Introduction
To date, hemorrhage remains the first cause of potentially preventable death in trauma. Reference Eastridge, Holcomb and Shackelford1 For life-threatening bleeding originating from the limbs, tourniquets are used in the prehospital setting, often allowing the patient to reach the hospital alive. Reference Richey2–Reference Kragh, Littrel and Jones4 Proper use of tourniquets is associated with increased systolic blood pressure on arrival to the emergency department, decreased use of blood products, and lower incidence of limb-related complications, which may lead to improved long-term outcomes and increased survival in trauma patients. Reference Smith, Ochoa and Wong5,Reference Covey and Gentchos6
Traditionally, tourniquets have been used in military settings and by Emergency Medical Services; however, there is strong evidence in the literature supporting their use by non-medical personnel. Reference Lee, Porter and Hodgetts7–Reference Teixeira, Brown and Emigh13 To spread awareness about the importance of using antihemorrhagic devices, in 2015, the American College of Surgeons (ACS; Chicago, Illinois USA) launched the Stop the Bleed campaign. Reference Rasmussen, Baer and Goolsby14,15 Its main aim is to train bystanders to act as immediate responders and treat massive external bleeding in emergency settings. Reference Goolsby, Jacobs and Hunt16 Since the training program’s inception, over 117,222 accredited instructors have held more than 134,510 classes in 118 different counties, certifying more than 2.4 million people as Stop the Bleed providers. 17
These recent efforts by the ACS have increased interest in tourniquets among civilians, and as more and more people are trained, it is reasonable to assume that the demand for tourniquet purchases by the non-medical civilian populations will continue to increase. However, due to the multitude of manufacturers, the majority of tourniquets available online are not recommended by the Committee on Tactical Combat Casualty Care (CoTCCC; Fort Sam Houston, Texas USA), have not obtained the Conformité Européenne (CE) marking, and have not been certified by the US Food and Drug Administration (FDA; Silver Spring, Maryland USA). Sparse anecdotal evidence and media coverage have reported the risk of “catastrophic failure” and reduced effectiveness in stopping limb hemorrhage when using counterfeit tourniquets. Reference Pegues18,Reference Elliott19 However, despite the diffusion of unlicensed models in the market and their use especially among the civilian population, the resilience and efficacy of uncertified tourniquets remain unclear. This study aims to compare CoTCCC-recommended and FDA/CE-certified Combat Application Tourniquets (CAT) Generation 7 tourniquets (CAT Resources, LLC; Rock Hill, South Carolina USA) with uncertified CAT look-alike tourniquets (LA-TQ) for differences in cost, length, force applied, force variation, and rupture rate.
Methods
The CAT consists of an external rod that rotates and allows an increasing circumferential pressure to the limb through a windlass system (Figure 1). When the pressure exerted on the limb is greater than the intravascular pressure, the blood flow is stopped. The CAT was selected for three main reasons: (1) they are one of the oldest commercial tourniquets, thus making them easy to find on the market, both in their certified and uncertified versions; (2) the CAT is one of the recommended tourniquets for the Stop the Bleed program and is included in public access Stop the Bleed kits; and (3) they are widely available world-wide. Reference Kragh, Burrows and Wasner20–22 The LA-TQ were selected based on visual appearance and immediate availability during an online search. Certified tourniquets are defined as tourniquets that have been certified by the FDA and marked with the sign of CE. For the LA-TQ sample, the absence of CE certification was assessed by visually inspecting the devices and the material provided by the manufacturer for the CE marking, and by searching for the devices, using the device name and manufacturer, on European online databases containing a list of CE-certified products. 23,24 To verify the devices’ lack of FDA approval, an online search of the LA-TQ was conducted using the FDA catalog of cleared and approved medical devices. 25 Tourniquets without FDA approval and CE certification were considered uncertified and could be included in the study. To ensure the generalizability of this study’s findings, the two groups of LA-TQ were purchased from two different vendors in two widely used and internationally available e-commerce retail platforms (Amazon [Seattle, Washington USA] and AliExpress [Hangzhou, Zhejiang, China]). After comparing the two groups for length and cost (ie, 25 CAT and 50 LA-TQ), all tourniquets were tested on a manikin’s leg. Tourniquet length (ie, the length of the strap, excluding the buckle) was assessed before each single-use application. During the application, the rupture rate, the force applied at the time of application, and its variability during one-hour and six-hour applications were measured. Tourniquet rupture was defined as complete mechanical failure (ie, breakage of the windlass, c-clip, or strap) during the positioning or application of the tourniquet. The rupture rate was calculated as the ratio between the tourniquets that suffered complete mechanical failure and the total number of same-type tourniquets used.

