Introduction
Today, the average life expectancy is steadily increasing, which results in a dramatic rise in chronic fatal diseases. As a result, there is an increasing need and demand for palliative care (PC) (Etkind et al. Reference Etkind, Bone and Gomes2017). Although numerous studies and projects on the subject are accumulating in many countries, the need for unmet PC remains an important problem. In addition to the treatment services in modern health-care delivery, PC services aim to provide physical, social, and psychological support to the patients and their families, prioritizing improvements in the individual’s life quality (Yakar et al. Reference Yakar, Batbaş and Pirinçci2021).
As in many countries of the world, in Turkey, families of patients with chronic diseases cannot provide the necessary care. This situation brings the need for professional care. This is due to the increasing proportion of the dependent elderly population, chronic diseases, and potential caregivers in the workplace (Lagman and Walsh Reference Lagman and Walsh2005; Yakar et al. Reference Yakar, Batbaş and Pirinçci2021). At this point, PC might be regarded as an alternative approach to meet the needs of patients and their relatives facing life-threatening diseases (Suikkala et al. Reference Suikkala, Tohmola and Rahko2021).
In most developed countries, nurses comprise the most prominent health-care professionals involved in PC service (Martins Pereira et al. Reference Martins Pereira, Hernández-Marrero and Pasman2021). Similarly, the PC is mostly conducted in Turkey through nursing services (Republic of Turkey Ministry of Health 2019). Therefore, evaluating the quality of PC provided by nurses is essential to improve the quality of patient care. The European Association of Palliative Care (EAPC) recommended assessing PC service with several measurement tools. It has been suggested that these assessment tools should evaluate not only patients’ needs but also the needs of their families and caregivers. In the related literature, PC measurement tools exist, such as Quality Care Questionnaire-PC (Barros et al. Reference Barros, Bassi-Dibai and Pontes-Silva2021) and Palliative Performance Scale (Anderson et al. Reference Anderson, Downing and Hill1996).
When the literature in Turkey is reviewed, it is seen that 4 different measurement tools are used in evaluation studies related to the PC (Akay and Özdemir Reference Akay and Özdemir2021; Akdeniz-Kudubes et al. Reference Akdeniz-Kudubes, Bektaş and Ayar2019; Hocaoğlu et al. Reference Hocaoğlu, Hepgül and Tunnard2020; Kocatepe et al. Reference Kocatepe, Kayıkçı and Saygılı2020). Only one of these scales evaluates palliative nursing care. This scale evaluates a limited number of components (death care, patient- and family-centered care, pain, delirium, dyspnea, and communication) (Akdeniz-Kudubes et al. Reference Akdeniz-Kudubes, Bektaş and Ayar2019). Other scales assess neonatal nurses’ PC attitudes and PC patients’ concerns and needs (Akay and Özdemir Reference Akay and Özdemir2021; Hocaoğlu et al. Reference Hocaoğlu, Hepgül and Tunnard2020; Kocatepe et al. Reference Kocatepe, Kayıkçı and Saygılı2020). However, the nursing care given in PC should be holistic and the quality of nursing care should be evaluated regularly. For this reason, there is a need for measurement tools that evaluate the PC given by nurses holistically in Turkey. These measurement tools should provide a detailed and practical assessment by addressing all bio-psycho-social dimensions of patients. It should include not only the care needs of the patient but also the needs of their families and the post-mortem care process.
The Palliative Nursing Care Quality Scale (PNCQS) deals with the patient, patient family, and caregiver with a multidimensional approach (Zulueta-Egea et al. Reference Zulueta-Egea, Prieto‐Ursúa and Bermejo Toro2020). The PNCQS, it contains all components that are recognized as essential components of PC by EAPC and the Worldwide Hospice Palliative Care Alliance (symptom management, effective communication, family involvement in care, assessment of family needs, preparing the family for the possible death of the patient, and providing support and spiritual care during bereavement).
The other significant point related to the scale is that the items are linguistically, culturally appropriate and understandable for Turkish society. Thus, it is thought that PNCQS can be a highly efficient tool by which PC nurses in Turkey can evaluate the care they provide and notice important clues helpful in increasing the quality of care. Therefore, this study was conducted to evaluate the validity and reliability of the Turkish version of the PNCQS. At the same time, it was planned to evaluate the quality of care of nurses giving PC and the factors affecting the quality of care.
Validation studies determine the suitability of a tool presented in the literature for a population, and only then can it be used. It is thought that a comprehensive assessment tool for nursing care is needed to evaluate the quality and effectiveness of PC in Turkey. With this scale after its validity, nursing care areas that need to be supported and strengthened in PC can be determined. Some possible suggestions for improving health-care services will be presented to meet the identified needs. It can be expected that announcing suggestions to meet these needs in different countries can be essential in promoting PC. Based on this idea, it is predictable that Palliative Nursing Care Quality Scale–Turkish (PNCQS-T) can be used as a PC assessment tool in Turkey. After the validation phase, this scale can be used in further studies to present the care data about patients needing PC to the world literature.
