The term ‘Mediterranean diet’ (MD) has been widely used to describe the traditional dietary patterns that dominated olive tree growing areas of the Mediterranean basin(Reference Bach, Serra-Majem and Carrasco1,Reference Idelson, Scalfi and Valerio2) . Despite potential differences across countries, the MD is characterised by prevalent consumption of fruits, vegetables, whole-grain cereals, legumes, nuts and seeds, with olive oil being the main source of added fat(Reference Idelson, Scalfi and Valerio2,Reference Naja, Hwalla and Itani3) . Other features of the MD include moderate intake of dairy products, little red meat consumption, coupled with a low to moderate intake of fish, poultry and wine(Reference Kafatos, Verhagen and Moschandreas4,Reference Willett, Sacks and Trichopoulou5) . Since 1975, when Keys & Keys(Reference Keys and Keys6) first introduced the term Mediterranean pattern, a plethora of studies examined the health effects of this pattern(Reference Naja, Hwalla and Itani3). These studies provided substantial evidence for a protective effect of the MD against several non-communicable diseases and cardiometabolic risk factors(Reference Willett, Sacks and Trichopoulou5,Reference Keys, Keys and Aravanis7–Reference Babio, Bulló and Salas-Salvadó11) . This may be due to its nutrient profile that is high in MUFA, dietary fibre, low glycaemic index carbohydrates and antioxidants, as well as a balanced ratio of n-6:n-3 fatty acids(Reference Idelson, Scalfi and Valerio2). Mounting evidence has also highlighted the MD as a sustainable dietary pattern because of its nutritional, environmental, economic and socio-cultural dimensions(Reference Dernini and Berry12).
At the time when the benefits associated with the MD have become pervasively recognised, a paradoxical observation is the decreased adherence to this diet by individuals living in its native countries(Reference Sibai, Nasreddine and Mokdad13). Globalisation, importation of Western habits, modernisation and shifts in lifestyle and the environment are among the potential drivers away from the traditional MD(Reference Dernini14). It has been postulated that these shifts may be particularly pronounced among adolescents, who tend to be more exposed to and influenced by food environmental factors related to the nutrition transition, such as food advertising and promotion. In addition, adolescents are increasingly adopting unhealthy eating behaviours such as the consumption of food away from home and the frequent intake of energy-dense, processed ‘fashionable’ foods(Reference Aurino, Fernes and Penny15,Reference Keats, Rappaport and Shah16) . This is of concern given that proper nutrition during adolescence is crucial for adequate physical, biological and cognitive development(Reference Salam, Hooda and Das17) and for establishing appropriate lifelong dietary behaviours(Reference Lipsky, Nansel and Haynie18). The health-related behaviours and conditions that underlie several non-communicable diseases usually start or are bolstered during the adolescent years, affecting the health and development of adolescents today while resulting in devastating effects on their health as adults tomorrow(19). According to the WHO guidance report on ‘Global Accelerated Action for the Health of Adolescents’, the 2030 Sustainable Developmental Agenda cannot be achieved without investments aimed at improving adolescent health and well-being(20).
Using different indexes and scores to assess adherence to the MD(Reference Idelson, Scalfi and Valerio2), several studies have reported low adherence to the traditional MD in the adolescent population(Reference Bargiota, Delizona and Tsitouras21–Reference Noale, Nardi and Limongi25), but studies investigating temporal trends in adherence to the MD in this age group are lacking. Such investigations are needed to allow for an evidence-based appraisal of the nutrition transition in this age group, provide insight on how dietary trends may vary between population subgroups and permit the identification of priority areas for intervention. This may be particularly true for the Eastern Mediterranean region (EMR), a region that is currently witnessing the nutrition transition, with its characteristic shifts in diet and lifestyle(Reference Sibai, Nasreddine and Mokdad13), and where adolescents represent approximately 20 % of the region’s population(26). Studies conducted in countries of the EMR highlight sky-rocketing levels of adolescent obesity and suggest a negative association between adherence to the MD and obesity in this age group(Reference Naja, Hwalla and Itani27). However, studies examining the extent of adolescents’ adherence to the MD and characterising the magnitude of dietary shifts over time are absent. The investigation of these shifts necessitates some kind of governmental commitment to public health nutrition or at least the availability of a local research infrastructure that supports such investigations. Within this context, a crucial prerequisite is the availability of nationally representative food consumption surveys conducted at different points in time among adolescents, using similar methodologies and protocols to allow for comparison. In Lebanon, a small country of the Eastern Mediterranean basin where adolescents constitute 17 % of the population, three nationally representative food consumption surveys were conducted in 1997, 2009 and 2015, respectively, providing data on the consumption level of various food groups by adolescents aged 10–19 years old(Reference Sibai, Nasreddine and Mokdad13,Reference Chamieh, Moore and Summerbell28,Reference Jomaa, Naja and Kharroubi29) , using similar data collection and dietary assessment procedures. Based on data stemming from these three national surveys, the present study aims to (1) investigate temporal trends in adherence to the MD among Lebanese adolescents, (2) examine potential sex-based differences in these trends and (3) predict adolescents’ adherence to the MD in the year 2030. Findings of this study will contribute to the characterisation of the nutrition transition in a middle-income country of the EMR and may serve as a stepping stone for the development of evidence-based interventions aimed at promoting adherence to the MD in this age group.