Figure 1. (a) Tourniquets Used in the Study, a Combat Application Tourniquet (top), and Two CAT Look-Alike Tourniquets (LA-TQ) (bottom and center); (b) Experimental Setup; and (c) Sensor Disposition: A Total of Eight Force Sensors were Positioned on Two Lower Limbs of a Manikin (four sensors per limb).
For measuring the force applied by the tourniquets, the setup described by Viola and colleagues was used. Reference Viola, Lagazzi and Ballardini26 Eight force-sensing resistors (FSR 402; Interlink Electronics; Camarillo, California USA) were positioned on the two lower limbs of a medical-grade manikin, below the groin (Figure 1). All tourniquets were positioned on the force-sensing resistors by Stop the Bleed instructors: the strap was tightened until no slack was appreciated between the tourniquet and the mannequin’s leg; the windlass rod was left free from the c-clip and kept perpendicular to the longitudinal axis of the mannequin’s leg until it was time to perform the windlass turns. Following tourniquet positioning, three clockwise 180-degree windlass turns were performed. The number of turns was decided based on evidence in the literature indicating that three turns are effective in obliterating the dorsalis pedis pulse at Doppler auscultation during most lower-limb applications. Reference Weppner, Lang, Sunday and Debiasse27 Each application lasted either one hour (20 CAT and 41 LA-TQ) or six hours (five CAT and nine LA-TQ), and force was recorded from the positioning to the end of the session at a sampling frequency of 1Hz. The force of each tourniquet was obtained by averaging the data from three sensors (ie, excluding the one under the plastic stabilization plate). Reference Viola, Lagazzi and Ballardini26 To compare the performance of the two groups of devices in the one-hour session, the averaged force after the application (five minutes after the third turn, h0) and at the end of the session (ie, the last five minutes, h1) were computed for each tourniquet. Further investigation was conducted to determine whether the applied force changed when the tourniquet was left in place for six hours. For each device tested in the six-hour sessions, the force was averaged in the last five minutes of each hour (h1 to h6).
Statistical Analysis
All the data were analyzed using Matlab R2021b (The MathWorks Inc.; Natick, Massachusetts USA) and SPSS Statistics 25 (IBM Corp.; Armonk, New York USA). Length difference was assessed using unpaired t-test. To analyze the force applied during the one-hour and six-hour sessions, a repeated-measure ANOVA was performed. The main effects included “Group” (two levels: CAT and LA-TQ) and “Time” (two levels for the one-hour session; six levels for the six-hour session) as between and within factors, respectively. Before running the ANOVAs, the normality of the data was assessed using the Anderson–Darling test; since the null hypothesis was rejected, the data were normalized using the fractional rank method. Reference Templeton28 Sphericity was also tested using Mauchly’s test, and when it was rejected (ie, six-hour recordings), the Greenhouse–Geisser correction was applied. Statistical significance was set at the family-wise error rate of α = 0.05.