Method
Participants
In the present study aiming to test the validity and reliability of the Turkish adaptation of PNCQS, using a methodological research design, the population consisted of nurses working in the PC clinic, oncology clinic, and intensive care unit of a university hospital. Other clinics were excluded from the scope of the study as they did not provide PC and end-of-life care. Inclusion criteria for the nurses can be listed as follows: providing PC and end-of-life care, willingness to participate in the study, and having at least 6 months of experience working in the units providing PC services. The study population consisted of 230 nurses working in the PC clinic, oncology clinic, and intensive care unit.
The sample size in validity and reliability studies should be 5–10 times the number of scale items (Özdamar Reference Özdamar2016; Tabachnick and Fidell Reference Tabachnick and Fidell2013). Since the scale contains 20 items, The total number of nurses included in the present study should be between 100 and 200. In the study, the scale was distributed to 230 nurses. However, 16 nurses did not want to participate in the study and 5 nurses had less than 6 months of working experience in these units. The research was completed with a total of 209 nurses.
Data collection instruments
Study data were collected online using the Personal Information Form and the PNCQS-T. The Personal Information Form designed by the researchers consisted of 9 questions regarding the sociodemographic and clinical characteristics of nurses providing PC.
Palliative nursing care quality scale
Zulueta-Egea et al. (Reference Zulueta-Egea, Prieto‐Ursúa and Bermejo Toro2020) consists of 20 items and a single subdimension. The scale was designed as a 5-point Likert type (1 = never, 2 = rarely, 3 = sometimes, 4 = mostly, and 5 = always). The scale consists of items that deal with a PC with a holistic approach. The items evaluate care as a whole, such as controlling and eliminating symptoms (such as pain, dyspnea, constipation, anxiety, and asthenia), countering the needs of family and primary caregivers, ensuring their participation in care, and establishing a therapeutic relationship with them and providing spiritual support. The total score that can be obtained from the scale varies between 20 and 100 points, with high scores indicating that the PC provided by nurses is of desired quality. In the original scale study, the Cronbach’s alpha value of the scale was 0.94 and the explained variance rate was 62.7%.
Development process of the research
The 5-stage model proposed by Brislin (Reference Brislin, Altman, Rapoport and Wohlwill1980) was utilized as a roadmap for translating the PNCQS into Turkish (Brislin Reference Brislin, Altman, Rapoport and Wohlwill1980). (1) PNCQS, originally in Spanish, was translated into Turkish by 2 professional translators. (2) The translation of each item was examined in terms of content integrity and their characteristics of correctly representing nursing care. (3) The items were translated back into Spanish by 2 different professional translators. (4) The lexical consistency of each item translated into Spanish with the corresponding item in the original scale was evaluated. (5) Finally, semantic editing was conducted by Turkish linguistics and nursing experts.
A pilot study was conducted with 32 nurses to check the comprehensibility of the items from the target group. The evaluation determined that all the items were comprehended in the target language and culture. The data obtained during the pilot application were not included in the factor analysis. After the pilot application, the scale was applied to 209 nurses to perform factor analysis. Thirty-six nurses from this group were asked to use pseudonyms on the questionnaires for the test–retest application. According to the literature, the ideal time interval for test–retest application is between 2 and 3 weeks (Özdamar Reference Özdamar2016). Therefore, the questionnaire was applied again to 36 nurses 3 weeks later.
Data analysis
Data analyses were performed using IBM SPSS V25 (Statistical Package for Social Science) and AMOS 21.0 programs. Frequencies, percentages, mean, and standard deviation were used to evaluate categorical and numerical variables. The validity and reliability analyses of the scale were carried out according to the guidelines of the World Health Organization for cross-cultural compatibility studies and the Consensus-Based Standards for the Selection of Health Measuring Devices (COSMIN) (Mokkink et al. Reference Mokkink, Terwee and Patrick2010; World Health Organization (WHO) 2019). Therefore, the Kasser–Meyer–Olkin (KMO) and Barlett Tests were used to determine the sample adequacy of the study. Content validity index, exploratory factor analysis (EFA), and confirmatory factor analysis (CFA) were carried out to determine the validity of the measurement tool. Cronbach’s alpha coefficients were used to determine the reliability of the PNCQS-T, and finally, its stability was evaluated with the Pearson correlation.
Ethical considerations
Permission for conducting the research was obtained from the institutional permission and ethical commission of the university hospital (decision no: 2021–06/10). Participants were informed about the research’s aim and scope, and written informed consent was obtained from each participant. The study was conducted in line with the Declaration of Helsinki.
Results
The study results were presented under 3 separate headings: participant characteristics of the nurses, psychometric measurements, and PNCQS-T scores.
