Good nutrition is necessary to maintain health during pregnancy. Nutrition during pregnancy has effects on fetal health and pregnancy duration, and longer-term effects on the offspring’s health during childhood and adulthood( Reference Harding 1 , Reference Gluckman, Hanson and Pinal 2 ).
Malnutrition, both macro- and micronutrient, is prevalent in women and children globally( Reference Black, Allen and Bhutta 3 ). In developing countries undernutrition of both macro- and micronutrients remains the major determinant of maternal and child health( Reference Black, Allen and Bhutta 3 ). In developed countries, such as New Zealand (NZ), maternal and child malnutrition is predominantly a combination of macronutrient overnutrition and micronutrient undernutrition( Reference Popkin 4 ).
At the NZ 2008/2009 National Nutrition Survey, obesity was present in 14 % of women aged 15–19 years, 25 % of those aged 20–30 years and 28 % of those aged 31–50 years( 5 , 6 ). This represented a 30 % increase in obesity prevalence among women of all ages compared with the prevalence described at the 1997 National Nutrition Survey( Reference Russell, Parnell and Wilson 7 ).
The available data on maternal micronutrient nutrition in NZ are also concerning. Fe deficiency prevalence among women aged 15 years and over increased from 3 % in 1997 to 7 % in 2008/2009( 5 ). Nineteen per cent of newborns in NZ have a 25-hydroxyvitamin D concentration <25nmol/l, a level sufficiently low to place them at risk of rickets( Reference Camargo, Ingham and Wickens 8 , Reference Gartner and Greer 9 ). As vitamin D status at birth is determined by maternal vitamin D status, it is likely that a similarly high proportion of pregnant women in NZ are also deficient in vitamin D( Reference Dawodu and Wagner 10 ).
National dietary recommendations for pregnant women in NZ were published by the Ministry of Health in 2006( 11 ). The recommended numbers of daily servings of foods from the four main food groups (vegetables and fruit; bread and cereals; milk and milk products; lean meat, meat alternatives and eggs) were based upon nutrient requirement estimates during pregnancy for Australia and NZ (Table 1)( 11 , 12 ). The dietary guidelines suggest that people try to choose low-fat dairy options and wholegrain cereals.
Table 1 New Zealand Ministry of Health recommendations for the number of servings of each of the four core food groups during pregnancy and foods that were included in the description of food group consumption( 11 )
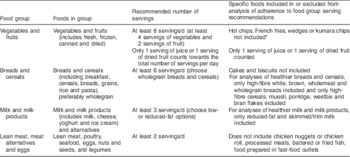
* French fries are long thinly cut slices of potato that are fried, whereas hot chips are more thickly sliced. Kumara is New Zealand’s native potato.
There is limited information about the diets of pregnant NZ women. Studies that have been reported to date have been small and non-representative of the population’s ethnic and socio-economic diversity( Reference Benny, Benny and Sin 13 – Reference Thompson, Wall and Becroft 17 ). Thus it is not possible to establish if the NZ recommendations regarding food group consumption for pregnant women are being met.
In the present study we sought to describe the overall dietary intake as compared with the recommended food and nutrition guidelines( 11 ). Our aim was to determine adherence to nutritional guidelines by pregnant women in NZ and to describe characteristics associated with adherence.
Methods
We utilised NZ’s new pre-birth cohort study, Growing Up in New Zealand. This sample of pregnant women was recruited to provide information that is broadly generalisable to all current NZ births( Reference Morton, Atatoa Carr and Grant 18 ). All pregnant women with an estimated delivery date between 25th April 2009 and 25th March 2010, residing within a geographical region defined by three adjacent area health board regions (Auckland, Counties – Manukau and Waikato), where approximately one-third of the country’s population resides, were eligible to participate( Reference Morton, Atatoa Carr and Grant 18 ). There were no other inclusion or exclusion criteria( Reference Morton, Atatoa Carr and Grant 18 ). Ethical approval was obtained from the Ministry of Health Ethics Committee. Written informed consent was obtained from all participating women.
A total of 6822 women consented and completed the antenatal interview. Enrolled women were comparable to the most recent NZ national birth statistics in relation to maternal age, ethnicity, parity and indicators of socio-economic position( Reference Morton, Ramke and Kinloch 19 ). The Growing Up in New Zealand cohort comprises 6846 children at birth( Reference Morton, Atatoa Carr and Grant 18 ).
A face-to-face computer-assisted interview was completed with each enrolled woman. Dietary data were gathered using a semi-quantitative, forty-four-item FFQ administered during the interview. In order to minimise recall bias only women interviewed before the child’s birth were included in this study of dietary patterns (n 5664).
