of two of the articles included in the review. She was not involved in the extraction/coding of data or risk of bias assessment of these studies. The other authors declare that there is no conflict of interest.
Author contributions
Evelina Liljeberg: Conceptualisation, Methodology, Validation, Formal analysis, Investigation, Writing – Original Draft, Visualisation, Project administration. Liz Payne: Methodology, Formal analysis, Investigation, Writing – Review & Editing. Malin Skinnars Josefsson: Methodology, Investigation, Writing – Review & Editing, Visualisation. Lisa Söderström: Methodology, Investigation, Writing – Review & Editing, Visualisation. Sandra Einarsson: Conceptualisation, Methodology, Validation, Formal analysis, Investigation, Writing – Original Draft, Visualisation, Project administration, Supervision.









