1. Introduction
Tobacco users are constantly exposed to the risk of noncommunicable diseases, leading to premature mortality among the risk population. Globally, eight million deaths are reported every year due to tobacco use [Reference Tselengidis, Dance, Adams, Freeman and Cranwell1]. Consequently, smokeless tobacco and cigarette smoking contribute to six and five percent disability-adjusted life years (DALYs), respectively [Reference Rezaei and Farzadfar2]. However, the prevalence of tobacco use has been decreasing globally since 1990 [Reference Rezaei and Farzadfar2], and most tobacco users live in low-middle-income countries (LMICs) [Reference Smith and Malone3]. India is also no exception compared with other LMICs; for example, Global Adult Tobacco Survey-2 (GATS) highlighted that nearly 29 percent of adults (42% male and 14% female) aged 15 years and above use some form of tobacco [Reference John, Sinha, Munish and Tullu4]. In addition, the fourth round of the National Family Health Survey (NFHS-4), conducted in 2015-16, showed that approximately 46% of males were tobacco users [Reference Islam, Saif-Ur-Rahman, Bulbul and Singh5]. Consequently, one million deaths were reported in India, and one-sixth of the world’s deaths were due to tobacco use [Reference Sivapuram, Nagarathna, Anand, Patil, Singh and Nagendra6]. The future prediction indicates that tobacco-related mortality and morbidity rates will substantially increase by 2050 and beyond [Reference Shahbabu, Dasgupta, Sarkar and Sarkar7].
Various tobacco products are available, which can be smoked, such as cigarettes, or chewed, such as different smokeless tobacco products. Furthermore, smoked tobacco includes cigars, cigarettes, bidis, hookah, pipes, and chillum, while smokeless tobacco includes khaini, gutka, pan with tobacco, and betel nut. Cigarettes are the most commonly consumable tobacco product worldwide [Reference Ng, Freeman and Fleming8]. In the Indian scenario, 2015-16, NFHS data revealed that cigarette smoking (32%) was dominant among men tobacco users, followed by chewing tobacco (2%) and cigar (0.23%). In addition, thirty percent of men use at least one tobacco product, eight percent are dual tobacco users, and two percent are polytobacco users [Reference Chen, Millett and Filippidis9].
Considering the socioecological differentials in tobacco products, including individual-level socioeconomic and contextual determinants, place of living is always concerned in terms of disparity in health issues due to cultural lag. People residing in rural areas are always disadvantaged regarding education, health awareness, healthcare utilization, etc. Extensive literature is available on rural-urban differentials in the use of tobacco products [Reference Gupta, Yadav and Anand10–Reference Roberts, Doogan and Kurti12]. The substantial rural-urban gap in the prevalence of current tobacco use was highlighted in a study conducted in India by Singh and Ladusingh that showed 52% prevalence in rural arears compared to 38% in urban ones [Reference Singh and Ladusingh13].
Many countries have adopted different policies to reduce tobacco use. However, quitting tobacco is quite a complex process, although some studies have tried to emphasize this issue [Reference Foulds, Gandhi and Steinberg14–Reference Borland, Partos, Yong, Cummings and Hyland16]. Healthcare providers are the key player in the cessation of tobacco use. With understanding of the globalization of the tobacco epidemic, the World Health Organization (WHO) took the initiative framework convention on tobacco control (WHO, FCTC) which was the first international treaty on tobacco control, participated by 181 countries held in 2003 [Reference Chung-Hall, Craig, Gravely, Sansone and Fong17]. The prime objective of the convention was to reduce the demand and supply of tobacco products, to control tobacco use. In this regard, the WHO introduced MPOWER measures, which is an effective measure to prevent tobacco use. The MPOWER packages provide six essential parameters to control the tobacco epidemic. In addition to that, it (MPOWER) indicates the following: M stands for monitor tobacco use, P stands for protecting people from tobacco smoke, O stands for offering help to quit, W stands for warning about the dangers of tobacco, E stands for enforcing bans on tobacco advertising, promotion, and sponsorship, and R stands for raising taxes on tobacco products [18]. GATS data provide comprehensive measures of MPOWER in the Indian scenario. In addition, a study highlighted that concrete action still needs to be addressed if the noncommunicable disease global voluntary target of a 30% reduction by 2025 in the prevalence of tobacco use among the 15 years and above population is to be achieved [Reference Song, Zhao and Palipudi19].
