Patients with postural orthostatic tachycardia syndrome often have multiple symptoms Reference Boris and Bernadzikowski1,Reference Shaw, Stiles and Bourne2 causing significant debilitation, including lightheadedness, nausea, headache, constipation, fatigue, and cognitive dysfunction. Some symptoms can become so severe as to be unmanageable with routine pharmacologic or non-pharmacologic therapies. Patients can also develop new or exacerbated symptoms, without effective management approaches. Such circumstances can lead to patients requiring acute care at their local Emergency Department. Historically, data have not been available regarding utilisation and associated diagnoses seen in these patients in this setting. We reviewed Emergency Department records at a single children’s hospital to better characterise how these patients utilise the Emergency Department.
Materials and methods
Medical records of patients in the Children’s Hospital of Philadelphia Postural Orthostatic Tachycardia Syndrome Program Database were reviewed to evaluate visits at the hospital’s Emergency Department. Patients were enrolled in the database if they were diagnosed and/or followed by one of the authors. The diagnosis of postural orthostatic tachycardia syndrome was made based on the presence of symptoms of significant disabling orthostatic intolerance for at least 3 months in the absence of other disorders that may have caused these symptoms. Patients also had to have a consistent increase in upright heart rate of at least 30 beats per minute during a 10-minute stand after supine positioning for 3–5 minutes. The dates reviewed included 1 July, 2011 to 2 June, 2014. Patient records were de-identified for analysis. Concurrently, all patient visits to the Emergency Department during the same timeframe not including patients from the database were de-identified as a control population. Assessment included date of visit, age, sex, all diagnoses, and corresponding International Classification of Diseases, Ninth Revision, codes. Patients aged 12–18 years were included for analysis. Patients with postural orthostatic tachycardia syndrome (subjects) were age- and sex-matched 1:1 with patients from the control group. Due to the relatively small number of subjects, a ± 3-year variance was used among control patients for age matching. Primary diagnosis and the total number of times a specific diagnosis or diagnostic category was used were recorded, although data were excluded if they were recorded twice for a patient. Categories included headache (e.g., migraine, other headache, etc.), gastrointestinal (e.g., nausea, vomiting, constipation, enteritis, gastrointestinal bleeding, etc.), autonomic (e.g., dizziness and giddiness, orthostatic hypotension, syncope, etc.), psychiatric (e.g., anorexia nervosa, depression, suicidal ideation, etc.), concussion, trauma/fracture, infection, poisoning, cardiac (e.g., cardiomyopathy, atrial flutter), asthma, gynaecologic (e.g., absence of menstruation, ulceration of vulva, etc.), and chest pain. “Other specified cardiac dysrhythmias” (International Classification of Diseases, Ninth Revision, code 427.89), which comprises postural orthostatic tachycardia syndrome and multiple other cardiac diagnoses, was included under the “autonomic” category if there were no other cardiac diagnoses associated with the encounter. As there has historically been a large female predominance noted in these patients, Reference Boris and Bernadzikowski1,Reference Shaw, Stiles and Bourne2 evaluation was performed for total, female, and male cohorts. Statistical analysis was performed using Social Science Statistics. 3 Chi-square analysis was performed for 2 × 2 contingencies, and one-way analysis of variance was used to assess independent measures. With Bonferroni correction, significance was set at <0.004. As these were data obtained in the course of clinical practice and were de-identified, this study was exempt under the Institutional Review Board of the Children’s Hospital of Philadelphia.
Results
A total of 297 patients with postural orthostatic tachycardia syndrome met criteria for inclusion. Concomitantly, there were 900 patients seen in the Emergency Department who were not followed in the Postural Orthostatic Tachycardia Syndrome Program from whom the control population was obtained. Only 357 control patients were appropriate for age- and sex-matching. A total of 239 females (80.5% of total, ratio 4.1:1) and 58 male patients were evaluated in both cohorts. The median age of the subject cohort was 15.1 (interquartile range 14.1–15.9) years, while the median age of the control cohort was 16.1 (interquartile range 14.4–17.4) years, p < 0.00001.
Primary diagnoses associated with gastroenterologic conditions and headache were seen in patients with postural orthostatic tachycardia syndrome significantly more frequently than in control patients in the total, female, and male cohorts (Table 1). Primary diagnoses associated with autonomic and psychiatric issues were seen in the control group significantly more frequently than in the group of patients with postural orthostatic tachycardia syndrome, including the total and female cohorts for both categories, and the male cohort for the autonomic category.
