Depression and diet
Several investigations have established the relationship between the foods the person eats and the manner the person acts or feels. Diet has been associated not only with mood fluctuations but also with several mental diseases and behavioural problems like autism, attention-deficit/hyperactivity disorder, schizophrenia, dementia, antisocial behaviour or depression.
We are at a critic moment regarding our mental health. Worldwide, 450 million people suffer from mental or neurological disorders or from psychological problems related to alcohol or drug abuse; some of these problems represent the most important causes of disability worldwideReference Longfield, Ryrie and Cornah1. The 2003 WHO report estimated that depression is the leading cause of morbidity among women and the fourth cause among men around the world (it is likely the proportion is higher in developed countries). Among subjects aged between 15 and 59 years, the disease is the second cause of morbility2.
Thus, it is essetial to study depression and its associated factors, including diet. And, how the Mediterranean diet affects depression?
Mediterranean diet and B vitamins
The Mediterranean diet is a dietary pattern characterised by a high fruits, nuts, vegetables, legumes, cereals, olive oil, and fish consumption, a low meat and dairy products consumption and a moderate alcohol intake. Thus, the adherence to this pattern ensures an adequate intake of vitamins, specifically B vitamins such as B1, B2, B12 and B6 vitamins and folic acid.
The protective role of these nutrients, especially of B6, B12 and folic acid on cardiovascular disease, Alzheimer or depressive disorders has been hypothesised by different epidemiological studies in the last yearsReference Hernandez-Diaz, Martinez-Losa, Fernandez-Jarne, Serrano-Martinez and Martinez-Gonzalez3, Reference Ravaglia, Forti, Maioli, Martelli, Servadei, Brunetti, Porcellini and Licastro4.
To understand the mechanisms of B vitamins involved in depression, it is important to describe the homocysteine cycle.
Homocysteine is an intermediate product produced in the methionine metabolism. Vitamin B12 and B6 serve as cofactors for enzymes involved in the conversion of homocysteine to methionine and cysteine, respectively. Methylenetetrahydrofolate reductase catalyses the conversion of 5, 10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, which remethylates homocysteine to methionine.
Moreover, methionine is a precursor of S-adenosylmethionine, which acts in several methylation reactions, including those involving neurotransmitters (monoamines and catecholamines) and phospholipids of the central nervous system. Therefore, a decreased intake of B vitamins may result in an accumulation of homocysteine and in a decreased synthesis of monoamines in brain, likely contributing to mechanisms related with the origins of depression.
On the other hand, folate metabolism is involved in the biopterin-dependent neurotransmitters synthesis. Tetrahydrobiopterin is a cofactor essential for the synthesis of biogenic amines whose precursors are tyrosine and tryptophan. Thus, folate deficiency may impair the synthesis of serotonin, dopamine or norepinephrine.
In conclusion, a deficit of B12 or B6 vitamins or folate would lead to an accumulation of homocysteine or its metabolites such as homocysteinic and cysteine sulphinic acid. These metabolites may inhibit the S-adenosylmethionine methylation reactions. In addition, its metabolites might also have an excitotoxic effect on the N-methyl-d-aspartate glutamate receptors in the central nervous system. (Fig. 1)

Fig. 1 Homocysteine cycle. Partially adapted from Bjelland et al. Reference Bjelland, Tell, Vollset, Refsum and Ueland9
Consequently, there are several mechanisms underlying the protective role of B vitamins on depression.
Numerous epidemiological studies have shown high prevalence of B vitamins deficiency in subjects with depression. Similarly, an association between high serum homocysteine levels and a higher prevalence of depressive symptoms has been reported in numerous cross-sectional and case-control studies.
A study comprising 412 subjects and published in 2005 showed an association of high homocysteine and low plasma folic acid levels with an increased severity of depressive symptoms among men. Likewise, when the authors analysed the association between folate levels and depressive symptoms in the overall sample, men and women, being in the lowest quartile of folic acid was associated with increased depressive symptomsReference Sachdev, Parslow, Lux, Salonikas, Wen, Naidoo, Christensen and Jorm5.
Similar results, but only among women, were obtained in the Sacramento Area Latino Study on Aging (SALSA) study, based on a US Latinos sampleReference Ramos, Allen, Haan, Green and Miller6. The OR for high depression symptoms in women in the lowest third of plasma folate was 2.04.