India is also not behind legislating tobacco policies and programs to control the tobacco epidemic in the country. The government of India came up with the cigarette act in 1975 to regulate the production, supply, and distribution of smoking tobacco [Reference Ruhil20]. Further, one major decision was taken in 1992, as tobacco in all dental products was banned [Reference Dhot21]. Furthermore, a significant act was introduced in 2003 called the Cigarettes and Other Tobacco Products Act (COTPA) with the prohibition of advertisement and regulation of trade and commerce, production, supply, and distribution of tobacco products in India [Reference Kaur and Jain22]. In addition, the act provides the provision restriction of smoking in public places, prohibition of advertisements of tobacco products, prohibition of the sale of tobacco products to minors aged below 18 years, ban on the sale of tobacco products within 100 yards of educational institutions, and mandatory display of pictorial health warning on the tobacco products. An evolutional study for the COTPA act was carried out in 2019 for the urban area among educational institutions and points of tobacco sales. The study revealed that, overall, complying with the norms of the COTPA act in urban areas, especially in Shimla, no tobacco-selling vendors were found selling tobacco to minors [Reference Chaudhary, Thakur and Chauhan23].
Even though several research studies have been done on tobacco consumption concerning different characteristics such as age, gender, place of residence, and media exposure, only a few studies had explored the current status of tobacco consumption with their cessation efforts made in the Indian context [Reference Singh and Ladusingh13, Reference Barik, Rai, Gorain, Majumdar and Chowdhury24]. With the increasing awareness and various other interventions, the variety of tobacco shows a crest and trough in consumption status. This study estimates the prevalence of a variety of tobacco concerning their consumption and cessation attempts among adults in India.
Consequently, there was a reduced roll tobacco use among adult men, although some socioecological and contextual factors still affect tobacco use in rural and urban areas among men. So, with the latest demographic and health survey data, this paper analyzes the prevalence, determinants, and cessation of tobacco use among men in India and focuses at the key strategies to address their dilemmas of increased use vis-a-vis cessation in various contexts.
2. Material and Methods
2.1. Data Source
The study utilized information from India’s latest National Family Health Survey-5 (NFHS-5) data. The NFHS is a nationally represented district-level survey conducted for all 36 states and union territories (UTs). The nodal agency for conducting this survey is the International Institute for Population Sciences (IIPS), Mumbai. The survey is cross-sectional and adopted a systematic, two-stage cluster sample of the household. The NFHS survey provides comprehensive information on several emerging issues, including family planning, education, nutrition, health problems, and health-related behaviors. This study includes 988,713 adult men aged 15 years and above, including 93,144 men aged 15-49. In addition, all the men’s interviews were done in the households selected for the state module among those aged 15 to 49. Additional information was collected from men 15 years and above at the district level.
2.2. Dependent Variables
The dependent variable for this study is current tobacco use by adult men in India. The response was recorded by asking the question “does currently smoke or use tobacco in any form?” The response was recorded as either “yes” or “no” where “no” is considered as a reference category in the analysis Further, to estimate the prevalence of tobacco use by adults by selected sociodemographic parameters, we used “cigarette smoking,” “bidi smoking,” and “smoke five or more cigarette/bidi” as dependent variables. Moreover, to estimate the prevalence of adults who had tried to quit smoking, we used “tried to stop smoking or to use tobacco in any other form in the past 12 months” and “advised to quit smoking or using tobacco in any form” among those who visited a doctor or other healthcare provider in the past 12 months as dependent variables. Lastly, we also used secondhand smoke as a dependent variable by asking “does anyone present when someone (other than themselves) was smoking in the home or elsewhere in the past 30 days?”
2.3. Covariates
The covariates for this study are age (15-19, 20-34, 35-49, 50-64, and 60 and above), level of schooling (no schooling, <5 years complete, 5-7 years complete, 8-9 years complete, 10-11 years complete, and 12 or more years complete), the religion of the household head (Hindu, Muslim, and others), caste/tribe of the household head (scheduled caste, scheduled tribe, other backward class, and others), and wealth quintile (lowest, second, middle, fourth, and highest).
2.4. Statistical Measures
The bivariate analysis was used to estimate the prevalence of tobacco use, quitting tobacco, and secondhand smoke associated with selected background variables and states/UTs in India. A multivariate logistic regression model was adopted to estimate the adjusted effect of various socioeconomic factors on different types of tobacco use (any tobacco use, smoking cigarette, and smoking bidi). The equation for multivariate logistic regression is given below.
The above regression equation portrays the log odds of probability of consuming any type of tobacco or smoking various tobacco products under the effect of various socioeconomic and behavioral drivers of tobacco use/smoking, i.e.,
![]() . In addition, to check the association between dependent and independent variables, a chi-square test has been performed.