The FFQ collected data that allowed description of the frequency of consumption of foods in the four main food groups (Table 1). Consistent with the national dietary recommendations, only one serving of juice or one serving of dried fruits could count towards the total number of servings of fruit per day( 11 ). The guidelines state that wholegrain cereals and low/reduced-fat milk products should be chosen. Therefore we described both the total number of daily servings of breads and cereals and also the number of daily servings of healthier breads and cereals (high-fibre white, brown bread, wholemeal and wholegrain bread; high-fibre cereals, muesli, porridge, weetbix and bran flakes). Similarly we reported both the total number of daily servings of milk and milk products and of healthier milk and milk products (reduced-fat or skimmed/trim milk).
We asked the pregnant women to describe the frequency of their intake of foods likely to be high in fats, sugars and/or salt (see online supplementary material, Supplementary Table 1)( 11 ). The recommendations for consumption of these foods during pregnancy are identical to the Ministry of Health guideline statements for healthy adults( 11 , 20 ). We also asked open-ended questions about foods and drinks the women deliberately avoided during pregnancy to assess adherence to recommendations that seek to reduce the risk of listeriosis (Supplementary Table 1)( 11 ).
Question formatting was consistent with that used in the dietary history questionnaire component of the 2008/2009 NZ Adult National Nutrition Survey( 21 ). Show cards with pictures of standard serving sizes were used to assist description of portion size consumed. Allowing portion size to be described has been shown to increase the agreement between FFQ and reference dietary measures( Reference Cade, Thompson and Burley 22 ). Frequency categories were used in increasing order: not at all, less than once per month and number of times per month, week or day.
Interviewers received comprehensive training in the FFQ administration. Content and delivery of the FFQ (as part of the entire antenatal interview) were refined during piloting with an ethnically diverse group of 200 pregnant women enrolled approximately 6 months earlier and from the same geographical area as the main cohort( Reference Morton, Atatoa Carr and Bandara 23 ).
For the analyses presented here, ethnicity was defined as the mother’s self-prioritised ethnicity. The self-prioritised ethnicities were gathered from participants at the most detailed level possible and were then coded into six Level 1 categories following Statistics New Zealandʼs coding criteria: (i) European; (ii) Māori; (iii) Pacific Peoples; (iv) Asian; (v) Middle Eastern; Latin American and African; and (vi) other( 24 ). Parental socio-economic status, educational qualifications and household income items were based on measures taken from Statistics New Zealand’s 2006 national census and 2008 General Social Survey( 25 , 26 ). The measures are among those included in the Core Questions module, a set of questions designed to allow comparability across social surveys( 27 ).
Area-level socio-economic deprivation was measured using the NZ Index of Deprivation (NZDep06), grouped as quintiles( Reference Salmond, Crampton and Atkinson 28 , Reference White, Gunston and Salmond 29 ). NZDep06 is derived from 2006 census data on nine socio-economic characteristics (means-tested benefits, employment, household income, access to a telephone, access to a car, single-parent family, qualifications, home ownership, household overcrowding) at aggregations of approximately 100 people and assigned to individual observations based on geo-coded address data.
Descriptive statistics were used to investigate adherence to the recommendations on frequency of consumption of: (i) vegetables and fruit; (ii) breads and cereals; (iii) milk and milk products; and (iv) lean meat, meat alternatives (nuts and seeds, and legumes) and eggs. In the analyses we did not include processed foods such as cakes and biscuits, fruit juice, processed meats or hot chips.
Associations of maternal ethnicity, age at pregnancy, education and area-level socio-economic deprivation with adherence to food group recommendations were described. Proportions were compared using the χ 2 test and, for ordinal-level variables, the χ 2 test for trend. Logistic regression models were then developed to examine the likelihood of women adhering to the nutritional recommendations during pregnancy. Each recommendation was modelled separately with maternal ethnicity, age and education, with parity and pregnancy planning, and with household income and socio-economic deprivation. The reference group for household income was $NZ 70 001–100 000 because the median household gross income in NZ in 2010 was $NZ 75 700( Reference Perry 30 ). All analyses were conducted using the SAS statistical software package version 9·2. A two-sided P value of <0·05 was considered statistically significant.
Results
Of the 5664 respondents, information on the expected due date was available for 5584. For these 5584 respondents the mean gestational age at the time of interview was 31 (sd 4) weeks. Most (n 4365, 78 %) were interviewed during the third trimester (weeks 28 to birth). Cohort births occurred from March 2009 to May 2010.
The self-prioritised ethnicity breakdown was 56 % European, 13 % Māori, 13 % Pacific, 14 % Asian and 4 % other ethnicities. The median (range) age was 31 (15–47) years, 70 % had tertiary education, 58 % had older children, 62 % had a planned pregnancy and 26 % lived in households within the most deprived areas (deciles 9 and 10).