Methods
The data for the present analysis were derived from three nationally representative cross-sectional surveys conducted in Lebanon during three time periods: 1997, 2009 and 2015. Details about the protocols used in these surveys have been published elsewhere(Reference Jomaa, Naja and Kharroubi29–Reference Naja, Nasreddine and Itani31). The studies were carried out by the same research group at the American University of Beirut. Similar protocols and data collection methods were used for the three surveys. The three study samples were based on sampling frames provided by the Ministry of Social Affairs(32–34). Stratification by governorate was carried out and districts/neighbourhoods made up the various clusters. At the level of the cluster, the selection of the households was based on a probability-proportional-to-size approach. In the three surveys, the household was the sampling unit. In the household, in case more than one subject was eligible, the Kish method was used to recruit one subject at random(Reference Kish35). The distribution of participants was proportional to that of the Lebanese population, according to age, sex and district distribution. Few differences in the target population existed among the three surveys. More specifically, while the 1997 and 2009 surveys included males and females aged 6 years and above, the 2015 survey targeted children aged 4–18 years and their mothers. The number of participants in the three surveys was n 2004 in 1997, n 3656 in 2009 and n 1204 in 2015. The refusal rates in these surveys were 10 % in 1997, 10 % in 2009 and 23 % in 2015. For the purpose of this study, data of adolescents aged 10 to 19 years from the three surveys were used (1997 n 451, 2009 n 527 and 2015 n 666). The design and conduct of all three surveys were performed according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the Institutional Review Board of the American University of Beirut. Informed consent and assent were obtained from all parents and children, respectively.
For all surveys, data collection was conducted at the participants’ house through face-to-face interviews. Data collection was performed by research nutritionists who had received extensive training in dietary and anthropometric assessment as well as in ethical research conduct. The duration of the interviews ranged between 40 and 60 min approximately. The collected data included sociodemographic and lifestyle information, anthropometric measurement, as well as dietary intake assessment. A multi-component questionnaire was used to obtain information on demographic, socioeconomic and lifestyle characteristics. Common to the three surveys were the following variables: age (in years), sex (male, female), the region of residence (governorate), mother’s and father’s education levels (intermediate or less, high school or technical diploma and university or more) and crowding index. This index, calculated as the ratio of the number of individuals currently living in the household over the number of rooms, is considered a reliable proxy for the measurement of household socio-economic status(Reference Melki, Beydoun and Khogali36–Reference Riva, Plusquellec and Juster38). The anthropometric measurements taken in all three studies included weight (kg), height (m) and waist circumference (cm). These measurements were conducted using standardised protocols and calibrated equipment(Reference Lee and Nieman39). In brief, body weight and height were measured using a calibrated electronic weighing scale (Seca) and a portable stadiometer (Holtain), respectively. Subjects’ weights were recorded to the nearest 0·1 kg in light indoor clothing, with bare feet or stockings. Height was measured without shoes to the nearest 0·5 cm. A calibrated plastic measuring tape was utilised to measure waist circumference at the level of the umbilicus to the nearest 0·1 cm after normal expiration and with the subject standing.
For the assessment of dietary intake, the 24-h dietary recall method was used(Reference Fouad, Rastam and Ward40). For the three surveys, the 24-h dietary recall followed a structured interview format and aimed at capturing detailed information about dietary intake (foods and beverages) consumed by the participants in the past 24 h. The dietary interview was conducted directly with the adolescent subject, in the presence of the mother for assistance. Specific attention was given to food items that have been documented as frequently forgotten (such as condiments and butter). During the dietary assessment, participants’ mothers were asked to provide detailed information about the methods used in the preparation of the food items and to indicate whether any fat or oil (or other substance) was added during cooking. In order to assist in portion size estimation, participants were presented with the choice to report their intake in terms of grams or reference portion size. The latter represented one standard serving expressed in commonly used household measures such as cups and spoons. In addition, real portion size photos were used to help subjects estimate their portion sizes. The Nutritionist Pro software (Nutritionist Pro, Axxya Systems, version 5.1.0, 2014) was used for the analysis of dietary intake data. Within the Nutritionist Pro, the US Department of Agriculture database was selected for analysis. For local traditional dishes not included in the Nutritionist Pro database, recipes were added based on a local cookbook(Reference Kamal and Osman41). Food items were grouped into eighteen groups, and percent energy intakes contributed by various food groups were determined. The composition of each of the eighteen groups is found in online Supplementary Table S1.
