Smoking is known to be associated with low bone mass and increased risk of fracture, one of the plausible mechanisms being depressed 25-hydroxyvitamin D (25(OH)D) levels among smokers.
Vitamin D is also a versatile modulator of the immune system with anti-inflammatory and antioxidant properties(Reference Baeke, Takiishi and Korf1). Pregnant women in Finland were studied from 1997 to 2004, and during this time a significant increase of daily mean vitamin D intake from 6·2 to 8·9 µg was recorded(Reference Prasad, Lumia and Erkkola2). However, the higher level is below the recommended daily intake of 10 µg.
The adverse effects of tobacco on reproductive health and pregnancy are well established. Tobacco increases the risk of infertility in both women and men. Increased risk of pregnancy loss is also observed among smokers compared with non-smokers(3). Tobacco contains hundreds of harmful substances and well-known carcinogens. Nicotine itself is a vasoconstrictor and a neuroteratogen impacting cytotrophoblast proliferation and differentiation(Reference Rogers4). Nicotine and carbon monoxide cross the placenta rapidly and, with chronic exposure, the levels in the fetal compartment exceed those on the maternal side. Although the exact mechanisms are unknown, tobacco results in adverse pregnancy outcomes and the association between tobacco and increased risk of fetal mortality has been recognized for decades(3). Smoking is associated with low birth weight, preterm birth, placental abruption, stillbirth, sudden infant death syndrome and neurobehavioral effects such as attention-deficit hyperactivity disorder. Maternal smoking has profound effects on pregnancy and the future health of the offspring throughout life. Low birth weight and intra-uterine growth retardation are often followed by childhood obesity and metabolic changes leading to elevated blood pressure and even elevated risk of type 2 diabetes(Reference Rogers4).
In Denmark, Brot et al. reported a 10 % decrease in circulating level of 25(OH)D in smoking perimenopausal women(Reference Brot, Jensen and Sorensen5). Level of 25(OH)D has been shown to decline in a dose-dependent manner in correlation with increased pack-years of smoking(Reference Piazzolla, Castrovilli and Liotino6). During pregnancy smoking appears to have a similar effect, with the decline of maternal 25(OH)D being of the order of 10–15 %. Maternal 25(OH)D level in turn correlates with fetal concentration, and 25(OH)D is known to cross the placenta in in vitro placental perfusion studies whereas 1,25-dihydroxycholecalciferol (calcitriol) does not(Reference Kovacs7). However, the transfer of 25(OH)D from the maternal to the fetal compartment has very little effect on maternal 25(OH)D.
Vitamin D is involved in several bone homeostasis and immunoregulatory pathways where it has complex roles. Some studies suggest that prenatal exposure to vitamin D deficiency, or lower than non-pregnant parathyroid hormone levels, affects neonatal outcomes such as skeletal health, caries and growth(Reference Cooper, Westlake and Harvey8, Reference Schroth, Lavelle and Tate9). In addition, vitamin D plays a role in the human immune system and its deficiency is suggested to be associated with a number of pregnancy complications such as pre-eclampsia, small-for-gestational-age infants, gestational diabetes mellitus and recurrent pregnancy loss(Reference Wei10–Reference Hu, Zhang and Wang14). However, in pregnant women with severe vitamin D deficiency and vitamin D-dependent rickets type I or type II, in the absence of vitamin D supplementation, no change is observed in their own health or for their infant’s skeletal health(Reference Kovacs15).
The present study aimed to evaluate the effect of smoking and season on maternal 25(OH)D level in early pregnancy prior to pregnancy-related haemodilution and profound metabolic changes. The cohort with non-smoking and smoking women was selected from uncomplicated pregnancies to rule out the effects of pregnancy complications on 25(OH)D level. The cohort represents a population with low sun exposure.
Methods
We used the national population-based Finnish Medical Birth Register (FMBR) to identify smoking and non-smoking women and to investigate the effect of smoking during pregnancy on vitamin D level(Reference Raisanen, Lehto and Nielsen16).
FMBR contains data on demographics, pregnancy and delivery characteristics, as well as diagnoses on all live births or stillbirths since 1987 delivered after pregnancy week 22 or weighing >500 g during the first postnatal week. When data from multiple pregnancies were available, the most recent was used as an index pregnancy. A control group consisting of women with uncomplicated pregnancies from an unpublished pregnancy complication study included 359 uncomplicated pregnancies. Of these women, forty-six were smokers and 313 non-smokers. Serum samples from first trimester were identified within the Finnish Maternity Cohort (FMC) by a unique personal identification code, which has been assigned to each resident of Finland. Selected serum samples were then analysed for vitamin D levels.
The FMC of the Northern Finland Biobank Borealis was established in 1983 as a nationwide effort of the National Institute for Health and Welfare, Finland and is comprised of 2 million serum samples collected during the first and early second trimester of pregnancy (5th–95th percentile: months 2–4 of pregnancy) from over 950 000 women. The FMC covers more than 98 % of pregnancies in Finland with archived prenatal serum specimens drawn for routine screening for congenital infections (HIV, hepatitis B and syphilis). Following informed consent, the remaining serum samples (one sample of 1–3 ml for each pregnancy) are stored at −25°C in a protected biorepository at the Northern Finland Biobank Borealis in Oulu and are available for scientific research (www.esis.fi).