Participant characteristics
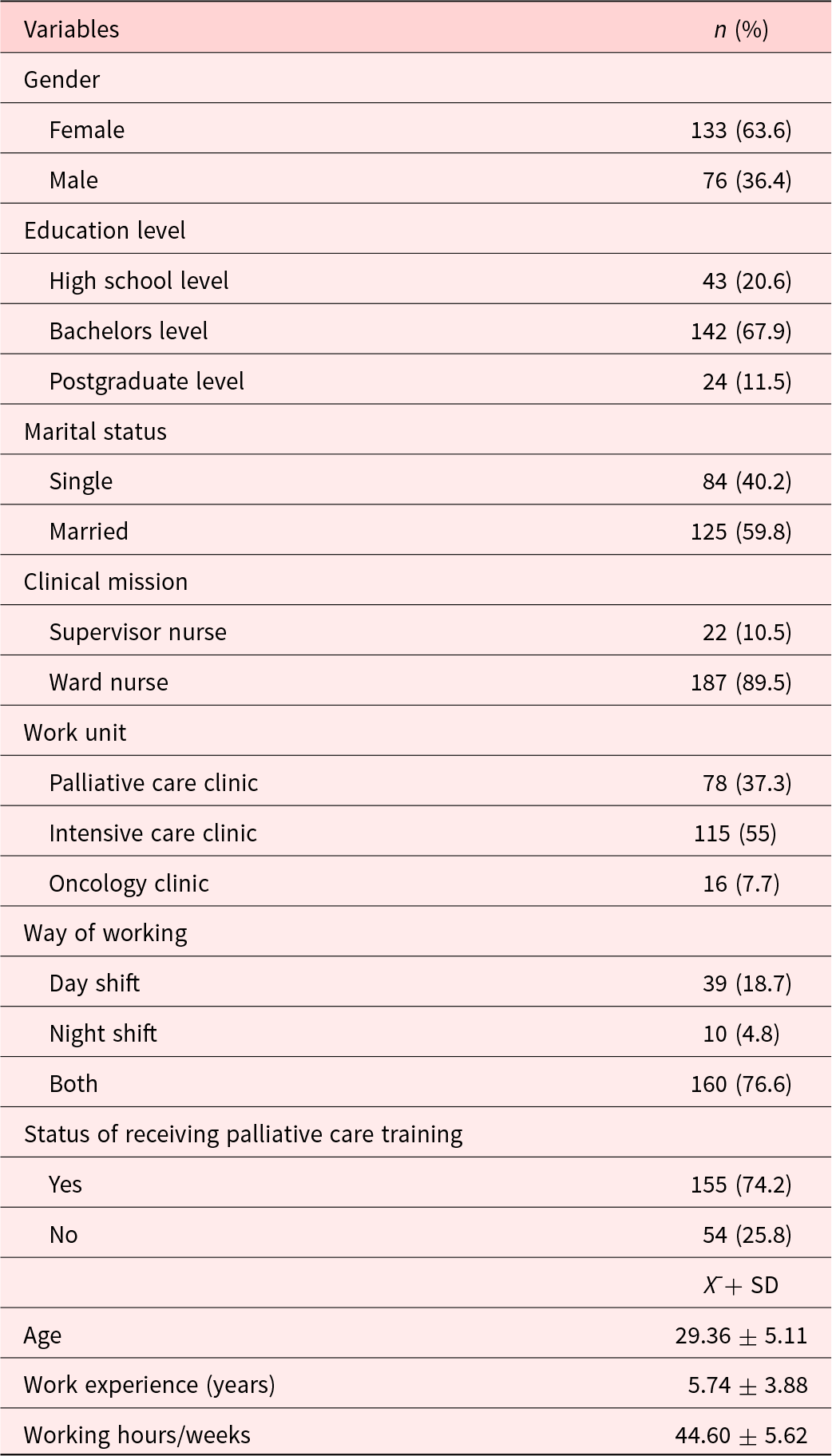
A review of the characteristics revealed that 63.6% of the nurses participating in the study were female, 67.9% had bachelor’s degrees, and 59.8% were married. About 89.5% of the nurses worked as ward nurses, 55% worked in intensive care clinics, and 76.6% worked both day and night shifts. The mean age of the participants was 29.36 ± 5.11, the mean years of their work experience annually was 5.74 ± 3.88, and the mean value of their weekly working hours was 44.60 ± 5.62. About 74.2% of the nurses stated that they had received instruction on the PC (Table 1).
Table 1. Participant characteristics
Psychometric measurements
Content validity ratio
After the translation phase, 10 specialists tested the Turkish language validity of the PNCQS-T. The content validity ratio (CVR) was calculated for each item by considering each expert’s opinions. The accepted CVR value for 10 experts was ≥0.80 (Ayre and Scally Reference Ayre and Scally2014). Since none of the items had a CVR value of <0.80, no item was excluded from the scale.
Pilot study
In the scale adaptation studies, at least 30 participants should be reached in the pilot application, the internal consistency value should be 0.70 and above, and the item-total correlation value should be above 0.30 (Çapık et al. Reference Çapık, Gözüm and Aksayan2018). According to the analysis of the data obtained from the pilot study with 32 nurses, the internal consistency value was found to be 0.95. In addition, there was no item with an item-total correlation value of less than 0.55.
