Introduction
Cervical cancer, primarily caused by persistent infections with high-risk human papillomavirus (hrHPV), continues to be a major global health concern. Human papillomavirus (HPV) types 16 and 18 are recognized as the leading contributors to cervical cancer, accounting for nearly 70% of cases globally (Walboomers et al., Reference Walboomers, Jacobs, Manos, Bosch, Kummer, Shah, Snijders, Peto, Meijer and Muñoz1999; Burd, Reference Burd2003; Bouvard et al., Reference Bouvard, Baan, Straif, Grosse, Secretan, Ghissassi, Benbrahim-Tallaa, Guha, Freeman, Galichet and Cogliano2009; Rodríguez et al., Reference Walboomers, Jacobs, Manos, Bosch, Kummer, Shah, Snijders, Peto, Meijer and Muñoz2010). In China, cervical cancer is the second most common cancer among women aged 15–44 years (Chen et al., Reference Chen, Zheng, Baade, Zhang, Zeng, Bray, Jemal, Yu and He2016).
While comprehensive data specific to the prevalence of HPV in southwest China are lacking, studies from other regions, such as Shenzhen in Southern China, indicate significant HPV prevalence rates among women with cervical lesions. For example, Mai et al. (Reference Mai, Yang, Cheng, Wu and Wu2021) reported a prevalence rate of 17.83% in Shenzhen, highlighting the importance of addressing HPV infections in urban Chinese populations.
Awareness of hrHPV and its implications for cervical cancer development is crucial for effective prevention strategies. However, there is a notable gap in awareness and understanding among Chinese women, particularly regarding the benefits of HPV vaccination and regular cervical screenings (Schiller and Lowy, Reference Schiller and Lowy2012; Zhang et al., Reference Zhang, Wang, Liu, Fan, Liu, Wang and Nie2016; Chen et al., Reference Chen, Song, Ruan, Zhang, Lin, Zhang, Wu, An, Dong and Sun2018; Zhang et al., Reference Zhang, Chen, Zhou, Huang, Feng and Li2022).
This study aims to investigate socio-demographic and behavioural factors influencing awareness and knowledge of hrHPV infection and cervical diseases among women of reproductive age in China, focusing on developing targeted public health interventions. By analysing prevalent HPV subtypes and their impact on cervical health, this study will provide essential insights to enhance HPV-related health education and vaccination strategies, particularly in regions with limited data like southwest China.
Materials and methods
Study design and data collection
This retrospective study was conducted at the health examination centre of a tertiary hospital in southwest China, focusing on Han Chinese women of childbearing age. The aim was to perform an in-depth analysis of the prevalent hrHPV subtypes and the stages of cervical epithelial conditions diagnosed in these women. Data collection occurred between December 2022 and April 2023, sourcing records from the hospital’s database. These records included demographic information such as age, marital status, education level, and place of residence, along with clinical data comprising economic status and the specifically diagnosed hrHPV subtypes. The study was approved by the hospital’s Ethics Committee, ensuring adherence to ethical standards in the handling and analysis of patient data.
HPV detection and typing
All patients in the cohort underwent hrHPV testing and typing as part of their routine diagnostic process. These procedures were performed using the polymerase chain reaction technique on cervical swab specimens, enabling the identification of specific hrHPV subtypes.
Cervical intraepithelial neoplasia classification
Patients were categorized based on their diagnosed conditions of cervical intraepithelial neoplasia (CIN) as recorded in their medical files. The classifications followed include: No Intraepithelial Neoplasia or Malignant Lesion (negative for intraepithelial lesion or malignancy); Atypical Squamous Cells of Undetermined Significance (ASC-US); Low-grade Squamous Intraepithelial Lesion (LSIL) encompassing Cervical Intraepithelial Neoplasia 1 (CIN 1); and High-grade Squamous Intraepithelial Lesion (HSIL), including Cervical Intraepithelial Neoplasia 2 and 3 (CIN 2, CIN 3). This approach ensures a focused and accurate assessment of the severity of cervical epithelial abnormalities.