Mediterranean diet scores
Numerous indexes and scores were proposed to examine adherence to the MD(Reference Bach, Serra-Majem and Carrasco1). For the purpose of this study, two indexes were selected: the composite Mediterranean diet (c-MED) index(Reference Issa, Darmon and Salameh42) and the Lebanese Mediterranean diet (LMD) index(Reference Naja, Hwalla and Itani3). Both of these two indexes were derived in Lebanon using dietary intake data of Lebanese populations. The c-MED index, developed by Issa et al.(Reference Issa, Darmon and Salameh42), consisted of eight components: whole grains, refined cereals and pastries, olive oil:saturated fat ratio, fruits, vegetables, legumes, fish and seafood and sugar-sweetened beverages (SSB)/liquid sweets. For presumed beneficial foods, participants who consumed an amount above the median intake received 1 point and 0 points for participants consuming amounts below the median. The beneficial foods included whole grain, olive oil, fruits, vegetables, legumes and fish and seafood. For foods/food groups presumed to be harmful (refined cereals and pastries and SSB/liquid sweets), an inverse score was assigned. More specifically, subjects consuming amounts above the median received 0 points while those below the median got 1 point. The total c-MED score was computed as the sum of points obtained for these eight food groups and hence ranged between from 0 (low adherence) and 8 (high adherence). The LMD index and its corresponding score were developed by Naja et al.(Reference Naja, Hwalla and Itani3). The index consisted of nine food items/foods: fruits, vegetables, legumes, olive oil, burghul (crushed whole wheat), milk and dairy products, starchy vegetables, dried fruits and eggs. Intakes of these various food groups were divided into tertiles. One, two and three points were given for participants falling in the first, second and third tertiles of consumption, respectively. These points were summed to obtain an LMD score for each participant. Higher scores indicated a better adherence to the LMD.
Statistical analysis
Data entry and analysis were conducted using IBM SPSS statistics software version 25 for Windows and the statistical software package Stata/SE version 13. Descriptive statistics were performed and presented as mean values with their standard errors and proportions representing continuous and categorical variables, respectively. Differences in sociodemographic and anthropometric characteristics by survey year were examined using ANOVA and the χ 2 test. Furthermore, differences among the 3 years with regard to dietary intakes from various food groups (expressed as % contribution to energy intake) as well as MD adherence scores were examined using ANOVA. To compare the proportions of the study population’s level of adherence to the MD across the 3 years, χ 2 was used. Adherence was defined as having a MD score above the median, taking the year 1997 as the reference. In order to examine the association between adherence to the MD and surveys’ years, simple and multiple linear regression analyses were conducted, in which the MD scores were considered as the dependent variable and the surveys’ years as the independent variable. In the multiple models, in addition to age and sex, sociodemographic characteristics and anthropometric measurements that were significantly associated with the surveys’ years in the univariate analyses were entered as independent variables. Results from the linear regression models were expressed as β coefficients with 95 % CI. Estimations (projections) of mean MD scores and the proportion of study participants’ adherence to the MD scores for the year 2030 were calculated using slopes and intercepts of the best-fit linear regression line corresponding to the data from the three survey years. P values lower than 0·05 were considered statistically significant. For all multiple comparisons, the Bonferroni correction was used for post hoc analyses.
Results
Table 1 shows the sociodemographic and anthropometric characteristics of participants aged 10–18·9 years by survey year (1997, 2009 and 2015). The mean age of adolescents was significantly higher in 2009 compared with the 1997 and 2015 samples. In the 3 years, the sample populations included more females than males, though there was no difference in sex distribution across the 3 years. Overall, around 1 in 4 households had a crowding index of 2 or higher with a greater proportion observed in the year 2015. Approximately 16 % of mothers attained university level education in the three surveys. On the other hand, a higher proportion of adolescents with a father’s education at university level or above was observed in 1997 (28 %) as compared with 2009 and 2015. As for anthropometric measurements, adolescents belonging to the 2015 survey had significantly larger waist circumferences and had higher prevalence rates of obesity as compared with the two other groups (Table 1).
Table 1. Sociodemographic characteristics of the total study population by survey year among Lebanese adolescents aged 10–19 years*
(Mean values with their standard errors for continuous variables and absolute numbers and percentages for categorical variables)
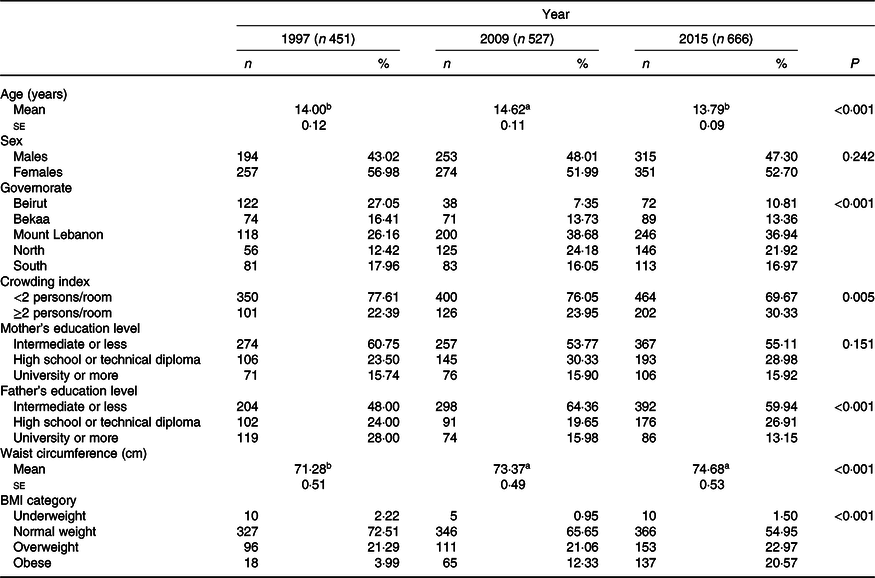
a,b Mean values within a row with unlike superscript letters were significantly different between the corresponding groups.