Item analysis
EFA and principal component analysis were used to examine the construct validity and factor structure of the scale. Initially, KMO and Bartlett tests were performed to determine whether the sample size was suitable for factor analysis. In the factor analysis for PNCQS-T, the KMO value was calculated as 0.935. This result shows that the sample size is sufficient for factor analysis (KMO > 0.500). The Bartlett test revealed that the X2 value was 1470.843 and statistically significant (p < 0.05). These results showed that normal distribution conditions of the data were attained. Therefore, it was concluded that the data were appropriate for factor analysis.
Principal component analysis was used in factor analysis. In order to determine the factor structure of the scale, the Scree Plot showing the scattering of the eigenvalues was examined. Factors with an eigenvalue above 1.00 were taken as criteria. As a result of principal component analysis, it was determined that the Turkish version of the scale was collected under a single factor, as in the original version.
Explained variance rate and factor loadings of the items are shown in Table 2. With factor analysis, items with factor loadings below 0.30 are considered inadequate as they contribute <10% variation of the latent construct measured. Hence, it is often recommended to retain items that have factor loadings of 0.40 and above (Boateng et al. Reference Boateng, Neilands and Frongillo2018; Özdamar Reference Özdamar2016; Raykov Reference Raykov2011). Therefore, item 4 (factor load: 0.34) and item 20 (factor load: 0.32) were removed from the scale to provide a strong structure. An examination of the total score correlations of the 18 items that make up the scale revealed that the item-total score correlation values ranged between r = 0.45 and 0.67. The explained variance rate of the scale was 42.1% (Table 2).
Table 2. Descriptive and psychometric properties of PNCQS-Turkish (N: 209)
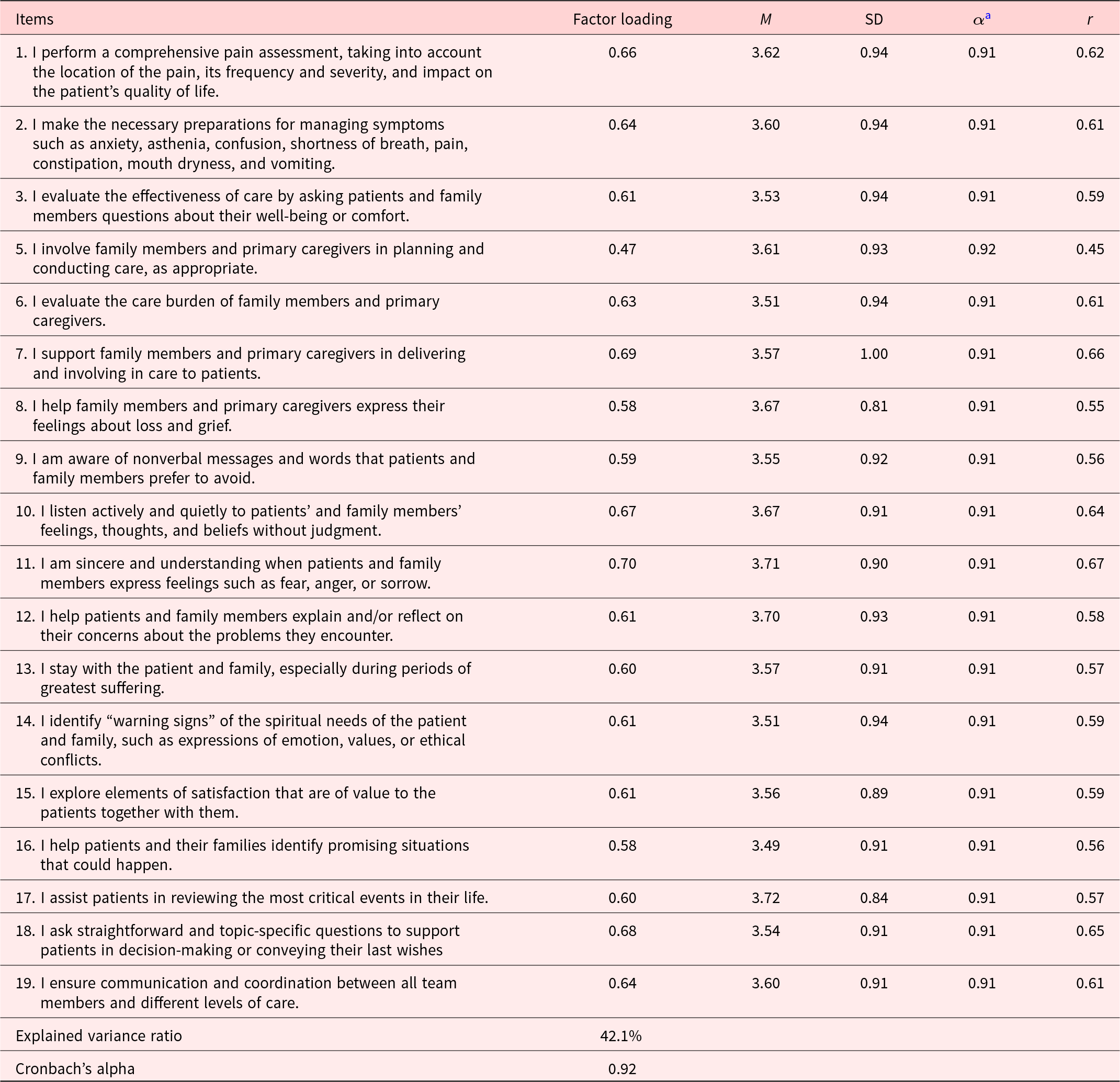
a α Cronbach’s alpha if item deleted; r, corrected item-total correlation; M, mean; SD, standard deviation
Construct validity
CFA was performed to test the construct validity of the PNCQS-T. The findings indicate that the Chi-Square Fit Statistics (CMIN)/degrees of freedom (DF), root mean square error of approximation (RMSEA), comparative fit index (CFI), incremental fit index (IFI), and Tucker–Lewis index (TLI) values were excellent, and the goodness-of-fit index (GFI) values were acceptable (Table 3). The diagram of the AMOS program, in which the CFA analysis was performed, is presented in Figure 1.
