Introduction
The SARS-CoV-2 (COVID-19) pandemic is an unprecedented global public health crisis, entailing the loss of 6,231,018 lives and infection of more than 506 million patients worldwide as of April 20, 2022 (World Health Organization, 2022). Social interactions changed profoundly due to stay-at-home orders and curfews, travel restrictions, social distancing norms, school closures, and shifts to remote work. The pandemic also triggered a deep global economic recession (World Bank, 2020), which reverberated across the world and was also reflected in the US economy. The National Bureau of Economic Research reported that the United States witnessed its largest economic contraction during the pandemic since 1947, when record-keeping began (NBER, 2020). During this pandemic, unemployment rates spiked dramatically and deepened existing inequalities. Those most affected by unemployment were women, racial/ethnic minorities, low-wage workers, and workers with lower educational attainment (Stevenson, Reference Stevenson2020). Of concern, families with children experienced greater income losses and food shortages than those without children (Monte et al, Reference Monte2020). For instance, the rate of food insecurity doubled in the United States during the pandemic, but tripled among families with children (Schanzenbach & Pitts, Reference Schanzenbach and Pitts2020). These health, social, and economic vicissitudes exacted a major toll on population mental health, with a disproportionate burden of these effects falling on the most vulnerable groups in society (Condon et al., Reference Condon, Dettmer, Gee, Hagan, Lee, Mayes, Stover and Tseng2020; Czeisler et al., Reference Czeisler, Lane, Petrosky, Wiley, Christensen, Njai and Rajaratnam2020; Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020; Purtle, Reference Purtle2020). We aim to highlight these vulnerable groups, and this review has three major goals.
Our first goal is to summarize evidence and statistics characterizing the social determinants of mental health disparities during COVID-19 in the United States. Specifically, we summarize evidence of greater increases in mental health problems during the pandemic among socially or economically marginalized groups in the United States, including (a) people with low income or experiencing homelessness, (b) racial and ethnic minorities, (c) women and lesbian, gay, bisexual, transgender, queer, and questioning (LGBTQ+) communities, (d) immigrants and migrants, (e) children and people with a history of childhood adversity, and (f) the socially isolated and lonely. We also highlight how those who belong to multiple vulnerable groups experienced more detrimental impacts.
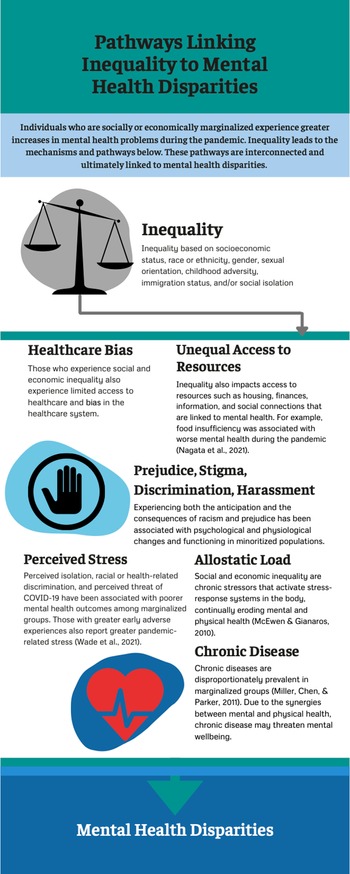
The second goal of this review is to discuss possible mechanisms explaining these disparities by linking current data from COVID-19 to existing theories (e.g., theory of fundamental causes, allostatic load theory, early-life stress sensitization theory) and prior evidence on health disparities, stress, or resilience. For each marginalized group, we first describe the evidence on mental health disparities during COVID-19, followed by a discussion of possible mechanisms contributing to these disparities. Figure 1 depicts a summary of mechanisms and pathways that may have contributed to the compounding of stress and mental health inequities for these groups during this pandemic.

Figure 1. Infographic on mechanisms and pathways linking social and economic inequality to mental health disparities surveyed in this review.
Lastly, our third goal is to propose concrete, actionable recommendations for policy, intervention, and practice that would reduce existing mental health disparities and prepare us for future calamities. We propose a new framework for promoting societal resilience that is centered on five “pillars” considered essential to societal resilience to future disasters: (1) economic safety and equity; (2) accessible healthcare (including mental health services); (3) combating racial injustice and promoting respect for diversity, equity, and inclusion; (4) child and family protection services; and (5) social cohesion. Because prior studies on mental health disparities tend to document their existence but stop short of suggesting concrete solutions, we aimed to advance this literature by connecting each section on risk to a corresponding set of solutions for promoting societal resilience. These constructive recommendations can be used by policymakers and practitioners to begin addressing mental health disparities through policy changes and intervention programs that can have tangible benefits for marginalized groups.
The scope of the review included peer-reviewed empirical studies from the United States published up to July, 2021 focused on mental health, COVID-19, and the marginalized populations of interest we specified a priori based on the broader health disparities literature (Krieger, Reference Krieger2020; Phelan et al., Reference Phelan, Link and Tehranifar2010; Williams et al., Reference Williams, Lawrence and Davis2019). We focused primarily on national and nationally representative studies as the main source of pandemic evidence to prioritize generalizability, but also drew on smaller studies or pre-pandemic research when discussing possible mechanisms and solutions, or when national studies were not available. We also restricted our review to studies from the United States as a case study, given international differences in responses to the pandemic and the need to tailor policy recommendations, but draw parallels with other countries where possible.
Low income and homelessness
Evidence on disparities during COVID-19
The COVID-19 pandemic threatened the physical, social, and emotional well-being of populations worldwide, and can be considered a traumatic event given its life-threatening, disruptive, and unpredictable nature (Goldmann & Galea, Reference Goldmann and Galea2014).
Consistent with this pattern, there was an overall increase in the prevalence of mental health problems during the pandemic compared to previous periods, but these mental health consequences were stratified based on socioeconomic status (SES). For instance, pronounced spikes in depression symptom prevalence were noted during the pandemic, with some estimates suggesting a threefold increase compared to pre-pandemic levels (Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020). However, these impacts were unequally distributed by SES, with higher levels of depression symptoms affecting those who had lower income, less than $5,000 in savings, and who experienced more stressors (Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020). Converging evidence supporting low income as a risk factor comes from the nationally representative Understanding America Study of 6,901 adults. In this panel study, participants whose income fell below the federal poverty level had 4.58 times higher odds of developing significant distress during the pandemic compared to those above the poverty level (Riehm et al., Reference Riehm, Holingue, Smail, Kapteyn, Bennett, Thrul and Pu2018). Furthermore, analyses from 63,674 participants of the US Census Household Pulse Survey conducted in 2020 revealed that food insufficiency was associated with worse mental health during the pandemic, particularly symptoms of anxiety and depression (Nagata et al., Reference Nagata, Ganson, Whittle, Chu, Harris, Tsai and Weiser2021). However, the receipt of food aid was associated with an attenuated effect of the pandemic on these symptoms (Nagata et al., Reference Nagata, Ganson, Whittle, Chu, Harris, Tsai and Weiser2021), suggesting policy solutions that could partially alleviate stress exposure through food aid programs.
People experiencing homelessness or unstable housing were particularly vulnerable during COVID-19, suffering higher rates of infection and illness than the general population, and exhibiting high rates of comorbidity with psychiatric illness and substance use (Fuchs et al., Reference Fuchs, Carter, Evans, Graham-Squire, Imbert, Bloome, Fann, Skotnes, Sears, Pfeifer-Rosenblum, Moughamian, Eveland, Reed, Borne, Lee, Rosenthal, Jain, Bobba and Kanzaria2021). Adolescent and young adult substance users who were homeless were particularly affected, with one study estimating that 16-28% reported increased use of alcohol, tobacco, and marijuana after the onset of the pandemic (Tucker et al., Reference Tucker, D'Amico, Pedersen, Garvey, Rodriguez and Klein2020). With shelter-in-place mandates and economic instability limiting residential mobility during the first year of the COVID-19 pandemic, incidences of intimate partner violence increased, and victims were placed at a greater risk for experiencing homelessness (Goodsmith et al., Reference Goodsmith, Ijadi-Maghsoodi, Melendez and Dossett2021). Future disaster-preparedness programs should address the needs of groups vulnerable to housing instability. Hotel-based isolation and quarantine intervention programs such as Project Roomkey implemented across California (Goodsmith et al., Reference Goodsmith, Ijadi-Maghsoodi, Melendez and Dossett2021) and the isolation/quarantine program implemented in San Francisco, California, provided housing and services to these groups, reducing rates of infection and leading to behavioral stabilization and improvement (Fuchs et al., Reference Fuchs, Carter, Evans, Graham-Squire, Imbert, Bloome, Fann, Skotnes, Sears, Pfeifer-Rosenblum, Moughamian, Eveland, Reed, Borne, Lee, Rosenthal, Jain, Bobba and Kanzaria2021). The State of California utilized Coronavirus Aid, Relief, and Economic Security (CARES) Act funding and followed up these efforts with Project HomeKey, a program that provided funding to local agencies to purchase and repurpose housing (e.g., hotels, motels) to provide housing to Californians experiencing homelessness. These interventions suggest viable strategies for managing and reducing mental health problems among those experiencing homelessness and could serve as a starting point for providing stable housing, service delivery, and social reintegration support.
Possible mechanisms
Although the COVID-19 pandemic is unique in the severity of its health, social, and economic disruptions, we propose that its disproportionate impact on lower-SES groups was largely predictable based on existing sociological and psychobiological theories. The sociological theory of fundamental causes, originally formulated by Link and Phelan (Reference Link and Phelan1995), proposes that SES “embodies an array of resources, such as money, knowledge, prestige, power, and beneficial social connections that protect health no matter what mechanisms are relevant at any given time” (Phelan et al., Reference Phelan, Link and Tehranifar2010, p. S28). This theory and accumulating evidence in support of this theory explains the emergence of socioeconomic disparities in health for numerous health outcomes, over different time periods, and across countries. Because the “flexible resources” (Phelan et al., Reference Phelan, Link and Tehranifar2010) provided by SES can circumvent health risks in any given context, they constitute fundamental causes of health disparities and thus apply equally well to patterns observed during the pandemic. In the context of the pandemic, high SES provided greater protection against wage losses and more opportunities for remote work, as well as greater flexibility to avoid public transportation and crowding (Brough et al., Reference Brough, Freedman and Phillips2021), to name just a few protections. In turn, this flexibility protected higher SES people against escalating mental health problems.
Psychobiological theories of stress such as the allostatic load model (McEwen & Gianaros, Reference McEwen and Gianaros2010) also provide plausible biological mechanisms for explaining socioeconomic disparities in the effects of the pandemic. Because social and economic inequality function as chronic stressors that activate stress-response systems such as the hypothalamic–pituitary–adrenal (HPA) axis, autonomic nervous system, and immune system, they can continually erode the mental and physical health of socially and economically marginalized groups (Blair & Raver, Reference Blair and Raver2016; McEwen & Gianaros, Reference McEwen and Gianaros2010). Thus, these groups can be expected to experience exacerbated neurobiological stress responses during new crises like the pandemic.
For low-income groups, mental health deterioration and higher rates of COVID-19 morbidity and mortality were inextricably linked to preexisting chronic diseases that are known to be more prevalent among socially and economically marginalized groups, such as cardiovascular, metabolic, and immune conditions (Miller et al., Reference Miller, Chen and Parker2011). Thus, social inequality can create a worsening spiral of mutually reinforcing mental and physical health problems (Hostinar et al., Reference Hostinar, Nusslock and Miller2018). Due to these synergies between mental and physical health, chronic disease morbidity represents an ongoing barrier to the resilience of low-income people, as it threatens both physical and mental well-being and it constrains one’s ability to cope with new crises. This may also undermine societal resilience, a point we develop further in our concluding section on societal resilience.
