Introduction
Emergency field amputations are a rare but potentially life-saving procedure. Situations where one may consider a field amputation include entrapped victims in motor vehicle collisions, industrial and agricultural accidents, natural disasters, or terrorist attacks. Reference Ho, Conterato, Mahoney, Miner and Benson1–5 Time is of the essence as the patient or the safety of the scene may rapidly deteriorate, a dedicated traumatic amputation surgical team may not be available, or, in the case of a mass-casualty event, quickly stretched thin as infrastructure fails and resources deplete. Reference Mustafa and Department2 In this context, most of the literature on prehospital amputations is limited to case studies. Few studies have analyzed the tools regularly carried by Emergency Medical Service (EMS) agencies for amputations, and those that do were performed on porcine samples or had limited sample sizes. Reference Emmerich, Stilley, Sampson, Horn, Pollock and Stilley6,Reference Leech and Porter7
As of 2019, only two percent of publicized EMS protocols listed specific tools for field amputation. Reference Emmerich, Stilley, Sampson, Horn, Pollock and Stilley6 Scalpels, the Gigli saw, or electric orthopedic oscillating saws are routinely utilized by hospital and surgical amputation teams. Most of these are not standard equipment carried by EMS crews. Furthermore, few emergency physicians receive training in the use of Gigli saws or amputation techniques, with most textbooks deferring to military medicine and instead focusing on hemostasis. Reference Tintinalli, Ma, Yealy, Meckler, Stapczynski and Cline8
A variety of devices are carried by EMS and fire rescue units. McNicholas analyzed utilizing a hydraulic Holmatro Core cutting device (Holmatro; Glen Burnie, Maryland USA) to perform an amputation. The Holmatro effectively amputated lower extremities but caused significant comminuted bone damage and needed repeat attempts on several occasions. Reference McNicholas, Robinson, Polyzois, Dunbar, Payne and Forrest9 Emmerich compared the Gigli saw, hacksaw, and reciprocating saw on porcine lower extremities and noted a lack of difference in skin, soft tissue, and tendon disturbance while demonstrating a superior time to completion with the reciprocating saw and hack saw. Reference Emmerich, Stilley, Sampson, Horn, Pollock and Stilley10 Reciprocating saws are likely to be more familiar to the prehospital provider as they are standard equipment on fire and rescue units and carried by many EMS physicians. Reference Emmerich, Stilley, Sampson, Horn, Pollock and Stilley6 Holloway, et al did study extremity amputations on cadavers using multiple tools such as the Fiskars tree looper (Fiskars; Helsinki, Finland); however, there was no mention of tissue damage. Reference Holloway, Sordo, Brandfellner, Goode and Aydelotte11
The reciprocating saw has demonstrated the fastest field amputation time compared to the Holmatro extrication device, hack saws, or Gigli saws. Reference Leech and Porter7 Situations where field amputation is necessary are dire, with the general understanding that there are three primary situations where it would be necessary to perform such a procedure: (1) entrapment that will otherwise compromise the patient’s life; (2) entrapment that would otherwise create a dangerous or unsafe rescue environment; and (3) entrapment that would be impossible to extricate without the amputation. Reference Osmond-Clarke12 Therefore, correct, reliable equipment must be available to perform the task and provide the best outcome.
As most EMS providers and their support crews carry reciprocating saws, the goal in this study was to assess which saw blade would offer the best outcomes and the quickest extrication of an entrapped patient in an experimental setting. The blades that were compared differed in their teeth-per-inch (TPI) and, in turn, the material they were designed to cut.
This is the first published study to specifically evaluate if the TPI of a reciprocating saw blade impacts the speed and success of a field amputation.
As field amputations are rare, studies and data are limited to case reports and few studies comparing tools on animal models or cadavers. This study’s objective was to experimentally compare four different commercially available reciprocating saw blades when used for amputations on cadavers in a controlled environment. The saw blades differed in TPI, which measures how many saw teeth can fit in an inch when measured from the tooth bottom or gullet. Typically, blades with higher TPI are recommended to cut metal and harder materials, while lower TPI are recommended for wood and softer materials.
The primary outcome was to compare the amputation speed. Secondary outcomes were the degree of tissue damage present, and how difficult the operating repair would be, instrument malfunction rate, the temperature increase of the blade, the amount of splatter, and subjective user feedback.