Table 3. The goodness-of-fit indices of PNCQS-T (n: 209)
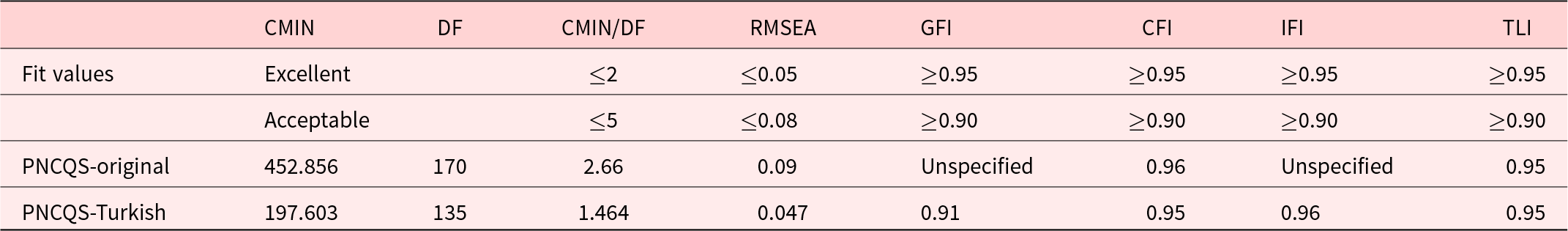
CMIN, χ 2; DF, degrees of freedom; CFI, comparative fit index; GFI, goodness-of-fit index; TLI, Tucker–Lewis index; PNCQS-T, Palliative Nursing Care Quality Scale–Turkish; RMSEA, root mean square error of approximation; IFI, incremental fit index.
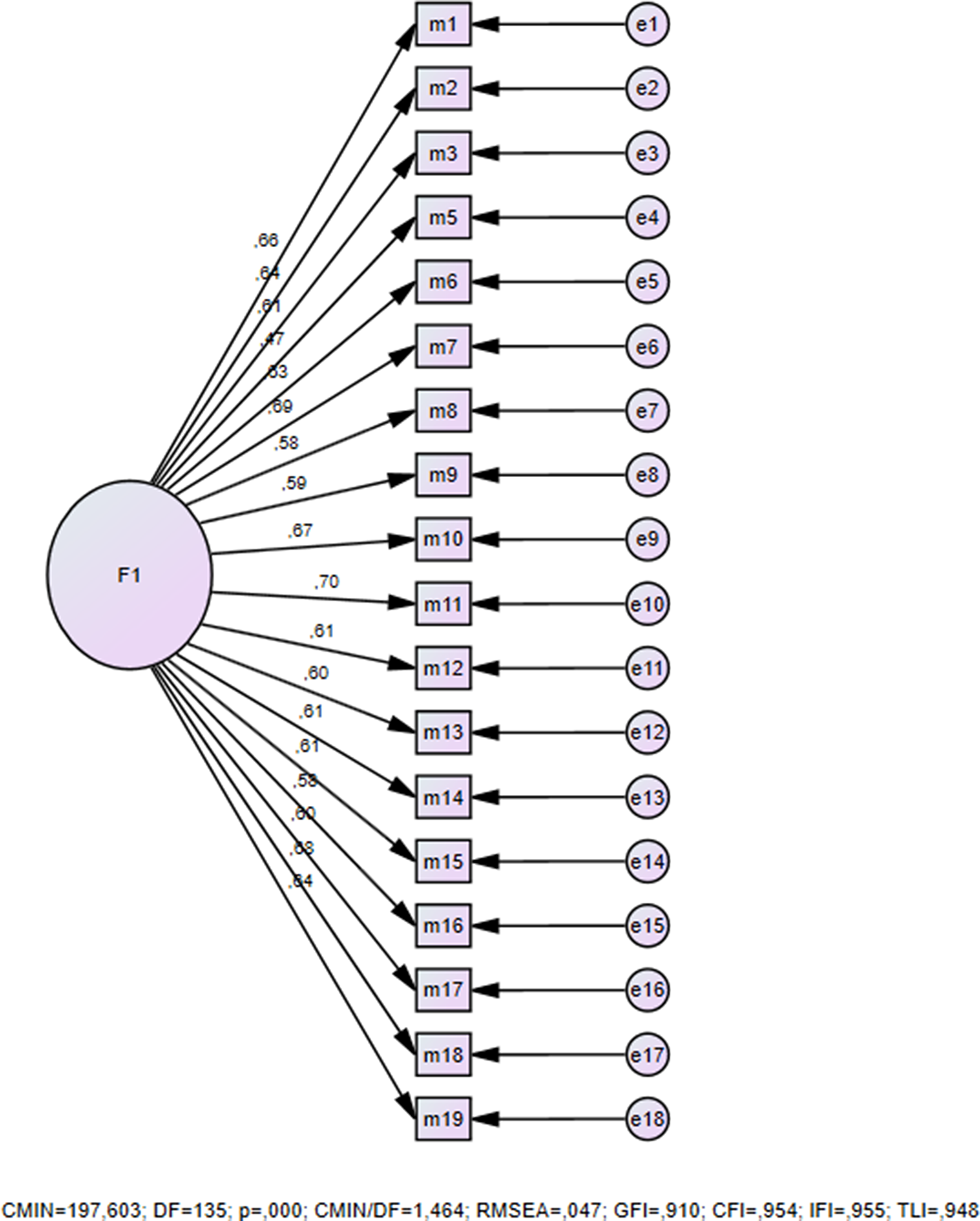
Fig. 1. Construct validity.
Internal consistency
Cronbach’s alpha value was analyzed to determine the internal consistency of the PNCQS-T. The Cronbach’s alpha value of the PNCQS-T was 0.92 (Table 2).
Stability
Thirty pairs of data are regarded as sufficient to test the time invariance of a measurement tool (Özdamar Reference Özdamar2016). Therefore, the PNCQS-T was retested 3 weeks later with 36 nurses. The correlation coefficient of both measurements was found to be r = 0.730, which indicated that measurements obtained from the same participants at different times were significantly correlated (p < 0.05).
Nurses’ PNCQS-T scores
Considering the 18-item version of the adapted scale, the minimum score obtained from the scale is 18 and the maximum score is 90. The comparison of the PNCQS-T mean scores of the participants with their sociodemographic characteristics is given in Table 4. The mean PNCQS-T score of the participants was determined as 64.74 ± 10.66. This result shows that the PC provided by nurses is of high quality.
Table 4. Comparison of nurses’ PNCQS-T mean scores
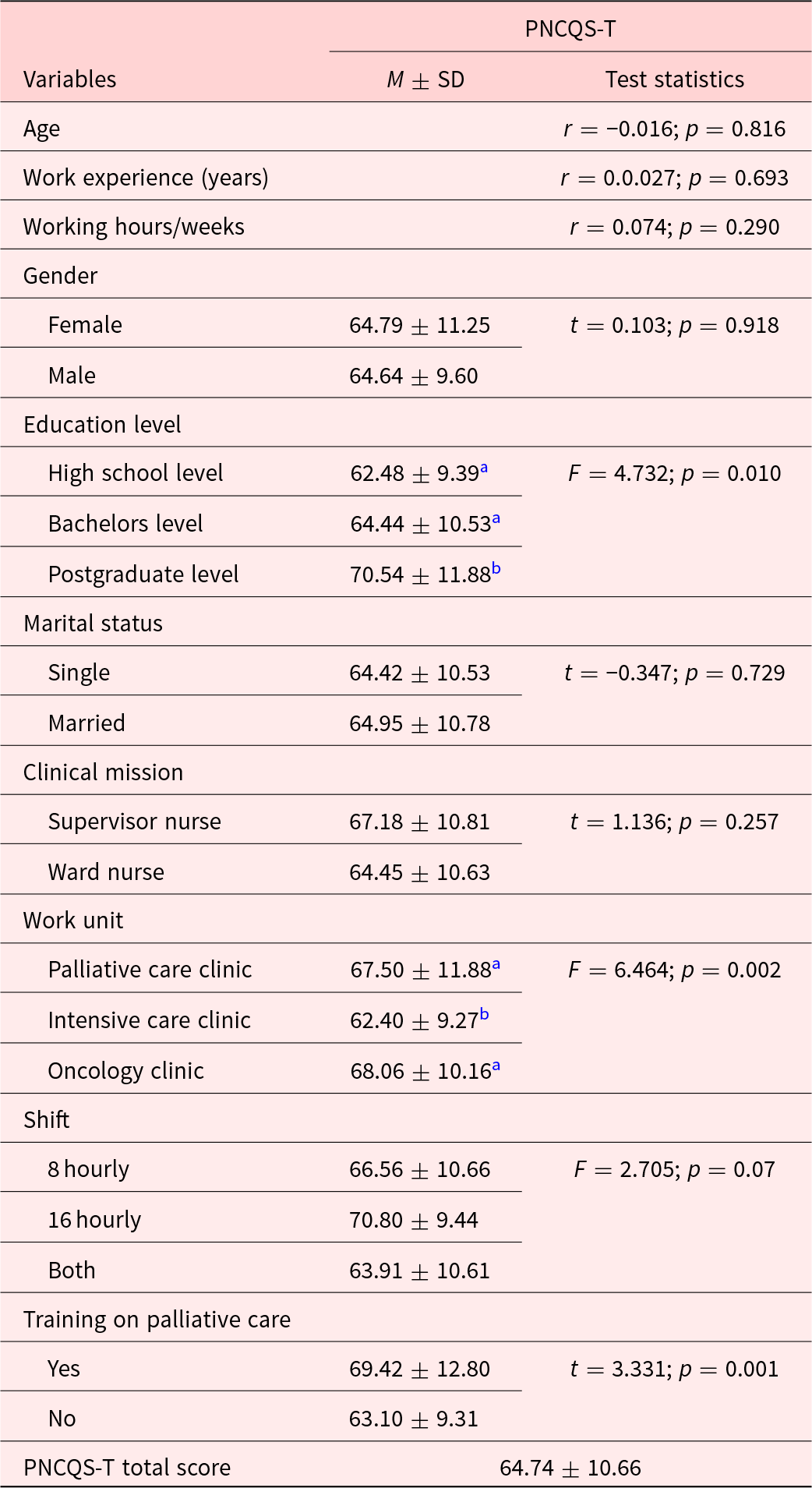
PNCQS-T, Palliative Nursing Care Quality Scale–Turkish; M, mean; SD, standard deviation; F, one-way ANOVA; t, independent samples t test.
a, b there is no statistically significant difference between values with the same letter.