Food group consumption during pregnancy
Consumption of food groups during pregnancy is shown in Table 2. The number of daily servings of vegetables consumed during pregnancy was evenly distributed across 1, 2, 3 or ≥4 servings, with a smaller proportion (7 %) having <1 serving of vegetables/d. The number of daily servings of fruit showed similarly wide variance but with a larger proportion (43 %) consuming ≥4 servings/d. Almost all (99 %) of the pregnant women consumed breads and cereals on a daily basis, with 68 % of women consuming healthier breads and cereals on a daily basis. Milk and milk products were also consumed on a daily basis by almost all (96 %) and healthier milk and milk products on a daily basis by 42 %. Most (79 %) of the women consumed servings of lean meat, meat alternatives or eggs no more frequently than once daily.
Table 2 Number of servings consumed per day (during the past month) by food group among pregnant women (n 5664) enrolled in the Growing Up in New Zealand birth cohort study, 2009–2010
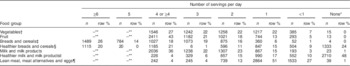
* None=not in the past 4 weeks.
† Does not include hot chips, French fries, wedges or kumara chips.
‡ Does not include cakes and biscuits.
§ Breads: high-fibre white, brown bread, wholemeal, wholegrain; cereals: high-fibre cereals, muesli, porridge, weetbix, bran flakes.
|| Milk: reduced-fat or skimmed/trim milk.
¶ Does not include chicken nuggets or chicken roll, processed meats, battered or fried fish, food prepared in fast-food outlets.
** Most frequent category asked was 4+ per day.
Consumption of foods likely to be high in fats, sugars and/or salt
Table 3 shows consumption of foods likely to be high in fats, sugars and/or salt. Fried potatoes including kumara, NZ’s native potato, were consumed at least weekly by 56 % of the pregnant women; battered or fried fish or seafood by 15 %; processed meats by 46 %; and takeaways by 38 %. Soft drinks or energy drinks were consumed at least weekly by 40 % and at least daily by 10 %. Seventy-six per cent of the women consumed confectionery, lollies, sweets and chocolate at least weekly and 20 % consumed these daily. Snacks such as crisps and nuts were consumed at least weekly by 64 % and daily by 10 %.
Table 3 Consumption of foods and beverages (during the past month) likely to be high in fats, sugars and/or salt among pregnant women (n 5664) enrolled in the Growing Up in New Zealand birth cohort study, 2009–2010
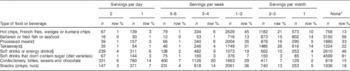
* None=not in the past 4 weeks.
† Processed meats includes ham, bacon, pastrami, salami, luncheon meat and canned corn beef.
‡ Takeaways includes foods from fast-food outlets
§ Soft drinks include carbonated beverages and energy drinks.
Avoidance of foods
As shown in Table 4, specific food or drinks were deliberately avoided by 87 % of the pregnant women. These included foods that the Ministry of Health recommended that pregnant women avoid.
Table 4 Foods that were avoided during pregnancy among pregnant women (n 5664) enrolled in the Growing Up in New Zealand birth cohort study, 2009–2010

Adherence to recommendations for main food groups
The recommended number of daily servings of vegetables and fruit (≥6) were met by 25 % of the pregnant women, with 27 % meeting the recommendations for vegetables (≥4 servings/d) and 82 % for fruit (≥2 servings/d). The recommended number of daily servings of bread and cereals (≥6) were consumed by 26 % of the women, of milk and milk products (≥3 servings/d) by 58 % and of lean meat, meat alternatives or eggs (≥2 servings/d) by 21 %. Overall, 24 % (n 1347) of the pregnant women did not meet any of the Ministry of Health recommendations, while 38 % (n 2144) met one, 25 % (n 1437) met two, 10 % (n 577) met three and 3 % (n 159) met all four food group serving recommendations.
Figure 1 shows the percentage of pregnant women meeting the food group serving recommendations by ethnicity, age, education and socio-economic deprivation. In unadjusted analyses, adherence to the recommendations varied by all four of these variables. Adherence varied by ethnicity for breads/cereals (P<0·001), milk/milk products (P<0·001) and meat/eggs groups (P<0·001; Fig. 1(a)). Adherence varied by age for the vegetables/fruit (P<0·001), breads/cereals (P<0·001) and meat/eggs groups (P<0·001; Fig. 1(b)). Adherence varied with maternal education for all four food groups (P<0·001 for vegetables/fruit, breads/cereals and meat/eggs groups; P=0·005 for milk/milk products; Fig. 1(c)). Adherence varied with area-level deprivation for vegetables/fruit (P=0·009), breads/cereals (P<0·001) and meat/eggs groups (P<0·001).
