Introduction
Congestive heart failure (CHF) with acute pulmonary edema (APE) is associated with significant mortality and high consumption of intensive care services in the hospital. Reference Sacchetti, Ramoska, Moakes, McDermott and Moyer1–Reference Wilson, Kwiatkowski, Millis, Purakal, Mahajan and Levy3 There are limited data regarding the incidence of CHF with APE in the prehospital setting; in-hospital data suggest that 16% of patients admitted with decompensated heart failure present with APE. Reference Sacchetti, Ramoska, Moakes, McDermott and Moyer1 Sublingual (SL) nitrates, which are commonly used in the prehospital setting for treatment of APE, frequently fail to provide adequate reductions in preload and afterload; this experience is confirmed by physiological and clinical studies which suggest that high doses of nitrates are required to achieve the rapid reductions in preload and afterload that form the cornerstone of treatment of APE. Reference Uil CA4–Reference Kelly, Gibbs and O’Rourke7
A common approach to treating APE in the prehospital setting includes SL nitroglycerin (NTG) and continuous positive airway pressure (CPAP). This approach is suboptimal for two reasons. First, the bioavailability of SL NTG is poor. Reference Noonan and Benet6 Second, it is impractical to deliver SL NTG concomitantly with CPAP. As both nitrates and CPAP have been shown to improve outcomes in APE, providers utilizing this approach are forced to choose between removing the CPAP mask to administer SL NTG or prolonging the time to drug administration. Reference Cotter, Metzkor and Kaluski5,Reference Hubble, Richards, Jarvis, Millikan and Young8–Reference Bertini, Giglioli and Biggeri11 In-hospital studies have suggested that high doses of intravenous (IV) nitrates are both safe and effective for the treatment of APE, showing rapid reductions in blood pressure, improvements in oxygenation, and reduced need for invasive airway management and intensive care unit (ICU) admission. Reference Wilson, Kwiatkowski, Millis, Purakal, Mahajan and Levy3,Reference Levy, Compton and Welch12–Reference Hsieh, Lee, Kao, Hsu and Chong15 Previous work and clinical guidelines also suggests that mortality is improved by earlier administration of vasoactive medications to patients with decompensated heart failure. Reference Peacock, Emerman, Costanzo, Diercks, Lopatin and Fonarow16–Reference Cotter, Kaluski, Moshkovitz, Milovanov, Krakover and Vered19 Most recently, work by Patrick, et al has suggested the safety of prehospital administration of high-dose IV bolus (IVB) NTG for the treatment of APE. Reference Patrick, Ward and Anderson20
This study describes the implementation of a prehospital treatment algorithm that utilizes IVB NTG at a dose of 400mcg, a lower dose than has been previously described, as well as a subsequent maintenance infusion available for prolonged transport times. All patients received initial treatment with SL NTG and CPAP, as tolerated.
Methods
This is a retrospective chart review of all Emergency Medical Services (EMS) patient care reports of patients who received IVB NTG for APE from May 1, 2019 through January 31, 2020 in a large, geographically diverse EMS system in Minnesota and Wisconsin (USA). The service operates approximately 125 ground ambulances and seven helicopters across the service area. Ambulances are staffed by a mix of emergency medical technicians and paramedics; the helicopters are staffed by certified flight paramedics and registered nurses. The service transports approximately 70,000 patients per year, some 3,500 of these are by air. An exemption from review was granted by the Institutional Review Board of North Memorial Health (Robbinsdale, Minnesota USA).
Patients were deemed eligible for treatment under this protocol according to inclusion criteria outlined in the departmental training program and treatment protocols, as outlined in Figure 1. The diagnosis of APE was clinical and based on the attending paramedic or nurse’s impression. Emphasis was placed on history of heart failure and/or APE and/or the presence of physical exam findings consistent with APE (eg, pulmonary rales, pink frothy sputum, severe dyspnea, and orthopnea) and oxygen saturation (SpO2) ≤93% prior to treatment. Reassessments of the patient were conducted every two minutes according to the Treatment Algorithm (Figure 2) and consisted of evaluation for on-going signs of APE, including dyspnea, rales, hypoxia, and systolic blood pressure ≥120mmHg.