Methods
Study Design and Setting
The study was performed at the Texas Tech University Health Sciences Center Paul L. Foster School Of Medicine, Department of Medical Education Cadaver Lab in El Paso, Texas USA on two self-donated cadavers. The cadavers were both elderly males and lightly embalmed; neither had suffered from extremity trauma or any condition affecting the limbs’ integrity (to the authors’ knowledge). Multiple procedures had already been performed on the cadavers, including thoracotomies, cricothyroidotomies, and fasciotomies. Despite this, the architecture of the limbs was intact and undamaged by previous procedures. Specifically, all bones and connective tissue were untouched by instrumentation before the experiment, except for two proximal thighs with an escharotomy through the skin.
Four participants performed the study’s amputations: a board-certified Emergency Medicine physician with an EMS subspecialty certification and three Emergency Medicine residents, all with prior emergency medical technician/EMT training. None of the users had performed a live field amputation. All participants wore full personal protective equipment.
The study was exempt from the IRB process as approval was not required on research involving previously collected, non-identifiable human tissue samples.
Eight guillotine amputations were performed with each blade. All amputations had a proximal tourniquet placed but not fully tightened as the tissue was not living and therefore could not demonstrate effective tourniquet application. The distal limb was secured in a vice to simulate an entrapment. Upper limb amputations included the distal and proximal forearm and humerus. Lower limb amputations included the distal and proximal tibia-fibula and femur. There were four amputations per limb, and a total of 16 amputations were made per cadaver. A total of 32 amputations were performed. Amputations took place from distal to proximal, with all amputations being approximately eight-to-ten centimeters proximal from the vice. Saw operators were assigned in a rotating fashion such that each anatomical site was amputated by every operator at least twice with minimal operator fatigue. Each blade was utilized to perform all eight amputations in succession then switched to a different TPI blade type. The saw battery was replaced with a new fully charged saw battery after 16 amputations.
Tool Selection
The equipment used was a Craftsman V20 cordless reciprocating saw providing 3,000 strokes per minute and a one-inch stroke length (Craftsman; Towson, Maryland USA). Four blades were tested in total. Three nine-inch blades were used: a Diablo 3-TPI DSO903CP carbide pruning blade (Diablo Tools; High Point, North Carolina USA), a DeWalt 6-TPI DWAR966 bi-metal designed for wood demolition applications (DeWalt; Baltimore, Maryland USA), and a DeWalt 10-TPI DWAR960 bi-metal designed for metal and wood demolition. The fourth was an eight-inch DeWalt 14-TPI DW4809 bi-metal blade designed for metal demolition. The Diablo 3-TPI is further described as having “large gullets… for fast chip removal in extreme cutting applications” and coated with a “Perma-Shield,” which is advertised to prevent gumming or sticking (Diablo Tools). The DeWalt 6-TPI and 10-TPI are both described as having a patented tooth form for optimized chip removal; however, no details about design are offered (DeWalt Demolition Bimetal). The DeWalt 14-TPI was the only of the series from that brand advertised as having “anti-stick coating” similar to the Diablo blade. It was also cited to have a patented sharper tooth design (DeWalt 8”). Nine-inch and an eight-inch blades were selected as pretrial blade assessment revealed the 12-inch blade and longer blades had unsatisfactory lateral movements often described as “whipping” back and forth. It was also noted that none of the tools utilized in this study have Food and Drug Administration (FDA; Silver Spring, Maryland USA) approval for human subjects. Times were kept using a stopwatch with millisecond capabilities, and blade temperatures were taken with a laser thermometer. Data analysis was performed with Excel for Mac Version 16.7 by the Microsoft Corporation (Redmond, Washington USA).