* Differences among group means were tested by ANOVA (for continuous variables), and Bonferroni was used for post hoc analyses. For categorical variables, the χ 2 test and χ 2 post hoc analysis with Bonferroni correction were used. BMI was stratified according to the WHO 2007 criteria(43).
Mean intakes of various foods, expressed as percent contribution to total energy, and their comparisons among the three survey years are displayed in Table 2. Data are presented among all participants and then for each sex separately. Absolute intake of various food groups in grams is presented in online Supplementary Table S2. Among participants, energy intake (kcal) was higher in 2009 as compared with that in 1997 (2072·25 (se 35·20) v. 1968·75 (se 31·84)). While intake of bread decreased across the years (from 20·04 (se 0·67) in 1997 to 12·24 (se 0·42) in 2015), that of cereals and starchy vegetables increased (cereals: 11·70 (se 0·76) in 1997 to 17·16 (se 0·72) in 2015; starchy vegetables: 5·86 (se 0·42) in 1997 to 7·68 (se 0·43) in 2015). The highest intakes of fruits (whole fruits) and vegetables were observed in 1997 (6·05 (se 0·36) and 6·51 (se 0·37), respectively) and lowest intakes were in 2015 (3·44 (se 0·22) and 3·83 (se 0·26), respectively). On the other hand, intakes of chips and salty snacks increased to reach the highest contribution to energy in 2015 (7·66 (se 0·44)), while intakes of SSB and added fats and oils reached the highest contribution to energy in 2009 (7·13 (se 0·31) and 5·75 (se 0·34), respectively). When comparison across the years was carried out for males and females separately, the results showed similar trend to that of the overall sample (Table 2).
Table 2. Daily food consumption (% energy intake) of sample contributed by various food groups according to survey year in the study population, Lebanon, 1997, 2009 and 2015 among adolescents aged 10–19 years*
(Mean values with their standard errors)
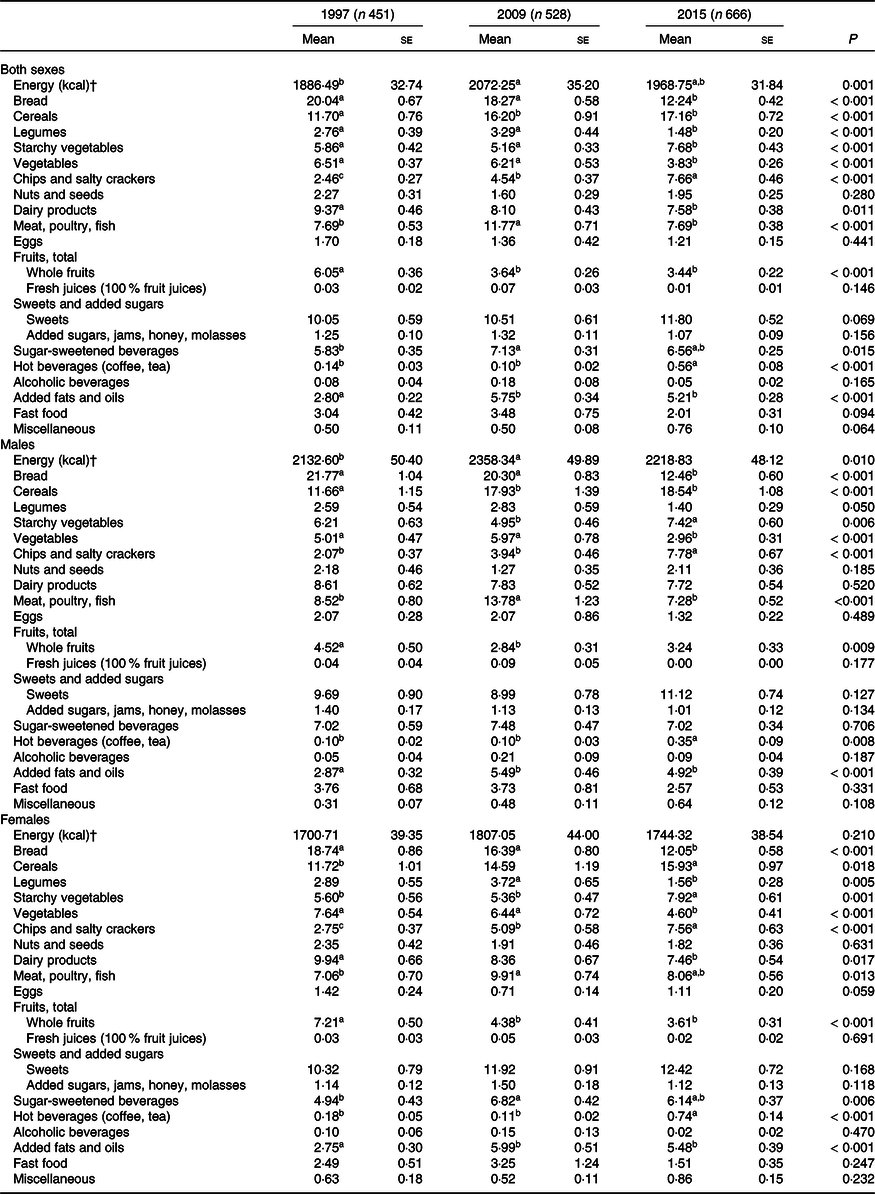
a,b Mean values within a row with unlike superscript letters were significantly different (post hoc, P ≤ 0·05).