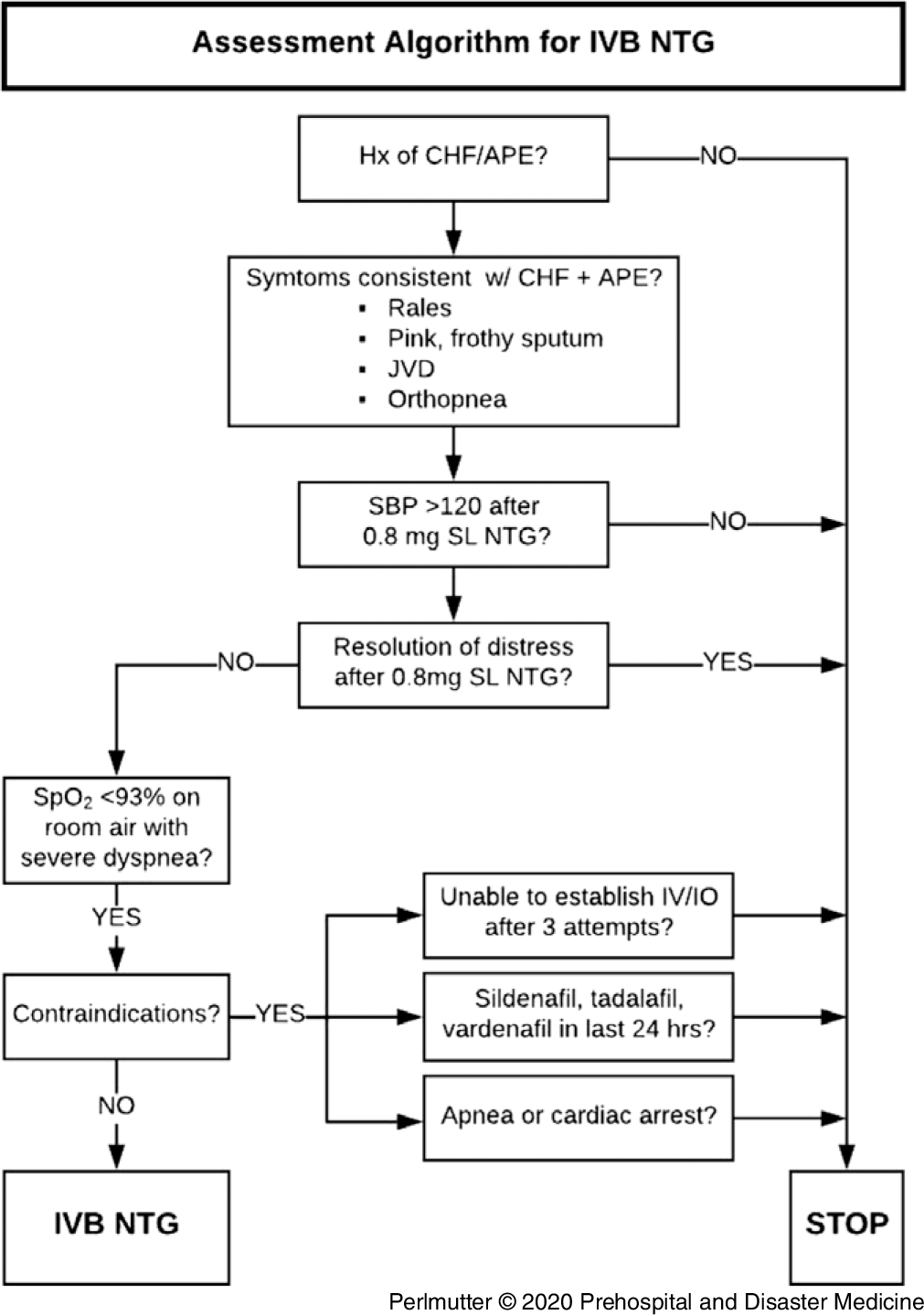
Figure 1. Assessment Algorithm for IVB NTG.