Assessment of knowledge on HPV and CIN
Knowledge and awareness of HPV infection and CIN were evaluated using the ‘Questionnaire on the Status and Awareness of Cervical High-risk Human Papillomavirus (HPV) Infections and Cervical Intraepithelial Neoplasia among Women of Childbearing Age’. This instrument, administered during hospital visits, was designed to probe participants’ understanding of HPV and its link to CIN, assessing risk factors, prevention, and treatment strategies. The questionnaire featured a series of multiple-choice questions and scales to measure the depth of knowledge comprehensively. Responses were analysed and scored, classifying participants into ‘High Awareness’ and ‘Low Awareness’ groups based on their answers, which facilitated a focused and binary statistical analysis of knowledge levels among the study population.
Statistical analysis
We utilized descriptive statistics to summarize the demographic and clinical characteristics of the participants. Chi-square tests were used to explore the relationships between different characteristics and HPV and cervical disease knowledge. Univariate and multivariate logistic regression models were used to identify the factors associated with higher knowledge levels. A p-value < 0.05 was considered statistically significant. All statistical analyses were carried out using R software.
Results
Demographic and socioeconomic characteristics of the study participants
Table 1 summarizes the demographic and socioeconomic profiles of 102 women of reproductive age who are at high risk for cervical HPV infection. The data delineate a diverse group predominantly comprised of unmarried women, reflecting varied educational backgrounds predominantly at or below high school level. The employment status of participants spans several categories, with a notable number engaged in casual work, administrative roles, or self-employment. Residency splits nearly evenly between urban and rural settings, indicating a broad geographical representation within the study cohort. The analysis also highlights significant variations in household income and demonstrates a general trend of low awareness about high-risk cervical HPV infection among the participants. Further details and specific percentages are available in Table 1.
Table 1. Demographic and socioeconomic characteristics of the study participants
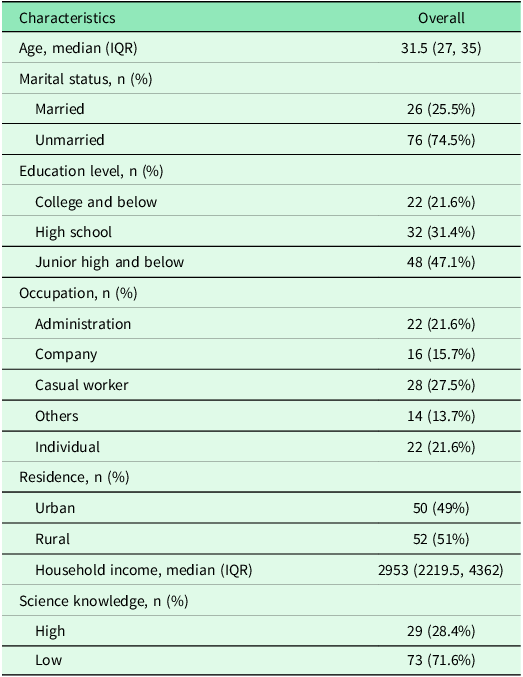
Note: Table presents the overall characteristics of the study participants. Age and Household Income are presented as medians with interquartile range (IQR). Marital Status, Education Level, Occupation, Residence, and Science Knowledge are presented as numbers with percentages. Percentages might not add up to 100% due to rounding.
Comparison of characteristics between high- and low-awareness groups for high-risk cervical HPV infection
Table 2 outlines the disparities between women with high- and low-awareness of high-risk cervical HPV infection. It highlights significant differences in demographic and socioeconomic attributes across the two groups. The analysis shows that younger women tend to have higher awareness levels, with significant differences also noted in marital status, education levels, occupation, place of residence, and household income. Specifically, women in the high-awareness group generally hold higher educational qualifications, are more likely to be married, and reside predominantly in urban areas. Moreover, they demonstrate markedly higher household income and greater knowledge of science related to HPV compared to their counterparts in the low-awareness group. These variations are statistically significant, suggesting strong correlations between these factors and awareness levels of hrHPV infections. Detailed statistical values and comparisons are provided in Table 2.