Results
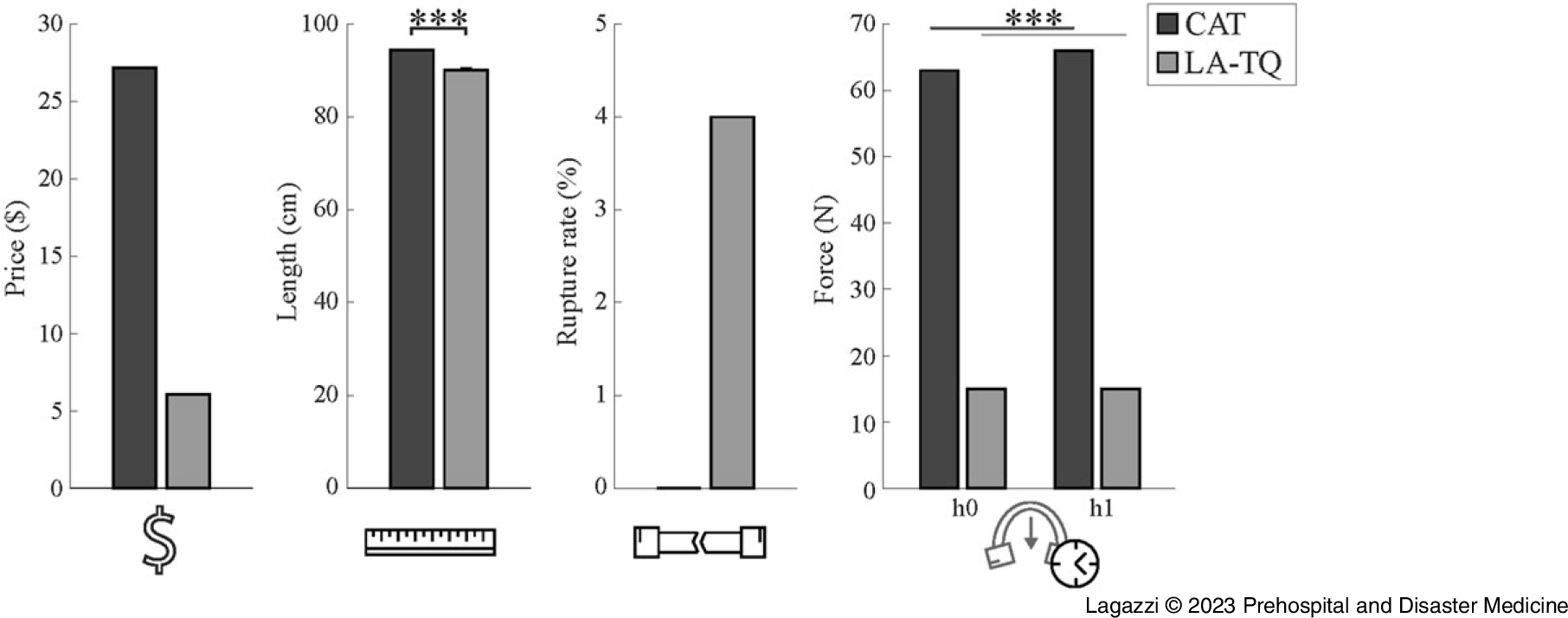
A total of 75 tourniquets, of which 25 CAT and 50 LA-TQ, were included in this study. As the tourniquet size is one of the parameters evaluated by the CoTCCC, the length of the CAT and LA-TQ prior to the application was assessed. Compared to the CAT, the LA-TQ were significantly shorter and had higher variability (CAT: mean 94.5 [SE = 0.1] cm; LA-TQ: 90.1 [SE = 0.5] cm; P <.001). The LA-TQ were cheaper than the CAT (mean price per device: US$6.07 versus US$27.19). Out of 75 devices tested, two of the LA-TQ and zero of the CAT broke during the positioning (4% versus 0%; Figure 2).

Figure 2. Bar Graph Showing the Differences in Price, Length, Rupture Rate, and Force Applied between Combat Application Tourniquets (CAT) and CAT Look-Alike Tourniquets (LA-TQ).
Note: *** indicates P <.001.