Abbreviations: APE, acute pulmonary edema; CHF, congestive heart failure; IO, intraosseous; IV, intravenous; IVB, intravenous bolus; JVD, jugular venous distention; NTG, nitroglycerin; SPB, systolic blood pressure; SpO2, oxygen saturation.
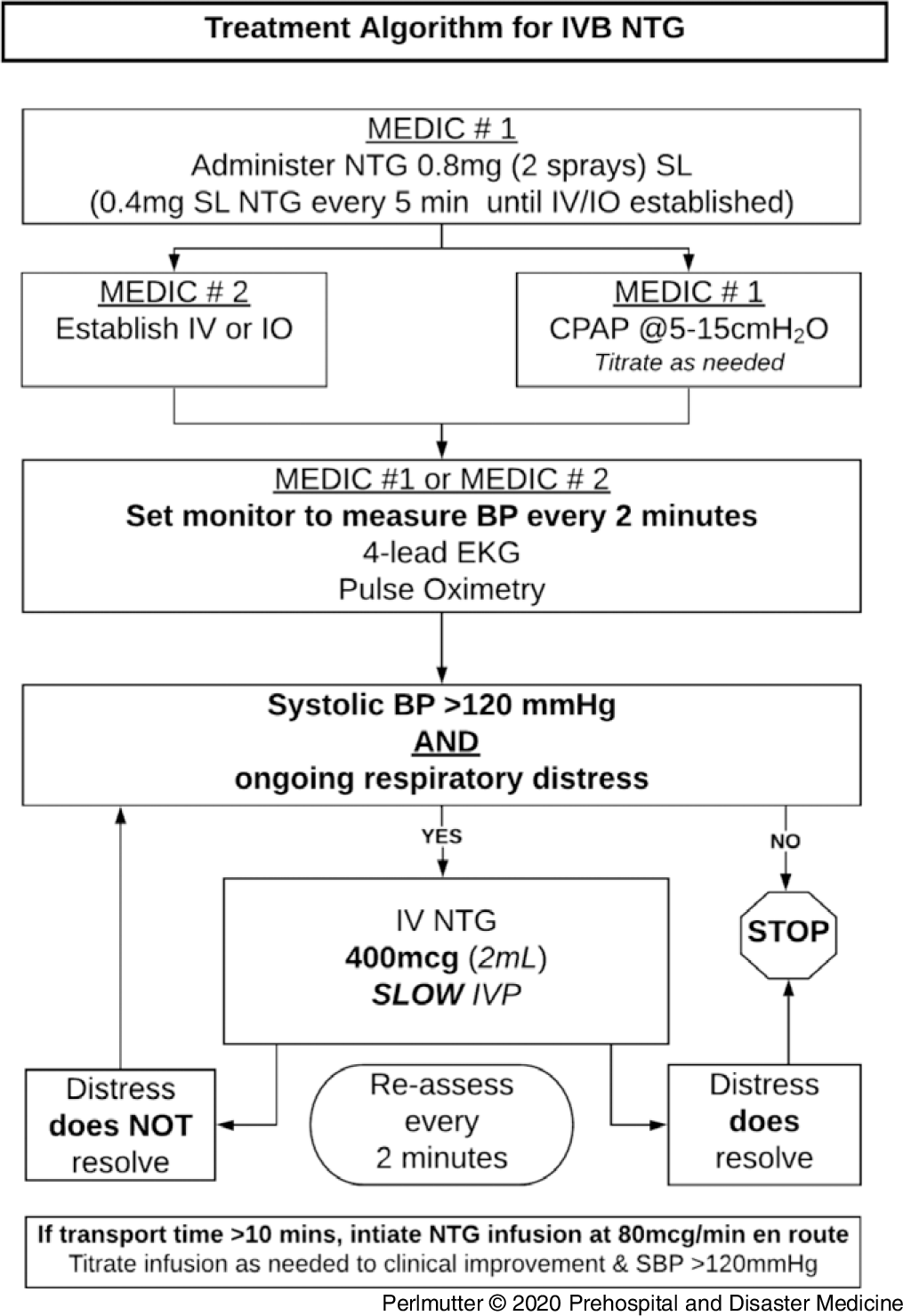
Figure 2. Treatment Algorithm for IVB NTG.
