Headaches are common and debilitating, but frequent use of acute medications may lead to the development of medication overuse headache (MOH). MOH is defined by the International Classification of Headache Disorders-3 (ICHD-3) as headache occurring on 15 or more days per month in the context of 3 or more months of medication overuse. 1 The ICHD-3 definition of overuse varies by agent and is based on expert opinion. Treatment of MOH typically involves withdrawal of overused medications, often with initiation of a prophylactic agent. Reference Carlsen, Rouw and Westergaard2
Adverse childhood experiences (ACEs) are a risk factor for the development of chronic migraine and chronic daily headache, possibly through the over-sensitization of brain pain pathways in early life. Reference Tietjen3 ACEs are defined, in accordance with previous studies, Reference Anda, Tietjen, Schulman, Felitti and Croft4 as any of the following occurring before age 18: abuse (whether sexual, physical, or emotional), neglect (physical or emotional), or exposure to household dysfunction (parental violence or substance abuse, mental illness, criminal behavior, parental separation, or divorce). Some authors argue for the extension of the vulnerable period until age 25 or 30, when the brain has completed development, as well as the inclusion of less well-described ACEs such as bullying. Reference Afifi, Salmon and Garcés5
MOH risk factors are not completely understood but may include depression, anxiety, and obsessive-compulsive disorder, among others. Reference Diener, Holle, Solbach and Gaul6 The type of overused medication is thought to influence risk of MOH, with opioids and barbiturates carrying a higher risk than triptans or NSAIDs. Reference Bigal, Serrano, Buse, Scher, Stewart and Lipton7
Prognostic factors influencing successful medication withdrawal remain unclear. A recent systematic review did not find a correlation between overused medication type and prognosis, while another study suggested that opioid use was associated with more frequent relapse. Reference Tietjen3,Reference Grazzi, Grignani, D’Amico, Sansone and Raggi8 Another study suggested that early life emotional distress and recent stressful events are negative prognostic factors in MOH detoxification. Reference Bottiroli, Galli and Viana9
We examined the frequency of ACEs in patients with MOH and whether the presence of ACEs impacts MOH treatment responsiveness.
Data Collection
We performed a retrospective chart review of new patients assessed at our center from October 2015 to October 2016. Inclusion criteria were (1) any age, (2) underlying diagnosis of chronic daily headache or migraine with superimposed MOH, (3) absence of another headache diagnosis, and (4) at least one follow-up visit within 8 months. The search was run by visit type for the year under study using documented diagnosis of medication overuse headache followed by manual exclusion of charts with other documented diagnoses. We collected data at initial visit and one follow-up, including demographics, headache diagnosis and duration, use of acute and preventative medications, Patient Health Questionnaire 4 (PHQ-4) score, and presence/absence of ACEs, determined through open-ended, sensitive questioning within the context of the initial patient assessment. We documented headache-related disability using the Migraine Disability Assessment (MIDAS). The MIDAS documents headache-related disability over the preceding 3 months, with a maximum score of 270, and a score of 21+ indicating Grade IV or severe disability. We defined response to treatment as change in MIDAS disability grade or 50% reduction in headache days per month.
Statistical Analysis
Deidentified data were entered into Microsoft Excel. No a priori statistical power calculations were conducted. The study used a nonprobability sampling technique which included all patients who met the inclusion criteria specified above. Comparative analyses were conducted using Fisher’s exact test for categorical variables, t-test for parametric continuous variables, and Kruskal–Wallis test for nonparametric continuous variables. Shapiro–Wilk test for normality was utilized. Values are expressed as mean ± standard deviation where applicable. A p-value of 0.05 is considered statistically significant.
Ethics Approval
This study was approved by the Women’s College Hospital Research Ethics Board (2016-0110-E). Being a retrospective chart review of routine clinical care, consent was not required.
Demographic and Baseline Data
We identified 784 new patient visits via Epic electronic medical record search. Among these, 620 were excluded for alternate diagnoses, 39 were excluded due to another concomitant headache disorder such as post-traumatic headache, 25 were excluded due to lack of follow-up, 28 were excluded for <15 headache days per month at initial assessment, and 4 for lack of data regarding ACEs. Sixty-eight patients were included in analysis, of whom 37 (54.4%) endorsed a history of ACEs. Patient characteristics are reported in Table 1. No significant difference was found between patients with and without ACEs for any of these categories (p > 0.05).