Racial and ethnic inequality
Previous work has shown that socioeconomic factors alone do not fully account for health disparities, and racism is another major contributing factor (Williams, Reference Williams1997). Both structural and cultural racism negatively exacerbate racial/ethnic disparities in mental and physical health outcomes (Williams et al., Reference Williams, Lawrence and Davis2019). These disparities exist in a broader context of structural racism. Structural racism consists of differential treatment and access to resources among racial/ethnic minorities across multiple levels and systems in society – housing, education, employment, criminal justice, and healthcare (Reskin, Reference Reskin2012; Williams et al., Reference Williams, Lawrence and Davis2019). These systems are interconnected and upheld by society, reinforcing inequality. Police brutality, an example of structural racism, set the stage for a year of racial reckoning in 2020, following the murder of George Floyd (New York Times, 2021). The increased awareness of systemic inequities that African Americans have long been confronting led to international protests and calls to action to promote antiracist policies to reduce health disparities from many organizations, including the American Heart Association (Churchwell et al., Reference Churchwell, Elkind, Benjamin, Carson, Chang, Lawrence, Mills, Odom, Rodriguez, Rodriguez, Sanchez, Sharrief, Sims and Williams2020). These events exposed the ongoing systemic racism and police brutality faced by minoritized populations, which are compounded by the effects of a global pandemic that disproportionately affected disenfranchised groups.
Racially minoritized groups also face cultural racism, which consists of an internalized community-level ideology that reinforces structural racism and generates prejudice, bias, and stereotypes (Williams et al., Reference Williams, Lawrence and Davis2019). Overall, these forms of racism have been linked to heightened stress among racialized groups, both before and during the pandemic (McKnight-Eily et al., Reference McKnight-Eily, Okoro, Strine, Verlenden, Hollis, Njai, Mitchell, Board, Puddy and Thomas2021; Williams et al., Reference Williams, Lawrence and Davis2019). Thus, it has been proposed that racism is also a fundamental cause of health inequalities (Williams, Reference Williams1997), akin to SES (Link & Phelan, Reference Link and Phelan1995).
Evidence on disparities during COVID-19
Evidence supports an increase in racial disparities in mental and physical health during the COVID-19 pandemic (Cooper & Williams, Reference Cooper and Williams2020; Selden & Berdahl, Reference Selden and Berdahl2020). Some of these disparities can be traced back to pre-pandemic structural factors such as residential segregation, which can reduce access to healthcare and expose racial/ethnic minority groups to more acute and chronic stressors (Kramer & Hogue, Reference Kramer and Hogue2009; White & Borrell, Reference White and Borrell2011).
During the COVID-19 pandemic, the effects of racism and discrimination on mental health were exacerbated by the disproportionate impact of the pandemic and related crises on racial/ethnic minority groups. Specifically, people of color had a higher risk of infection and death, due to the greater likelihood of being employed as essential workers, with Black workers most represented in high-risk occupations (Hawkins, Reference Hawkins2020; Purtle, Reference Purtle2020). Further, Black individuals at risk for severe illness are more likely to live in households with healthcare workers (Selden & Berdahl, Reference Selden and Berdahl2020). During COVID-19, frontline healthcare workers experience heightened physiological distress and mental health challenges (Kinman et al., Reference Kinman, Teoh and Harriss2020; Lai et al., Reference Lai, Ma, Wang, Cai, Hu, Wei, Wu, Du, Chen, Li, Tan, Kang, Yao, Huang, Wang, Wang, Liu and Hu2020). In addition, the devastating job losses and financial insecurity during the pandemic disproportionately affected racial and ethnic minorities (Purtle, Reference Purtle2020), specifically Black and Latina women (Gould and Wilson, Reference Gould and Wilson2020). The pandemic has also had a damaging effect on racial/ethnic minorities' mental health. In a CDC report from June 2020, the percentage of respondents who had seriously considered suicide was significantly higher in Hispanic and Black individuals compared to other groups (Czeisler et al., Reference Czeisler, Lane, Petrosky, Wiley, Christensen, Njai and Rajaratnam2020). During the height of the pandemic in 2020 in Maryland, Black individuals’ suicide rates doubled compared to previous years (Bray et al., Reference Bray, Daneshvari, Radhakrishnan, Cubbage, Eagle, Southall and Nestadt2020). Because COVID-19 mortality rates were higher for minoritized groups, this resulted in elevated rates of grief and related mental health symptoms for family members of individuals who lost their lives due to COVID-19 (Purtle, Reference Purtle2020).
In addition to experiencing greater economic stress during the pandemic, racial/ethnic minorities are at a greater risk of developing severe cases or dying of COVID-19, which adds to pandemic-related stress (Simon et al., Reference Simon, Saxe and Marmar2020). Racial/ethnic minority groups are more likely to experience psychosocial stress during the pandemic, particularly in Hispanic/Latino individuals (McKnight-Eily et al., Reference McKnight-Eily, Okoro, Strine, Verlenden, Hollis, Njai, Mitchell, Board, Puddy and Thomas2021). Social vulnerability and exclusion, more likely to be experienced by African Americans, have also been found to be associated with an increased COVID-19 death rate (Kim & Bostwick, Reference Kim and Bostwick2020). Racial disparities in vulnerability for severe COVID-19 illness emerge by middle age, and disparities in hospitalizations are greater than expected by preexisting conditions alone (Wiemers et al., Reference Wiemers, Abrahams, AlFakhri, Hotz, Schoeni and Seltzer2020). Structural racism leads to these disparities in COVID-19 illness. A recent study found that increases in COVID-19 cases and deaths were greater in areas with residential segregation, and this relation was amplified by income inequality (Yu et al., Reference Yu, Salvador, Melani, Berg, Neblett and Kitayama2021). Furthermore, life expectancy for Black and Latino populations is expected to be reduced nearly 3 to 4 times more than the reduction in life expectancy for White individuals after the pandemic. The COVID-19 pandemic has eliminated the gains made in recent years to close the Black-White life expectancy gap (Andrasfay & Goldman, Reference Andrasfay and Goldman2021). While communities grieve in the wake of these COVID-19 deaths, research shows another “wave” of the pandemic: a crisis in mental health, which is disproportionately impacting Black and Hispanic individuals (McKnight-Eily et al., Reference McKnight-Eily, Okoro, Strine, Verlenden, Hollis, Njai, Mitchell, Board, Puddy and Thomas2021; Simon et al., Reference Simon, Saxe and Marmar2020). The sudden loss of a family member and pandemic-related social disruptions can increase a risk of developing a mental health issue such as prolonged grief disorder or major depressive disorder (Simon et al., Reference Simon, Saxe and Marmar2020; Verdery et al., Reference Verdery, Smith-Greenaway, Margolis and Daw2020). Further, in a sample of Black Americans, those who perceived COVID-19 as a threat to one’s health reported higher levels of psychological distress (Cobb et al., Reference Cobb, Erving and Byrd2021). Indeed, being at a greater risk of developing COVID-19 or having a relative who has passed away from the coronavirus is likely a major contributor to mental health problems in these communities, particularly among those with preexisting mental health conditions (Cooper & Williams, Reference Cooper and Williams2020; SAMHSA, 2020).
Since the onset of the pandemic, instances of racism have increased (Bhaskar et al., Reference Bhaskar, Rastogi, Menon, Kunheri, Balakrishnan and Howick2020; Serhan & McLaughlin, Reference Serhan and McLaughlin2020). Asian communities in particular have been the targets of racism as a direct result of COVID-19 (Bhaskar et al., Reference Bhaskar, Rastogi, Menon, Kunheri, Balakrishnan and Howick2020; Serhan & McLaughlin, Reference Serhan and McLaughlin2020). There are increased reports of racism, discrimination, and violent attacks on Asian individuals across the world, and some have devastatingly turned lethal (Shear & Wright, Reference Shear and Wright2021). Some political leaders have incited negative racial stereotypes through language and phrases that attach a location or ethnicity to COVID-19, such as “Wuhan Virus” (Levenson, Reference Levenson2020). Statements like these, coupled with daily instances of discrimination, are associated with an array of negative mental health outcomes, including anxiety and depression (Hwang & Goto, Reference Hwang and Goto2008). Social media may also play a role in recent racism against Asian communities, as a stronger acceptance of social media content is associated with higher reported prejudice toward Chinese individuals (Croucher et al., Reference Croucher, Nguyen and Rahmani2020). Moreover, the proportion of tweets with negative sentiments toward Asians increased over 68% from November 2019 to June 2020 (Nguyen et al., Reference Nguyen, Criss, Dwivedi, Huang, Keralis, Hsu, Phan, Nguyen, Yardi, Glymour, Allen, Chae, Gee and Nguyen2020). Results from the “Asian Implicit Association Test” indicate anti-Asian bias declined prior to 2020, but began to increase starting in March 2020, perhaps following stigmatizing rhetoric in the media (Darling-Hammond et al., Reference Darling-Hammond, Michaels, Allen, Chae, Thomas, Nguyen and Johnson2020). Among Chinese American families surveyed in 2020, over 76% of parents and children reported vicarious racism, and nearly half reported perceived health-related anti-Chinese sentiment (Sinophobia). Exposure to racism was related to higher anxiety and depressive symptoms in both adults and children, and health-related Sinophobia was related to poor psychological well-being in adults (Cheah et al., Reference Cheah, Wang, Ren, Zong, Cho and Xue2020).
Ethnic and racial minorities have historically been disproportionately affected by other natural disasters and economic crises, now compounded by the pandemic. Following Hurricane Ike, African Americans were more likely to report posttraumatic stress disorder (PTSD) and depression compared to White and Latino respondents, and African American and Latino participants reported a greater loss of essential services due to the disaster (Davidson et al., Reference Davidson, Price, McCauley and Ruggiero2013). In some cases, these historically marginalized communities who may be rebuilding after previous disasters or acts of racism are now differentially impacted by the COVID-19 pandemic, with a potential new “wave” of mental health issues to ensue.
Possible mechanisms
Experiencing the consequences of racism has been linked to heightened stress and the development of mental health symptoms (Williams et al., Reference Williams, Lawrence and Davis2019). Over time, these experiences accelerate physical health decline, as has been shown by evidence supporting the weathering hypothesis (Geronimus, Reference Geronimus1992) for a variety of health outcomes (Forde et al., Reference Forde, Crookes, Suglia and Demmer2019).
For example, anticipating prejudice has been associated with a heightened physiological stress response and increased vigilance among Latina participants (Sawyer et al., Reference Sawyer, Major, Casad, Townsend and Mendes2012). Stereotype threat, the threat of being judged or treated unfairly due to culturally held negative stereotypes, can also affect various aspects of psychological functioning in minoritized populations. Stereotype threat has also been linked to long-term mental health outcomes such as depression and anxiety, particularly when the threat of stereotype spills over into other domains (Inzlicht et al., Reference Inzlicht, Tullett, Gutsell, Inzlicht and Schmader2012; Spencer et al., Reference Spencer, Logel and Davies2016). Internalized racism, involving an individual’s acceptance of negative race-related stereotypes, is associated with poorer mental health and increased discrimination-related distress (Millan & Alvarez, Reference Millan, Alvarez and David2014). Discrimination, internalized racism, and stereotype threat further compound disparities in mental health. In Asian Americans, stereotypes such as the “model minority stereotype,” which overlooks current racism and discrimination, can reduce access to healthcare and asking for help, as this group exhibits low usage of mental health services (Chen et al., Reference Chen, Zhang and Liu2020; Park et al., Reference Park, Stimpson, Pintor, Roby, McKenna, Chen and Ortega2019).