Abbreviations: BP, blood pressure; CPAP, continuous positive airway pressure; EKG, electrocardiogram; IO, intraosseous; IV, intravenous; IVB, intravenous bolus; NTG, nitroglycerin; SL, sublingual; SPB, systolic blood pressure.
Patients whose symptoms of severe respiratory distress did not resolve following the administration of 800mcg of SL NTG were placed on CPAP, as tolerated, after which 400mcg of SL NTG was administered every five minutes until vascular access was established, at which point 400mcg IVB NTG was administered every two minutes and repeated as necessary, as outlined in Figure 2. For patients with on-going respiratory distress and estimated transport times greater than 10 minutes, an infusion of IV NTG was initiated at 80mcg/min and titrated to effect. Patients no longer judged to be in severe respiratory distress after initial SL NTG were excluded from treatment with IVB NTG and were treated with CPAP and further SL NTG if necessary.
Initial chart review included a search in the electronic patient care record (ePCR) database for all patients who received NTG by any route of administration during the study period. From these, all cases were identified in which NTG had been administered by IVB, IV infusion, or both. Abstractors were trained and monitored and used a standardized data abstraction form to collect data from EMS ePCRs. Conflicts regarding data abstraction were resolved through a consensus process among the authors. Study variables included demographic information, medical history, and vital signs throughout the encounter. Electrocardiogram findings, patient transport times, and EMS on-scene times were reviewed. Data regarding doses and route of administration of all NTG administered were collected. The incidence of CPAP use was tabulated, as well as the incidence of advanced airway management. Finally, the incidence of out-of-hospital cardiac arrest was assessed in the cohort of patients treated with IVB NTG.
Analysis was completed using Microsoft Excel version 16.37 (Microsoft Corporation; Redmond, Washington USA) and RStudio v1.1.463 (R Foundation for Statistical Computing; Vienna, Austria). Reference Team21 Descriptive statistics are reported as medians with interquartile ranges (IQR) for continuous variables. Categorical variables are reported as frequencies (%).
Results
During the study period, 3,284 patients received NTG from EMS for a variety of indications. Patients who received only SL NTG, regardless of indication, were excluded from review. Forty-four patients with APE were treated with IVB NTG during the study period. Of these, 21 (48%) were male; 23 (52%) were female. The mean age of these patients was 72 years old and most had comorbidities, as outlined in Table 1. The SpO2 data were missing for one patient due to equipment failure in the setting of profound agitation.
Table 1. Patient Demographics (N = 44)

Note: Race/Ethnicity is not documented in electronic patient care record (ePCR).
a Cardiac disease includes a history of myocardial infarction, coronary artery bypass graft, percutaneous coronary intervention, atrial fibrillation, and heart disease not otherwise specified.
b Pulmonary disease includes asthma, chronic obstructive pulmonary disease, and pulmonary fibrosis.
Of the 44 patients treated with IVB NTG for APE during the study period, 24 (55%) were treated with IVB NTG alone, never receiving NTG infusion. These patients received a median (IQR) total bolus dose of 400mcg (400-1100). Twenty patients (45%) were treated with NTG infusion following IVB NTG. The median infusion rate was 80mcg/min, which was the initial infusion rate per the protocol. No patients received NTG infusion without prior IVB NTG. For all routes of IV NTG administration, the initial median (systolic IQR) blood pressure prior to NTG was 191/113mmHg (175-216). Five minutes after IVB NTG, the median (IQR) blood pressure was 160/94mmHg (142-178), and on arrival at the emergency department (ED) was 152/90mmHg (129-172; Figure 3). Initial SpO2 prior to IVB NTG was 88% (80-92). Five minutes after IVB NTG, median SpO2 was 92% (89-96) and on arrival to the ED, it was 94% (90-97) as illustrated in Figure 4. Of the patients who received IVB NTG, 42/44 (95%) had a reduction of systolic blood pressure and 38/44 (86%) had increased SpO2 five minutes after medication administration. These observations, as well as median reductions in blood pressure and improvements in pulse oximetry, are presented in Table 2. There was one episode of hypotension following IVB NTG that resolved without intervention three minutes later. There were no other reported adverse events and no cases requiring advanced airway management in this series.