Methods
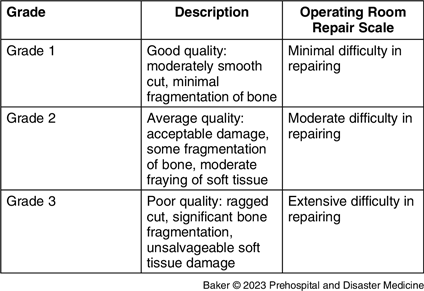
The saw was brought to full speed, and timing was initiated at skin contact and stopped at limb disconnection. All attempts were made at 90 degrees to the limb’s axis and performed in a guillotine fashion in the transverse plane as performed during emergency battlefield medicine. Reference Osmond-Clarke12 A visual depiction of placement of the vice grip and the location of the sequential amputations can be seen in Figure 1. The number of attempts was recorded; the temperature of the blades immediately pre- and post-amputation were recorded with a laser temperature probe. The rescuer’s perceived effort to complete the amputation was recorded; subjective splatter and limb damage were evaluated. Splatter was recorded on a three-point scale with one representing minimal splatter isolated to the immediate surroundings of the amputation; two representing tissue splatter to the surroundings, including the operator’s arms; and three being significant splatter extending up the operator’s chest and including the operator’s face/eyes. The amputation was deemed a failure if it could not be completed in one guillotine attempt, and/or if a “rescue” method was employed. The rescue method was a #10 surgical scalpel for any tissue that the saw blade was having difficulty cutting. Post-procedure, four photographs of the limb were taken for post-amputation orthopedic analysis: head-on, 90 degrees horizontal, 60 degrees horizontal, and 60 degrees vertical. All photos were subsequently analyzed by an orthopedic attending physician, blinded to the blade used, and graded on a damage scale. The amputation was graded on the amount of tissue damage present and how complicated the subsequent operating room repair would be. No grading system currently exists to score the quality of a prehospital amputation, so the scale described in Table 1 was utilized.
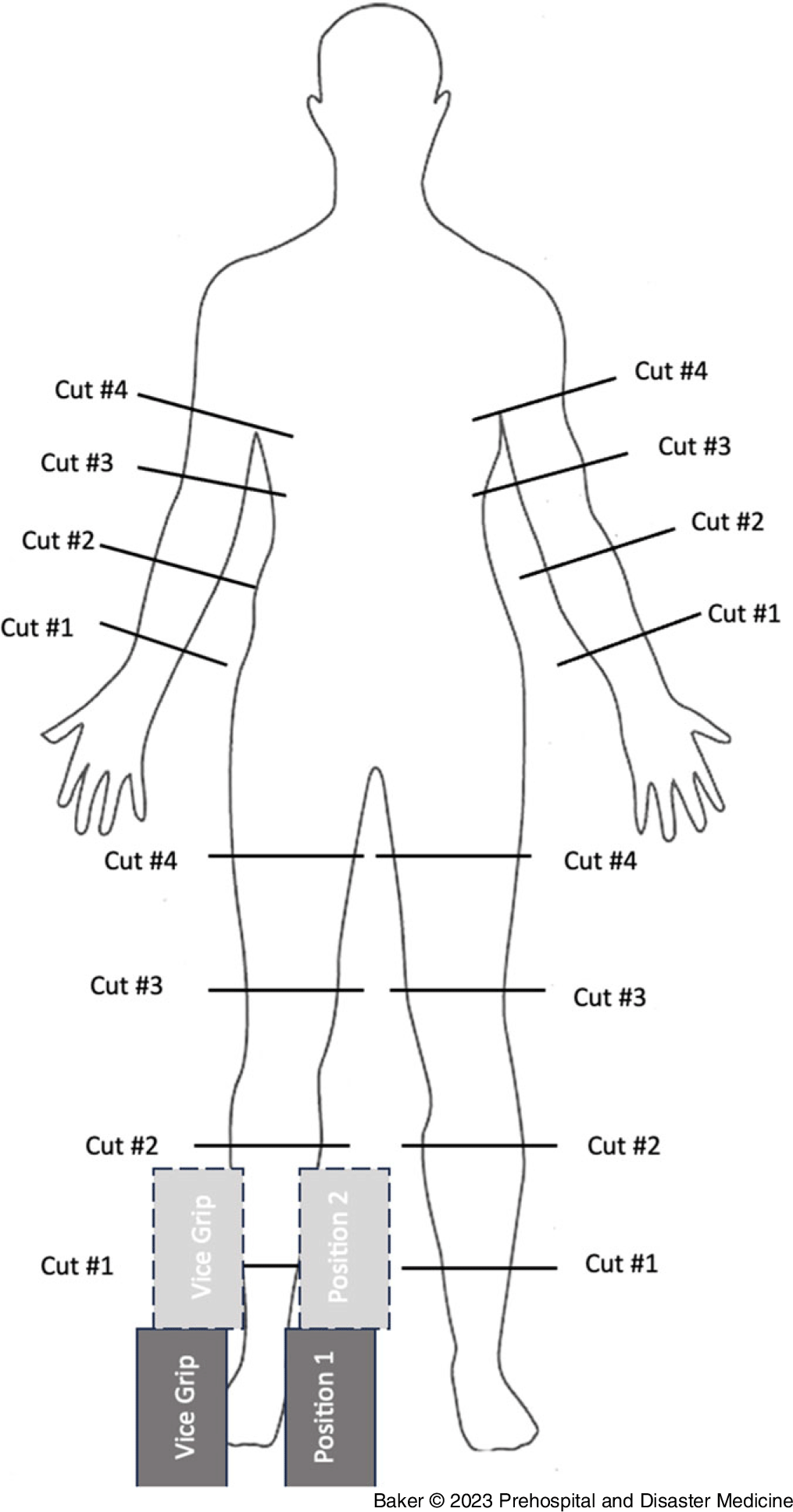
Figure 1. Visual Depiction of Amputation Strategy.