Table 2. Comparison of characteristics between high- and low-awareness groups for high-risk cervical HPV infection
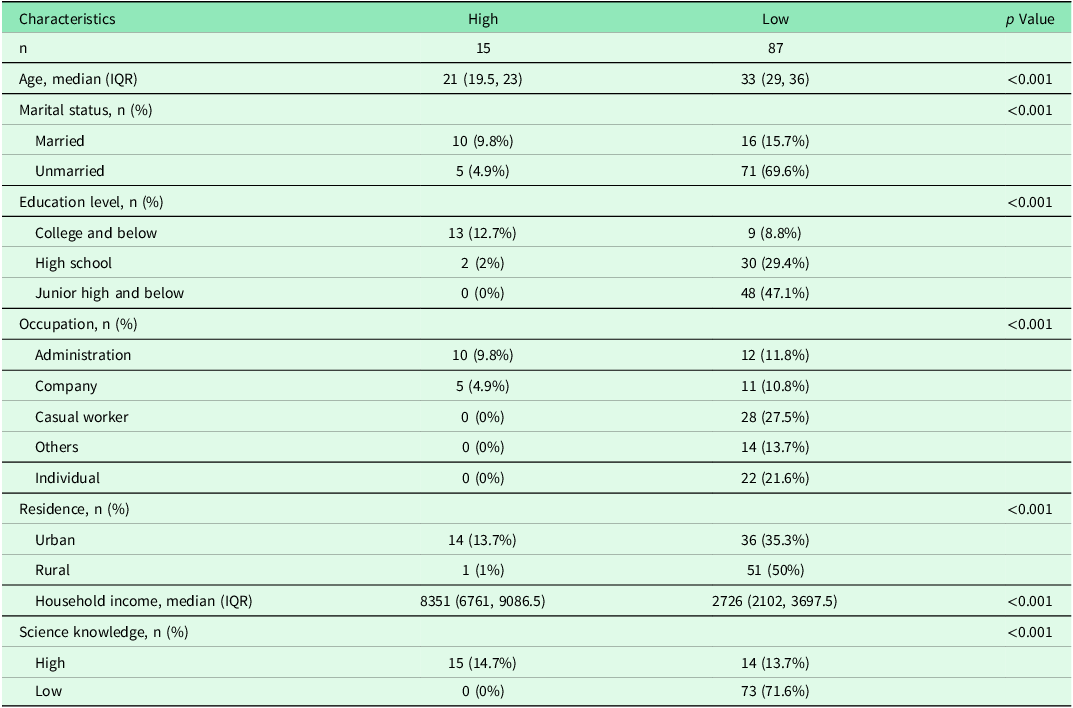
Note: The table compares the characteristics of the study participants between high awareness (n = 15) and low awareness (n = 87) groups for high-risk cervical HPV infection. Age and Household Income are presented as medians with interquartile range (IQR). Marital Status, Education Level, Occupation, Residence, and Science Knowledge are presented as numbers with percentages. Statistical analyses were conducted using Chi-square tests for categorical variables and Mann–Whitney U-tests for continuous variables to compare between the high- and low-awareness groups. p Values indicate the level of statistical significance for differences between the groups, with a value less than 0.05 considered significant. Percentages might not add up to 100% due to rounding.
Univariate and multivariate analysis of factors associated with awareness of hrHPV infection and CIN
Table 3 outlines the statistical analyses used to identify factors influencing awareness of hrHPV infection and CIN. The analyses delineate how marital status, education level, and residence significantly affect awareness levels. Notably, being unmarried, having a lower education level, and residing in rural areas are associated with lower awareness. These factors remain significant predictors in both univariate and multivariate models, highlighting their robust impact on awareness disparities among the study population. Specific odds ratios (OR) and statistical significance details are detailed in Table 3, demonstrating the strength and consistency of these associations across different analytical approaches.