. In addition, to check the association between dependent and independent variables, a chi-square test has been performed.
Further, to see the extent of clustering in tobacco consumption at various levels, we have used multilevel random and fixed effect binary logistic regression model and calculated the ICC values. A multilevel logistic regression model with a random intercept was used to understand clustering in any tobacco use within PSU or “community” and households [Reference Rabe-Hesketh and Skrondal25]. The application of the multilevel modeling was justified by the hierarchal structure of the survey, where men were nested within household and the household were nested within PSUs. In a preliminary analysis, a “baseline” or intercept model was examined only to assess the extent of the dependent variable’s variation between “communities” and the advisability of using a multilevel modelling strategy. In multilevel analysis, a systematic model building procedure was adopted to finalize the key covariates to be included in the model. Finally, the model included sociodemographic and economic variables such as respondents’ age, educational attainments of the respondents, place of residence, caste affiliation, household wealth, and the religious affiliation of the respondents The following is the equation of the model:

where Yijk is the current tobacco consumption for individual i in the household j in PSU k in state l. In addition, α = constant, Xijkl, Zjkl, Wkl, and Ul are the vectors of variable; β, γ, δ, and φ are the regression coefficients; and r 0l, s 0kl, d 0jkl, and e 0ijkl are the residuals at the individual level, state level, PSU level, and household level, respectively.
The outcomes of the multilevel mixed effect logit regression have been done at 95% confidence interval to show fixed effect of the explanatory variables. Further, to show the random effect, intraclass correlation coefficient (ICC) was computed at the state level, PSU level, and household level. The following is the equation of the ICC:

where ICC is the intraclass correlation coefficient and VARn is the variance at the nth level of regression.
All the analyses were performed using STATA version 17 software. Further, map was drawn using GIS version 10.2.
3. Results
The prevalence of tobacco consumption among men aged 15 and above who live in rural and urban areas is presented in Table 1. The study includes 988,788 men aged 15 and above years. The overall prevalence of tobacco consumption (any form) was 38%, which varies from 29% in urban areas to 43% among men living in rural areas. Tobacco uses are more prevalent in rural areas than in urban areas. The prevalence of tobacco use increased along with age; the prevalence is the highest in the age category 50-64 years across rural and urban areas. Men without schooling had the highest prevalence (65%) of tobacco use in rural areas. The prevalence shows a declining trend as the level of schooling increases in rural and urban areas. Men who belong to the schedule tribe category and reside in rural areas had the highest prevalence of tobacco consumption (53%). Also, the predictor wealth quintile shows a similar pattern. Men from the lowest wealth quintile had the highest prevalence of tobacco consumption (58%), while it was the lowest among men belonging to the highest wealth quintile (21%).
Table 1: Percentage of the population age 15 years and over who currently use any tobacco, according to background characteristics, India, 2019-21.

Figure 1 shows the prevalence of tobacco consumption among men aged 15 and above by their place of residence (rural, urban, and total) across the states/UTs in India. Among all Indian states and union territories (UTs), tobacco consumption was the highest in northeastern states, such as Mizoram (73%) has the highest percentage of tobacco users of any state/UT, followed by Andaman and Nicobar (59%), Manipur and Meghalaya (58% each), Tripura (57%), Assam and Odisha (52%), and Arunachal Pradesh (50%). In addition, Chandigarh, Punjab, Puducherry, Kerala, and Goa have the lowest tobacco use prevalence (less than 20%).

Figure 1: Percentage of the men age 15 years and above who currently use any tobacco by urban, rural, and total.
District-level prevalence of tobacco consumption (any form of tobacco) among men aged 15 and above years shown in Figure 2. Results show that most of the districts of southern states, such as Telangana, Andhra Pradesh, and Tamil Nadu, found a lower prevalence of consumption (less than 20%). Moreover, northeastern states reported higher tobacco consumption (50% and above) in almost all the districts. The higher prevalence (50% and above) of tobacco consumption was reported in almost all the districts of Mizoram, Assam, Meghalaya, and Arunachal Pradesh.

Figure 2: Proportion of men with tobacco consumption age 15 years and above at the district level.