Table 1. Scale and Gradation of Tissue Damage and Feasibility of Operating Room Repair
Results
Primary Outcomes
The results from the amputations can be found in Table 2. The primary outcome of amputation speed was different between the blades, and results are presented in both the time it took to saw through one centimeter of tissue and the time it took to perform the actual amputation by body location in Figure 2 and Figure 3.
Table 2. Time in Seconds per Centimeter of Tissue by Blade Used
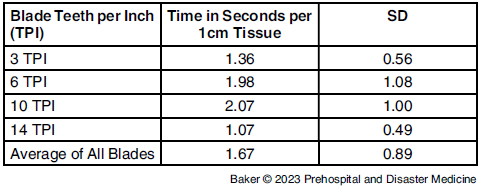
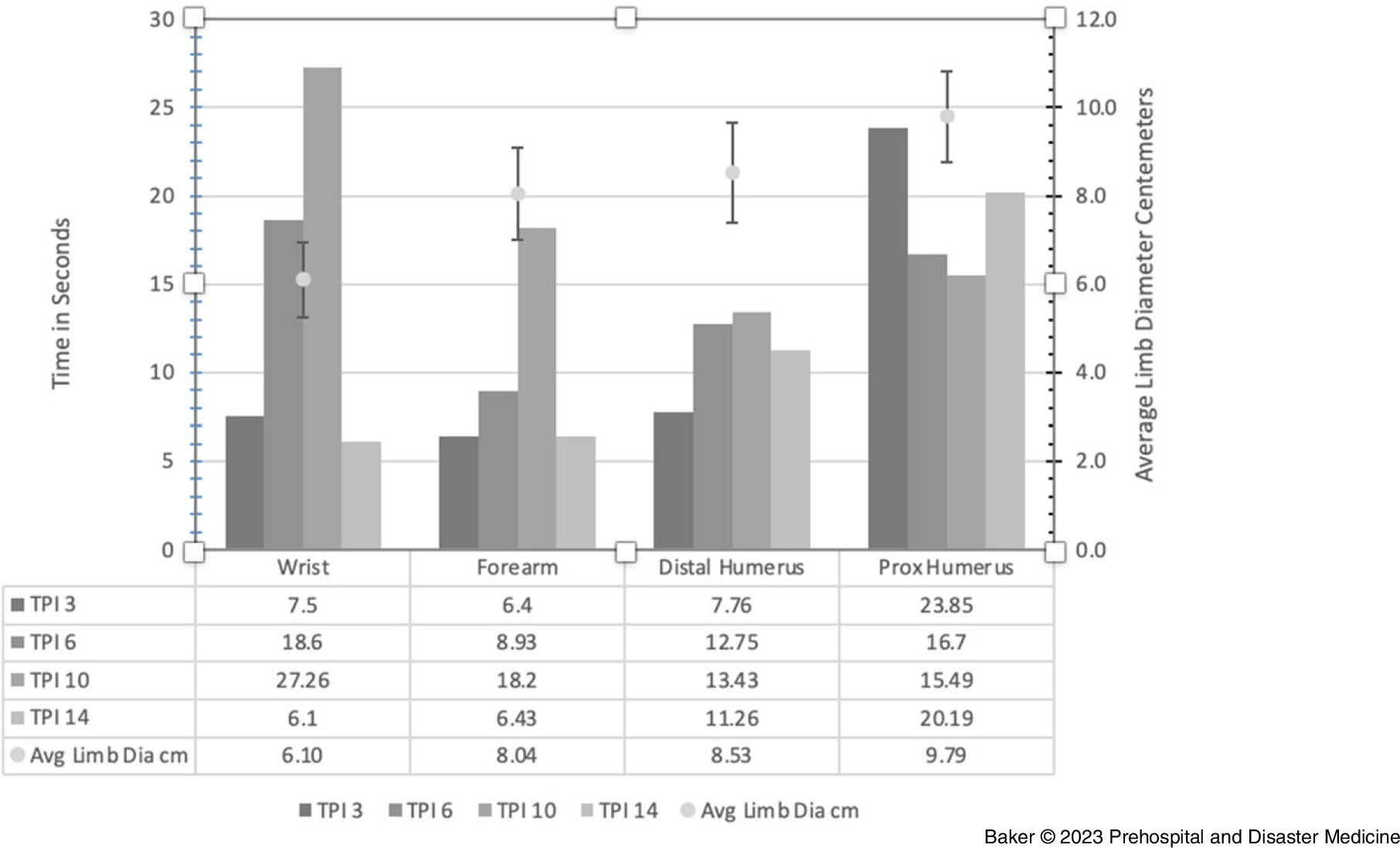
Figure 2. Amputation Time versus Average Limb Diameter Upper Extremity.