Table 3. Univariate and multivariate analysis of factors associated with awareness of hrHPV infection and cervical intraepithelial neoplasia
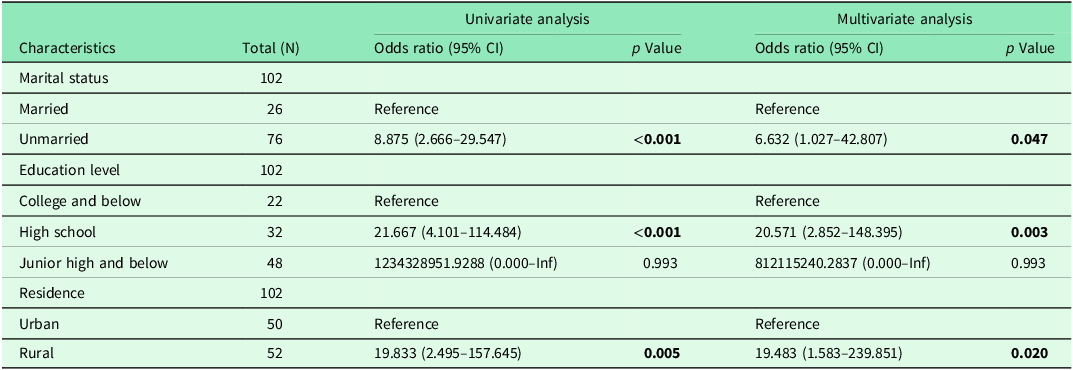
Note: N denotes the total sample size. In the univariate and multivariate analyses, ORs are provided with their respective 95% CIs. The reference category for each variable is indicated in the table. For marital status, ‘Married’ serves as the reference category; for education level, ‘College and Below’ is the reference; and for residence, ‘Urban’ is used as the reference. These categories were used as the baseline for the calculation of ORs in both univariate and multivariate logistic regression analyses. Statistical significance was assessed using logistic regression models, which allow for the adjustment of various covariates in the multivariate analysis. p Values < 0.05 are considered statistically significant. ‘Inf’ represents infinity, indicating an undetermined upper limit for the confidence interval in this data due to extreme OR values observed particularly for some categories of educational level.
Bold values indicate statistically significant results (p < 0.05).
Distribution of hrHPV infection subtypes across various categories of cervical epithelial conditions
Table 4 examines the distribution of hrHPV subtypes within different cervical epithelial conditions, categorized as No Intraepithelial Neoplasia or Malignant Lesion, Undetermined Significance of Atypical Squamous Epithelium, LSIL, and HSIL. The analysis reveals the varying prevalence of each subtype across these categories, highlighting specific patterns of distribution. For example, HPV-16 and HPV-52 emerge as significant subtypes, showing varying prevalences that suggest differing pathological impacts on cervical epithelial conditions. Detailed percentages and case numbers for each subtype and category are elaborated in the table, providing a comprehensive overview of the landscape of HPV subtype infection in relation to cervical disease severity.