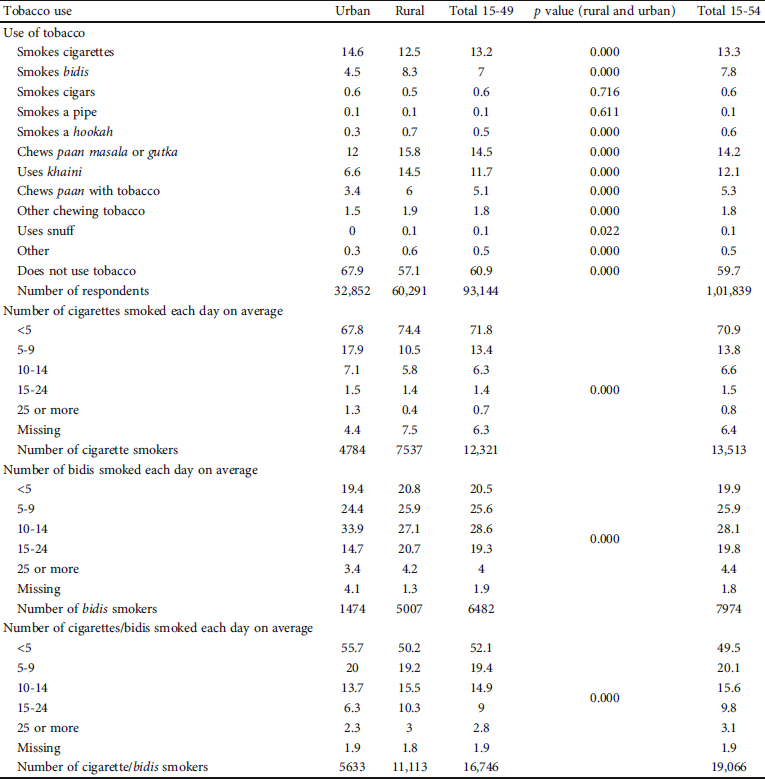
Table 2 describes tobacco smoking in different forms by men aged 15-49 and 15-54 years in rural and urban India. From the result, cigarette smoking (13%) and bidi smoking (7%) were more frequent than other tobacco products, such as paan masala or gutka, khaini, and bidis, in rural and urban areas. Bidi smoking (8.3%) and the use of khaini (14.5%) were greater in rural areas than in urban areas. Around seven percent of cigarette smokers from urban areas smoke 10-14 cigarettes per day, and 18% smoke 5-9 cigarettes daily. Similarly, a significant proportion of the men (21%) who live in rural areas smoked 15-24 bidis per day. Moreover, among tobacco users, 50% smoke an average of less than five bidi/cigarette per day in rural areas while 56% in urban areas. Also, 15% of men use an average of 10-14 bidi/cigarette per day among 15-49 years, and at the same time, there was not much difference in the tobacco smoking in the age category 15-49 and 15-54 years.
Table 2: Percentage of men aged 15-49 and men age 15-54 by their use of tobacco and percent distribution of those who smoke cigarettes or bidis by number of cigarettes/bidis smoked each day on average, India, 2019-21.
The prevalence of any kind of tobacco use, smoking cigarette, and bidi five or more per day by their background characteristics is presented in Table 3. The consumption of any form of tobacco and smoking five or more cigarettes/bidis was the highest in the 35-49 years of age group (51% and 57%, respectively) than the smokers of other age categories. Results found a significant difference (10%) among the users of tobacco who consume any kind of tobacco live in rural areas than the urban areas. According to the years of schooling, men who had completed 12 or more years of schooling reported a lower prevalence of tobacco use, while it was the highest among those who never visited the school or had less than five years of schooling. Tobacco consumption was the highest (52% who consume any form of tobacco) among the men belonging to the scheduled tribes. Also, lower consumption of tobacco in any form (22%), cigarette smoking (11%), and bidi smoking (35%) was found among the men who have their place in the highest wealth quintiles. However, tobacco consumption was the highest among the men who belong to the lowest wealth quintile.
Table 3: Percentage of men aged 15-49 who use any kind of tobacco and percentage who smoke cigarettes or bidis and, among those who smoke cigarettes or bidis, the percentage who smoke 5 or more cigarettes or bidis each day on average, by background characteristics, India, 2019-21.