Abbreviation: TPI, teeth-per-inch.
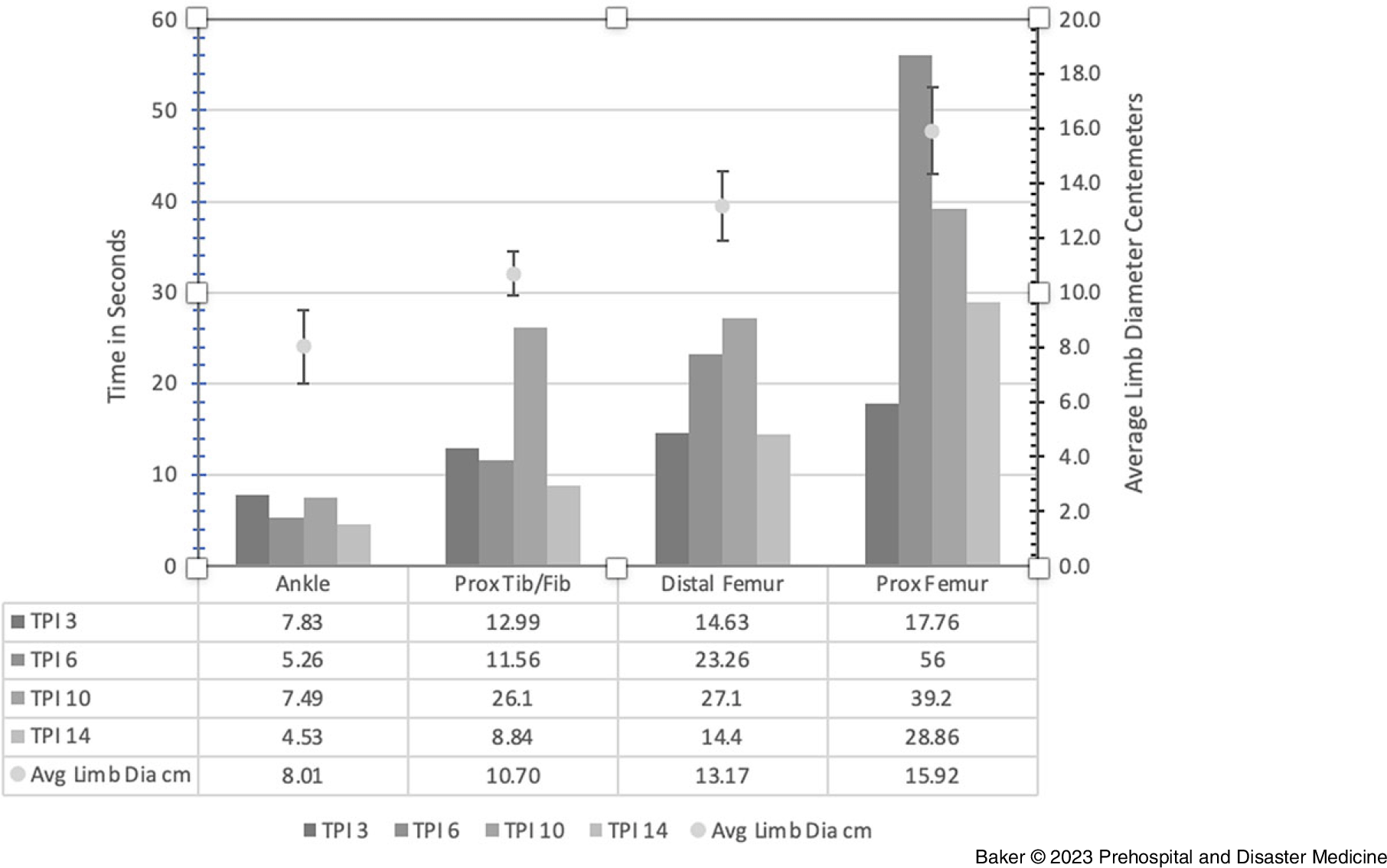
Figure 3. Amputation Time versus Average Limb Diameter Lower Extremity.