Table 1. Primary diagnosis, N (%).
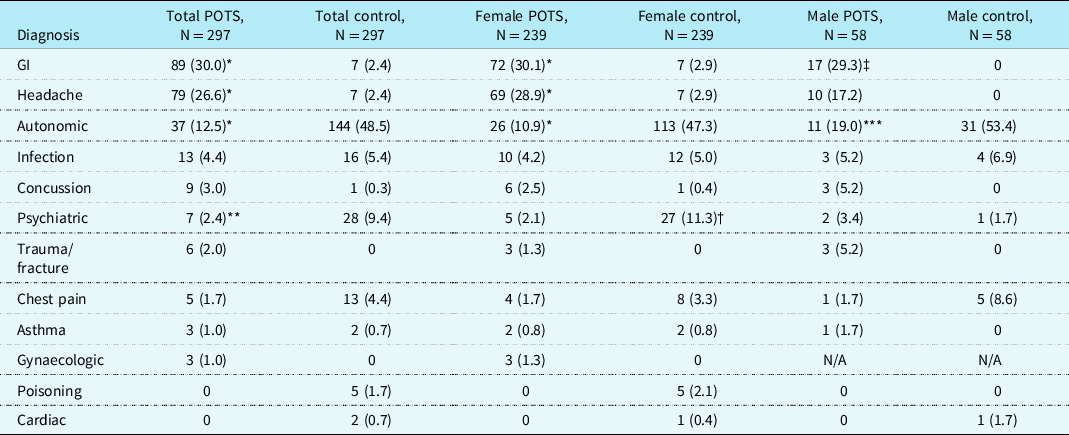
POTS = postural orthostatic tachycardia syndrome; GI = gastrointestinal.
* p < 0.00001 versus control.
** p = 0.0003 versus control.
† p = 0.00006 versus control.
‡ p = 0.00004 versus control.
*** p = 0.0001 versus control.
When total diagnoses for each patient were assessed, gastroenterologic and headache diagnoses were seen in the total, female, and male postural orthostatic tachycardia syndrome cohorts significantly more frequently than in control patients. Autonomic diagnoses were significantly greater in the total, female, and male control patients than in the postural orthostatic tachycardia syndrome cohorts, and psychiatric diagnoses were seen in significantly greater numbers in the total and female control patients versus the postural orthostatic tachycardia syndrome cohort (Table 2).
Table 2. Total diagnoses, N (%).
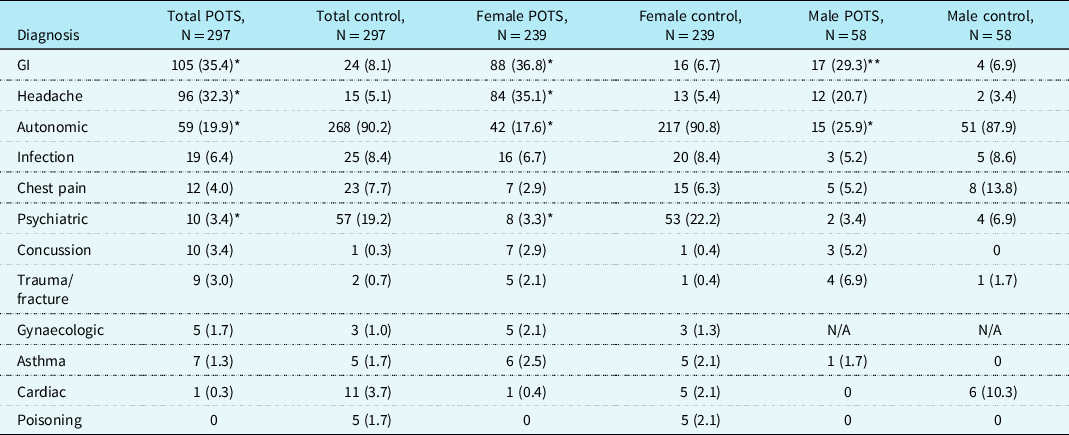
POTS = postural orthostatic tachycardia syndrome; GI = gastrointestinal.
* p < 0.00001 versus control.