From a developmental perspective, racism may exert its effects most profoundly during particular windows of development, such as adolescence, a time of ethnic identity development and active socialization of racial/ethnic values (French et al., Reference French, Seidman, Allen and Aber2006; Umaña-Taylor et al., Reference Umaña-Taylor, Quintana, Lee, Cross, Rivas-Drake, Schwartz, Syed, Yip and Seaton2014). Pre-pandemic research suggested that racial/ethnic minoritized adolescents report lower levels of positive affect compared to White youth (Deer et al., Reference Deer, Shields, Ivory, Hostinar and Telzer2018), which constitutes a risk factor for depression and suicidal ideation (Rubio et al., Reference Rubio, Oyanedel, Bilbao, Mendiburo-Seguel, López and Páez2020). During the pandemic, a study analyzing support-seeking data from a national text-based crisis service reported an increase in suicidal ideation among children and adolescents compared to pre-pandemic levels, with racial/ethnic minorities, LGBTQ and gender-nonconforming youth at greatest risk (Runkle et al., Reference Runkle, Yadav, Michael, Green, Weiser and Sugg2022). Previous studies have also shown that perceived racial discrimination in young Black men (ages 20 to 23) predicted an increase in future anxiety and depression symptoms nearly 10 years later (Assari et al., Reference Assari, Moazen-Zadeh, Caldwell and Zimmerman2017). In Mexican-origin adolescents, reported ethnic discrimination was related to daily stress levels and sleep quality (Zeiders, Reference Zeiders2017). Similarly, in another racially diverse sample, adolescents who experienced higher discrimination coupled with poor sleep quality also experienced greater depressive symptoms over time; with higher discrimination related to concurrent depressive symptoms (Yip, Reference Yip2015). School-aged youth who reported greater experiences of direct racism also had higher loneliness and depressive symptoms (Priest et al., Reference Priest, Perry, Ferdinand, Paradies and Kelaher2014). In addition, White adults who work with children have been shown to hold negative stereotypes of minority children and adolescents, perhaps impacting the functioning of youth in other psychological domains (Priest et al., Reference Priest, Slopen, Woolford, Philip, Singer, Kauffman, Mosely, Davis, Ransome, Williams and Steele2018). In addition to adolescent identity development, there are other mechanisms by which racism likely impacts individuals throughout their development. For example, chronic stress experienced by pregnant women due to racism, prejudice, and discrimination may become biologically embedded during the perinatal period, impacting the developing fetus (Conradt et al., Reference Conradt, Carter and Crowell2020). Thus, experiences of racism and their impact on human development likely start early in development and have implications for future generations of racial/ethnic minorities.
The impact of COVID-19 on women and LGBTQ+ communities
Evidence on disparities during COVID-19
Sexism, heterosexism, and gender binarism represent societal systems that privilege men, heterosexual, and cisgender people, leading to unequal health outcomes (Krieger, Reference Krieger2020). These are patterns of health disparities that have been noted before the pandemic, but emerging evidence suggests that pandemic-related mental health symptoms followed the same patterns, disproportionately affecting women and LGBTQ+ people.
Nationally representative surveys examining gender differences between those identifying as women and those identifying as men reported higher rates of distress among women during the pandemic. For example, one nationally representative survey of adults ages 18 and older in the United States showed that the prevalence of elevated depression symptoms was 33.3% in women and 21.9% in men during April 2020 (Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020). The higher prevalence of distress and depressive symptoms among women compared to men during the pandemic has been documented across specific subpopulations, including seniors (Barcellos et al., Reference Barcellos, Jacobson and Stone2021), healthcare workers (Prasad et al., Reference Prasad, McLoughlin, Stillman, Poplau, Goelz, Taylor, Nankivil, Brown, Linzer, Cappelucci, Barbouche and Sinsky2021), and parents (Zamarro & Prados, Reference Zamarro and Prados2021). Nuanced results emerged in college students, among whom women exhibited greater increases in alcohol use disorder than men during the pandemic, but similar increases in symptoms of depression (Kim et al., Reference Kim, Rackoff, Fitzsimmons-Craft, Shin, Zainal, Schwob, Eisenberg, Wilfley, Taylor and Newman2021). Pregnant women emerged as a particularly vulnerable group during the pandemic, experiencing high rates of depression (36%), thoughts of self-harm (20%), and anxiety (22%) (Liu et al., Reference Liu, Zhang, Wong, Hyun and Hahm2020). Thoughts of self-harm were four times higher among pregnant women who reported death of a family member due to COVID-19 (Liu et al., Reference Liu, Zhang, Wong, Hyun and Hahm2020), suggesting a direct role of the pandemic in the development of these symptoms. Another study revealed that fear of contagion and lack of control doubled the rates of obsessive-compulsive disorder among pregnant women in the United States, reaching 7.13% (Mahaffey et al., Reference Mahaffey, Levinson, Preis and Lobel2021). Future research will need to examine the potential long-term consequences of these mental health problems on both mothers and the offspring who were in utero during the pandemic.
Studies have also begun revealing significant increases in mental health symptoms such as depression and anxiety compared to pre-pandemic levels in the LGBTQ+ population in the United States (Flentje et al., Reference Flentje, Obedin-Maliver, Lubensky, Dastur, Neilands and Lunn2020; Gonzales et al., Reference Gonzales, Loret de Mola, Gavulic, McKay and Purcell2020) and in multiple other countries (Gato et al., Reference Gato, Barrientos, Tasker, Miscioscia, Cerqueira-Santos, Malmquist, Seabra, Leal, Houghton, Poli, Gubello, Ramos Mde, Mónica, Urzúa, Ulloa and Wurm2021; Kneale & Bécares, Reference Kneale and Bécares2021). Evidence suggested greater levels of symptoms among sexual and gender minority (SGM) participants than non-SGM participants, even after controlling for preexisting mental health symptoms and lifetime discrimination (Kamal et al., Reference Kamal, Li, Hahm and Liu2021). Specifically, some data reported greater increases in mental health symptoms among those experiencing discrimination during the pandemic (Kneale & Bécares, Reference Kneale and Bécares2021). Substance use prevalence may have also increased in this population during the pandemic. Among SGM college students in the United States, 32% reported greater alcohol use since the start of the pandemic, with effects being particularly pronounced among those whose sex at birth was female (Salerno et al., Reference Salerno, Shrader, Algarin, Lee and Fish2021). Closures of universities and colleges also increased distress for LGBTQ+ students returning home to families who were unsupportive of their identity (Gonzales et al., Reference Gonzales, Loret de Mola, Gavulic, McKay and Purcell2020).
Overall, this evidence indicates that mental health inequities affecting women and LGBTQ+ groups may have exacerbated during the pandemic, but also that more research is needed that specifically collects fine-grained data regarding gender and sexual orientation in order to begin implementing strategies for promoting health equity (Gorczynski & Fasoli, Reference Gorczynski and Fasoli2020).
Possible mechanisms
Prevailing theory suggests three general pathways that lead to health disparities for women and LGBTQ+ people (Krieger, Reference Krieger2020). These include structural forces (e.g., laws, policies, and rules) that place these groups at a disadvantage and limit their economic opportunities; interpersonal exposures such as discriminatory behaviors and beliefs of privileged groups against these groups; and internalized beliefs by women and LGBTQ+ people that may harm mental health (Krieger, Reference Krieger2020). Internalized beliefs represent an individual’s acceptance of others’ biased views of them as accurate, leading to shame and mental health difficulties (Krieger, Reference Krieger2020). This is exemplified by women experiencing self-blame in the aftermath of experiencing gender-based violence. In addition to these factors suggested by Krieger (Reference Krieger2020), there are also additional sociocultural and psychobiological factors that disproportionately impacted women during the pandemic.
One specific social and cultural factor with widespread impact on mental health during the pandemic has been increased demand for unpaid care work (e.g., care for dependent children, family caregiving for adults with chronic illness). At the beginning of the pandemic, many schools and daycare centers were closed, and many care services and supports for adults with chronic or acute health needs became inaccessible or curtailed, leaving gaps in childcare and eldercare that were, and continue to be, disproportionately filled by women (Connor et al., Reference Connor, Madhavan, Mokashi, Amanuel, Johnson, Pace and Bartz2020; Power, Reference Power2020). Caregiving during COVID-19 has been associated with poorer mental health regardless of gender. Family caregivers of adults with chronic illness reported increases in caregiving intensity, complexity, and caregiver burden as a result of the pandemic, in addition to reporting higher anxiety, depression, and substance use to manage COVID-19 stressors than non-caregiving adults (Beach et al., Reference Beach, Schulz, Donovan and Rosland2021; Cohen et al., Reference Cohen, Kunicki, Drohan and Greaney2021; Czeisler et al., Reference Czeisler, Lane, Petrosky, Wiley, Christensen, Njai and Rajaratnam2020; Park, Reference Park2021). Similarly, parents caring for minor children reported significantly higher anxiety, depression, suicidal ideation, and alcohol use than adults without childcare responsibilities (Czeisler et al., Reference Czeisler, Lane, Petrosky, Wiley, Christensen, Njai and Rajaratnam2020; Gadermann et al., Reference Gadermann, Thomson, Richardson, Gagné, McAuliffe, Hirani and Jenkins2021). For both parents and family caregivers, the burden of care and associated adverse mental health outcomes were more likely to be borne by women. During the pandemic, women have spent significantly more time than men caring for children or for adults with chronic illness, even while maintaining employment (Cohen et al., Reference Cohen, Kunicki, Drohan and Greaney2021; Gadermann et al., Reference Gadermann, Thomson, Richardson, Gagné, McAuliffe, Hirani and Jenkins2021). In terms of mental health, mothers of young children have reported significantly greater psychological distress during COVID-19 than fathers or women without young children in the home (Zamarro & Prados, Reference Zamarro and Prados2021). Similarly, for caregivers of patients with chronic illness, poor mental health outcomes in response to caregiving stress have been significantly worse for female caregivers (Beach et al., Reference Beach, Schulz, Donovan and Rosland2021). The widening of gender disparities in mental health during the pandemic has been driven in part by inequitable increases in unpaid care work and will likely have long-term impacts on women’s health (Almeida et al., Reference Almeida, Shrestha, Stojanac and Miller2020; Connor et al., Reference Connor, Madhavan, Mokashi, Amanuel, Johnson, Pace and Bartz2020; Power, Reference Power2020).
To further specify the psychobiological pathways by which inequality translates into unequal mental and physical health outcomes, the minority stress model has been proposed (Lick et al., Reference Lick, Durso and Johnson2013; Meyer, Reference Meyer2003). Experiencing or fearing possible harassment, discrimination, and stigma can increase distress and undermine well-being (Lick et al., Reference Lick, Durso and Johnson2013), as these experiences constitute forms of social stress (Meyer, Reference Meyer2003). Studies of stressful experiences among SGM groups have implicated some of the same stress-physiological pathways previously studied in connection with other chronic stressors, such as activation and possible dysregulation of the autonomic nervous system, HPA axis, and immune system, which increase allostatic load and risk of mental and physical health problems (Lick et al., Reference Lick, Durso and Johnson2013). More research with these populations is needed to fully specify these mechanisms and to test their effects during COVID-19, but initial evidence suggests the need to allocate increased mental health resources to women and LGBTQ+ groups.
Immigrants, migrants, and mental health
Evidence on disparities during COVID-19
How cultural risk factors and mechanisms have impacted mental health outcomes for immigrants and migrants during the COVID-19 pandemic is relatively understudied. Further examination of COVID-19’s impacts on mental health outcomes for immigrant and migrant communities is necessary and could inform strategies and interventions for improving mental health outcomes for this group.
Because evidence suggests that, before the pandemic, immigrants and migrants were at increased risk of experiencing mental health problems (Garcini et al., Reference Garcini, Murray, Zhou, Klonoff, Myers and Elder2016), research examining how COVID-19 has potentially exacerbated this risk requires further investigation. Currently, we are aware of two studies that have. One study measured immigrant outpatient mental health outcomes pre-pandemic compared to mental health outcomes during the pandemic and found significant increases in levels of depression, anxiety, and psychological stress (Serafini et al., Reference Serafini, Powell, Frere, Saali, Krystal, Kumar, Yashaswini, Hernandez, Moody, Aronson, Meah and Katz2021). Another study examining the effects of social distancing measures (i.e., shelter-in-place orders) found similar results when measuring immigrant workers’ mental health (i.e., depression, anxiety, and stress levels) following a dormitory outbreak of COVID-19 (Saw et al., Reference Saw, Tan, Buvanaswari, Doshi and Liu2021). The authors found that social distancing measures were positively associated with stress and depression symptomatology, and increased worry about being diagnosed with COVID-19 was positively associated with anxiety symptomatology (Saw et al., Reference Saw, Tan, Buvanaswari, Doshi and Liu2021). Furthermore, the authors found that immigrant workers who had greater uncertainties about job security, perceived their health as poor, or who had greater exposure to COVID-19 reported higher rates of stress, depression, and anxiety (Saw et al., Reference Saw, Tan, Buvanaswari, Doshi and Liu2021). Together, these findings suggest that the mental health of immigrant and migrant communities was affected by the pandemic. Yet, more work is needed to better understand mental health outcomes in these communities.