* Differences among group means were tested by ANOVA. Bonferroni was used for post hoc analyses.
† To convert kcal to kJ, multiply by 4·184.
Table 3 showed a description of the two MD indexes used in this study: the c-MED and the LMD. Common food groups that contributed positively to the total score for these indexes were fruits, vegetables and legumes. As for olive oil, the c-MED score accounted for its intake as a ratio of olive oil: SFA, while the LMD score considered the absolute amount of olive oil consumed. Although the c-MED score could have ranged between 0 and 8, the results showed a range of 0–6 among study participants. Similarly, the LMD score range in this study was 9–20 despite a possible range of 9–27 (Table 3).
Table 3. Description of the selected Mediterranean diet scores*
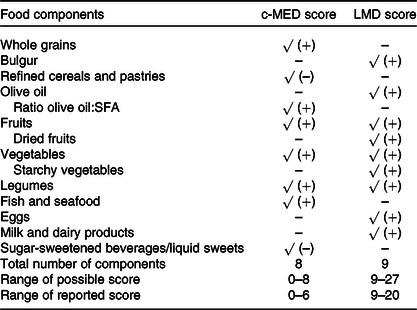
c-MED, composite Mediterranean diet; LMD, Lebanese Mediterranean diet.
* √ refers to the food components that are part of the corresponding score computation. (+) was used when a higher score was assigned to a greater intake, (–) was used when a higher score was assigned to a lower intake.
Fig. 1 showed the mean adherence score by survey year for all participants and for males and females for the c-MED (Fig. 1(a)) and LMD indexes (Fig. 1(b)). In addition, the projections for the year 2030 were also indicated on the graphs. The results showed a steady decrease in the c-MED score, more consistent for females as compared with males. Similarly, mean LMD scores decreased across the years of the surveys. Projections for both scores showed further decrease in the scores in the year 2030 (Fig. 1).
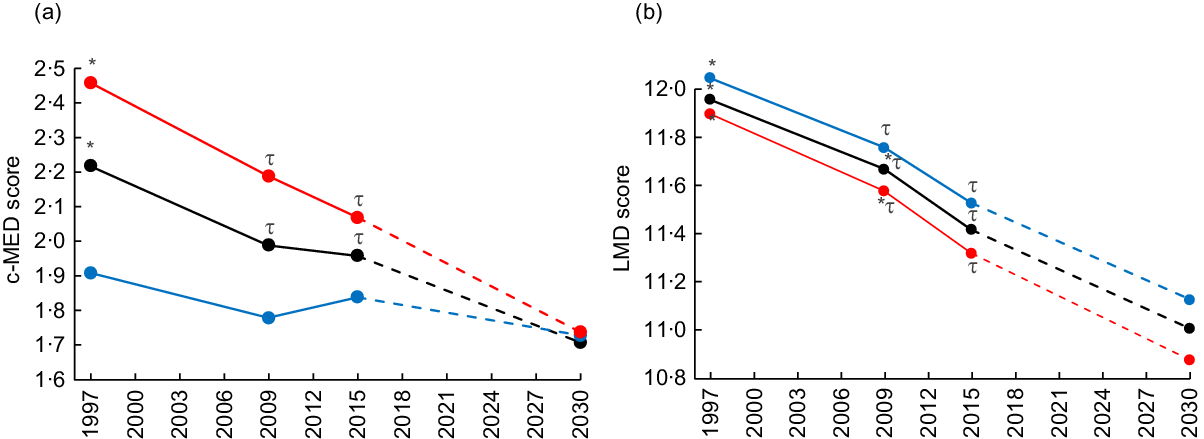
Fig. 1. Mean Mediterranean diet scores distribution among adolescents by sex and survey year and projections in 2030. c-MED, composite Mediterranean diet; LMD, Lebanese Mediterranean diet. Projections are presented by the dashed lines. Different symbols indicate significant difference between the corresponding groups. ![]() , Both sexes;
, Both sexes; ![]() , males;
, males; ![]() , females.
, females.
Comparisons of the proportions of study participants (overall, males and females) who were adherent to the MD across the 3 years were presented in Fig. 2 using the c-MED score (Fig. 2(a)) and the LMD score (Fig. 2(b)). Projections were made for the year 2030. Using the c-MED score, the results showed that adherence decreased from 35·03 % in 1997 to 30·3 % in 2009 reaching 27·63 % in 2015. Statistical difference was found between the years 1997 and 2015. The projections for the year 2030 showed a proportion of 21·59 % to remain adherent to the MD. Using this score, the steady decrease in the proportions of adolescents adhering to the MD was mainly observed among females as compared with males (Fig. 2(a)). Similarly, using the LMD scores, adherence to the MD decreased significantly between 1997 and 2015 for the overall sample as well as for each sex. In the overall sample, the proportion of adolescents adhering to the MD decreased from 38·58 % in 1997 to 24·62 % in 2015. The projections for the year 2030 showed that the adherence to the MD among adolescents, using the LMD index, would decrease further to reach 14·76 % (Fig. 2(b)).