Figure 3. Blood Pressure during EMS Encounter (N = 44).
Abbreviations: ED, emergency department; EMS, Emergency Medical Services; IVB, intravenous bolus; NTG, nitroglycerin.

Figure 4. Pulse Oximetry during EMS Encounter (N = 44).
Abbreviations: ED, emergency department; EMS, Emergency Medical Services; IVB, intravenous bolus; NTG, nitroglycerin; SpO2, oxygen saturation.
Table 2. Vital Signs during EMS Encounter - Median (IQR)

Abbreviations: BPM, beats per minute; ED, emergency department; IV, intravenous; NTG, nitroglycerin.
Forty-one patients received one or more doses SL NTG prior to IVB NTG, as detailed in Table 3, while three patients were treated with IVB NTG without previous SL medication. Of those three patients, two subsequently received an IV NTG infusion. The median (IQR) dose of SL NTG prior to IVB NTG amongst all patients in this series was 800mcg (800-1600). All bolus and infused NTG was administered by IV; no intraosseous device was placed in this series. The median (IQR) scene time was 19 (8-28) minutes; median transport time was 14 minutes (4-24).
Table 3. Prehospital Interventions (N = 44)
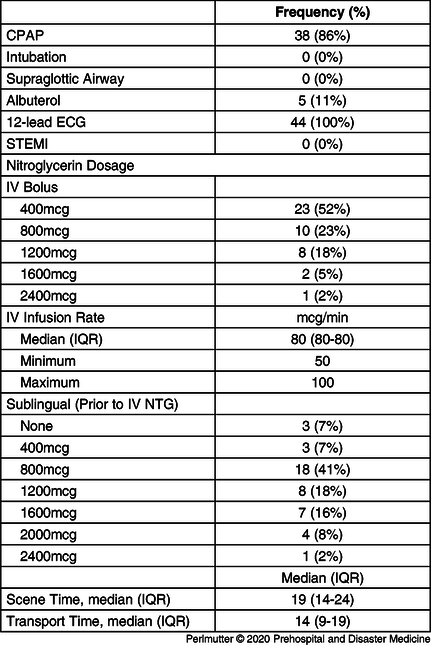
Abbreviations: CPAP, continuous positive airway pressure; ECG, electrocardiogram; IV, intravenous; NTG, nitroglycerin; STEMI, ST elevation myocardial infarction.
Of the 44 patients treated with IVB NTG, 38 were also treated with CPAP. Of the six who were not, two could not tolerate the mask. Two patients did not have CPAP applied prior to IVB NTG and improved with treatment to such a degree that the treating paramedic deferred application. The inadvertent absence of a CPAP device on an ambulance prevented its use in one case. In the last case, the ePCR did not specify the reason that CPAP was not applied.
Discussion
These results suggest that patients with APE can be treated with IVB NTG by paramedics in the field. In this series, a 20% median reduction in systolic blood pressure was observed following treatment with IV NTG. This is consistent with guidelines for immediate blood pressure reduction in the setting of APE and hypertensive crisis. Reference Mebazaa, Gheorghiade and Piña17,Reference Carey and Whelton22,Reference Nieminen, Bohm and Cowie23 Improvements in pulse oximetry were also observed, with median SpO2 rising from 88% prior to the administration of IVB NTG to 92% five minutes later and 94% at ED arrival. It is particularly notable that these results were observed using smaller bolus doses of IV NTG than have been previously reported. Most recently, Patrick, et al reported similar clinical improvements in the prehospital setting, but using IVB NTG doses of 1mg, repeated once and without IV infusion. Other work in the ED setting, such as that from Wilson, et al and Levy, et al, have reported similar improvements in hemodynamic status, as well as improvements in oxygenation and ventilation status, but did so using doses of 2mg or more.