Table 4 presents the results of adjusted odds ratios from logistics regression for any tobacco use, smoking cigarette, and smoking bidi among men aged 15-49 years with selected background characteristics. Among the men aged 35-49 years, the odds were significantly higher for consuming any form of tobacco (AOR: 7.36, CI: 6.72-8.05), smoking cigarettes (AOR: 2.56, CI: 2.23-2.94), and smoking bidi (AOR: 7.12, CI: 4.75-8.82) compared with their counterparts. Moreover, men who live in urban areas are more likely to consume any form of tobacco, smoke cigarette, and smoke bidi compared with rural residents. Educational attainments (years of schooling) significantly affect tobacco use. Men with 12 or more years of schooling were significantly less likely to use tobacco, cigarettes, or bidi compared to illiterate and those with less than five years of schooling. Men from the scheduled tribes’ caste were more likely to consume any form of tobacco (AOR: 1.15; CI: 1.04-1.26) than men from other caste categories. For the predictor wealth quintiles, it is observed that the probability of consuming any form of tobacco, smoking cigarette, and smoking bidi declines with the rising wealth status.
Table 4: Unadjusted and adjusted effect of any tobacco use, smoking cigarette, and smoking bidi by background characteristics among 15-49 years of the men in India.
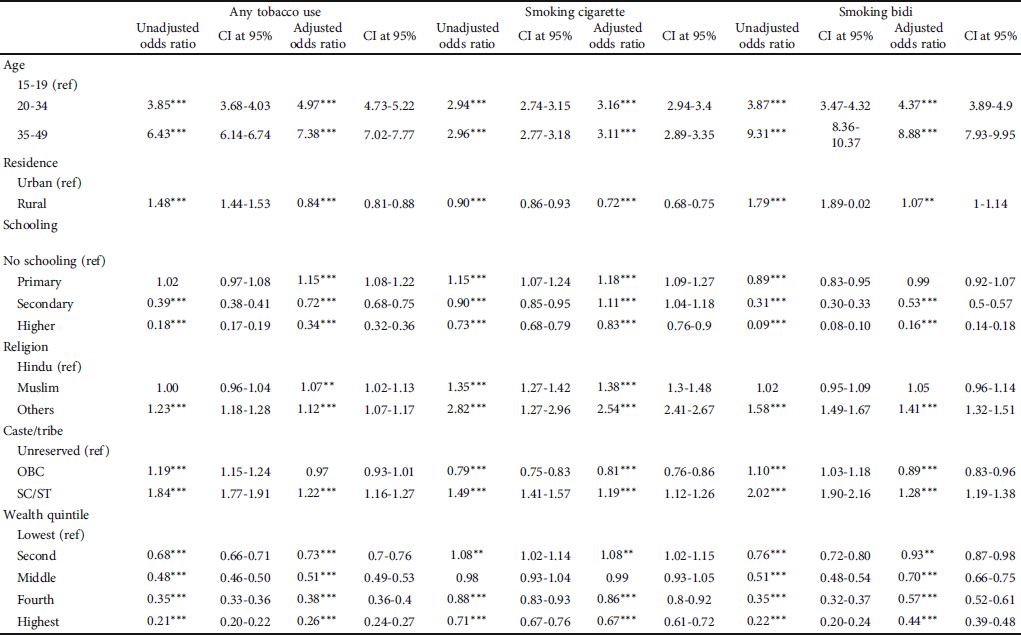
*** Significant at p value ≤ 0.005,
** significant at p value ≤ 0.05.
As presented in Table 5, the null model explained 15% of the clustering of tobacco use at the state level, while 29% and 38% of the clustering at the PSU and household levels, respectively. While considering the full model with a set of covariates as fixed effects, the clustering in tobacco use has increased significantly at the household level (48%). There has not been substantial changes at the PSU and household levels. Analyzing the fixed effects of various covariates, it is evident that men between the ages of 20-34 and 35-49 had greater adjusted odds ratios (AOR = 9.70, CI 8.9-10.5) for any tobacco use than those between 15 and 19 years. In terms of education, men with greater levels of education had lower chances (AOR: 0.18, CI: 0.16-0.19) than males without any education. Those from schedule caste and tribes had higher tobacco consumption as compared to those from non-SC/ST and non OBC (AOR: 1.40, CI: 1.30-1.50).
Table 5: Multivariable multilevel random and mixed effect logistic regression model for any tobacco use among men in India, NFHS-5.


*** Significant at p value ≤ 0.005.
The percentage of men who made cessation efforts for quitting tobacco received advice from the healthcare provider and had exposure to secondhand smoke by selected background characteristics described in Table 6. Men who were in the age category 35-49 years attempted to stop consuming tobacco (30%). However, 58% of men who visited the hospital were advised to quit tobacco in the last 12 months, and 62% were exposed to secondhand smoke. There were not many differences in the percentage of cessation efforts made by men in rural and urban areas. Barely 25% of illiterate men tried to stop consuming tobacco in the last 12 months. Though 27% of men tried to quit tobacco in the last 12 months and 69% of men are exposed to secondhand smoke, 51% of men who received advice for quitting tobacco and visited the hospital in the last 12 months belong to the lowest wealth quintile.