Abbreviation: TPI, teeth-per-inch.
The secondary outcome was evaluating blade failures. A total of 11 failures were observed. Blade failure was defined as any cut that required a blade repositioning or a rescue technique to be used. All the failures consisted of the blade cutting through the soft tissue and supporting osseous structures, leaving tendons and soft tissue on the underside. At this point, the blades latched onto the remaining tendonous and cutaneous structures and moved them back and forth without cutting through them. A scalpel was utilized as a successful amputation rescue technique in every failure.
The blades’ temperature was measured pre- and post-procedure to detect if any significant burn, cautery, or potential ignition source would be produced from the amputation technique. The highest temperature increase was seen on 3-TPI and was an 8°C increase from 16°C to 24°C when amputating the distal femur. None of the blades were noted to create a spark during the amputation procedure.
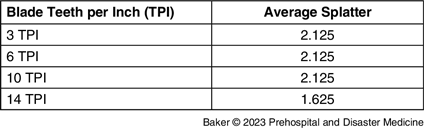
The blades’ amount of splatter is summarized in Table 3 and was equal for all blades except for the 14-TPI blade. The 3-TPI, 6-TPI, and 10-TPI blades all produced splatter up the arms and some onto the face shield, but the 14-TPI blade produced a minimal to moderate amount of splatter limited to the operator’s arms and the local area surrounding the amputation.
Table 3. Average Splatter by Blade
Operator perceived effort was unaffected by which blade was utilized. All amputators rated all the amputations as “easy” on a four-point scale from easy, moderate, difficult, and extremely difficult.
A blinded attending orthopedic surgeon performed a post-amputation analysis to evaluate the guillotine amputation technique’s quality and if the blade type would affect the post-amputation operative repair. He was given high-resolution photos of each cut in multiple different angles and then was asked to rank the damage caused by the blade on a one-to-three scale and how difficult the operative repair would be on a one-to-three scale (one being the easiest, three being the most difficult). Table 1 summarizes the detailed descriptions of these scales.
Overall, the 14-TPI blade caused the least damage and the blade with 3-TPI caused the most tissue damage. The 14-TPI blade was deemed to cause wounds that were the easiest in terms of surgical repair, followed closely by the 10-TPI blade. The only blade that was deemed a three was the blade with 3-TPI at the proximal femur. The surgeon commented: “At this very proximal level, with the observed jagged and irregular cuts, additional bone and soft tissue would have to be taken to permit skin closure and if this was not possible, may result in a hip disarticulation.” He also felt that utilizing the guillotine amputation technique on the proximal joint locations may not provide enough skin and tissue to repair the amputation without performing a disarticulation at the joint in the operating room.
Discussion
A prehospital amputation is a high-risk, rare procedure for entrapped patients where the most difficult decision is usually the decision to perform the procedure. The key to good outcomes for patients with prehospital injuries is timely extrication and transport to definitive care. Reference Brown, Rosengart and Forsythe13 Furthermore, entrapment situations tend to be high risk for the providers as the most common reported scenario where amputation is needed in the field is structural collapse. Reference Gander14 Although many tools have been described as appropriate for this procedure, a powered tool can significantly decrease the time a victim is entrapped and EMS time on the scene. Data on the use of power tools are sparse; however, as in the most recent meta-analysis on prehospital amputation, of the 14 cases found and described, only one was reported to have used a reciprocating saw. Reference Gander14 Keeping in mind patient outcomes and provider safety being heavily reliant on a multitude of factors, chief among them time, the goal in this study was to provide data on commonly available reciprocating saw blades so that the decision to cut remains the only factor to resolve.