Analysis of one-hour recordings revealed that the force applied was significantly different in the two groups, with greater forces applied by the CAT compared to the LA-TQ (CAT: 65 [SE = 3] N; LA-TQ: 14 [SE = 1] N; group effect: F [1,73] = 105.65; P <.001); Table 1. Interestingly, the force applied increased significantly over time only in the CAT group (time effect: F [1,71] = 4.08; P = .047; time*group effect: F [1,71] = 11.36; P = .001). Analysis on a subset of devices (five CAT and nine LA-TQ) positioned for six hours showed similar results. During the six-hour sessions, the CAT applied greater force than the LA-TQ (group effect: F [1,12] = 9.79; P = .009; Figure 3). Nevertheless, both groups did not lose application force for the entire duration of the session (time effect: F [1.32,15.85] = 2.38; P = .138; time*group effect: F [1.32,15.85] = 2.63; P = .117).
Table 1. Force Applied by the Two Groups of Tourniquets (mean [SE]) at the Beginning (h0, namely first five minutes after the third turn) and the End of the One-Hour Application (h1, minutes 55 to 60)

Abbreviations: CAT, Combat Application Tourniquet; LA-TQ, look-alike tourniquets.

Figure 3. Force Applied by the Two Tourniquet Types during the Six-Hour Application.
Note: The points show the mean force computed averaging the last five minutes of each hour (h1-h6); the bars indicate the standard error of the mean of the force recorded. ** indicates P <.01.
Abbreviations: CAT, Combat Application Tourniquet; LA-TQ, look-alike tourniquets.
Discussion
When compared to the CAT, the LA-TQ were cheaper, shorter, had a higher rupture rate, and applied reduced force. While in both groups the initial application force was maintained throughout the experiment, the CAT demonstrated an increase in applied force during the observation compared to the LA-TQ.
Currently, uncontrolled limb bleeding remains a leading cause of preventable death, Reference Davis, Satahoo and Butler29 with tourniquets playing a major role in managing life-threatening extremity hemorrhage in the prehospital setting. Regardless of the type or mechanism of action, the tourniquet’s main function is to apply on the limb a circumferential pressure superior to the arterial pressure, thus obliterating arterial flow to the extremity. Even in certified devices, the application of insufficient force by the tourniquet due to incorrect application (eg, too much slack, insufficient windlass turns, or incorrect positioning) is associated with increased blood loss, major limb complications, and limb loss. Reference Inaba, Siboni and Resnick12,Reference Polston, Clumpner, Kragh, Jones, Dubick and Billings30–Reference King, van der Wilden, Kragh and Blackbourne35 Namely, insufficient application force can result in the failure of obliterating the distal arterial blood flow while blocking venous return from the limb, which may lead to venous tourniquet application with paradoxical bleeding, limb edema, and compartment syndrome. Reference King, van der Wilden, Kragh and Blackbourne35,Reference Mikdad, Mokhtari and Luckhurst36 The findings of this study show that the LA-TQ applied a significantly lower force than the CAT, despite optimal tourniquet application by Stop the Bleed instructors in a controlled setting. While it remains unclear if the difference in the applied force between the two cohorts is due to the use of different materials in the main tourniquet components or to subtle mechanical differences, it is reasonable to assume that the LA-TQ application by untrained personnel in an emergent setting might lead to an even lower application force than what was reported in this study. While the use of tourniquets is not without risks, there is strong evidence in the literature supporting the use of appropriately positioned certified tourniquets in the setting of life-threatening extremity hemorrhage. Reference Richey2,Reference Smith, Ochoa and Wong5,Reference Eilertsen, Winberg, Jeppesen, Hval and Wisborg11 Conversely, the use of uncertified tourniquets unable to reach an adequate pressure could potentially lead to adverse outcomes, especially in the context of wide-spread public use. In this framework, complete mechanical failure of the tourniquet could further decrease the chances of achieving bleeding control in life-threatening limb hemorrhages. While there are limited data in the literature regarding failure to control the bleeding following tourniquet rupture, Weppner and colleagues showed that mechanical failure, defined as the rupture of one of the tourniquet key components, was associated in all cases with the inability to stop the distal pulse. Reference Weppner, Lang, Sunday and Debiasse27 In the present study, the LA-TQ had a higher rupture rate compared to the CAT. The observed difference in rupture rates between the cohorts, due to the implications of a complete mechanical failure in the setting of life-threatening hemorrhage, strongly supports the need for further testing of what devices are available to the public and advocates for increased layperson education on the use of uncertified devices.