Table 4. Distribution of hrHPV infection subtypes across various categories of cervical epithelial conditions
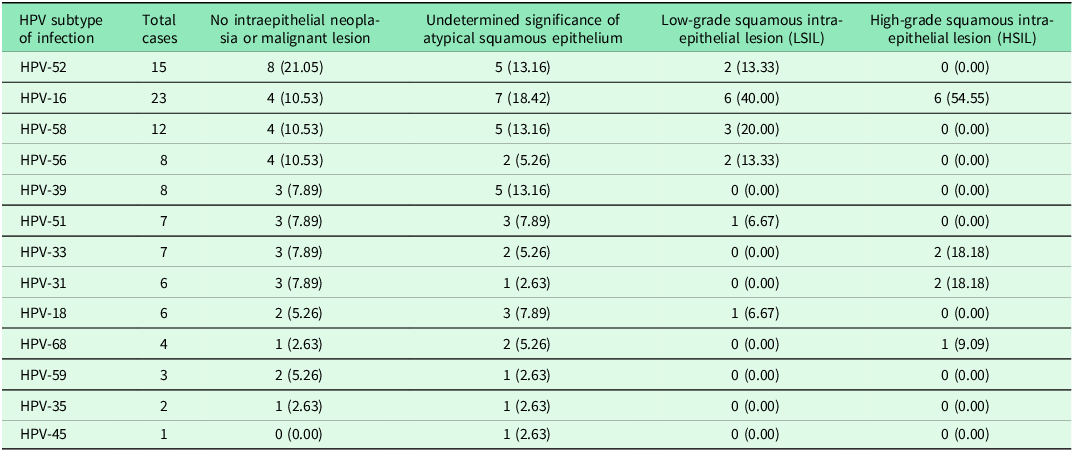
Note: This table represents the distribution of different hrHPV subtypes across various categories of cervical epithelial conditions. Number of cases and percentage (%) are indicated. Percentages are calculated with respect to the total number of cases within each category. The categories are No Intraepithelial Neoplasia or Malignant Lesion, Undetermined Significance of Atypical Squamous Epithelium, LSIL, and HSIL. The number of cases for each HPV subtype and the percentage distribution in each category are provided. Please note that the percentages are calculated as a proportion of the total number of cases for each HPV subtype.
Discussion
Our study results underscore a significant lack of awareness regarding high-risk HPV infection and cervical diseases among women of reproductive age in southwest China, echoing prior studies that report a general HPV knowledge deficiency (Zhang et al., Reference Zhang, Wang, Liu, Fan, Liu, Wang and Nie2016; George et al., Reference George, Roberts, Brennen, Deveaux and Read2020; Chido-Amajuoyi et al., Reference Chido-Amajuoyi, Jackson, Yu and Shete2021). Notably, age, marital status, education level, urban or rural residence, income, and scientific literacy emerged as significant factors influencing these awareness levels. Furthermore, the data revealed unique HPV subtype prevalence across various cervical conditions, providing valuable insights for potential preventive strategies and interventions.
Our analysis revealed a stark association between socio-demographic attributes, such as marital status and education level, and the awareness level of the participants. Both unmarried women and those who had attained a high school education or less were found to have a significantly higher likelihood of displaying low awareness, compared to their respective counterparts. This observation resonates with previous research that has similarly identified marital status and educational level as significant predictors of HPV awareness and vaccine acceptability (Adegboyega et al., Reference Adegboyega, Obielodan, Wiggins, Dignan and Williams2023; Hailu et al., Reference Hailu, Wirtu, Tesfaye and Getachew2023).
Importantly, our findings indicate age as a key determinant of HPV awareness. Younger women demonstrated higher levels of knowledge regarding HPV and associated cervical diseases. This could be attributed to the advent of newer, more comprehensive sexual health education programmes that are more accessible to the younger generation (Chesser et al., Reference Chesser, Burke, Reyes and Rohrberg2016). Moreover, younger women tend to be more familiar with digital technologies, including the internet and social media platforms, which have been increasingly employed in recent years for health education and promotion (Gough et al., Reference Gough, Hunter, Ajao, Jurek, McKeown, Hong, Barrett, Ferguson, McElwee, McCarthy and Kee2017). In contrast, older women presented a more worrying gap in awareness. This could be attributed to a lack of targeted educational initiatives for this age group, who may also have had limited exposure to sexual health education during their school years. Furthermore, older women may be less comfortable or adept at accessing digital health resources. There is also the possible effect of age-related cognitive decline, which can affect the retention and understanding of new health-related information (Tuohy et al., Reference Tuohy and Cooney2019). This highlights a pressing need for the development of tailored, age-specific HPV education interventions. Particularly for older women, these interventions could involve more traditional and familiar modes of delivery, such as print media and face-to-face health talks, and should ideally be embedded within routine health services to ensure optimal reach and impact (Kruk et al., Reference Kruk, Gage, Arsenault, Jordan, Leslie, Roder-DeWan, Adeyi, Barker, Daelmans, Doubova, English, García-Elorrio, Guanais, Gureje, Hirschhorn, Jiang, Kelley, Lemango, Liljestrand, Malata, Marchant, Matsoso, Meara, Mohanan, Ndiaye, Norheim, Reddy, Rowe, Salomon, Thapa, Twum-Danso and Pate2018).