In addition to these mental health concerns, variations in immigration status and socioeconomic position have also contributed to immigrants’ and migrants’ access to mental healthcare resources and treatment. During the pandemic, undocumented immigrants suffered from fear of deportation, lack of access to social services such as healthcare, did not qualify for national unemployment benefits, were initially excluded from government relief packages, and some remain ineligible for federally funded health insurance programs (Page et al., Reference Page, Venkataramani, Beyrer and Polk2020; Wilson & Stimpson, Reference Wilson and Stimpson2020). Some immigrant and migrant communities are also at higher risk of living under poor conditions that exacerbate COVID-19 transmission (e.g., facilities with poor sanitation, confined living conditions), tend to come from lower socioeconomic backgrounds, and have limited access to healthcare and mental health resources (Bhaskar et al., Reference Bhaskar, Rastogi, Menon, Kunheri, Balakrishnan and Howick2020).
Despite efforts by local state governments to support immigrant and migrant groups through policies such as extending stimulus checks to undocumented immigrants in California (Botts, Reference Botts2021), the further marginalization of immigrant and migrant groups during the pandemic created additional barriers to accessing mental healthcare treatment (Page et al., Reference Page, Venkataramani, Beyrer and Polk2020). Due to the disproportionate impact COVID-19 has had upon the immigrant and migrant community, more action is needed to provide a more effective economic “safety net” to protect this vulnerable group within the United States.
Possible mechanisms
Examining cultural factors may help elucidate the mechanisms by which the pandemic differentially affected immigrant and migrant communities. Because immigrants are not a monolithic entity, we see significant cultural variability in how immigrants have adapted to US culture and the pandemic (Barry, Reference Barry1997; Liem et al., Reference Liem, Andre, Hannam, Lam and Hall2021). In the United States, differences between collectivistic versus individualistic cultures can broadly provide valuable insight into possible mechanisms shaping mental health outcomes during and after the COVID-19 pandemic. In collectivistic cultures, for example, cultural values such as familism and filial piety are associated with mental health outcomes (Schwartz et al., Reference Schwartz, Weisskirch, Hurley, Zamboanga, Park, Kim, Umaña-Taylor, Castillo, Brown and Greene2010). During the pandemic, researchers found that Latino families’ increased worry was connected to concern for one’s local family and community as well as for family members living abroad (Moyce et al., Reference Moyce, Velazquez, Claudio, Thompson, Metcalf, Aghbashian, Vanderwood and Sisson2021). In a separate study, communities that endorsed more family-oriented beliefs also had increased worries about spreading the coronavirus to relatives (Germani et al., Reference Germani, Buratta, Delvecchio and Mazzeschi2020). Another study found that Latino mothers who were essential workers reported economic cutbacks and higher rates of stress and depressive and anxiety symptoms (Hibel et al., Reference Hibel, Boyer, Buhler-Wassmann and Shaw2021). Foreign-born respondents, Latinos, Asians, women, and families with children under 18 also reported higher levels of subjective fear and worry during the pandemic (Fitzpatrick et al., Reference Fitzpatrick, Harris and Drawve2020). Overall, these studies provide an understanding of cultural mechanisms that contribute to increased stress, fear, or worry during the pandemic and can help identify pathways by which negative psychological outcomes develop as a result of COVID-19.
Some research has also highlighted the benefits of cultural resources and coping mechanisms in promoting mental health and resilience throughout the COVID-19 pandemic. Despite strict social distancing measures and stay-at-home orders, researchers found that increased reliance on the community and increased communication with family members promoted positive feelings of unity and support (Moyce et al., Reference Moyce, Velazquez, Claudio, Thompson, Metcalf, Aghbashian, Vanderwood and Sisson2021). In addition, telecommunication created space for immigrant and migrant communities to reconnect with family in their native countries, promoting social support and social connectedness (Moyce et al., Reference Moyce, Velazquez, Claudio, Thompson, Metcalf, Aghbashian, Vanderwood and Sisson2021). However, decreases in social support have had the opposite effect. In Chinese adolescents, lower social support increased depression and anxiety symptomatology (Qi et al., Reference Qi, Zhou, Guo, Zhang, Min, Li and Chen2020). Thus, across cultures it appears that maintaining close relationships and utilizing alternative forms of social support is important for alleviating some of the negative mental health consequences resulting from the pandemic. For immigrant communities specifically, increasing collective efficacy can provide additional protective effects against negative mental health outcomes among immigrant-dense neighborhoods (Feldmeyer et al., Reference Feldmeyer, Madero-Hernandez, Rojas-Gaona and Sabon2019).
In sum, developing a deeper understanding of the cultural mechanisms impacting mental health during the COVID-19 pandemic is an important area of research. Recognizing how cultural mechanisms can exacerbate risk or promote resilience will provide valuable information for future policy and serve as a blueprint for navigating future disasters. More specifically, for immigrant and migrant communities who are among the most vulnerable populations affected by the pandemic, we can alleviate some of the negative mental health outcomes by providing equitable access to mental healthcare resources and treatment. To achieve this goal, it will be important to develop greater access to affordable health and mental healthcare options and provide culturally sensitive resources to immigrant and migrant communities (e.g., news and resources tailored to each community’s native language, culturally appropriate resources and treatment). As we discuss in more depth in our later section on promoting societal resilience, we also recommend training clinicians and mental health professionals in adopting a cultural humility framework (Tervalon & Murray-García, Reference Tervalon and Murray-Garcia1998; Murray-García et al., Reference Murray-Garcia, Harrell, Garcia, Gizzi and Simms-Mackey2014) to dismantle mental health inequities affecting immigrants and migrants.
Childhood adversity and the pandemic
Evidence on disparities during COVID-19
Adverse childhood experiences (ACEs) are “potentially traumatic events that occur in childhood (0–17 years)” (Centers for Disease Control and Prevention, 2020) and encompass a wide range of experiences, from child maltreatment to parental incarceration. Experiencing more ACEs is associated with altered stress physiology (Deer et al., Reference Deer, Bernard, Hostinar, Welling and Shackelford2019) and poorer mental and physical health outcomes across the lifespan (Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards, Koss and Marks1998). These outcomes, in turn, are associated with decreased productivity and earlier mortality, which have been shown to have negative economic consequences at the societal level (Bellis et al., Reference Bellis, Hughes, Ford, Ramos Rodriguez, Sethi and Passmore2019; Metzler et al., Reference Metzler, Merrick, Klevens, Ports and Ford2017).
Researchers and practitioners believe the COVID-19 pandemic has increased and exacerbated the prevalence of child maltreatment and domestic violence, especially in low SES communities (Bryant et al., Reference Bryant, Oo and Damian2020; Campbell, Reference Campbell2020). Pre-pandemic research had already established links between low SES, income inequality, and child maltreatment (Berger, Reference Berger2005; Eckenrode et al., Reference Eckenrode, Smith, McCarthy and Dineen2014). The Georgetown University Center on Education & the Workforce (2021) estimated that 23 million Americans lost their jobs in April 2020, in addition to a vast number of Americans who had their hours and wages reduced during the pandemic. Therefore, the economic impact of COVID-19 on families is an important variable to include when considering what factors led to increases in ACEs during the pandemic.
Lawson et al. (Reference Lawson, Piel and Simon2020), who found that job loss during the pandemic increased the likelihood of child maltreatment, provides further support for the link between the pandemic’s impact on family income and child maltreatment. Similarly, Lee et al. (Reference Lee, Ward, Lee and Rodriguez2021) found that job loss due to the pandemic was associated with increased use of physical punishment as a form of discipline. Additionally, Brown et al. (Reference Brown, Doom, Lechuga-Peña, Watamura and Koppels2020) reported that precarious financial circumstance and symptoms of anxiety or depression were associated with greater child abuse potential in a survey study of 183 families in the United States with children under the age of 18. Increases in stress and strain among parents and caregivers are worrying, because they may impair parents’ and caregivers’ abilities to serve as stress buffers for children, thus having spillover negative impacts on child mental health (Condon et al., Reference Condon, Dettmer, Gee, Hagan, Lee, Mayes, Stover and Tseng2020).
Parental social isolation is another common predictor of child maltreatment in the pre-pandemic literature (Berlin et al., Reference Berlin, Appleyard and Dodge2011). This is concerning, as the COVID-19 pandemic has necessitated the loss of physical contact to control the spread of the disease. As such, many schools, businesses, and religious institutions suspended operations or transferred to remote work (Bartik et al., Reference Bartik, Bertrand, Cullen, Glaeser, Luca and Stanton2020; Olneck-Brown, Reference Olneck-Brown2021). Shelter-in-place and social distancing orders therefore led children and adolescents to spend more time at home, potentially with their abusers (Campbell, Reference Campbell2020). Indeed, parental social isolation during the pandemic has been linked to increased verbal aggression as well as harsh discipline and greater conflict between parents and their children (Lee et al., Reference Lee, Ward, Lee and Rodriguez2021). This higher risk of exposure to maltreatment is compounded by the fact that children and adolescents had reduced contact with mandated reporters and more limited opportunities to disclose their maltreatment to someone they trust outside the home (Donagh, Reference Donagh2020; Welch & Haskins, Reference Welch and Haskins2020). Both parents and their children had reduced interactions with friends, teachers, extended family members, larger peer groups, and other community members, limiting their access to social support networks (Rogers et al., Reference Rogers, Ha and Ockey2021).
As a result of the pandemic, maltreatment rates are suspected to have increased, but seem to be underreported. For instance, Swedo et al. (Reference Swedo, Idaikkadar, Leemis, Dias, Radhakrishnan, Stein and Holland2020) found that the proportion of emergency room visits due to child abuse/neglect increased in 2020 compared to 2019, and a greater number of these visits ended in hospitalization, although reports of child maltreatment to government agencies decreased by an estimated 40–60% (Weiner et al., Reference Weiner, Heaton, Stiehl, Chor, Kim, Heisler, Foltz and Farrell2020). Similar patterns can be seen when examining natural disasters and other large-scale emergencies. For example, one study revealed that child abuse rates increased from 1 year before to after Hurricane Hugo in South Carolina and after the Loma Prieta earthquake in California’s Bay Area (Curtis et al., Reference Curtis, Miller and Berry2000). Overall, the literature tends to show that rates of child maltreatment and domestic violence often increase following these types of events, but this is not always reflected in formal reports (Campbell, Reference Campbell2020; Curtis et al., Reference Curtis, Miller and Berry2000; Parkinson, Reference Parkinson2019; Seddighi et al., Reference Seddighi, Salmani, Javadi and Seddighi2019; but see also Cerna-Turoff et al., Reference Cerna-Turoff, Fischer, Mayhew and Devries2019).
In summary, there is strong evidence that childhood adversity can have serious negative long-term consequences for mental and physical health, which are costly for society and individuals alike (Edwards et al., Reference Edwards, Holden, Felitti and Anda2003; Gilbert et al., Reference Gilbert, Breiding, Merrick, Thompson, Ford, Dhingra and Parks2015; Herzog & Schmahl, Reference Herzog and Schmahl2018; Hughes et al., Reference Hughes, Bellis, Hardcastle, Sethi, Butchart, Mikton, Jones and Dunne2017; Thompson et al., Reference Thompson, Kingree and Lamis2019). The COVID-19 pandemic has increased the number of ACEs children and adolescents have experienced, and could be, itself, considered an ACE event for many people. However, while some ACEs are likely detrimental for all children, there is variation in their impact and individual interpretation, as trauma is a subjective experience. For example, the pandemic may be experienced differentially among children from varying levels of SES (Barnett, Reference Barnett2008; Lawson et al., Reference Lawson, Piel and Simon2020). Therefore, more research is needed to understand the development of individual differences in response to ACEs. Doing so will help elucidate how an event like the COVID-19 pandemic can be a traumatic experience as well as help determine protective factors that combat the negative consequences of the pandemic. Serious efforts need to be made to prevent ACEs, rather than simply trying to mitigate their consequences.