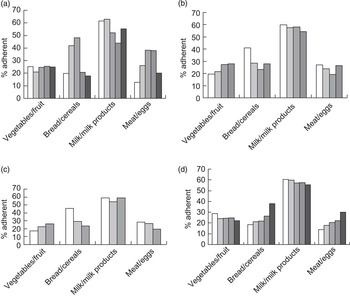
Fig. 1 Adherence to the New Zealand Ministry of Health nutritional guidelines in pregnancy by maternal demographics among pregnant women (n 5664) enrolled in the Growing Up in New Zealand birth cohort study, 2009–2010. (a) Adherence by maternal ethnic group (![]() , European;
, European; ![]() , Māori;
, Māori; ![]() , Pacific Peoples;
, Pacific Peoples; ![]() , Asian;
, Asian; ![]() , other). Ethnic group associations within food groups as follows. Vegetables/fruit group: none (P trend=0·18); breads/cereals group: in comparison with European women, a larger proportion of Māori (42 % v. 20 %) and Pacific (48 % v. 20 %) women were adherent (P trend<0·001); milk/milk products group: adherence >50 % for all ethnic groups (European 62 %, Māori 63 %, Pacific 52 %, other 55 %) except Asian (44 %; P trend<0·001); meat/eggs group: in comparison with European women, a larger proportion of Pacific (38 % v. 13 %) and Asian (38 % v. 13 %) women were adherent (P trend<0·001). (b) Adherence by maternal age group (
, other). Ethnic group associations within food groups as follows. Vegetables/fruit group: none (P trend=0·18); breads/cereals group: in comparison with European women, a larger proportion of Māori (42 % v. 20 %) and Pacific (48 % v. 20 %) women were adherent (P trend<0·001); milk/milk products group: adherence >50 % for all ethnic groups (European 62 %, Māori 63 %, Pacific 52 %, other 55 %) except Asian (44 %; P trend<0·001); meat/eggs group: in comparison with European women, a larger proportion of Pacific (38 % v. 13 %) and Asian (38 % v. 13 %) women were adherent (P trend<0·001). (b) Adherence by maternal age group (![]() , <20 years;
, <20 years; ![]() , 20–29 years;
, 20–29 years; ![]() , 30–39 years;
, 30–39 years; ![]() , 40+ years). Age group associations within food groups as follows. Vegetables/fruit group: adherence increased with increasing age (P trend<0·001); breads/cereals group: adherence highest in those <20 years old (41 %) and lowest in those aged 30–39 years (23 %; P trend<0·001); milk/milk products group: none (P trend=0·66); meat/eggs group: adherence lower in those aged 30–39 years (19 %) than in younger (<20 years 27 %, 20–29 years 24%) or older (40+ years 27 %) age groups (P trend<0·001). (c) Adherence by maternal education (
, 40+ years). Age group associations within food groups as follows. Vegetables/fruit group: adherence increased with increasing age (P trend<0·001); breads/cereals group: adherence highest in those <20 years old (41 %) and lowest in those aged 30–39 years (23 %; P trend<0·001); milk/milk products group: none (P trend=0·66); meat/eggs group: adherence lower in those aged 30–39 years (19 %) than in younger (<20 years 27 %, 20–29 years 24%) or older (40+ years 27 %) age groups (P trend<0·001). (c) Adherence by maternal education (![]() , primary;
, primary; ![]() , secondary;
, secondary; ![]() , tertiary). Educational group associations within food groups as follows. Vegetables/fruit group: adherence increased with increasing education (P trend<0·001); breads/cereals group: adherence decreased with increasing education (P trend<0·001); milk/milk products group: for all levels of maternal education recommendations were met by >50 % of the pregnant women (P trend=0·005); meat/eggs group: adherence decreased with increasing education (P trend<0·001). (d) Adherence by area-level socio-economic deprivation, measured using the NZ Index of Deprivation (NZDep06), grouped as quintiles(
Reference Salmond, Crampton and Atkinson
28
,
Reference White, Gunston and Salmond
29
) (
, tertiary). Educational group associations within food groups as follows. Vegetables/fruit group: adherence increased with increasing education (P trend<0·001); breads/cereals group: adherence decreased with increasing education (P trend<0·001); milk/milk products group: for all levels of maternal education recommendations were met by >50 % of the pregnant women (P trend=0·005); meat/eggs group: adherence decreased with increasing education (P trend<0·001). (d) Adherence by area-level socio-economic deprivation, measured using the NZ Index of Deprivation (NZDep06), grouped as quintiles(
Reference Salmond, Crampton and Atkinson
28
,
Reference White, Gunston and Salmond
29
) (![]() , Dep 1–2 (least deprived);
, Dep 1–2 (least deprived); ![]() , Dep 3–4;
, Dep 3–4; ![]() , Dep 5–6;
, Dep 5–6; ![]() , Dep 7–8;
, Dep 7–8; ![]() , Dep 9–10 (most deprived)). Socio-economic deprivation associations within food groups as follows. Vegetables/fruit group: adherence decreased with increasing household deprivation (P trend=0·009); breads/cereals group: adherence increased with increasing household deprivation (P trend<0·001); milk/milk products group: none (P trend=0·11); meat/eggs group: adherence increased with increasing household deprivation (P trend<0·001). P trend determined using the χ