It was noted that there was no relationship between the participant’s age, work experience, and weekly working hours and their PNCQS-T mean score (p > 0.05). At the same time, it was determined that the PNCQS-T score averages of the nurses participating in the study did not show a statistically significant difference in terms of gender, marital status, positions in their clinics, and shift type (p > 0.05). However, the PNCQS-T mean scores of the nurses who were postgraduates and those who had training on PC were found to be statistically significantly higher (p < 0.05). At the same time, the mean PNCQS-T scores of the nurses working in the PC clinic and the oncology clinic were statistically significantly higher than those of the nurses working in the intensive care clinic (p < 0.05).
Discussion
Quality nursing care is a service requested by patients and provided by nurses, directly influencing patients’ well-being (Virdun et al. Reference Virdun, Luckett and Lorenz2020). Therefore, PC provided by nurses should be of efficient quality. Unfortunately, the number of measurement tools that can effectively evaluate PC provided by nurses is limited. However, as in many other countries, PC mainly relies on nursing care in Turkey. Despite this, there is only one scale evaluating palliative nursing care in Turkey (Akdeniz-Kudubes et al. Reference Akdeniz-Kudubes, Bektaş and Ayar2019). In addition, many of these assessment tools focus more on the physical care of patients needing PC. Therefore, there is an inevitable need to provide measurement tools suitable for the nature and philosophy of PC.