Possible mechanisms
Childhood adversities may increase risk of mental health problems during the pandemic through the mechanism of early-life stress sensitization, which involves amplification or dysregulation of neurobiological stress responses among those with childhood trauma (Hostinar et al., Reference Hostinar, Swartz, Alen, Guyer and Hastings2021; Post & Weiss, Reference Post and Weiss1998; Tsur & Abu-Raiya, Reference Tsur and Abu-Raiya2020). Another mechanism is stress accumulation, whereby those who experience early-life adversity often continue to live in environments that expose them to higher rates of adversity and trauma in adulthood, thus compounding the effects of early-life stress throughout the lifespan (Hostinar et al., Reference Hostinar, Lachman, Mroczek, Seeman and Miller2015; Widom et al., Reference Widom, Czaja and Dutton2008). As an example of stress sensitization, John-Henderson (Reference John-Henderson2020) examined the effects of childhood trauma on sleep quality in a population of American Indian adults. Childhood trauma was a significant predictor of greater stress and decreased sleep quality during the COVID-19 pandemic, even after controlling for current socioeconomic circumstances statistically. Similarly, Wade et al. (Reference Wade, Prime, Johnson, May, Jenkins and Browne2021) found that having more pre-pandemic ACEs predicted greater pandemic-related stress and mental health symptoms among adult caregivers, independently of COVID-19-related stress. Parental mental illness is, in itself, considered an ACE (Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards, Koss and Marks1998) and may be another mechanism by which children may be experiencing an increased exposure to ACEs during the COVID-19 pandemic.
Preliminary evidence supports the early-life stress sensitization pathway. For instance, Guo et al. (Reference Guo, Fu, Liu, Zhang, Wang and van Ijzendoorn2020) examined pre-pandemic ACEs and mental health ratings taken during the COVID-19 pandemic in a sample of Chinese adolescents. They found that exposure to more pre-pandemic ACEs predicted more anxiety in their sample, and PTSD symptoms were increased among adolescents who experienced more pre-pandemic ACEs and more COVID-19-related stressors, such being infected with the coronavirus or having a family member, friend, or acquaintance suffer from COVID-19. In another study, Tsur and Abu-Raiya (Reference Tsur and Abu-Raiya2020) focused specifically on ACEs related to child maltreatment and examined whether histories of child abuse (sexual abuse, physical abuse, and emotional abuse) predicted COVID-19-related fear and stress. Data were collected in Israel during the early months of the pandemic (March through May 2020). Child abuse survivors experienced more symptoms of complex PTSD, which were in turn related to increased fear and anxiety about COVID-19 (Tsur & Abu-Raiya, Reference Tsur and Abu-Raiya2020).
Another likely pathway is suggested by the biological embedding model (Miller et al., Reference Miller, Chen and Parker2011), which describes pathways from experiences of childhood adversity like maltreatment or poverty to later chronic disease via alterations in cardiovascular, metabolic, and immune system functioning. Thus, childhood adversities can worsen physical health, and these preexisting health conditions can compromise immune competence during pandemics. In turn, these physical health problems can undermine mental health and limit the ability to cope with new crises.
Social isolation and loneliness during COVID-19
Evidence of disparities during COVID-19
When initial stay-at-home orders were implemented to curb the spread of COVID-19, a natural experiment began that exposed people to prolonged periods of reduced social interaction. Although evidence suggests mixed results regarding population-level increases in loneliness as a result of these social restrictions (Luchetti et al., Reference Luchetti, Lee, Aschwanden, Sesker, Strickhouser, Terracciano and Sutin2020), certain subsets of the population appeared to be at greater risk of experiencing loneliness during quarantine than others.
Given the vast literature that social isolation and loneliness are associated with negative health outcomes (Cacioppo et al., Reference Cacioppo, Cacioppo, Capitanio and Cole2015), it is important to identify those who may be at increased risk of being socially isolated and lonely during the pandemic. In the United States, mean-level increases in loneliness were not observed from pre- to 1 month post-pandemic onset in a nationally representative study of adults ages 18 and up (Luchetti et al., Reference Luchetti, Lee, Aschwanden, Sesker, Strickhouser, Terracciano and Sutin2020). In fact, participants reported increases in perceived support on average, though this result needs to be interpreted with caution because participants high in loneliness were less likely to participate in the follow-up waves during the pandemic. In addition, certain subgroups such as older adults (65 years or older) reported a small acute increase in loneliness immediately after the stay-at-home orders in March 2020, which levelled off by follow-up in April 2020. Across waves, participants with chronic disease and those who lived alone reported higher levels of loneliness compared to those without chronic disease and those living with others (Luchetti et al., Reference Luchetti, Lee, Aschwanden, Sesker, Strickhouser, Terracciano and Sutin2020), suggesting similar risk factors for loneliness before and after the pandemic. Consistent with this result, cross-cohort analyses of data from adults in the United Kingdom captured before and during the pandemic also found that risk factors for loneliness were nearly identical before and during the pandemic, suggesting that people who were already at risk of being lonely pre-pandemic were at heightened risk during the COVID-19 pandemic (Bu et al., Reference Bu, Steptoe and Fancourt2020). Those at risk, specifically, were young adults, people living alone, people with lower education or income, women, and racial/ethnic minority groups (Bu et al, Reference Bu, Steptoe and Fancourt2020). This is especially alarming, considering that groups who already face health disparities due to their age, sex, race, and SES (Phelan et al., Reference Phelan, Link and Tehranifar2010; Victor & Bowling, Reference Victor and Bowling2012; Williams et al., Reference Williams, Lawrence and Davis2019) seem to share more of the burden of the impact of social distancing efforts implemented to halt the spread of COVID-19.
In a cross-sectional study, Liu et al. (Reference Liu, Zhang, Wong, Hyun and Hahm2020) assessed the potential risk and protective factors for mental health problems in young adults aged 18-30 years old after the onset of the pandemic. Researchers found that a key predictor associated with depression, anxiety, and PTSD during the pandemic was loneliness. Specifically, those participants with high levels of loneliness and worries about the COVID-19 pandemic were more likely to score above clinical cutoffs for depression, anxiety, and PTSD during the pandemic. Although the majority of respondents reported feeling lonely during the first 2 months of the pandemic (61.5% of this young adult sample), as well as having low resilience (72%) and low distress tolerance (74.1%), this sample also reported having access to both social support and instrumental support (Liu et al., Reference Liu, Zhang, Wong, Hyun and Hahm2020). Concerningly, however, 37% of respondents reported low family support.
Because adults 65 years and older had the highest risk of suffering negative outcomes due to contracting COVID-19 (CDC, 2021), strategies to avoid the spread of coronavirus were especially important for this age group. However, it was feared that these strict measures would have the unintended consequence of increasing social isolation and loneliness. To better understand the experiences of older adults during the COVID-19 pandemic, Kotwal et al. (Reference Kotwal, Holt-Lunstad, Newmark, Cenzer, Smith, Covinsky and Perissinotto2021) interviewed 460 community-dwelling older adults in the San Francisco Bay Area during the shelter-in-place orders. While some participants successfully used technology to maintain social connections, others mentioned either discomfort with it or not having adequate access to the Internet (Kotwal et al., Reference Kotwal, Holt-Lunstad, Newmark, Cenzer, Smith, Covinsky and Perissinotto2021). Additionally, over half of participants reported worsened feelings of loneliness and were more likely to self-report worsened depression and anxiety during the study period. In follow-up interviews, several of these participants experienced increased loneliness scores or had loneliness scores that remained high over time. In open-ended responses from participants who reported worsened loneliness, participants described the COVID-19 restrictions as amplifying prior social losses and reported difficulty using technology, overwhelming feelings of being trapped, and loneliness affecting their physical and mental health (Kotwal et al., Reference Kotwal, Holt-Lunstad, Newmark, Cenzer, Smith, Covinsky and Perissinotto2021).
While emerging new evidence is shedding light on the associations between preventative measures enacted to curb the spread of the coronavirus and feelings of loneliness, much more research is needed to identify individual differences in susceptibility to loneliness. The data described here were collected during the first few months of the stay-at-home orders; however, the COVID-19 pandemic is a worldwide stressor without a foreseeable endpoint. Because of this, there is a need for longitudinal studies to focus on long-term trends beyond the first few months of the pandemic. Interventions aimed at decreasing social isolation and feelings of loneliness should target specifically those who need it most and those who experience barriers to using technology to connect with others.
Possible mechanisms
Social isolation and loneliness have long been recognized as risk factors for depression and anxiety, as well as for premature mortality from varying causes (Banerjee & Rai, Reference Banerjee and Rai2020; Cacioppo et al., Reference Cacioppo, Cacioppo, Capitanio and Cole2015; House et al., Reference House, Landis and Umberson1988). Mechanistic studies have suggested that social isolation and loneliness can elicit neural, neuroendocrine, and behavioral responses that can lead to changes in brain function across multiple brain regions (Cacioppo et al., Reference Cacioppo, Cacioppo, Capitanio and Cole2015). In adults, perceived isolation and loneliness can lead to heightened attention to social threats and negative social stimuli, along with increased anxiety, hostility, and social withdrawal (Cacioppo et al., Reference Cacioppo, Cacioppo, Capitanio and Cole2015). Social isolation can also activate stress-response systems, continually affecting neural architecture and behavior via changes in gene expression (McEwen, Reference McEwen2018). Specifically, growing evidence suggests that in humans, loneliness and social threat are associated with chronic activation of neuroendocrine stress-response systems like the HPA axis. This is a cause for concern, given that chronically elevated stress hormone production can lead to “wear and tear” (allostatic load) on the body, increasing the risk of numerous deleterious psychological and physical health outcomes (Cacioppo et al., Reference Cacioppo, Cacioppo, Capitanio and Cole2015). This research suggests the importance of promoting social cohesion and access to social support at a societal level, particularly during periods when global stressors such as quarantines and other crises diminish social interactions.
Conclusions and lessons from COVID-19: Promoting societal resilience to future disasters
Resilience has been defined as the capacity to adapt to challenges and threats and can characterize individuals as well as broader systems such as countries (Masten, Reference Masten2020). The resilience of individuals depends on the proper functioning of higher-order social systems that individuals are embedded in, such as local communities and national governments (Masten, Reference Masten2020). When higher-order systems break down, more stress is placed upon individuals and family systems to compensate. Because of these continuous dynamic transactions between the resilience of individuals and that of society as a whole, we propose strategies to promote five “pillars” of societal resilience (Figure 2). In this model, we consider how (1) economic safety and equity, (2) accessible healthcare, (3) combating racial injustice and promoting respect for diversity, equity, and inclusion, (4) child and family protection services, and (5) social cohesion are beneficial for ensuring the resilience of both individuals and society as a whole. We suggest policies, interventions, and individual or community-level changes that will promote these foundational aspects of societal resilience in response to future disasters.