Table 6: Percentage of men aged 15-49 who tried to stop tobacco, who were advised to quit tobacco, who visited a doctor, and who were exposed to secondhand smoke, by background characters, India, 2019-21.

Men aged 15-49 years who had tried to stop using any form of tobacco had been advised to quit tobacco and were exposed to secondhand smoke by states and union territories (UTs) in India, as shown in Table 7. Overall, 30% of men had tried to quit tobacco, 62% were exposed to secondhand smoke, and 54% of men who were advised to quit tobacco visited the hospital in the last 12 months. The highest percentage of men were reported for quitting tobacco in Manipur (48%), followed by Odisha (46%), Uttarakhand (45%), and Gujarat (41%). Most of the men who visited healthcare providers received advice to quit tobacco found in the states Punjab (82%), Haveli and Daman Diu (75%), and Andhra Pradesh (68%). Also, exposure to secondhand smoke among men was found to be the highest in Mizoram (91.5%), Delhi (81.4%), and Rajasthan (80%).
Table 7: Among men age 15-49 who currently use any kind of tobacco, percentage who have tried to stop using any tobacco and, among current users of tobacco who visited a doctor or other healthcare provider in the 12 months preceding the survey, percentage who were advised to quit any form of tobacco and percentage who were exposed to secondhand smoke.

4. Discussion
The latest dataset from the National Family Health Survey-5 has been utilized to study the prevalence of tobacco consumption, types of tobacco use, and cessation of any form of tobacco consumption among men aged 15 and above years in India. With 275 million tobacco consumers, India is the second-largest tobacco consumer in the world after China [Reference Hasan, Quazi, Sarangapani and Alam26]. However, there is a substantial decline in the prevalence of tobacco use among adults, but still, adequate socioeconomic inequalities are found in the prevalence of tobacco use among adults. The result from the study reveals that the overall prevalence of tobacco consumption (any form) was 38%, while the prevalence of any form of tobacco was 29% in rural and 43% in urban areas. Cigarette smoking and bidi smoking were more frequent than other tobacco products, such as paan masala or gutka, khaini, and bidis, in rural and urban areas. Bidi smoking and the use of khaini were more significant in rural areas than in urban areas. Men living in urban areas are more likely to consume tobacco, smoke cigarettes, and smoke bidi than rural residents. There were slight differences in the percentage of cessation efforts made by men in rural and urban areas. The prevalence of tobacco is the highest in the age category 50-64 years across rural and urban areas. For instance, rural-urban differentials in tobacco use have been documented well in the pieces of literature [Reference Shahbabu, Dasgupta, Sarkar and Sarkar7, Reference Gupta, Yadav and Anand10, Reference Ozga, Romm and Turiano27].
There is a subsequent reduction in tobacco use among adult men 15 years and above. However, it is still prevalent in many countries, and India is no exception. Relatively, death due to tobacco consumption (8 million deaths per year) appears to receive less attention globally. In 2012, a study conducted for 13 low-middle-income countries reported that 769 million are tobacco users [Reference Palipudi, Gupta and Sinha28]. In addition, another study estimated that 14 countries from the GATS survey highlighted 852 million are tobacco users, including 275 million in India [Reference Giovino, Mirza and Samet29]. A recent study has reported that tobacco consumption among men has risen by around 40 million. The estimates showed that tobacco consumption has increased from 1.050 billion in 2000 to 1.093 billion in 2018 [Reference Tripathy30]. India is more complex because of various smoking and smokeless tobacco products. Our study found that men who belong to the schedule tribe category and reside in rural areas had the highest prevalence of tobacco consumption. Tobacco consumption was the highest (52% who consume any form of tobacco) among the men belonging to the scheduled tribes. Men from the scheduled tribes’ caste were more likely to consume tobacco than men from other caste categories. Compared with other countries, India has the second largest country in tobacco production after China, and many of these tobacco products are manufactured in the cottage and small industries in India [Reference Gupta and Ray31].