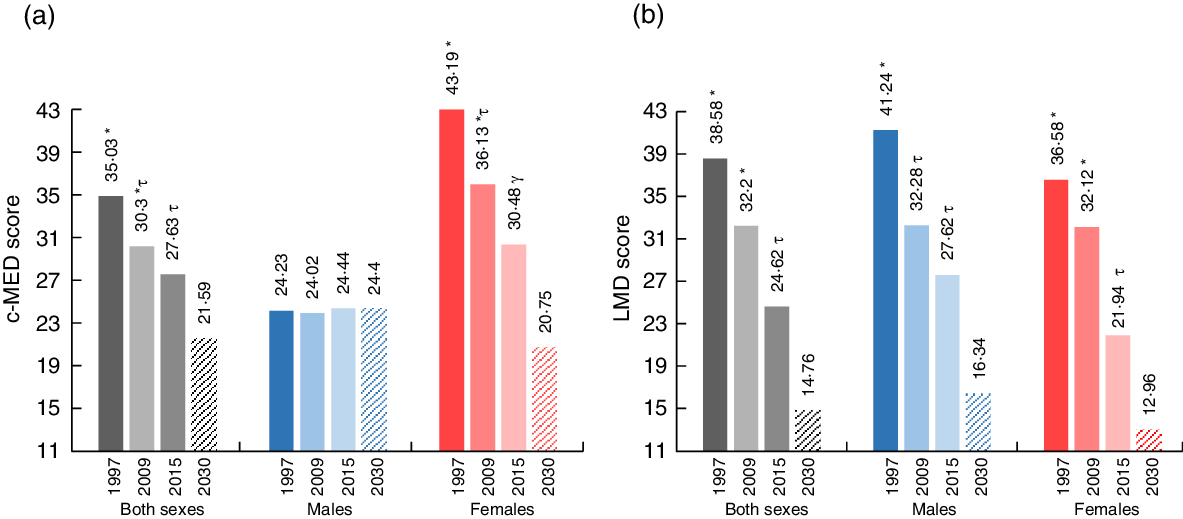
Fig. 2. Proportion of the study population’s level of adherence to the Mediterranean diet scores by sex and survey year and projection to 2030. c-MED, composite Mediterranean diet; LMD, Lebanese Mediterranean diet. Projections are presented by the dashed rectangles. Different symbols indicate significant difference between the corresponding groups.
The regression coefficients and their corresponding 95 % CI depicting the association of survey year with the MD adherence scores were presented in Table 4. Three models were carried out: model 1 (crude) with no adjustment, model 2 adjusted for age and sex and model 3 adjusted for age, sex, governorate, crowding index, father’s education and energy intake. In the third model, variables that were found to be significantly different among the three study populations were included. The results of these analyses showed that belonging to the year 2009 was associated with significantly lower MD scores as compared with belonging to the year 1997, even after adjustment for potential covariates (c-MED score β = –0·16, 95 % CI –0·30, –0·01); LMD score β = –0·42, 95 % CI –0·67, –0·17)). Similar results were obtained when comparing survey year 2015 with 1997 (Table 4).
Table 4. Simple and multiple linear regressions between Mediterranean diet adherence scores (treated as continuous) and surveys’ years*
(β Coefficients and 95 % confidence intervals)
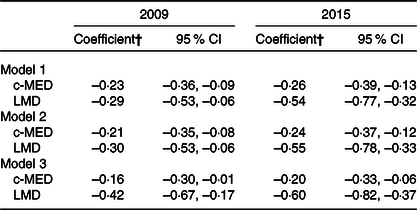
c-MED, composite Mediterranean diet; LMD, Lebanese Mediterranean diet.
* Model 1: crude; model 2: adjusted for age and sex; model 3: adjusted for age, sex, governorate, crowding index, father’s education and energy intake.
† Reference category is the year 1997.
Discussion
To our knowledge, this study is the first to investigate and characterise temporal shifts in adherence to the MD among adolescents. Based on individual national nutrition surveys conducted in 1997, 2009 and 2015 among Lebanese adolescents, the study findings documented a steady secular decrease in MD adherence scores based on two country-specific indexes. In parallel, the proportions of adolescents adhering to the MD were found to significantly decrease over time, with approximately only a quarter of adolescents remaining adherent to this dietary pattern in 2015, and with further decreases being projected for 2030.