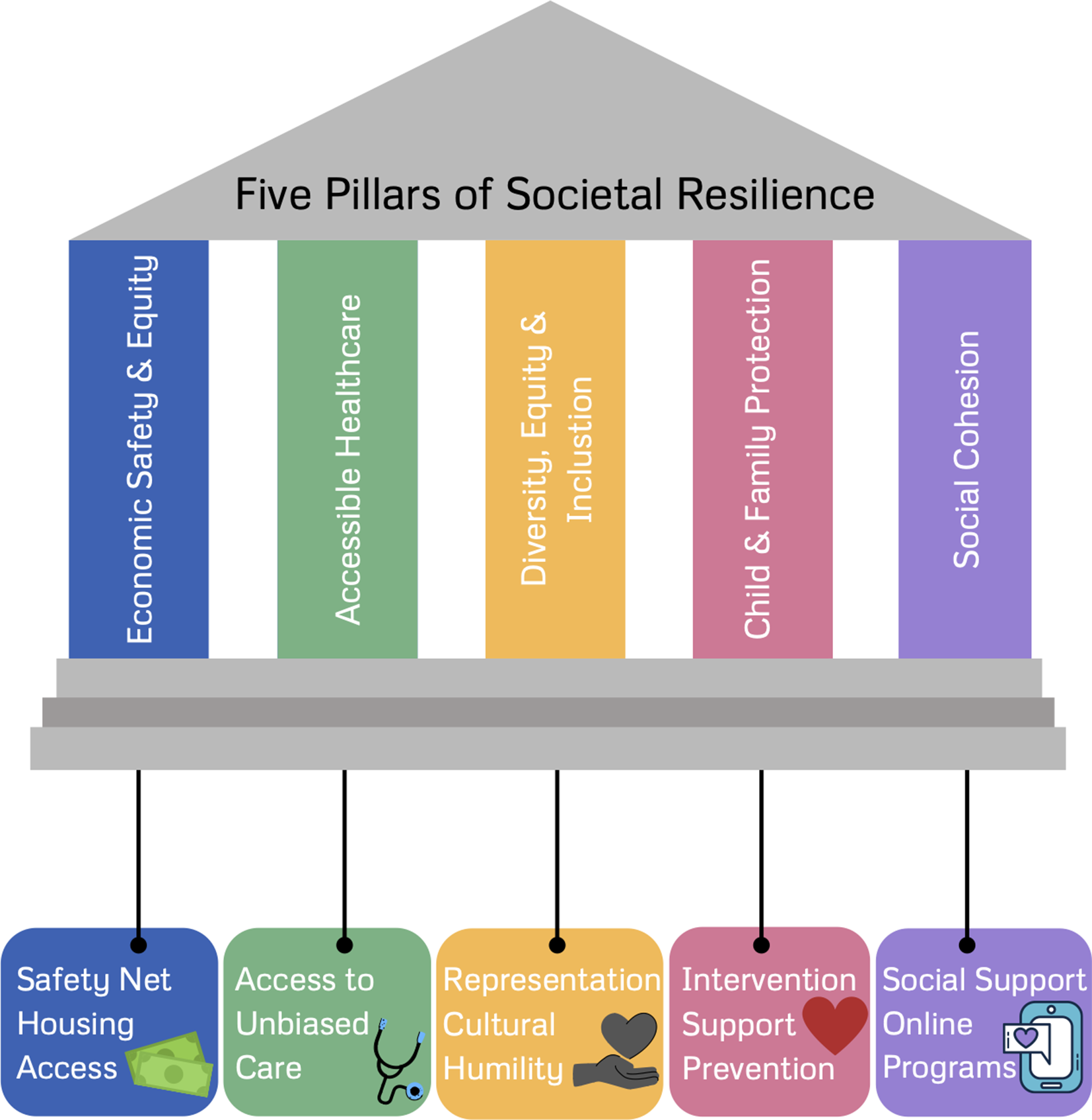
Figure 2. Five proposed “pillars” of societal resilience.
During the COVID-19 pandemic, countries with greater income inequality, as reflected by the Gini coefficient, witnessed higher COVID-19 cases and deaths, even after accounting for these countries’ gross domestic product, average life expectancy, proportion of population aged over 65, and stringency of lockdown measures (Wildman, Reference Wildman2021). This pattern suggests that social and economic inequality undermines societal resilience, and that removing these sources of inequality may provide greater societal resilience during times of crisis.
Economic safety and equity
Beyond the deleterious impacts of poverty on mental health (Blair & Raver, Reference Blair and Raver2016; Yoshikawa et al., Reference Yoshikawa, Aber and Beardslee2012), economic inequality also has a salient impact on life expectancy and mental health in countries like the United States (Hill & Jorgenson, Reference Hill and Jorgenson2018; Ribeiro et al., Reference Ribeiro, Bauer, Andrade, York-Smith, Pan, Pingani, Knapp, Coutinho and Evans-Lacko2017). Much like the impact of previous disasters, the brunt of the COVID-19 pandemic has been experienced by lower-resourced communities (Fothergill & Peek, Reference Fothergill and Peek2004; Hawkins, Reference Hawkins2020), thus economic safety and equity should be prime targets for promoting population mental health and societal resilience.
To promote resilience to future calamities, existing economic “safety net” policies require expansion, and new policies need consideration and examination. These include cash transfer and income supplement programs, broader food assistance programs, and more support for housing and residential mobility. In late March 2020, the United States passed the CARES Act, the largest stimulus bill passed until March 2021. The CARES Act provided a one-time cash transfer to individuals and families that maintained poverty at precrisis levels (Parolin et al., Reference Parolin, Curran and Wimer2019), but did not fully alleviate the economic stress in lower-resourced communities (Bitler et al., Reference Bitler, Hoynes and Schanzanbach2020). Two later stimulus payments in December 2020/January 2021 and March 2021 were provided. The evidence suggests that sustained cash transfer programs piloted in other nations have been shown to reduce stress, prevent family violence, and increase long-term living standards (Handa et al., Reference Handa, Natali, Seidenfeld, Tembo and Davis2018; Haushofer et al., Reference Haushofer, Ringdal, Shapiro and Wang2019). A monthly child allowance has been projected to completely eliminate severe child poverty in the United States, potentially disrupting intergenerational cycles of poverty (Shaefer et al., Reference Shaefer, Collyer, Duncan, Edin, Garfinkel, Harris, Smeeding, Wimer, Waldfogel and Yoshikawa2018). The Child Tax Credit is an example of a policy that has been effective at reducing the rate of child and family poverty to historic lows (Wise & Chamberlain, Reference Wise and Chamberlain2022). Cash transfers and child allowances have also shown more efficacy in reducing food insecurity in Canada than the Supplemental Nutrition Assistance Program (SNAP) in the United States, a program tied to income and limited in eligibility terms (Loopstra, Reference Loopstra2018).
Additionally, housing unaffordability remains a structural barrier to disaster resilience. Providing permanent housing to the unhoused has become urgent during the COVID-19 pandemic and has increased popularity for innovative policies that aggressively address housing insecurity (Batko et al., Reference Batko, Gerken, Girod and Moraras2022). For people living in high-poverty neighborhoods, residential mobility programs such as Moving to Opportunity have shown reductions in personal distress and improved well-being 15 years later (Leventhal & Brooks-Gunn, Reference Leventhal and Brooks-Gunn2003; Ludwig et al., Reference Ludwig, Duncan, Gennetian, Katz, Kessler, Kling and Sanbonmatsu2012). Among individuals from high-poverty neighborhoods, one standard deviation reduction in neighborhood poverty reduced stress to levels equivalent to those of individuals above the poverty line. Community investments and residential mobility opportunities can be offered in tandem to improve communities for those who wish to remain and provide flexibility for individuals and families seeking new communities. These poverty reduction measures may promote resiliency among higher-level systems, allowing lower-level systems to adapt to stress.
Accessible and equitable healthcare
Accumulating research has documented the impact of biases and discriminatory behaviors by healthcare providers on patients’ physical and mental health. Patients who have low SES (Arpey et al., Reference Arpey, Gaglioti and Rosenbaum2017; Woo et al., Reference Woo, Ghorayeb, Lee, Sangha and Richter2004), belong to a racial/ethnic minority group (Hoffman et al., Reference Hoffman, Trawalter, Axt and Oliver2016; Miconi et al., Reference Miconi, Li, Founfelker, Santavicca, Cénat, Venkatesh and Rousseau2020), are LGBTQ+ (Cahill & South, Reference Cahill and South2002; Willging et al., Reference Willging, Salvador and Kano2006), are immigrants (Hacker et al., Reference Hacker, Anies, Folb and Zallman2015), are experiencing serious mental illness (Kaufman et al., Reference Kaufman, McDonell, Cristofalo and Ries2012), or have obesity (Phelan et al., Reference Phelan, Burgess, Yeazel, Hellerstedt, Griffin and van Ryn2015) experience barriers to care, as well as biased treatment from providers. The expectation of insufficient care may cause distress or mistrust in healthcare settings, and overall poorer mental health (Phelan et al., Reference Phelan, Burgess, Yeazel, Hellerstedt, Griffin and van Ryn2015). Bias exhibited by providers has been shown to elicit identity and stereotype threat, which can cause distress and, in the long term, have been linked to depression and anxiety (Burgess et al., Reference Burgess, Warren, Phelan, Dovidio and van Ryn2010; Eliacin et al., Reference Eliacin, Matthias, Cunningham and Burgess2020; Phelan et al., Reference Phelan, Burgess, Yeazel, Hellerstedt, Griffin and van Ryn2015). For these reasons, we propose that equitable and accessible healthcare, including mental health services, would reduce significant sources of inequality and promote societal resilience.
These biases and barriers are not only present in medical settings focused on physical health, they also exist within mental healthcare settings. Biases from mental health providers, and the structure of the mental health system itself, contribute to worse mental health outcomes for patients (Eliacin et al., Reference Eliacin, Matthias, Cunningham and Burgess2020; Merino et al., Reference Merino, Adams and Hall2018). Misinterpretation of patients’ symptoms due to differences in culture and lived experience, a lack of education on specific issues facing different groups, as well as microaggressions committed by providers, may impact diagnosis as well as adherence to and efficacy of treatment (Merino et al., Reference Merino, Adams and Hall2018). Additionally, accessing treatment can be difficult for marginalized groups. Previous work found that patients’ SES and race predict providers’ decisions to take on new patients, with middle-class and White patients being the primary receivers of care (Kugelmass, Reference Kugelmass2016). Additionally, even when patients find treatment, there can still be barriers to successful patient-therapist interactions. Individuals who identify as LGBTQ+, especially those living in rural or underserved areas, may encounter providers who may not have specific training in issues related to their identity, leading to worse therapy outcomes (e.g., Willging et al., Reference Willging, Salvador and Kano2006).
Research examining the effects of the COVID-19 pandemic largely documents that the effects of biases in the healthcare system on mental health have persisted and, in some cases, been amplified. In the United States, as already mentioned, Black and Latino populations have been hit especially hard, with mortality rates much higher than those of White Americans, leading to three-to-four times larger reduction in life expectancy for Black and Latino populations (Andrasfay & Goldman, Reference Andrasfay and Goldman2021). This disparity in health outcomes has led to heightened mental health concerns. Black Americans have reported experiencing increased distress due to the heightened impact of COVID-19 on Black communities (Sneed et al., Reference Sneed, Key, Bailey and Johnson-Lawrence2020), especially among those who already held the belief that Black Americans face racial discrimination in health settings (Cobb et al., Reference Cobb, Erving and Byrd2021). Similarly, previously discussed research found that Chinese Americans have experienced an increase in perceived health discrimination, which was associated with poorer mental health (Cheah et al., Reference Cheah, Wang, Ren, Zong, Cho and Xue2020). Many LGBTQ+ youth, who are already at a higher risk of mental health disorders, lost access to mental health services provided in schools when distance learning was instituted (Salerno et al., Reference Salerno, Williams and Gattamorta2020). In an attempt to address the amplification of these preexisting disparities, there has been an increase in the use of strategies thought to decrease access disparities, such as the increased availability of telehealth, and increased Medicare reimbursement for Federally Qualified Health Centers (FQHCs) through the CARES Act to serve marginalized populations (Demeke et al., Reference Demeke, Zilversmit Pao, Clark, Romero, Neri, Shah and Rose2020). However, preexisting divides in access to care have widened. Current research demonstrates that the digital divide between rural and urban access to internet, as well as lower use of telehealth services among Black, Latino, and LGBTQ+ individuals, despite increased funding for FQHCs, may contribute to the widening disparities (Jaffe et al., Reference Jaffe, Lee, Huynh and Haskell2020; Ruprecht et al., Reference Ruprecht, Wang, Johnson, Xu, Felt, Ihenacho, Stonehouse, Curry, DeBroux, Costa and Phillips2021). With the augmentation of these preexisting effects of bias experienced on mental health, it is important to examine ways to address these biases.