Young age and peer pressure are the dominant risk factors for tobacco consumption. Among all tobacco consumption, smoking is persistent, where adolescence phase is a very potential stage to develop this habit. A study by Kamble et al. among 400 college students in Delhi found that 23% were ever smoked, 16% were current smokers, and most were adolescents [Reference Kamble, Acharya, Jethani, Chellaiyan, Singh and Chaku32]. The result from our study pointed out that the consumption of any form of tobacco and smoking five or more cigarettes/bidis were the highest in the 35-49 years of age group (51% and 57%, respectively) than the smokers of other age categories. Also, the odds were significantly higher for consuming any form of tobacco, smoking cigarettes, and smoking bidi compared with their counterparts. A study by Singh and Kashyap suggested that most tobacco users are young and mainly belong to the northeastern states [Reference Singh and Kashyap33]. In addition, initiation of tobacco consumption at an early age leads to mature and regular tobacco consumption at later ages and results in various severe health issues. Plaipudi et al. reported higher consumption of tobacco use found in the age group of 45 to 64 years [Reference Palipudi, Gupta and Sinha28].
Although the age at initiation and the age at quitting tobacco consumption have been interesting issues for policymakers [Reference Kumar, Patel, Chauhan and Gupte34], the cessation of tobacco consumption is the prime goal for many countries to control the tobacco epidemic. Further, it is well documented that aggressive tobacco cessation may result in several benefits to achieving the targets. In addition, tobacco cessation is important and strengthens the program to reduce tobacco consumption, which is integral to cultural practice [Reference Slama35]. Findings from our study expose that among all Indian states and union territories (UTs), tobacco consumption was the highest in northeastern states. Almost similar findings were found in a previous study [Reference Gupta, Yadav and Anand10]. Overall, 30% of men had tried to quit tobacco, 62% were exposed to secondhand smoke, and 54% of men were advised to quit tobacco when they visited the hospital in the last 12 months. However, it is a challenging and complex process to complete cessation of tobacco consumption among current users. Due to higher reversal rate in the process of behavior change where a person passes through stages of precontemplation, contemplation, preparation, action, and confirmation, an extraordinary effort is required to promote it and prevent the reversal. There may be many benefits of quitting tobacco before age 50, as they would reduce almost half of the risk of dying in the next 15 years [Reference Murthy and Saddichha36]. Intensive promotion and preventive initiatives have been adopted internationally and nationally to combat the tobacco epidemic. In this arena, 181 countries came into a single platform where WHO (World Health Organization) organized a framework for tobacco control (FCTC) [Reference Yadav, Singh and Yadav37]. Reduction in smoking cigarettes and smokeless tobacco remained the main priority of the convention. The government of India is also not behind in implementing such policies, making lots of effort to control the current situation where healthcare providers are key drivers. In 2003, the Indian government created a Cigarettes and Other Tobacco Products Act (COTPA) to reduce tobacco use through taxation, pictorial depiction of tobacco products, and other measures [Reference Kaur and Jain22]. A recent study reported that 35% of tobacco users were in 2009-10, reduced to 27% in 2016-17 [38]. Reduction in tobacco use may result from measures adopted by India’s government.
This study identified that men from the lowest wealth quintile had the highest prevalence of tobacco consumption, while it was the lowest among men belonging to the highest wealth quintile. Tobacco consumption was the highest among the men who belong to the lowest wealth quintile. The chance of consuming any form of tobacco, smoking cigarette, and smoking bidi declines with the rising wealth status. Twenty-seven percent of men tried to quit tobacco in the last 12 months, 69% of men are exposed to secondhand smoke, and 51% of men who received advice for quitting tobacco belongs to the lowest wealth quintile. This may be due to the better advantages of health education on the upper wealth quintile than lower wealth quintile [Reference Prinja and Kumar39]. Contextual effects can explain the higher prevalence of smoking in urban areas. The “contextual effect” emphasizes the significance of the social and demographic composition of people’s lives in urban areas [Reference Diez Roux40]. Some previous studies found that higher education leads to lower tobacco consumption [Reference Singh, Schensul and Kashyap41–Reference Biswas, Syiemlieh, Nongrum, Sharma and Siddiqi43].
Educational attainments (years of schooling) significantly affect tobacco use. The prevalence shows a declining trend as the level of schooling increases in rural and urban areas. According to the years of schooling, men who had completed 12 or more years reported a lower prevalence of tobacco use, while it was the highest among those who never visited school or had less than five years of schooling. Men with 12 or more years of schooling were significantly less likely to use tobacco, cigarettes, or bidi compared to illiterate and those with less than five years of schooling. Around twenty-five percent of illiterate men tried to stop consuming tobacco in the last 12 months.