2 test for trend
, Dep 9–10 (most deprived)). Socio-economic deprivation associations within food groups as follows. Vegetables/fruit group: adherence decreased with increasing household deprivation (P trend=0·009); breads/cereals group: adherence increased with increasing household deprivation (P trend<0·001); milk/milk products group: none (P trend=0·11); meat/eggs group: adherence increased with increasing household deprivation (P trend<0·001). P trend determined using the χ
2 test for trend
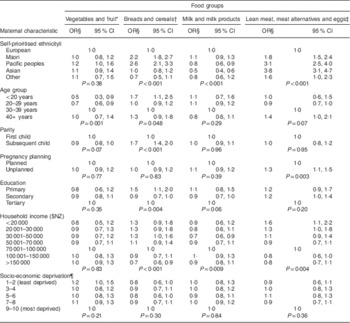
Multivariate analysis of adherence for the four main food groups
Table 5 presents the results of multivariate analysis of adherence for the four main food groups by maternal characteristics.
Table 5 Adherence to the New Zealand Ministry of Health nutritional guidelines in pregnancy by maternal characteristics among pregnant women (n 5664) enrolled in the Growing Up in New Zealand birth cohort study, 2009–2010
* Does not include hot chips, French fries, wedges or kumara chips.
† Does not include cakes and biscuits.
‡ Does not include chicken nuggets or chicken roll, processed meats, battered or fried fish, food prepared in fast-food outlets.
§ Odds ratios are adjusted for all the other variables in the table.
|| External prioritisation was used for the approximately 4 % of mothers with more than one ethnicity.
¶ Area-level socio-economic deprivation was measured using the NZ Index of Deprivation (NZDep06), grouped as quintiles( Reference Salmond, Crampton and Atkinson 28 , Reference White, Gunston and Salmond 29 ).
Vegetables and fruit
Maternal age was the only variable independently associated with adherence to the recommendations for the vegetables/fruit group. In comparison with pregnant women aged 30–39 years, women were less likely to meet the recommendations if they were less than 20 years old (OR=0·5) or 20–29 years old (OR=0·7).
Breads and cereals
Adherence to recommendations for the breads/cereals group varied with maternal ethnicity, age, parity and education and with household income. Māori women (OR=2·2) and Pacific women (OR=2·6) were more likely than European women to be adherent. Women less than 20 years old (OR=1·7) were more likely to meet the recommendations than women aged 30–39 years. Women with older children (OR=1·7) were more likely to meet the recommendations than women for whom this was their first child. Women with only primary education (OR=1·5) were more likely to meet the recommendations than women with tertiary education. Adherence to the recommendations varied inversely with household income. In comparison with households with an annual income of $NZ 70 001–100 000, pregnant women living in households with an annual income greater than $NZ 150 000 were less likely (OR=0·7) and those living in a household with an annual income of $NZ 30 000–50 000 (OR=1·3) were more likely to meet the recommendations.
When the multiple variable analyses were limited to healthier breads and cereals, adherence to recommendations varied with maternal ethnicity, age and pregnancy planning (see online supplementary material, Supplementary Table 2). Associations with parity, maternal education and household income were no longer apparent. Māori women (OR=1·3) were more likely and women of Asian (OR=0·4) and other (OR=0·5) ethnic groups were less likely than European women to be adherent. Women aged 20–29 years were less likely (OR=0·8) and women 40 years and older were more likely (OR=1·4) to meet recommendations than women aged 30–39 years. Women whose pregnancy was unplanned were less likely (OR=0·8) to meet recommendations.
Milk and milk products
Recommendation adherence for the milk/milk products group varied with ethnicity and household income. Pregnant Pacific (OR=0·8) and Asian (OR=0·5) women were less likely than European women to meet the recommendations for the milk/milk products group. In comparison with households with an annual income of $NZ 70 001–100 000, women living in households with an annual income of $NZ 30 001–50 000 were less likely to meet the recommendations (OR=0·7).
When the multiple variable analyses were limited to healthier milks and milk products, adherence to recommendations still varied with maternal ethnicity and household income and also with parity. Pregnant Asian (OR=0·3) women were less likely than European women to meet the recommendations for the milk/milk products group. In comparison with households with an annual income of $NZ 70 001–100 000, pregnant women living in households with an annual income less than $NZ 20 000 were less likely to meet the recommendations (OR=0·4). Women with older children (OR=0·8) were less likely to meet recommendations.