For the assessment of temporal trends in MD adherence, two locally derived and tested indexes were selected: the c-MED, an a priori score developed by Issa et al.(Reference Issa, Darmon and Salameh42), and the LMD, an a posteriori score developed by Naja et al.(Reference Naja, Hwalla and Itani3). The study results showed a steady decrease in both the c-MED and the LMD scores across the years of the surveys. Given that adherence to the MD may be modulated by individual, demographic and socio-economic characteristics(Reference Idelson, Scalfi and Valerio2), we have further examined the association between adherence to the MD and surveys’ years, while adjusting for potential confounders. These analyses showed that the decreases in MD adherence scores remained significant even after adjusting for several factors, including age, sex, energy intake and socio-economic indicators, such as crowding index and parental education level. In parallel, the proportions of adolescents adhering to the MD were found to consistently decrease over time, from 35·03 % in 1997 to 27·63 % in 2015 for the c-MED and from 38·58 % in 1997 to 24·62 % in 2015 for the LMD. A recent review of studies examining MD adherence in children and adolescents living in Southern European countries suggested a trend towards poorer adherence over time, although formal trend analysis was not conducted(Reference Grosso and Galvano44). Our estimates of adolescents adhering to the MD in Lebanon fall within those reported in a recent systematic review where MD adherence among adolescents was found to range between 4·3 and 43·7 % in Greece; 20·3 and 53·6 % in Spain 8·8 and 16·5 % in Italy, while an estimate of 22·9 % was reported for Turkey(Reference Idelson, Scalfi and Valerio2). It is important to note that the comparability of study findings may be limited by the fact that studies conducted in various countries may have adopted different dietary assessment methods, disparate age groups or distinct MD adherence indexes that differed with respect to the number of food items included, the cut-off values adopted and the definition of what dietary component is considered detrimental or protective, hence limiting(Reference Grosso and Galvano44).
In our study, sex differentials in MD adherence trends were observed. More specifically, the decrease in the c-MED score and in the proportions of adolescents adhering to the MD was more consistent for females as compared with males. Studies reporting on sex differentials in adherence trends are lacking, but available evidence on MD adherence per se reported inconsistent evidence based on sex. A recent systematic review by Idelson et al.(Reference Idelson, Scalfi and Valerio2) concluded that, contrary to findings reported among adults whereby women tend to have better dietary habits and higher MD adherence, evidence among children and adolescents is conflicting and does not support such sex differentials. During the past two decades, Lebanon has experienced significant changes in its socio-cultural norms, alleviating some of the cultural barriers that young girls used to face such as the negative connotations associated with going out and participating in social activities(45). These changes may have contributed to the fostering of modern ‘westernised’ habits among young girls, such as eating out in restaurants and fast food chains, which may at least partly explain the consistent temporal decrease in MD adherence among Lebanese girls(Reference Jodhun, Pem and Jeewon46).
To better understand the drivers of the observed decline in MD adherence, we investigated changes in food groups’ intakes. Since fruit and vegetable consumption is positive contributors to MD adherence scores, the observed secular decrease in the intake of these food groups may have contributed to the decline in MD adherence during the study period. The observed decrease in fruit and vegetable consumption in Lebanese adolescents is contradictory to findings reported among adolescents from European Mediterranean countries where fruit and/or vegetable intakes were found to increase or to remain stable over time(Reference Vereecken, Pedersen and Ojala47). In parallel, our study findings showed an increase in the consumption of ‘harmful’ foods such as refined cereals and SSB. In fact, the consumption of cereals and cereal-based products, which comprise refined-grain food items such as white rice, pizzas, pies, has significantly increased during the study period. Similarly, the intake of SSB has increased in Lebanese adolescents, from 241·4 g/d in 1997 to 321·7 g/d in 2009 and 301·6 g/d in 2015. Contrary to our findings, Ribas-Barba et al.(Reference Ribas-Barba, Serra-Majem and Salvador48) and Lioret et al.(Reference Lioret, Dubuisson and Dufour49) did not report any significant increase in SSB intakes among adolescents from Catalonia (Spain) and France. Taken together, our study findings identified the food groups that are potentially driving the decline in MD adherence and the nutrition transition among adolescents in Lebanon. The results also showed that, in many instances, the observed shifts in food groups’ intakes are not consistent with those reported from European Mediterranean countries, the latter being at a different nutrition transition stage compared with the EMR. Furthermore, unlike Lebanon, where policy development is lagging behind, several European countries were proactive in implementing public health nutrition programmes to foster healthier dietary habits(Reference Weichselbaum, Hooper and Buttriss50,51) .
Lebanon, like other countries of the EMR, has witnessed during the past two decades a westernisation of dietary habits, losing part of its food heritage and dietary idiosyncrasies(Reference Sibai, Nasreddine and Mokdad13,Reference Nasreddine, Ayoub and Hachem52) . These dietary shifts have been particularly seen as of the 1990s, after the end of the Lebanese civil war(Reference Nasreddine, Ayoub and Hachem52), when Lebanon witnessed important socio-economic and socio-cultural transformations that have led to changes in the food supply chain and food demand. Examples of such changes are rapid urbanisation, technical development in the food industry and increased importation of foods. The impact of these transformations may have been more pronounced on adolescents, who are particularly influenced by an array of commercial, technological and communication factors. The low adherence of Lebanese adolescents to the MD raises a public health concern, given that this dietary pattern has been consistently associated with higher dietary diversity and nutritional adequacy(Reference Idelson, Scalfi and Valerio2). A recent systematic review showed that higher MD adherence was associated with healthier nutrients’ profiles in adolescents, including high fibre intake, optimal MUFA:SFA ratio and low SFA intake(Reference Idelson, Scalfi and Valerio2). Available evidence also indicates that higher MD adherence is linked to higher micronutrient adequacy in children and adolescents, particularly for Ca, Fe, Mg, K, P and vitamins B6, A and C(Reference Castro-Quezada, Román-Viñas and Serra Majem53). Fostering healthy dietary habits and ensuring optimum nutrition in the adolescent years are crucial given its potential health impacts in the short and longer terms(Reference Costarelli, Koretsi and Georgitsogianni54). Several studies have suggested that higher MD adherence may decrease the risk of excessive weight gain(Reference Martin-Calvo, Chavarro and Falbe55) and foster healthier BMI status in adolescents(43,Reference Lazarou, Panagiotakos and Matalas56–Reference Grosso, Marventano and Buscemi58) . The trends in MD adherence described in our study occurred at a time of growing concern about adolescent obesity in Lebanon, which have increased from 5·9 to 10·2 % between 1997 and 2009(Reference Nasreddine, Naja and Chamieh59). It is even more worrisome that the projections for 2030 highlight further decreases in MD adherence scores and in the proportions of adolescents adhering to the MD, with only 14–20 % of Lebanese adolescents remaining adherent to this dietary pattern in 2030. As adolescents’ health and well-being have been identified as central to achieving the Sustainable Development Goals(20), these projections do not bode well for the future of Lebanon and its development.