To address the aforementioned disparities, it is imperative to first document their existence. Medical providers and government agencies could collect more uniform and comprehensive data on patient demographics, such as race/ethnicity, sexual orientation, gender identity, disability status, and SES (Daugherty Douglas et al., Reference Daugherty Douglas, Dawes, Holden and Mack2015; Maragh-Bass et al., Reference Maragh-Bass, Torain, Adler, Schneider, Ranjit, Kodadek, Shields, German, Snyder, Peterson, Schuur, Lau and Haider2017). Lack of information in this area can prevent institutions from fully understanding the extent of inequalities and disparities. While race/ethnicity is documented in the United States, information on LGBTQ+ identity, disability status, and SES, among other identities, is not as uniformly recorded, if at all (Daugherty Douglas et al., Reference Daugherty Douglas, Dawes, Holden and Mack2015). Better understanding of these biases can provide a foundation for more targeted interventions.
Anti-bias interventions for healthcare providers aim to increase cultural awareness among providers through increasing knowledge, changing attitudes, and increasing comfort level, in order to improve patients’ experiences. Interventions aimed at promoting positive attitudes may involve patient panels discussing barriers to care, whereas interventions aimed at increasing provider comfort may involve strategies like role play and group discussion (Morris et al., Reference Morris, Cooper, Ramesh, Tabatabai, Arcury, Shinn, Im, Juarez and Matthews-Juarez2019). Interventions aimed at increasing knowledge about and comfort working with patients have been successful for providers working with LGBTQ+ and obese populations (Gendron et al., Reference Gendron, Maddux, Krinsky, White, Lockerman, Metcalfe and Aggarwal2013; Morris et al., Reference Morris, Cooper, Ramesh, Tabatabai, Arcury, Shinn, Im, Juarez and Matthews-Juarez2019; Phelan et al., Reference Phelan, Burgess, Yeazel, Hellerstedt, Griffin and van Ryn2015). These interventions have also been successful in increasing racial/ethnic sensitivity among psychiatric mental health nursing students, particularly those whose training occurred in underserved settings and those who were more advanced in their training (Boyer et al., Reference Boyer, Rice, Sorrell and Spurling2019). However, interventions aimed at promoting positive attitudes toward LGBTQ+ and obese populations have been less successful, with recent reviews documenting mixed results (Morris et al., Reference Morris, Cooper, Ramesh, Tabatabai, Arcury, Shinn, Im, Juarez and Matthews-Juarez2019; Phelan et al., Reference Phelan, Burgess, Yeazel, Hellerstedt, Griffin and van Ryn2015). Overall, how we teach providers principles of cultural awareness and humility, particularly in the context of racial/ethnic disparities, cannot be a one-time training. Single or infrequent sessions, unintegrated with practice and without facilitated learning, may be counterproductive for both the clinician and the patients they serve (Murray-Garcia et al., Reference Murray-Garcia, Harrell, Garcia, Gizzi and Simms-Mackey2014). We discuss principles of effective cultural humility interventions in more depth in the next section.
In conclusion, a robust healthcare system with equitable access, expanded telehealth infrastructure, and greater emphasis on reducing bias among providers may provide a foundation for more psychological resilience to disasters. Rampant inequality around access to healthcare among medically underserved groups has perpetuated greater disparities in the impact of COVID-19 on physical and mental health (Mackey et al., Reference Mackey, Ayers, Kondo, Saha, Advani, Young and Kansagara2020). Expanded telehealth can provide greater overall access to healthcare and may reduce access disparities among underserved communities (Menon & Belcher, Reference Menon and Belcher2020; Ortega et al., Reference Ortega, Rodriguez, Maurer, Witt, Perez, Reich and Bates2020). Expansion of telehealth should include infrastructure for increased broadband internet among underserved and rural communities (Bauerly et al., Reference Bauerly, McCord, Hulkower and Pepin2019). Although an emphasis on equity throughout healthcare can promote resilience to future disasters, this cannot occur without an effort to combat systemic racism and promote diversity, equity, and inclusion.
Combating racial injustice and promoting diversity, equity, and inclusion
As highlighted previously in this review, racial/ethnic minority and immigrant populations were disproportionately impacted by the COVID-19 pandemic and previous disasters (Abedi et al., Reference Abedi, Olulana, Avula, Chaudhary, Khan, Shahjouei, Li and Zand2021; Finch et al., Reference Finch, Emrich and Cutter2010). Solutions to the legacy of racism in the United States are needed because the evidence is clear that racial injustice remains a public health issue that weakens these communities’ ability to adapt to disasters (Wrigley-Field, Reference Wrigley-Field2020). At a structural level, these communities can be bolstered against disaster through a policy emphasis on environmental and economic justice, as well as infrastructure investment (Bolin, Reference Bolin2007). In addition, more resources should be allocated to factors that promote community resilience (Xu et al., Reference Xu, Xiang, Proverbs and Xiong2020).
Recognizing that interventions which target racism and discrimination are crucial, an important next question is whether to enact change at the individual or community level. Interventions to change social norms may be more effective when they target group-level processes, such as collective action, which broaden the potential mechanisms to change behavior (Prentice & Paluck, Reference Prentice and Paluck2020). Specifically, experimental evidence shows that participatory processes can shift attitudes toward social authority and justice (Wu & Paluck, Reference Wu and Paluck2020). Beyond community-level interventions, promoting “identity-safe” environments can be accomplished by promoting diverse racial representation and increasing interracial contact across sectors of society. Representation of racial and ethnic minorities provides a cue to members of minority groups that diversity is valued in a given environment, such as a healthcare setting (Burgess et al., Reference Burgess, Warren, Phelan, Dovidio and van Ryn2010). Interracial contact through structured diversity programs has been shown to increase comfort and understanding among different racial groups. In a study of physicians, Onyeador et al. (Reference Onyeador, Wittlin, Burke, Dovidio, Perry, Hardeman, Dyrbye, Herrin, Phelan and van Ryn2020) found that those who had greater and more positive contact with Black individuals before medical school showed less anti-Black bias in residency. Even accounting for previous contact, positive interracial contact during medical school predicted less bias during residency in non-Black physicians.
Education also plays a key role in mitigating the impacts of racism on mental health disparities. Educating children and adults about racism and its effects, changing racist policies, and dispelling racist stereotypes will shift us closer toward more equitable environments (Burgess et al., Reference Burgess, Warren, Phelan, Dovidio and van Ryn2010; Spencer et al., Reference Spencer, Logel and Davies2016). Additionally, universal economic policies, such as the Child Tax Credit, could also contribute to alleviating racial disparities in child and family wealth and health, particularly among Black and Hispanic families (Marr, Reference Marr2021).
To reduce racial injustice in healthcare settings, the lens of cultural humility may be one way to mitigate health disparities. Cultural humility is a concept from medical education that has been applied broadly across healthcare disciplines and settings, including mental health services provision (Tervalon & Murray-Garcia, Reference Tervalon and Murray-Garcia1998). In contrast to the concept of cultural competence, which suggests that an endpoint of cultural mastery may be suitably achieved (Botelho & Lima, Reference Botelho and Lima2020), cultural humility is framed as an ongoing process of continual engagement with three key principles (Tervalon & Murray-Garcia, Reference Tervalon and Murray-Garcia1998): (1) lifelong learning and critical self-reflection, (2) recognizing and challenging power imbalances, and (3) institutional accountability. The first principle, lifelong learning and critical self-reflection, involves an ongoing commitment to listen and learn from individuals and communities that we serve, to recognize and acknowledge what we do not know or understand about their experiences, and seek out knowledge and resources that will improve our ability to provide high-quality care that meets their unique needs and experiences. This process also involves engaging in candid reflection and self-critique to identify biases or actions that perpetuate disparities in care delivery. Lifelong learning and critical self-reflection bring to focus the power differentials that exist in relationships between individual clinicians and patients/families, and between health systems and underserved communities. Recognizing these imbalances, and acting to remedy them in an effort to deliver equitable care, are essential components of the second principle of cultural humility. The third principle, institutional accountability, suggests that the same processes of ongoing learning and self-critique, and remedying power imbalances, must occur on the institutional level, and that institutions must be held publicly accountable for commitments they have made to mitigate health disparities.
Implementing cultural humility principles in the context of COVID-19 has important implications for reducing mental health disparities. One of the immediate repercussions of COVID-19 on mental health service provision was a rapid expansion of telemedicine. Cultural humility is one effective approach that mental health providers used during COVID-19 to successfully build therapeutic alliances with diverse patients (Glass & Bickler, Reference Glass and Bickler2021). Mental healthcare delivered using cultural humility principles may also be important for underrepresented individuals and communities who have experienced trauma during the pandemic. There are long-standing disparities by racial, ethnic, and SES in terms of both exposure to traumatic experiences and access to mental health services to mitigate long-term sequelae of trauma exposure.
Who participates in cultural humility interventions may be important for their success. Previous work has found that cultural awareness training is more successful if it works with the entire workforce, including physicians and nurses as well as less front-facing employees such as administrators and security guards (Bonvicini, Reference Bonvicini2017; Gendron et al., Reference Gendron, Maddux, Krinsky, White, Lockerman, Metcalfe and Aggarwal2013). In order for real progress to be felt, these changes need to be systemic. Another potential way to increase the efficacy of these cultural awareness programs is if, in addition to working with the general workforce, special attention is paid to providers who are most likely to come into contact with underserved populations. Previous work in this area has shown that the barriers to care and biases held by providers cause patients to delay care until it is an emergency (Bonvicini, Reference Bonvicini2017). This means that their first point of contact with a healthcare provider may be in an emergency setting like an emergency room or a phone hotline (Bonvicini, Reference Bonvicini2017; Merino et al., Reference Merino, Adams and Hall2018; Phelan et al., Reference Phelan, Burgess, Yeazel, Hellerstedt, Griffin and van Ryn2015). In addition to this being the first point of contact, this may be a high-stakes situation, with the patient experiencing a life-threatening mental or physical health emergency, so it is especially important that providers have the tools to successfully care for the patient. The larger context of the cultural climate is another aspect that should be incorporated into the training. In contexts like those of the current global COVID-19 pandemic, there are specific stressors that communities are facing, so education about these stressors needs to be incorporated into treatment plans. Recent literature has drawn attention to the importance of providers understanding these specific stressors and the need for compassion (Li & Galea, Reference Li and Galea2020).
An important and highly cited call to action to remedy different forms of bias is to increase the diversity within the medical field (e.g., Bonvicini, Reference Bonvicini2017; Burgess et al., Reference Burgess, Warren, Phelan, Dovidio and van Ryn2010). The presence of providers of similar identities to patients can signal safety to patients and may alleviate stereotype threat and associated stress. However, simply increasing diversity is not enough. Supports need to be in place for underrepresented minority (URM) providers entering and working in the healthcare field, as they are just as likely to experience the same discrimination and biased treatment as patients (Burgess et al., Reference Burgess, Warren, Phelan, Dovidio and van Ryn2010). Prior research has identified strategies for retaining URM providers, such as the use of social networks, visible institutional support through tangible resources, and having administrators who are committed to workplace diversity (Peek et al., Reference Peek, Kim, Johnson and Vela2013). Additionally, there is a need for more research regarding the effects of interventions to decrease healthcare providers’ biases on the mental health of the patients served by these providers. While the presence of these biases has been documented, we still need to examine whether these interventions impact patient mental health. There is a risk that, while these interventions may improve provider knowledge and comfort, these effects are not actually being felt by the patients interacting with these providers. Additionally, the literature in this area emphasizes the need to examine intersectional identities, as the influence of these biases on mental health is likely influenced by all of patients’ identities, such as their gender, race, sexual orientation, and SES (e.g., Anastas et al., Reference Anastas, Miller, Hollingshead, Stewart, Rand and Hirsh2020; Willging et al., Reference Willging, Salvador and Kano2006). While some studies have explicitly examined intersectional identities, this is still a growing area in the literature that needs further exploration.
In conclusion, the COVID-19 pandemic has clearly widened existing racial and ethnic disparities in mental health, highlighting the need for culturally responsive services for affected individuals and communities. Delivering these services with cultural humility principles in mind will likely be beneficial for promoting equity in mental health services access and quality for diverse patients, families, and communities (Melendez Guevara et al., Reference Melendez Guevara, Lindstrom Johnson, Elam, Hilley, McIntire and Morris2021).