Additionally, the location of residence was another significant determinant of HPV awareness, with women residing in rural areas exhibiting an alarmingly higher risk of low awareness compared to their urban counterparts. This finding is congruent with prior research highlighting the critical disparity in HPV awareness and cervical cancer screening between rural and urban women, attributable to the unavailability or inaccessibility of health services and educational resources in rural areas (Johnson et al., Reference Johnson, Armstrong and Joyce2018; Rosser et al., Reference Rosser, Hamisi, Njoroge and Huchko2015).
Interestingly, our study found HPV-16 to be the most prevalent subtype, especially among the cases with high-grade intraepithelial neoplasia. This finding is consistent with the global trend of HPV-16 being the leading cause of cervical cancer worldwide (Choi et al., Reference Choi, Ismail, Pappas-Gogos and Boussios2023). The identification of HPV-16 as the leading subtype underlines the necessity of a vaccination programme targeting this subtype for the efficient prevention of cervical cancer.
While our study provides important insights, it is not without limitations which must be acknowledged when interpreting our findings. Firstly, the assessment of participants’ knowledge about HPV and cervical diseases was estimated based on documented interactions and health education provided during their hospital visit. However, this estimation might not fully capture the complexity of each patient’s understanding, and their individual interpretation could add complexity to our findings (Althubaiti, Reference Althubaiti2016).
Secondly, the generalizability of our findings may be limited as our sample was solely drawn from the southwest region of China. This geographic specificity might influence the results. The levels of knowledge about HPV and cervical diseases observed in our sample might have been influenced by the specific socio-cultural environment and available healthcare resources in this region. These factors might not be representative of other regions in China, which could have different cultural attitudes towards cervical cancer and access to different healthcare resources.
Thirdly, despite our sample size being adequate, it might not have been large enough to capture the broad spectrum of socio-demographic factors influencing awareness about HPV infection and cervical diseases. A larger and more diverse sample might have provided more robust and generalizable results.
Lastly, while this study has identified certain socio-demographic factors associated with awareness, it is likely that there are other unidentified factors, such as psychological, cultural, or environmental elements, which might influence an individual’s knowledge and perceptions about HPV infection and cervical diseases. Future research might benefit from considering these aspects to provide a more comprehensive understanding of the determinants of HPV awareness. These limitations underscore the necessity of further research, incorporating a broader geographical scope and diverse methodologies, to corroborate and extend our findings.
Conclusions
Our findings provide crucial insights for the development of targeted interventions aimed at improving awareness about HPV infections and CIN in the southwest region of China. The results underscore the need for public health strategies that account for the socio-demographic characteristics of the target population, as well as the necessity of expanding vaccination programmes to cover prevalent HPV subtypes.
Data availability statement
The datasets analysed during the current study are not publicly available due to privacy but are available from the corresponding author at a reasonable request.
Acknowledgements
We would like to express our sincere gratitude to all individuals who contributed to the completion of this study. This study followed the EQUATOR network guidelines.
Author contributions
LJ H and KX N: designed this study and prepared this manuscript and are responsible and accountable for the accuracy and integrity of the work. JG and XH L: collected and analysed clinical data.
Funding statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
None.
Ethical statements
This investigation was undertaken with the sanction of the Ethics Committee of The Affiliated Hospital of Southwest Medical University (Ethics code number: KY2024184) and an exemption for informed consent was obtained from the Ethics Committee of The Affiliated Hospital of Southwest Medical University. All methods were conducted in compliance with relevant guidelines, regulations, and the Declaration of Helsinki.