The study revealed a reciprocating saw with a 14-TPI blade was superior across all aspects examined. It was the quickest, caused the least damage to the patient, created the least exposure to a patient’s bodily fluids and tissues, and was least likely to fail. Nevertheless, all blades tested could successfully perform a limb amputation if an additional commonly encountered instrument to cut soft tissue like a scalpel were also available.
Depending on the blade, the average time to perform a guillotine amputation of an extremity was between 1.07 seconds per one centimeter of tissue (SD = 0.49 seconds) for the 14-TPI blade to 2.07 (SD = 1.0) second per one centimeter of tissue for the 10-TPI blade. It remains unclear if this small-time difference is clinically significant when performing a prehospital amputation. It has been estimated, based on porcine models, that a reciprocating saw using a 12-inch 14-TPI blade would take 16 seconds to amputate a human mid-calf. Reference Emmerich, Stilley, Sampson, Horn, Pollock and Stilley6 In this study on cadaveric specimens, it was demonstrated that the below the knee amputation would take between 8.84 to 12.99 seconds to complete.
Secondary outcomes revealed the 14-TPI blade generating less heat, potentially making it the safer blade to utilize of the ones tested. The 14-TPI blade had zero failures, not needing an amputation rescue technique to be employed, and being optimum for surgical repair.
Strengths
This study was performed with multiple variables controlled and measured. The variety of operators included females and males, those who consider themselves familiar with electric saws and those who had rarely used one, and various upper body strength levels. The inclusion of an orthopedic surgeon to evaluate the high-resolution pictures taken of the cadaver is a notable strength since surgery will always be the patient’s ultimate fate if they survive the field amputation. The orthopedic surgeon was blinded to the technique used, the blade TPI, operator size or gender, and reported results solely on the post-procedure pictures. As far as the authors know, there are no other similar studies on field amputations that include orthopedic surgeon input.
Limitations
The study does have multiple limitations. Elderly male cadaveric specimens were utilized that were lightly embalmed and over one-month post-mortem, which could alter the tissue and bone strength. There is always post-mortem tissue degradation altering the tissue’s integrity despite embalming techniques. The cadavers may have had osteoporotic bone compared to a younger cadaver, and the tissue preservation may have affected the pliability and retractability of the muscle and soft tissue specimens. This may have contributed to clogging of the saw blade teeth, blade dulling, and the soft tissues’ laxity contributing to blade failures.
The repeat usage of the saw blades and battery drainage may contribute to instrument failures, but each blade only performed eight amputations and may be an accurate representation of a lightly used reciprocating saw blade found in the prehospital environment. Likewise, despite battery changes, power levels could have varied between cuts, although no subjective degradation was perceived. This, however, is another reality of prehospital medicine where equipment can degrade despite regular care.
The adjustable vice used to simulate an entrapped extremity may have also been insufficient to recreate an actual crushed and entrapped extremity. This method was utilized for all amputations to minimize cofounding variability between amputation equipment and operator.
Only one attempt at the guillotine amputation technique was allowed, and if the blade did not cut through all tissues, a rescue technique was utilized. The duration of saw use was subjective based on the operator’s perceived chance of success. It is possible that with multiple repositioning techniques, the reciprocating saw may have been able to complete the cut.
The temperature of the reciprocating saw motor was not measured, which may provide enough heat to be a potential ignition source if volatile gasses are present at the scene, but it is unknown at this time.
Finally, the amputation technique consisted of an amputation in the transverse plane amputating from top to bottom. This represents the limb’s optimal positioning, which may rarely be encountered in the prehospital environment, and as commented by the orthopedic surgeon, may not be the ideal cut for a good patient outcome.
The operators measuring the subjective outcomes worked individually without conferring, but had seen the technique performed, creating a potential observer bias. This bias would be minimized, as each provider performed eight amputations.
Finally, a proximal tourniquet was applied but not cinched down thoroughly before each amputation, which may have affected the amputation success.
Conclusion
In studying the saw blades that can be used with a reciprocating saw for the purposes of field amputation, the use of a 14-TPI blade is suggested as the tool of choice. The 14-TPI blade was demonstrated to be the quickest, the most reliable while producing the least fluid and tissue splattering, and easiest predicted in-hospital operative repair.
Conflicts of interest/funding
This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors. The authors report no conflict of interest.
Author Contributions
RB was responsible for the study design, oversight, data analysis, and manuscript writing. PP and SM participated in the study and contributed to manuscript writing and revisions. WW performed grading of limb damage and operating room repair. SB oversaw data collection, photography, and manuscript revisions.