The CoTCCC process to evaluate commercial tourniquets is based on a multi-parameter scoring that includes the effectiveness of arterial occlusion; speed and easiness of application; optimal occlusion pressure; size and weight; occurrence of published complications, failures, or safety issues of devices; and combat usage reports, civilian usage reports, and user preferences in literature. Reference Shackelford, Butler and Kragh8 In the present study, the straps of the LA-TQ were significantly shorter compared to the CAT. While there is a paucity of data in the literature regarding the impact of strap length on tourniquet efficacy, it can be presumed that for the tourniquet to be secured through the buckle, the strap length should be superior to the circumference of the limb. In a study conducted on the US military population, the average thigh circumferences ranged from 49cm to 77cm. Reference Gordon, Churchill and Clauser37 Within this specific population, the strap lengths of both the LA-TQ and the CAT would be greater than the limb circumference. However, it must be noted that due to the increased prevalence of obesity in the civilian population, further studies need to be done to assess if shorter straps might have detrimental effects on tourniquet use, especially in lower limb applications. Reference Stierman, Afful and Carrol38
Limitations
Several limitations must be considered. All tourniquet applications were performed on a simulated limb in a controlled setting. While the use of a manikin allowed for prolonged application times, future studies should replicate the present results in a more realistic scenario, such as in perfused models. Another limitation concerns the fact that the tourniquet applicators were not blinded to the tourniquet type they were using due to the small visual differences (ie, the printed logo on the strap, and the raised lettering in the strap buckle and windlass rod). To ensure optimal tourniquet application despite this limitation, five Stop the Bleed instructors were enrolled to position the devices. Furthermore, the number of LA-TQ tested was twice the number of the CAT (50 versus 25). During the design phase, to increment the generalizability of the present study’s findings, two groups of 25 LA-TQ devices were purchased from two distinct high-volume vendors. However, since the two groups’ price, visual aspect, and commercial availability were nearly identical, the decision was made to pool all LA-TQ devices within one group, regardless of the vendor. This is supported by one of the results of this study, as the standard error of the mean force applied by all LA-TQ was as low as 1N, suggesting that they applied a similar force. Lastly, it was not possible to include in this study all types of LA-TQ currently available online, as this number is high and constantly increasing. For the purposes of this exploratory study, the choice was made to include two tourniquets that are immediately available to the general public on two international and widely used e-commerce platforms. Future studies will be required to: (1) determine whether the LA-TQ could produce the same force as the CAT devices, with a higher number of turns, without breaking; (2) assess whether laypersons can safely and effectively position the LA-TQ; and (3) determine physical and mechanical properties of the LA-TQ.
Conclusion
The LA-TQ applied a significantly lower force and had a higher rupture rate than the CAT, potentially affecting tourniquet performance in the context of public bleeding control. Due to the increased availability of uncertified tourniquets to non-medical users, the Stop the Bleed campaign would be the optimal framework to provide increased layperson education regarding the use of certified devices. Lastly, these findings warrant additional investigations on the effectiveness of uncertified devices in real-world applications.
Conflicts of interest/funding
The authors have no conflict of interest to disclose. No external funding was obtained for the realization of this study.
Acknowledgments
This study was conducted primarily by members of the Italian Trauma League, a non-profit organization with the main goal of furthering trauma-related knowledge and education. The authors thank Giorgio Carlini for his help in designing the measurement tool, and Maura Casadio and Marco Chirico for their support in the design and data acquisition phases.
Authors Contributions
EL and MB designed the study; GB, LV, and SR designed and implemented the measurement tool; EL, AD, LV, EM, VV, MB, and SR ran the experiments; GB, LV, and SR analyzed the data; EL, AD, GB, EM, VV, MB, DK, JL, and SR wrote and revised the manuscript.