25(OH)D was measured in the first-trimester serum samples available in the FMC using a chemiluminescence microparticle immunoassay on an Architect i2000SR automatic analyser (Abbott Diagnostics) according to the manufacturer’s instructions. The chemiluminescence microparticle immunoassay test of Abbott Diagnostics has previously been found to succeed best at assaying serum 25(OH)D compared with other available methods(Reference Cashman, Dowling and Skrabakova17). Furthermore, storage time has been found to have no effect on 25(OH)D level(Reference Agborsangaya, Toriola and Grankvist18). CV, derived from repeated quality control samples included in the assay with the study samples, were calculated. In internal control samples with ‘high’ 25(OH)D (>100 nmol/l), the CV was 3·5 %; in samples with ‘medium’ 25(OH)D level (~80 nmol/l), 1·8 %; and in internal control samples with ‘low’ 25(OH)D level (<40 nmol/l), the CV was 3·0 %. In blinded quality control pairs where 25(OH)D levels were not known, the CV was 1·1 %.
Smoking status in the present study is self-reported. Individuals who reported they do not smoke were considered ‘non-smokers’ (n 313) and those who reported continued smoking after the first trimester of pregnancy were considered ‘smokers’ (n 46).
Statistical analyses
The independent-samples t test was used to assess the statistical departure of vitamin D levels in smokers’ sera from levels observed in non-smokers, because BMI did not differ between groups (Table 1) and no other data were available to be included as covariates. Vitamin D data were normally distributed according to the Kolmogorov–Smirnov test in both smokers and non-smokers. According to the Shapiro–Wilk test, non-smokers’ vitamin D data were not normally distributed (P=0·003); however, by observation of the data histograms and box plots, this was deemed to be due to two outliers (less than 1 % of data) with extremely high levels of vitamin D, while the bulk of the data conformed well to the normal distribution. We are aware that the sample sizes differ between smokers and non-smokers, but homogeneity of these groups was verified by Levene’s statistical test and no heterogeneity of variance was discovered. In the sub-analysis by season, the non-equal variance probability values are reported when Levene’s test of homogeneity of variance indicated departure from equal variances. Statistical analyses were carried out in the statistical software package IBM SPSS Statistics version 24.
Table 1 Clinical characteristics of pregnant women from a Finnish birth register cohort by smoking status
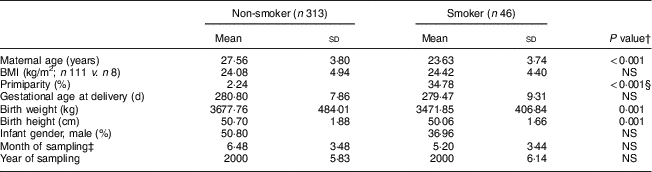
† P<0·05 is considered statistically significant.
‡ 1=January; 12=December.
§ Mann–Whitney U test; otherwise t test if not indicated.
Results
We have analysed serum 25(OH)D levels during the first trimester of healthy pregnancies in a Finnish population. The clinical characteristics of the study population are described in Table 1.
Mean serum 25(OH)D levels in the first trimester are shown in Fig. 1, which shows that 25(OH)D was significantly lower (P<0·001) in smokers (mean 32·1 (sd 14·6) nmol/l) than in non-smokers (mean 41·6 (sd 19·5) nmol/l). Figure 1 is in corroboration of previously published data indicating the decreasing effect of smoking on vitamin D level(Reference Piazzolla, Castrovilli and Liotino6).

Fig. 1 Mean serum 25-hydroxyvitamin D (25(OH)D), with 95 % CI indicated by vertical bars, by smoking status among pregnant women from a Finnish birth register cohort. Women who smoked (n 46) during pregnancy had significantly lower serum 25(OH)D than non-smoking (n 313) women: ***P<0·001
The main finding is that the mean serum 25(OH)D level of smokers in winter was 74 % of that of non-smokers and 77 % in summer. Figure 2 shows that the relationship between smoking and vitamin D was more pronounced in the winter months when exposure to sun is extremely low. The smoking–vitamin D association was observed during summer months (P=0·028) and winter months (P<0·001). Within the groups, the difference in mean serum 25(OH)D between summer and winter seasons was 41 % among smoking and 38 % among non-smoking pregnant women.