Based on this requirement, the validity study of the Turkish adaptation of the PNCQS measurement tool was conducted, and its Turkish version was consistently designed (PNCQS-T). PNCQS addresses the patients, the patient’s family, and the caregiver from a multidimensional perspective (Zulueta-Egea et al. Reference Zulueta-Egea, Prieto‐Ursúa and Bermejo Toro2020). In addition to the components of end-of-life care, PNCQS also deals with many supportive approaches within the context of the grieving process, mainly centering on the family’s coping strategies with post-mortem loss. Evaluation of nursing care in Turkey with this scale will likely enable the overlooked aspects of care to be effectively addressed. It will also contribute to strengthening PC policies by evaluating the levels of the adequacy of care. By introducing this scale, the PC nursing education program in Turkey can be reviewed and revised by drawing attention to the components of integrative care. Updating PC nursing principles and practices may be possible to keep up with global trends. On the other hand, the lack of measurement tools that evaluate PC quality has revealed the need to adapt and introduce this scale to the related literature in Turkey.
EFA and CFA were applied to the data obtained from the study group to determine the construct validity of the PNCQS-T. The concordance statistics obtained from the CFA demonstrated that the 18 items of the PNCQS-T could be grouped under a single factor. The items in this study were grouped into a single-factor structure in parallel with the design of the original scale, and the results of the present study demonstrate significant parallelism with the results obtained in the original study (Zulueta-Egea et al. Reference Zulueta-Egea, Prieto‐Ursúa and Bermejo Toro2020). In the literature review, no other study was found that adapted the original PNCQS to other languages. Therefore, we think it would be scientifically beneficial to repeat the factor structure with sample groups of different sizes.