Lean meat, meat alternatives and eggs
Adherence varied with ethnicity, pregnancy planning and household income. In comparison with pregnant European women, pregnant Māori (OR=1·8), Pacific (OR=3·1) and Asian (OR=3·8) women and pregnant women of other ethnic groups (OR 1·6) were more likely to meet the recommendations. Women whose pregnancy was unplanned were more likely to meet the recommendations (OR=1·3) than those for whom the pregnancy was planned. Women living in the two lowest household income groups (<$NZ 20 001, OR=1·6; $NZ 20 001–30 000, OR=1·3) were more likely to be adherent to the meat/eggs recommendations compared with pregnant women in the median income group ($NZ 70 001–100 000).
When season of enrolment was included in the multiple variable analyses, the significant associations of maternal characteristics with nutritional guideline adherence shown in Table 5 were unchanged. Season of enrolment was not independently associated with adherence for vegetables and fruit (P=0·16), breads and cereals (P=0·45) or lean meat, meat alternatives and eggs (P=0·75) but was for milk and milk products (P=0·003). In comparison with those enrolled in summer, enrolment in autumn was associated with increased odds of adherence with the recommended number of servings of milk and milk products (OR=1·23; 95 % CI 1·01, 1·51).
Discussion
In this nationally representative sample of pregnant NZ women, the average number of daily servings of vegetables and fruit, and breads and cereals varied widely. Less variability was present in daily servings of milk and milk products and of meat, meat alternatives and eggs.
For three of the four main food groups (vegetables/fruit, breads/cereals and meat/eggs), less than 30 % of the women met the Ministry of Health recommendations. The milk/milk products group was the only food group for which more than half (58 %) of the women met recommendations; however, for only 10 % of women was this recommendation met by the consumption of healthier milk and milk products. Within the vegetables/fruit group a larger proportion of the women met the recommendations for fruit (82 %) than they did for vegetables (27 %). One in four (24 %) of the women met none of the four food group recommendations and only 3 % met the recommendations for all four food groups.
The pregnant women consumed foods likely to be high in fats, sugars and/or salt at a frequency that exceeds the admittedly imprecise recommendations that these only be consumed ‘occasionally’. Most women demonstrated awareness of the recommendations to avoid certain foods during pregnancy (e.g. raw seafood) presumably because they were aware of the potential for such foods to compromise their health and the health of their fetus. However, less than half of the women avoided each individual risky food group. As has been shown in other countries, awareness of listeriosis and the foods in which it can be found is relatively poor in NZ( Reference Ogunmodede, Jones and Scheftel 31 ). A survey of pregnant women conducted within the region from which our cohort was recruited showed that only one in four (26 %) women were able to correctly identify all of the common foods that should be avoided( Reference Rungan and Badkar 32 ).
The current study is the largest one of dietary intake in pregnancy in NZ. The size of our cohort was determined by the need to have adequate explanatory power for analyses to be performed within the main ethnic and socio-economic population subgroups in NZ( Reference Morton, Atatoa Carr and Grant 18 ). Thus in multiple variable analyses we were able to demonstrate statistical significance for an odds ratio as small as 1·3, i.e. a 30 % difference between population subgroups in adherence to a dietary recommendation. Differences of this size are of both clinical and public health significance( Reference Nurminen 33 ).
The only other surveys that have population-specific dietary data are the National Nutrition Surveys. The most recent of these was a voluntary cross-sectional survey of 4721 New Zealanders aged 15 years and over( 5 ). Comparable questions were used to report intakes of vegetables and fruit. Fifty-six per cent of women aged 19–30 years consumed three or more servings of vegetables daily, compared with 49 % in the present study, and 61 % consumed two or more servings of fruit daily, compared with 81 % in the present study( 5 ). Thus, we believe that the poor adherence with dietary recommendations during pregnancy was likely to be present before these women became pregnant.
Assessment of diet was only one component of this antenatal interview which gathered information on the broad range of factors of relevance to the subsequent health of the child cohort. Hence it was necessary to limit the size of our FFQ to forty-four items. For an analysis of adherence to dietary recommendations, we believe this FFQ was sufficiently detailed. Maternal dietary pattern assessment using a twenty-item FFQ was recently shown to correlate highly (r=0·94) with the original 100-item FFQ used in the Southampton Women’s Survey( Reference Crozier, Inskip and Barker 34 ).