Child and family protection
Children are one of the most vulnerable populations to the effects of disasters, as they are highly dependent on their caregivers for survival. According to the family stress model, the effects of disasters on children are often mediated through breakdowns in family processes due to economic hardship (Conger et al., Reference Conger, Rueter, Conger, Crockett and Silbereisen2000; Scaramella et al., Reference Scaramella, Sohr-Preston, Callahan and Mirabile2008). Thus, poverty alleviation measures (cash allowance for children, increasing the minimum wage, food and nutrition assistance, job training programs) may alleviate parental stress and reduce rates of child maltreatment.
While poverty reduction measures can reduce the impacts of financial strain on families, current events have shown that sufficient economic relief is not always feasible (Prime et al., Reference Prime, Wade and Browne2020; Yoshikawa et al., Reference Yoshikawa, Wuermli, Britto, Dreyer, Leckman, Lye, Ponguta, Richter and Stein2020). Additional support through intervention programs for parents are needed. One potential strategy for delivering parenting interventions during dynamic disaster conditions, such as those experienced during the COVID-19 pandemic, is to adapt existing interventions for online delivery. Prior research suggests that some programs, such as Triple P – a brief intervention aimed at reducing child problem behavior and dysfunctional parenting – maintained efficacy when administered online during a randomized controlled trial (Baker et al., Reference Baker, Sanders, Turner and Morawska2017). Another parenting intervention aimed at improving parent-child relationships, The Family Check-up, has also maintained efficacy when administered online and has been shown to increase use of community resources for high-risk families (Danaher et al., Reference Danaher, Seeley, Stormshak, Tyler, Caruthers, Moore and Cardenas2018; Leijten et al., Reference Leijten, Shaw, Gardner, Wilson, Matthys and Dishion2015). Briefer interventions, such as educational campaigns, could also be promising. A number of organizations dedicated to child protection have disseminated online resources to promote child well-being. For example, UNICEF created a series of guides that provide information on positive parenting practices, coping strategies, nonviolent discipline techniques, and budgeting money during financially stressful times (see https://www.unicef.org/coronavirus/covid-19-parenting-tips). These guides can be accessed online and shared with community members who need additional assistance but may not have the time to participate in more extensive programs.
To prevent families from becoming socially isolated, community support groups could be created to provide social support and resources to vulnerable populations. In addition, these community support groups could receive training on identifying and reporting potential signs of domestic violence or child maltreatment in the home.
Prevention programs for prenatal and early-life care are also an important investment to promote resilience before disasters occur. The COVID-19 pandemic was a significant stressor for new and expecting mothers (Preis et al., Reference Preis, Mahaffey, Heiselman and Lobel2020). A recent investigation of a prenatal intervention for expecting mothers experiencing depression has shown that treating maternal depression has the potential to reduce psychopathology across the offspring’s lifespan (Davis et al., Reference Davis, Hankin, Swales and Hoffman2018). Home visiting programs that have served as effective interventions for at-risk and low-resourced recent and expecting mothers have quickly adapted to online formats, yet their efficacy is still to be determined (Williams et al., Reference Williams, Ruiz, Hernandez and Hancock2020). Crisis nurseries can also serve as a resource and support for families needing temporary assistance with childcare during a crisis (DePasquale et al., Reference DePasquale, Parenteau, Kenney and Gunnar2020). Finally, to reduce the impact of the pandemic on child and parental mental health, high-quality and easily accessible mental healthcare must be made available to everyone, including those in underserved, rural communities. This includes investing in telehealth options (Mead, Reference Mead2020). Mental health services may be more effective if they are provided within a unified infrastructure that addresses mental and physical health simultaneously (Bartlett & Stratford, Reference Bartlett and Stratford2021). In sum, high-quality mental healthcare, prevention of childhood adversity and multiple modality interventions will allow a more resilient response to future disasters.
Social cohesion
Social cohesion has been shown to play an important role in a community’s capacity to adapt to and recover from disasters such as wildfires and floods (Townshend et al., Reference Townshend, Awosoga and Kulig2015). Social cohesion has been defined as encompassing mutual trust, support, and assistance among community members, and a shared sense of belonging to the same group (Chan et al., Reference Chan, To and Chan2006). Cohesion can manifest in multiple ways, ranging from social support provided between individuals to volunteering and other forms of civic participation that strengthen communities and the social ties within them.
In the psychobiological literature, social support has been identified as a buffer against stress and a key promoter of resilience (Gunnar & Hostinar, Reference Gunnar and Hostinar2015; Hostinar, Reference Hostinar2015; Parenteau et al., Reference Parenteau, Alen, Deer, Nissen, Luck and Hostinar2020; Perry et al., Reference Perry, Johnson, Hostinar and Gunnar2021). Decades of correlational studies and laboratory experiments with children and adults alike have shown that social and emotional support can reduce the reactivity of the HPA axis and other stress-response systems, resulting in healthier biological profiles (Alen et al., Reference Alen, Sloan, Seeman and Hostinar2020; Hostinar, Reference Hostinar2015). Social support can not only reduce measures of allostatic load (McEwen & Gianaros, Reference McEwen and Gianaros2011), but can protect against the development of mental health problems. For example, Liu et al. (Reference Liu, Zhang, Wong, Hyun and Hahm2020) found that emotional support from family was associated with low levels of depression and PTSD in young adults during COVID-19, a finding consistent with prior research (Lee et al., Reference Lee, Ward, Lee and Rodriguez2021). Furthermore, social support attenuates the impact of chronic stressors such as poverty and inequality on mental and physical health (Chen et al., Reference Chen, Brody and Miller2017; Hostinar & Miller, Reference Hostinar and Miller2019). Given this robust evidence, promoting social cohesion and supportive social ties within communities would promote societal resilience during crises.
A potential barrier to promoting social cohesion during the COVID-19 pandemic is the need to use virus-containing measures such as social distancing, masking, and limits on large gatherings. Thus, programs that promote access to social support and overall social cohesion need to be re-envisioned during pandemics. Digital resources, such as internet applications and video chat, could potentially help reduce negative mental health outcomes (Banskota et al., Reference Banskota, Healy and Goldberg2020). Online support groups based on specific shared characteristics such as LGBTQ+ identity or being a parent may provide individual community members with coping strategies that are tailored for their specific circumstances. For example, some initial evidence indicates that short-term virtual support groups for parents are highly feasible, low-cost, scalable, and may provide an effective strategy to promote the resilience of parents and their children (Luthar et al., Reference Luthar, Kumar and Benoit2019). As already mentioned, expanding access to broadband internet and providing increased assistance to groups who experience difficulties with technology will be necessary for widespread use of virtual social support groups.
A recent review of interventions that were shown to be effective at reducing loneliness before the pandemic and are compatible with social distancing measures identified a few promising candidates (Williams et al., Reference Williams, Townson, Kapur, Ferreira, Nunn, Galante, Phillips, Gentry, Usher-Smith and Gray2021). Educational programs about friendship and social integration, social facilitation software, psychological interventions such as mindfulness meditation, and robotic pets, were the most effective anti-loneliness interventions among those compatible with social distancing measures, although the quality of the trials testing some of these interventions was deemed to be somewhat low (e.g., researchers not blinded to intervention, insufficient details on participant loss to follow-up; Williams et al., Reference Williams, Townson, Kapur, Ferreira, Nunn, Galante, Phillips, Gentry, Usher-Smith and Gray2021). Furthermore, all of this research was conducted before the pandemic, thus the ability of these interventions to reduce loneliness during pandemics and other disasters that prevent social contacts remains to be empirically tested.
In sum, there is robust evidence linking individual perceptions of social support and community-level social cohesion to greater individual and community resilience. However, understanding how to improve access to social support and social cohesion through interventions and during times of crisis necessitates further evidence from high-quality randomized controlled trials and may also require the development of new interventions.
Considering intersectionality to promote societal resilience
In summary, we have reviewed evidence that multiple forms of social and economic inequality undermine the ability of individuals and families to respond to disasters with resilience. An important conclusion is that individuals who are marginalized along multiple dimensions of their identity (e.g., being a low-income woman, or an LGBTQ adolescent with a prior history of multiple childhood adversities) have experienced a more negative impact of the pandemic on their mental health. This is because multiple forms of inequality interact and intersect to shape an individual’s experience and health in unique ways according to their social identity (Bauer, Reference Bauer2014; Lewis & Van Dyke, Reference Lewis and Van Dyke2018), as has been proposed by intersectionality theory (Cole, Reference Cole2009; Crenshaw, Reference Crenshaw1989). Intersectionality describes and considers the combined effects of belonging to multiple social identities (Cole, Reference Cole2009; Crenshaw, Reference Crenshaw1989). Originally used to examine the multidimensional experience of discrimination among Black women, intersectional frameworks have been extended to examine and characterize the experience of groups with multiple marginalized social identities (Cole, Reference Cole2009; Lewis & Van Dyke, Reference Lewis and Van Dyke2018). Intersectionality theory posits the impacts of these identities are not necessarily additive and may combine in unique, complex, and “intercategorical” ways (Bauer, Reference Bauer2014; Cole, Reference Cole2009; McCall, Reference McCall2005). For example, the experience of what it means to be a woman is different across cultures and racial groups, shaped through cultural processes, positionality, social policies, and historical trauma (Bauer, Reference Bauer2014; Cole, Reference Cole2009; Hurtado, Reference Hurtado1989).
Following an intersectional framework, individuals who hold multiple marginalized identities would be predicted to experience greater impacts on mental health during the COVID-19 pandemic. As emphasized, the effects of the pandemic and resulting containment measures did not affect individuals equally (Maestripieri, Reference Maestripieri2021; Purtle, Reference Purtle2020). A clear example is the disproportionate impact of the pandemic on women. Women, particularly mothers of young children, have faced a disproportionate impact of caregiving responsibility (lack of childcare, facilitating remote schooling, and providing care for elders) and were also disproportionately impacted by unemployment (Connor et al., Reference Connor, Madhavan, Mokashi, Amanuel, Johnson, Pace and Bartz2020; Gould & Wilson, Reference Gould and Wilson2020; Laster Pirtle & Wright, Reference Laster Pirtle and Wright2021). Women with lower SES and marginalized racial or ethnic identities experienced greater disadvantage and were overburdened in ways that impacted their well-being and mental health (Connor et al., Reference Connor, Madhavan, Mokashi, Amanuel, Johnson, Pace and Bartz2020; Laster Pirtle & Wright, Reference Laster Pirtle and Wright2021). The compounding effects of these multiple identities suggest the need to allocate additional resources and interventions for those who experience multiple forms of social or economic disadvantage.
The policies we proposed to build the foundational “pillars” of resilience would address these multiple intersecting types of inequality (Figure 2). As discussed, an expansion of economic “safety net” policies that promote economic safety and equity will create greater resilience among communities and families before a disaster occurs, allowing a more robust and adaptive response. Second, accessible and equitable healthcare will create healthier communities and build infrastructure for mental health treatment during and after crises. Third, addressing racial injustice, along with promoting respect for diversity and cultural humility in healthcare settings, may reduce the disparities in how marginalized communities are impacted by disasters. Fourth, strengthening child and family well-being through flexible interventions will allow greater access to support during times of crisis and create a healthy foundation for children’s development. Finally, interventions that promote social cohesion will improve access to social support, a key protective factor against stress. Because resilience is an ecological process that requires healthy systems across all levels of society (Masten, Reference Masten2020), addressing systemic inequalities will enhance both the resilience of individuals and that of society as a whole.
Acknowledgments
We thank Sarah Hudson for her comments on an early draft of this manuscript.
Funding statement
Angelica Carranza was funded by a Eugene Cota Robles Fellowship. Dr Bidwell is supported by the National Center for Advancing Translational Sciences, NIH, through grant number UL1 TR001860 and linked award KL2 TR001859. Dr Hostinar is supported by NICHD grant R01 HD104185. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Conflicts of interest
None.