Table 1: Patient characteristics
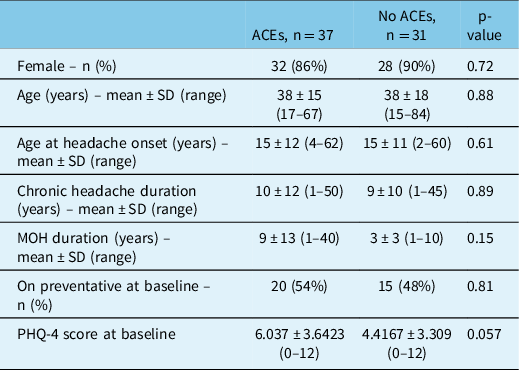
There was no significant difference between those with and without ACEs for baseline MIDAS (90 ± 72 vs 86 ± 18, respectively, p = 0.52) nor headache days per month (26 ± 4 vs 25 ± 4, p = 0.51).
Types of ACEs
Among the 37 patients reporting ACEs, the most commonly reported types were parental divorce (11 patients), followed by emotional abuse and bullying (9 patients each), and sexual abuse and parental substance abuse (8 patients each). Eighteen reported 1 type of ACEs, 11 had 2 different types of ACEs, and 8 had ≥3 types. Given small numbers, we could not perform further analysis as to the effects of different types or numbers of ACEs.
Medication Use
Forty-three percent (16/37) of patients with ACEs overused any opioid at baseline as compared to 25.8% without ACEs (8/31, p = 0.2). There was significantly more non-codeine opioid use in those with ACEs at 32.4% vs 3.2% (OR 14.4, 95% CI 1.7–118.5, p = 0.004) (Table 2).
Table 2: Patient medication use and headache-related disability
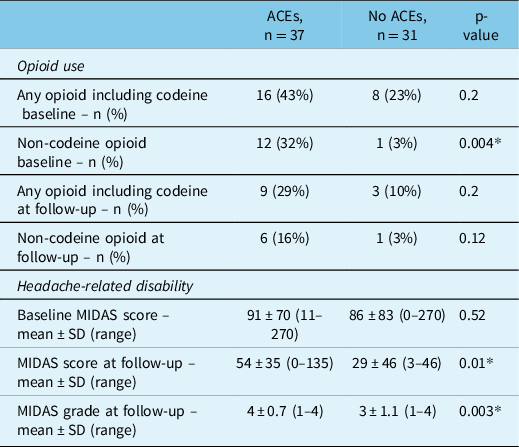
* Statistically significant, p < 0.05.
Intervention
As standard practice in our center, patients receive education, lifestyle and stress management strategies, nutraceutical therapy, adjustment of acute and preventative therapy, and bridge therapy with nabumetone or naproxen 500 mg twice daily for 2 weeks.
Post-intervention
All patients had a follow-up visit, however, 31/68 patients had missing/incomplete follow-up MIDAS outcome data. Statistical comparison of key baseline characteristics between patients with and without missing data did not reveal any significant differences.
At follow-up, 51.4% (19/37) of patients with ACEs versus 22.6% (7/31) of those without ACEs were still overusing medications (p = 0.02).
At follow-up, 16% (6/37) of patients with ACEs versus 3% (1/31) without were still overusing pure opioids (not significant, p = 0.12) (Table 2).
Headache Frequency and Headache-related Disability
At follow-up, there was no difference in average headache days per month between patients with and without ACEs (19.7 ± 8.9 vs 19.1 ± 10.2). Twenty-seven patients had at least a 50% reduction in headache days per month, including 14/35 of those with ACEs and 13/31 of those without (p = 0.87).
However, despite comparable baseline MIDAS scores, patients with ACEs reported a significantly higher MIDAS grade at follow-up, on average Grade 4 compared to patients without ACEs at Grade 3 (p = 0.003). Patients with ACEs also had higher MIDAS scores, on average of 54 ± 30.1 vs 29.4 ± 45.5 (p = 0.01) (Table 2).