Fig. 2 Mean serum 25-hydroxyvitamin D (25(OH)D), with 95 % CI indicated by vertical bars, by smoking status and season ( , winter, November–May;
, winter, November–May;  , summer, June–October) among pregnant women from a Finnish birth register cohort. Differences between serum 25(OH)D levels in smokers and non-smokers are particularly pronounced during the winter months, when sunlight is limited in Finland: ***P<0·001 (winter: smokers, n 29; non-smokers, n 175; summer: smokers, n 17; non-smokers, n 136)
, summer, June–October) among pregnant women from a Finnish birth register cohort. Differences between serum 25(OH)D levels in smokers and non-smokers are particularly pronounced during the winter months, when sunlight is limited in Finland: ***P<0·001 (winter: smokers, n 29; non-smokers, n 175; summer: smokers, n 17; non-smokers, n 136)
Discussion
We have studied serum 25(OH)D levels in the first trimester of pregnancy in a Finnish population according to season of sampling. Among the smokers, only four women (14 %) in winter and nine women (53 %) in summer had 25(OH)D of 40 nmol/l or more, in comparison with fifty-five women (31 %) in winter and 106 women (78 %) in summer among non-smokers. The recommended reference level for 25(OH)D in Finland is 40–80 nmol/l. Vitamin D deficiency is common in Finland particularly during the winter months(Reference Kauppi, Impivaara and Maki19). In contrast, the US National Health and Nutrition Examination Survey (NHANES) reported that 7 % are deficient at<30 nmol/l and 72 % of American pregnant and lactating women have 25(OH)D level of 50 nmol/l or more(Reference Looker, Johnson and Lacher20).
With a half-life of 14–20d, 25(OH)D is a long-lived plasma metabolite and has been considered a stable and reliable marker of vitamin D status(Reference Kovacs15). Although measurement is technically challenging, the evidence on the relative difference between non-smoking and smoking pregnant women is of the order of at least 25 % independent of seasonal variability (P<0·001). The selection of normal pregnancies to the present cohort excludes the bias brought about by pregnancy complications that may be associated with alterations in 25(OH)D concentration. On the other hand, the proportion of individuals who regularly use vitamin D supplements as part of their diet is not known in the registry data used in the present study(Reference Hauta-Alus, Holmlund-Suila and Rita21). While ethnicity of the study population is not recorded, the study population is considered homogeneous as a representation of the fair Finnish general population.
Although the exact mechanisms by which tobacco results in adverse effects on pregnancy are not known, the association between tobacco and increased risk of fetal mortality has been recognized for decades(3). We do not know the exact mechanisms behind smoking and vitamin D deficiency, and even less is known about how the exacerbated effect of smoking on 25(OH)D levels is mediated during pregnancy. In the present registry-based study, detailed and verified information on possible confounding factors was not available. However, our data support that, in susceptible women, smoking during pregnancy may be a particular risk for pregnancy complications during winter months, because this group has the lowest vitamin D levels and therefore the highest risk of pregnancy complications. Further studies are needed to decipher the interaction between parathyroid hormone, vitamin D and maternal smoking in relation to neonatal outcomes. There is no evidence of smoking affecting individuals’ parathyroid hormone level(Reference Andersen, Noahsen and Rex22). Furthermore, unlike 25(OH)D, parathyroid hormone does not cross the placenta(Reference Cooper, Westlake and Harvey8). Therefore, the possible adverse consequences of smoking during pregnancy in relation to Ca homeostasis are likely related to the exaggerated deficiency of vitamin D among the smoking mothers as observed in our data. Furthermore, these effects may be interrelated and may offer new options for early preventive measures.
Conclusion
The present study shows that smoking during pregnancy is associated with a 27 % decline in serum 25(OH)D level in the first trimester. Our results also indicate that seasonal variation in 25(OH)D level is similar among smoking and non-smoking pregnant women in their first trimester of pregnancy. Taken together, these changes result in very low serum 25(OH)D among pregnant smokers, especially in wintertime, since most of the smoking women are below the recommended reference limits. To what extent the compound effect of smoking and low sun exposure directs maternal and fetal outcomes and later development and immunology of the child are still open questions. In addition, our study does not address whether being below the recommended reference limits is more dangerous in early v. late pregnancy. This cohort needs to be expanded to address these issues in the future.
Acknowledgements
Acknowledgements: The technicians at the National Institute of Health and Welfare are thanked for their skill in the laboratory analysis. Financial support: This study was financially supported by Helsinki University Hospital (J.H.-E., research grant TYH2017104); and Academy of Finland (J.H.-E., grant number 137529). Also, Jascha Foundation has generously supported the study (H.S.N.). Funders had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: A.I.L. performed the analyses and wrote the first draft of the manuscript with J.H.-E. and S.H. S.H. formulated the study question. J.H.-E. analysed the patient data and H.Ö. compiled the clinical data sheet. H.S.N. is an expert in metabolism during pregnancy and acquired the majority of the funding for this study. H.-M.S. is the principal investigator of the birth registry cohort study for pregnancy complications and oversaw the laboratory assays for 25(OH)D. All co-authors contributed to and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the ethics committee of the Hospital District of Helsinki and Uusimaa (HUS/2186/2016). Verbal consent was witnessed and formally recorded, and the use of health registers was approved by the National Institute for Health and Welfare (THL/444/5.05.00/2013).