** p = 0.002 versus control.
Discussion
Patients with postural orthostatic tachycardia syndrome frequently utilise the Emergency Department both before and after receiving their diagnosis. Reference Shaw, Stiles and Bourne2 Although many symptoms have been associated with postural orthostatic tachycardia syndrome, Reference Boris and Bernadzikowski1,Reference Shaw, Stiles and Bourne2 certain symptoms may be associated with significant distress and disability. In our evaluation, gastroenterologic symptoms and headache were seen in much greater frequency in patients with postural orthostatic tachycardia syndrome versus an age- and sex-matched cohort of patients presenting to the Emergency Department. The associated pain, constipation, nausea, and/or emesis can interfere with activities of daily living, as well as lead to an inability to maintain adequate oral intake and hydration, potentially worsening overall symptoms of postural orthostatic tachycardia syndrome.
“Autonomic” symptoms and psychiatric symptoms were more prevalent in control patients. Tachycardia can be seen in multiple diagnoses unrelated to postural orthostatic tachycardia syndrome, such as infection, intoxication, anxiety, hyperventilation, and others, making it a non-specific marker of disease. The presence of increased psychiatric findings in the control group is curious, since many providers mistakenly associate postural orthostatic tachycardia syndrome with psychiatric disorders, or even misdiagnose them as having psychiatric disease, Reference Shaw, Stiles and Bourne2 despite a lack of increased prevalence of psychiatric disease in these patients. Reference Raj, Haman and Raj4
A number of limitations exist in this study. Our findings are specific to a large, tertiary care children’s hospital and may not be representative of community hospitals or adult emergency departments. We were unable to obtain data on patient admission for inpatient therapies. The lack of a dedicated International Classification of Diseases, Ninth Revision, code for postural orthostatic tachycardia syndrome potentially interfered with accurate diagnostic categorisation, specifically among the control patients, such that there may have been patients with postural orthostatic tachycardia syndrome not known to our clinic in the control population.
Value of this analysis
There have been no significant or substantial previous assessments of the utilisation of Emergency Departments by patients with postural orthostatic tachycardia syndrome. Thus, the data presented continue to expand clinical insight with the capacity to improve the assessment and management of these patients presenting to Emergency Departments. These findings confirm our knowledge of the diagnoses with which these patients typically present for emergency care. This study also provides increasing insight into patient volume and diagnoses specifically in the paediatric Emergency Department and further informs clinicians’ abilities to develop supportive and effective care plans for admission in this complex group of patients. Understanding this utilisation can lead to better education and clinical practice of Emergency Department staff, anticipation and recognition of associated severe symptoms with which these patients present, and preparation of patients and families requiring emergency services associated with postural orthostatic tachycardia syndrome. In patients who have a diagnosis of postural orthostatic tachycardia syndrome, providers in the Emergency Department who identify these patients can be more aware of these complications as being associated with this diagnosis, which may lead to access to faster treatment. Emergency Departments usually have protocols available for the evaluation and management of disorders, such as intractable headache, Reference Skora, Worden and Oakley5 constipation, Reference Deneau, Mutyala and Sandweiss6 and persistent emesis, 7 which can streamline efforts to implement effective therapeutic intervention and forestall admission. As well, parents and patients can be more aware that not only are these specific clinical entities that brought them to the Emergency Department associated with postural orthostatic tachycardia syndrome but also that they are often reversible with appropriate support and care. This is important, especially if these concerns are recurrent. If patients or parents are able to alert the providers to the associations of their complaints to their primary diagnosis, and after ensuring that there are no other potential aetiologies, more efficient access to therapeutic management can help to get the patients on their way.
Although Emergency Department utilisation remained stable from 2009 to 2019 in the United States, 8 Emergency Department length of stay has increased since the SARS-CoV-2 pandemic. Reference Lucero, Sokol and Hyun9 This increased crowding leads to Emergency Department staff having to manage a higher volume of patients in a shorter amount of time. Since >8% of patients nationally present with either gastrointestinal or headache complaints, 8 patients with postural orthostatic tachycardia syndrome represent a significant percentage of patients whose symptoms can be more readily recognised and treated. This can lead to improved accuracy and efficiency of patient care as well as throughput, reducing length of stay and crowding.
Acknowledgements
The authors would like to thank Dr Marni Falk and her staff in the Mitochondrial Medicine Frontier Program at the Children’s Hospital of Philadelphia for helping to maintain the Postural Orthostatic Tachycardia Syndrome Program Database. We would also like to thank Laura McMullen and Ibrahim George-Sankoh in the Mitochondrial Medicine Frontier Program for helping to obtain and age-/sex-match the control population data.
Financial support
This research received no specific grant funding from any agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.