That pregnant women in NZ appear no more adherent to dietary recommendations than non-pregnant women is consistent with recent data from Australia which show that neither being pregnant nor planning to become pregnant was predictive of diet quality( Reference Hure, Young and Smith 35 ). Data from the Southampton Women’s Survey, which established a pre-birth cohort, also showed that women’s diets during the first and third trimesters of pregnancy showed little change in comparison with their pre-pregnancy diet( Reference Crozier, Robinson and Godfrey 36 ).
The low level of adherence with dietary recommendations during pregnancy we observed is also consistent with recent data from Australia and Canada. In a sample enrolled at mid-pregnancy in Queensland, 9 % of women met recommendations for the number of servings of vegetables and fruit( Reference Wilkinson, Miller and Watson 37 ). In a pregnancy cohort from Ontario, 15 % did not meet the recommendations for minimum number of servings of any of four food groups and 4 % met the minimum recommendations for all four food groups( Reference Fowler, Evers and Campbell 38 ).
Our findings are consistent with the data reported previously in NZ on diet and nutrient intakes during pregnancy. While differences in the dietary measurement methods used prevent direct comparisons, intakes of several micronutrients (folate, vitamin B6, Fe, thiamin and Zn) were potentially inadequate in studies of small samples of pregnant women from Wellington (n 115) and Dunedin (n 95) in the 1980s( Reference Benny, Benny and Sin 13 , Reference McKenzie-Parnell, Wilson and Parnell 14 ). Low intakes of vitamin D, folate, Fe and Se were described in a study of 196 pregnant mostly European women from a semi-urban and rural region of NZ in the 1990s( Reference Benny, Benny and Sin 13 ). Low intakes during pregnancy of folate, riboflavin, vitamin A equivalents, Ca, Fe, Zn and Se were described from a study published in 1999 of an ethnically, socio-economically and geographically diverse sample of 504 pregnant women( Reference Watson and McDonald 16 ).
In the mid-1990s, in a sample of 870 NZ mothers of infants of appropriate size for gestational age, the proportion of women in the last month of pregnancy consuming servings of each of the main food groups that approximate current recommendations was: vegetables ≥3 servings/d, 12 %; fruit ≥2 servings/d, 53 %; dairy products >3 servings/d, 50 %; and meat ≥1 serving/d, 28 %( Reference Mitchell, Robinson and Clark 15 ). These frequencies are similar to our findings from 2009–2010.
Of the demographic variables examined, adherence with guidelines had the strongest associations with ethnicity. Larger proportions of women of non-European ethnic groups met the minimal recommendations for number of servings of the breads/cereals and meat/eggs groups. However, this greater adherence is not matched by better nutritional status. The prevalence of obesity among Māori (48 %) and Pacific (60 %) women aged 15 years or older is at least twice that described in women of NZ European and other ethnic groups (24 %). Vitamin D status at birth, which is a good marker of vitamin D status during pregnancy, is poorer in non-European ethnic groups in NZ( Reference Camargo, Ingham and Wickens 8 ).
When the associations with guideline adherence were limited to healthier choices of breads and cereals and of milk and milk products, ethnicity remained the demographic variable with the strongest associations. Of note, Māori women were more likely (OR=1·3) to adhere to recommendations for healthier breads and cereals and neither Māori nor Pacific women were less likely than European women to adhere to recommendations for healthier milks.
Dietary patterns are one of the key areas of lifestyle change that occur with adoption of a Western lifestyle( Reference Satia-Abouta, Patterson and Neuhouser 39 ). For example, comparisons of diet between US-born and Korean-born women living in the USA show that the US-born Korean women consumed more whole grains, red meat and nuts and had higher intakes of total fat and fat as a percentage of energy than Korean-born women( Reference Park, Murphy and Sharma 40 ). Comparisons of nutritional status show that such dietary changes were likely to be having an adverse effect on health, with the proportion of overweight or obese being more than three times greater for the US-born compared with the Korean-born women( Reference Park, Murphy and Sharma 40 ).
A significant proportion of NZ’s population are recent immigrants. For example, 36 % of the pregnant women enrolled into the Growing Up in New Zealand cohort were born overseas( Reference Morton, Atatoa Carr and Bandara 23 ). That such a diverse cohort has been enrolled provides new opportunities for nutrition policy development to benefit those population subgroups at greatest risk of nutrition-related health issues.
In our cohort, socio-economic disadvantage did not explain variations in adherence. Adherence with dietary recommendation did not vary with household deprivation and associations that were present with household income and maternal education did not indicate that adherence decreased as household income or maternal education decreased. In a recent Canadian pregnancy cohort the only maternal demographic characteristic predictive of adherence to food group recommendations was parity( Reference Fowler, Evers and Campbell 38 ).