Our results confirm the highly debilitating nature of MOH, with patients’ average MIDAS scores well above the severely disabled range. The characteristics that may predict a positive response to treatment unfortunately remain elusive.
We required that patients undergo a follow-up visit in the first 8 months. This may have introduced bias, as patients overusing medications (in particular opioids) may have been less likely to return for a follow-up when instructed to taper and discontinue overused medications. Given the sensitive nature of ACEs, patients with ACEs may have been less inclined to disclose a history of ACEs and/or attend follow-up visits and may therefore have been underrepresented. We assess the presence/absence of ACEs as a standard part of our initial assessment, but we did not use a structured ACEs questionnaire as we have found that these can trigger distress especially in new patients. This lack of structured interviewing may have introduced bias. In future, we hope to perform structured ACEs measurements. The prevalence of ACEs in our study population at 54.4% is however similar to that seen previously in migraine populations. Reference Tietjen3 Despite small sample size, we feel that our study has good internal validity and sheds light on an important aspect of care for migraine patients with ACEs.
Previous studies have found an association between emotional abuse and headaches, and an increasing prevalence of headache in those with a higher number of ACEs. Reference Afifi, Salmon and Garcés5,Reference Tietjen, Karmakar and Amialchuk10 Unfortunately, we were not able to glean any information regarding the different types of ACEs or the impact of multiple ACEs on MOH due to sample size.
We found significantly higher rates of opioid use in patients with MOH and a history of ACEs than in those without ACEs, a particularly salient finding in light of evidence that opioid use is associated with MOH treatment resistance and more frequent MOH relapse rates. Reference Tietjen, Karmakar and Amialchuk10 ACEs are known to increase vulnerability to addiction, possibly through alterations in the developing hypothalamic–pituitary–adrenal axis and mesolimbic dopamine pathways as well as the prefrontal cortex, impacting emotional control. Reference Sinha11
Although both subgroups had some improvement at follow-up, patients with ACEs tended to improve less, and reported a significantly higher MIDAS score and grade, despite similar average headache days per month between groups. This suggests that patients with ACEs may cope differently with their headaches and experience more disability.
Greater than half of our study participants with MOH reported ACEs. These patients were more likely to overuse opioids at baseline. MIDAS score and grade improved less in patients with ACEs at follow-up, despite no significant difference in headache days per month or 50% reduction in headache days per month. Future work will include examining longer follow-up data and whether different numbers or types of ACEs have different prognoses. Trauma-informed care and a focus on the whole person, rather than just the overused medication, may provide better long-term outcomes for this patient population.
Acknowledgements
The authors would like to thank Ann-Marie Surmava for her assistance with study design and data analysis, Dr. Manav Vyas for review of data analysis, and Ian Stanaitis for his tremendous support in reviewing research data and the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
Dr. Christine Lay participated in advisory boards for Lundbeck, TEVA, Eli Lilly and Novartis, and received research grants from Lundbeck and TEVA however, fees were submitted to Women’s College Hospital, Department of Medicine. Dr. Ana Marissa Lagman-Bartolome participated in advisory boards for Lundbeck, TEVA and Miravo, and received research grants from Lundbeck, TEVA and Amgen however, fees were submitted to Women’s College Hospital, Department of Medicine and Hospital for Sick Children. Valerie Lawler participated in advisory boards for Eli Lilly and Lundbeck. Dr. Suvendrini Lena participated in advisory boards for Allergan/Abbvie, Eli Lilly, Novartis, and Teva. Dr. Claire H. Sandoe participated in advisory boards for Lundbeck, Eli Lilly, Abbvie, Miravo, and Novartis.
Statement of Authorship
Conception and design of study: CHS, VL, SL, AMLB, CL.
Acquisition of data: CHS.
Analysis and/or interpretation of data: CHS, VL, SL, AMLB, CL.
Drafting the manuscript: CHS.
Revising the manuscript critically for important intellectual content: CHS, VL, SL, AMLB, CL.
Approval of the manuscript to be published: CHS, VL, SL, AMLB, CL.