Of 44 patients treated under this protocol, 24 (55%) were treated with IVB alone; 20 (45%) were treated with subsequent NTG infusion. There are several factors that explain this. Most encounters occurred in urban and suburban locations with short transport times; the median transport time in this series was 14 minutes. Scene times were also short, at a median of 19 minutes. In the context of treating medically complex, acutely ill patients with short on-scene and transport times, it is possible that paramedics chose to avoid the cognitive and logistical burdens of programming the infusion pump to provide continuous infusion by instead utilizing repeated boluses as outlined in the treatment algorithm. The rapid resolution of severe respiratory distress with IVB NTG may have also influenced paramedics’ decisions not to initiate a continuous infusion. This experience is consistent with the findings from Patrick, et al in the prehospital setting and Wilson, et al in the ED, who found that the symptoms of APE were substantially reduced or entirely resolved by IVB NTG alone. Reference Wilson, Kwiatkowski, Millis, Purakal, Mahajan and Levy3,Reference Patrick, Ward and Anderson20
A significant concern in the prehospital administration of IVB NTG is management of iatrogenic hypotension, angina, or syncope. There were no reported instances of angina or syncope during transport. One patient experienced an episode of transient hypotension during transport. In that case, 400mcg of IVB NTG was administered based on a blood pressure of 126/54 following SL NTG. The nadir blood pressure was 73/44 and occurred seven minutes after IVB NTG administration. Three minutes later, the patient’s blood pressure spontaneously improved to 93/54, and on ED arrival, it was 111/60 with on-going improvement in severity of dyspnea. In previous papers, a minimum systolic blood pressure of 160mmHg was a common inclusion criterion for utilization of IV NTG. It is possible that utilizing a higher systolic blood pressure minimum would result in a lower risk of hypotension. However, Wilson, et al reported an incidence of hypotension between one and two percent amongst patients receiving either IVB NTG alone or in combination with IV infusion, while Levy, et al reported one instance of hypotension that resolved with a single fluid bolus and without apparent clinical consequence. Similar findings were reported by Patrick, et al in the prehospital environment. Taken together, these findings suggest that hypotension associated with IVB NTG is uncommon and is either self-limited or readily treatable.
Limitations
Limitations of this study include its retrospective, non-randomized nature, as well as a relatively small sample size. Additionally, the data abstraction process was limited by the inability to blind the abstractors. Raters used a consensus process to resolve differences in chart abstraction in order to minimize the effect of this limitation.
The nature of the treatment protocol and study methodology is such that it is not possible to demonstrate a causal relationship between the use of IVB NTG alone or IVB NTG followed by continuous NTG infusion and the need for prehospital advanced airway management. Similarly, the on-going use of CPAP throughout the clinical encounter makes it difficult to attribute the observed improvements in clinical condition to the administration of IVB NTG alone. However, the treatment algorithm required patient reassessment following CPAP placement, and IV nitrates were only to be administered in the absence of clinical improvement following initial treatment with SL NTG and CPAP.
This study is also limited by the fact that it includes patients from a single EMS system and does not include subsequent ED data. Due to the geographical size of the EMS system, patients are transported to dozens of hospitals within several health care systems across two states, which precluded obtaining ED data.
Conclusion
In this case series, patients treated with IV NTG by paramedics for APE had reductions in blood pressure and improvements in SpO2 at five minutes following administration, which continued until arrival at the ED. There was one instance of transient hypotension that resolved without intervention en route. Subsequent investigations should explore optimal dosing, safety, and efficacy of prehospital IV NTG, and should aim to answer questions regarding its effects on overall mortality and the need for invasive ventilation and ICU utilization.
Conflicts of interest
Each author reports no conflicts of interest with regard to this work.