In contrast to this lack of association with diet as described by food groups, dietary quality has been shown to be associated with maternal education and deprivation in studies performed in the UK and the USA( Reference Northstone, Emmett and Rogers 41 , Reference Rifas-Shiman, Rich-Edwards and Kleinman 42 ). The limited associations of deprivation, education and household income with food group recommendations in our study could be due to food group descriptions providing limited information on diet quality. For example, meeting or exceeding the recommendations for number of servings of the breads/cereals, milk/milk products and meat/eggs groups could be achieved with a diet that is low in fibre, high in fat and a poor source of many micronutrients.
Our choice of the FFQ to estimate intake comes with potential limitations. Most importantly, FFQ can be inaccurate due to the necessity of relying on a ‘standard portion size’; methods using weighed intakes provide more accurate dietary assessments( Reference Emmett 43 ). FFQ can also be problematic in that some foods may be missed, for example vegetables used in composite dishes such as casseroles or sauces. However, comparative studies have indicated that misclassification of nutrient intakes from use of an FFQ is within acceptable boundaries( Reference Emmett 43 ). The ease of administering an FFQ means that in many research contexts, especially those with a large sample size, an FFQ is the only practical alternative( Reference Emmett 43 ).
The relative simplicity of FFQ facilitates their use for comparisons between studies and for measurement of change in dietary practices over time. The European Diet in Pregnancy Project recognises the usefulness of the FFQ for reporting on dietary intakes in large cohort studies( Reference Mendez and Kogevinas 44 ). That project has developed a protocol for the standardisation of food group intake data from existing studies in pregnant women across Europe. Its database includes data from more than 200 000 women. The protocol uses standardised FFQ and the food group descriptions are comparable to those in the present study. Thus, the less precise measurement of individual dietary consumption that an FFQ provides needs to be balanced against the greater potential for external comparability.
Our description of adherence with food group recommendations was predominantly during the third trimester of pregnancy and none of the women were interviewed during the first trimester. In the UK, nutrient intakes were shown to be similar in the first and third trimesters, and in the USA food and energy-adjusted nutrient intakes from foods alone were not appreciably different in the first compared with the second trimester( Reference Langley-Evans and Langley-Evans 45 , Reference Rifas-Shiman, Rich-Edwards and Willett 46 ). Our data on adherence are therefore likely to be an adequate representation of dietary patterns throughout pregnancy.
Pregnancy is widely accepted as an optimal time for altering various aspects of women’s lifestyles towards more health-promoting behaviours( Reference Harding 1 , Reference Cox and Phelan 47 ). That 87 % of the pregnant women in our study avoided certain foods or drinks at some point during their pregnancy implies that they were willing to make changes to their diet in order to improve their pregnancy health and the subsequent health of their infant. The relative lack of adherence to food group consumption and the relatively high frequency of consumption of foods likely to be high in fats, sugars and/or salt are consistent with women lacking knowledge about the specific health benefits of a more nutritious diet during pregnancy. For example, while women appear to be aware of the potential maternal complications of being overweight and obese during pregnancy, many have more limited awareness of the neonatal complications( Reference Sui, Turnbull and Dodd 48 ).
Our findings suggest that more support is needed to assist pregnant NZ women in adhering to recommended dietary patterns during pregnancy. The large variability in adherence to these guidelines between ethnic groups indicates the need for ethnicity-specific interventions that are consistent with the dietary practices and beliefs of these different groups.
Acknowledgements
Acknowledgments: The authors thank the children and the families who are part of the Growing Up in New Zealand study. They also thank all members of the Growing Up in New Zealand team, including the research and operations teams, as well as the Kaitiaki and Scientific Advisory Groups. Financial support: The authors acknowledge the key role of the Ministry of Social Development in identifying the need for a longitudinal study that reflects the diversity of today’s New Zealand and for its ongoing support. Other agencies, as well as The University of Auckland, have contributed to the cost of the study to date. These are: the Ministry of Health, the New Zealand Police, the Ministry of Justice, the Families Commission, the Children’s Commission, the Department of Labour, the Ministry of Education, Housing New Zealand and Sport and Recreation New Zealand. The funders have had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: S.M.B.M. led the design, development and completion of all aspects of Growing Up in New Zealand. S.M.B.M., C.C.G. and C.R.W. designed the study reported in this manuscript. S.M.B.M., C.C.G., C.R.W., P.E.A.-C. and V.I. developed the instruments used to collect the data reported in this manuscript. D.K.B. analysed the data. S.M.B.M., C.C.G., C.R.W., P.E.A.-C., H.M.I. and C.A.C. interpreted the data. C.C.G., C.R.W. and J.M.S. compiled a first draft of the manuscript that was revised by all of the authors. C.C.G. completed the final draft of the manuscript. All authors have given their final approval for the submitted manuscript. Ethics of human subject participation: Ethical approval was obtained from the Ministry of Health Northern Y Regional Ethics Committee.