Moreover, many studies found that tobacco consumption among the Muslim population is lower than any other religion [Reference Islam, Saif-Ur-Rahman, Bulbul and Singh5, Reference Pasupuleti, Mohan and Babu44, Reference Patel, Kumar, Srivastava and Chauhan45]. In contrast, this study has found that Muslim adults consume more tobacco than other religions, as one study found similar findings [Reference Rani, Bonu, Jha, Nguyen and Jamjoum46]. Furthermore, out of 36,378 current tobacco users, thirty percent intend to quit tobacco in the 15-49 age group. Looking for the predictors of quitting tobacco, adults who reside in rural areas had greater intention to quit tobacco which is a consistent finding from previous studies [Reference Kumar, Patel, Chauhan and Gupte34, Reference Sarkar, Arora, Gupta and Reddy47, Reference Panda, Venkatesan, Persai, Trivedi and Mathur48]. Secondhand smoke (SHS) is always considered a public health challenge in India, as there is no doubt that the risk of secondhand smoke exposure in India is relatively high. From previous GATS I and II studies, proportion of SHS was reported 48% and 35% in 2009-10 and 2016-17, respectively [Reference Verma, Kathirvel, Das, Aggarwal and Goel49]. In contrast, this study has found that more than 60% of adults aged 15-49 had been exposed to SHS. Since the COTPA act and MPOWER strategies, tobacco use has declined significantly. However, tobacco consumption remains a burning issue due to the poor implementation and dissemination of law and policy [Reference Venkatesan, Jhamtani, Gupta, Vinchurkar and Jain50].
Analysis of clustering in an event or behavior at different levels provides opportunities for suitable intervention for changing discourse of the events/behaviors. The clustering in tobacco use/smoking among men at different levels is another significant contribution of this study. Results of multilevel models indicated that, across all levels, tobacco use at the household level was found to be more concentrated (48%), which may be primarily explained by cognitive factors explaining intergenerational behavioral transition. Also, a substantial clustering in tobacco use at community/PSU level (29%) may be resulted due to neighborhood and other contextual effects, especially exhibited in negative behaviors. Last but not the least, a 13% clustering effect at the state level indicated the role of cultural and ecological factors affecting tobacco use/smoking in India.
5. Conclusions and Recommendations
Overall, the study concluded that predictors such as age, educational status, place of residence, caste, and wealth quintile had a statistically significant association with tobacco use in any form. Cessation attempt to stop tobacco smoking is a result of contribution by healthcare providers who adviced to quit tobacco to those individulas who visited to avail healthcare services. Our study also exposes that tobacco consumption was the highest in northeastern states among all Indian states and union territories (UTs). Nonetheless, the current scenario still warrants more significant public health attention and demand for better policy implementation. The study recommends three prone strategies to address the issue of tobacco epidemic in the country. First is emphasizing at specific population segments rather than adopting universal approach of prevention and control. This is primarily due to the fact that tobacco uses are higher among the northeastern states, scheduled caste and tribe, and lowest wealth quintile. Consequently, there is a need to focus on state-level approaches to control the tobacco epidemic. In addition, adults who belong to scheduled castes, tribes, and the lowest wealth quintile need to adopt a target-based approach to control tobacco use. Second, there is a need to adopt suitable strategies to focus at awareness and capacity building of rural folk as most of COTPA and MPOWER strategies are primarily targeting urban clients. The study also found that tobacco use is much higher in rural areas than in urban areas; hence, the study demanded the promotion of awareness regarding the adverse effect of tobacco use, especially in rural areas. Third, the health system response to the tobacco epidemic in the country should be strengthened by training of service providers in promoting cessation efforts through suitable counselling of all the patients visiting them in the context of tobacco usage in any form. The study also demands to educate individuals about the harmful effects of tobacco usage which is the key driver of increasing burden of NCDs, through community-based organizations.
6. Limitations of the Study
The study has some limitations too. The first limitation of this study is that tobacco use is consistently underreported in Indian scenarios. The second limitation of this is that the study is based on cross-sectional data, so it can neither explain the whole scenario of the tobacco epidemic nor could it draw causal inferences based on study findings. Moreover, the study only analyzed the male data. Hence, it could not give a picture of gender differences in tobacco use; this could also be one limitation. However, apart from all the limitations, the study provides a broad picture of the tobacco epidemic among adult men in India.
Data Availability
The data is freely available from gateway to demographic and health survey (DHS) and can be obtained from the following link: https://dhsprogram.com/data/available-datasets.cfm.
Conflicts of Interest
The authors declare that they have no conflicts of interest.