Cronbach’s alpha internal consistency coefficient was calculated to test the reliability of the PNCQS-T. The PNCQS-T Cronbach’s alpha value was 0.92, which indicates that the scale is a reliable measurement tool. The original study found Cronbach’s alpha value to be 0.94 (Zulueta-Egea et al. Reference Zulueta-Egea, Prieto‐Ursúa and Bermejo Toro2020). Another point in the scale reliability study was determining the invariance against time. The test–retest correlation coefficient is expected to be at least r = 0.70 for a newly developed scale (Özdamar Reference Özdamar2016). The test–retest reliability coefficient (r = 0.73) calculated in the present study has an acceptable value (r > 0,70). PNCQS-T explains 42.1% of the total variance. The higher the total variance ratio, the stronger the scale. Variance values between 40% and 60% are considered ideal in scales which measure attitudes and behavior (DeVellis Reference DeVellis2003). Considering these values, the total variance value of PNCQS-T was sufficient.
The minimum score obtained from the scale is 18, and the maximum score is 90. In this study, the mean PNCQS-T score of the nurses was 64.74 ± 10.66. This result shows that nurses adopt a holistic approach to their patients and provide quality PC services. When the items in the scale were examined, it was determined that the 2 items with the lowest average score were “I help patients and their families identify promising situations that could happen” and “I identify ‘warning signs’ of the spiritual needs of the patient and family, such as expressions of emotion, values or ethical conflicts.” Related literature reveals that there are ethical problems, especially in delivering PC, such as not being fully included in the care of patients and their relatives, not respecting their choices, and not communicating with patients and families in the planning of care (Özkan Reference Özkan2011). Similarly, the present study revealed that nurses did not adequately address the needs of patients and their relatives, especially in terms of spirituality and ethics. Therefore, nurses need to address the moral needs of patients and their families, deliver care by ethical principles and universal values, and provide physical and psychosocial care.
Nurses need to have knowledge about PC to deliver quality PC. According to Kassa et al. (Reference Kassa, Murugan and Zewdu2014), nurses’ PC knowledge level is between 45% and 76.2%, which is low. In this study, the mean PNCQS-T scores of PC education and graduate students were statistically significantly higher. Similarly, many studies in the related literature have also reported a positive relationship between the education level of nurses and their level of knowledge about PC (Huijer et al. Reference Huijer, Dimassi and Abboud2019; Knapp et al. Reference Knapp, Madden and Wang2009; Ronaldson et al. Reference Ronaldson, Hayes and Carey2008). Unfortunately, studies on the subject have determined that nurses generally have insufficient knowledge about PC (Ayed et al. Reference Ayed, Sayej and Harazneh2015; Iranmanesh et al. Reference Iranmanesh, Razban and Tırgarı2014; Prem et al. Reference Prem, Karvannan and Kumar2012; Youssef et al. Reference Youssef, Mansour and Al-Zahrani2015). These studies, conducted in different cultures with different methods, show a need for accurately evaluating the quality of care, thus increasing the quality and training activities promoting knowledge.
Another important finding of the study is that the PNCQS-T mean scores of the nurses working in the PC and oncology clinics are statistically significantly higher than those of the nurses working in the intensive care clinic. The reason for this situation is that the needs of PC patients are different from the needs of intensive care patients. Therefore, PC should be considered a separate area of expertise. Nurses working in intensive care units should receive appropriate training on the components required for PC and evaluate the patient holistically. While further studies are needed to reveal the underlying reasons, it is common knowledge that PC has not yet been fully adopted in all relevant clinics. PC is generally perceived as “supportive care” and “terminal-stage care” and mainly focuses on pain management. Therefore, it is naturally expectable that oncology and PC clinics could be more focused on PC services. However, it should be a priority that PC philosophy and principles be presented more effectively in all fields of nursing instruction and practice, which necessitates a comprehensive reorganization of health policies and instructional and training schemes.
Conclusion
In conclusion, based on the findings of this study, the PNCQS-T has a high item-total correlation value, internal consistency coefficient, and test–retest reliability coefficient as in the original. This result shows that the PNCQS-T is valid and reliable. It is thought that this adapted measurement tool which has a single factor like the original measurement tool can be used as a self-reporting measurement tool based on nurses’ statements. In addition, using the PNCQS-T in PC nursing can provide a holistic evaluation of the care given by nurses working in PC services in Turkey and increase the quality of care.
As another result of our research, it was found that postgraduate education, receiving PC education, and the clinic where nurses work affect the quality of PC. Based on these results, to increase PC quality, undergraduate nursing education curricula should include a “PC nursing course,” and regular PC training should be given to nurses working in the hospital.
Funding
This research received no specific grant from public, commercial, or not-for-profit funding agencies.
Conflict of interest
The authors declare no conflict of interest.