Several strengths can be allocated to our study. First, the study is based on national food consumption surveys that were carried out at three points in time in Lebanon. In all three surveys (1997, 2009 and 2015), similar data collection protocols and dietary assessment methods were used, and therefore, the trends observed in food consumption patterns cannot be attributed to discrepancies in methodologies. In addition, to allow for comparison between the three points in time, we used the same indexes to assess adherence to the MD (c-MED and LMD). In all three surveys, we did not rely on self-reported dietary data, but rather trained nutritionists, who received extensive training to decrease judgemental communication and minimise social desirability bias, administered the 24-h dietary recalls. However, the results of the study ought to be considered in light of the following limitations. Although a single 24-h dietary recall may not fully represent the usual dietary intake of individual adolescents, it is considered appropriate for the characterisation of the average usual diet of adolescents as a group, particularly that in each survey, the study sample was representative of the population under study(Reference Kroes, Müller and Lambe60). In addition, a specific attention was devoted by the research team to cover and equally represent all days of the week during data collection. It is also important to acknowledge that the 24HR approach may be associated with dietary under-reporting, given the possibility of missing some food items during the recall, which can have an impact on absolute intake levels of foods and nutrients(Reference Aparicio-Ugarriza, Cuenca-García and Gonzalez-Gross61). Given the fact that our study focused on trend in dietary intakes over time, this under-reporting may have had little implications on our findings since the three surveys were conducted using the same dietary assessment method. Finally, the characterisation of trends in food consumption patterns and MD adherence was based on three separate cross-sectional surveys with different samples. The differences in food consumption and MD adherence between the surveys could therefore be, at least partly due to a birth cohort effect. Hence, there is a need for further studies to elucidate such an effect and formulate cohort-specific strategies to halt the nutrition transition in the country(Reference Reither, Hauser and Yang62).
In conclusion, our study findings documented a significant decreasing trend in adherence to MD among Lebanese adolescents from 1997 to 2015. The study has also identified the main food groups that drive this decline, including the decrease in fruits and vegetables, coupled with the increase in refined cereals and SSB. The erosion of the MD among adolescents highlights the importance of monitoring dietary pattern changes and developing well-structured public health and community measures to preserve the traditional Mediterranean dietary pattern in Lebanon, with its well-documented health benefits(Reference Bach, Serra-Majem and Carrasco1,Reference Naja, Hwalla and Itani3) . A comprehensive food system approach tackling the food supply, food environment as well as the dietary behaviour of adolescents ought to be implemented to foster the promotion of the MD as a nutritionally balanced and sustainable dietary pattern in this population and re-anchoring it within the local culture and traditions. The successful implementation of a food system approach requires concerted actions from stakeholders, policy makers, consumers and academicians. Interventions tackling the food environment and the consumer ought to focus on young generations since, like most other lifestyle factors, healthy eating habits are more likely to take root and persist if they are acquired and practised earlier in life(Reference Berry63).
Acknowledgements
The authors would like to thank all participants for their time and effort. The authors would also like to thank Ms Mandy Taktouk for reviewing the manuscript.
This research was funded by Food and Agricultural Organization of the UN (FAO), RA I 0 I 0 I 000000/RA I 040200CT71. The original surveys were funded by the Lebanese National Council for Scientific Research (grant number: 03-12-08) through its support to the Associated Research Unit on Undernutrition and Obesity in Lebanon, the Training Programs in Epidemiology and Public Health Interventions Network (TEPHINET in the US), the WHO-Lebanon (grant number: TSA/08/00150. EM0882149) and the University Research Board at the American University of Beirut (grant number: 103006). The funders had no role in the design, analysis or writing of this article.
F. N. and L. N. conceptualised the study. F. N. supervised data analysis and interpretation. N. A. and F. A. Z. C. conducted data analysis. S. K. assisted in the statistical analysis for the study. N. H. led the conduct of the 1995 and 2009 surveys. L. J. led the conduct of the 2015 survey. M.-C. C. led the fieldwork related to dietary assessment. L. N. contributed to data interpretation. F. N., L. N. and L. J. wrote the first draft of the manuscript. N. H. and F. H. critically reviewed the final version of the manuscript. All authors read and approved the final manuscript.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114520002731