Penninx et al. did not find a significant effect on depression for plasma folate levels in a study based on 700 disabled, nondemented women aged 65. However, the subjects with B12 deficiency were 2.05 times as likely to be severely depressed as were nondeficient subjectsReference Penninx, Guralnik, Ferrucci, Fried, Allen and Stabler7.
There are evidences regarding the association between plasma folate and vitamin B12 levels and the prevalence of depressive symptoms, but what happens with intake?
The Kuopio Heart Study, a cohort study consisted of 2600 Finnish middle-aged men, analysed the relationship between folate intake and risk of depression during 13 years of follow-upReference Tolmunen, Hintikka, Ruusunen, Voutilainen, Tanskanen, Valkonen, Viinamaki, Kaplan and Salonen8. Those subjects below the median of energy-adjusted folate intake had a significant higher risk of getting discharge diagnosis of depression (RR 3.04, 95% CI: 1.58, 5.86) than those who had a folate intake above the median. There was no effect for a high vitamin B12 intake.
Low blood levels of folate have been linked with a poor response to antidepressant treatment. For that reason, a number of clinical trials have analysed whether the co-administration of vitamin B12, methylfolate, folinic acid or folic acid with the antidepressant treatment enhanced its effect.
Alpert et al. assessed the efficacy of methylfolate as an adjunctive treatment among adults with major depressive disorder and inadequate response to selective serotonin re-uptake inhibitors treatment. Sixteen participants completed this 8-week prospective open trial. The administration of folinic acid improved the depression scores on the HAM-D-17 scale and on the CGI-I scaleReference Alpert, Mischoulon, Rubenstein, Bottonari, Nierenberg and Fava10.
In this sense, a systematic review of clinical trials was carried out in 2004. The trials analysed the effectiveness of folate administration vs. placebo administration in the treatment of depression. Hamilton depression rating scale scores after the follow-up period were lower among patients who received folate than among subjects who received placebo. Coppen found that adding folate reduced statistically Hamilton score by 2.65 points [95% confidence interval (CI) − 5.07 to − 0.13]. Pooling the results of the two trials that compared folate with placebo in addition to other psychotropic medication, the weighted mean difference in Hamilton score between the groups at trial end point favoured treatment with folate (difference = − 2.65; 95% CI − 4.93 to − 0.38)Reference Taylor, Carney, Goodwin and Geddes11.
Nevertheless, the results obtained regarding the administration of cobalamin failed to assess a beneficial effect of this vitamin. A clinical trial analysing the effect of vitamin B12 did not find a significant depressive score differences between the administration of this vitamin or placebo after 3 months of follow-upReference Hvas, Juul, Lauritzen, Nexo and Ellegaard12.
B6 vitamin has also been studied as an adjuvant in depression treatment. A wide range of doses and follow-up periods has been analysed. Studies addressing premenstrual syndrome and hormone-related depression in women revealed a consistent message about the value of using vitamin B6 supplementationReference Williams, Cotter, Sabina, Girard, Goodman and Katz13.
Mediterranean diet and ω-3 fatty acids
Mediterranean diet is characterised by a moderate consumption of fish, main source of ω-3 fatty acids.
ω-3 fatty acids are long-chain polyunsaturated fatty acids (PUFA) that cannot be synthesised in the human body and therefore they have to be incorporated from diet. The most important ω-3 fatty acids are the α-linolenic acid (ALA), the eicosapentaenoic acid (EPA) and the docosahexaenoic acid (DHA). Vegetables are rich sources of ALA. This fatty acid can be metabolised into EPA and DHA. Similarly, EPA and DHA are provided by fish sources such as mackerel, herring, anchovy or salmon.
There are several mechanisms of action of ω-3 fatty acids in depression. Depression is associated with neuronal atrophy. Antidepressant medication can lead to an increment in nerve growth factors such as brain-derived neurotrophic factor which improves neurotransmission and synaptic plasticity. A number of investigations suggest that depression is associated with excessive production of proinflammatory cytokines. Proinflammatory cytokines and prostaglandin E2 may inhibit brain-derived neurotrophic factor expression. ω-3 fatty acids have been suggested as inhibitors of proinflammatory mediators synthesis such as cytokines, especially tumour necrosis factor α (TNF-α) and interleukin 1β (IL-1β), increasing, as a result, brain-derived neurotrophic factor. Moreover, proinflammatory cytokines interfere in neurotransmitters metabolism and alter neurotransmitters mRNA. In the same way, cytokines may decrease serotonin precursors such as tryptophan and activate the hypothalamic pituitary adrenal axis causing resistance to glucocorticoid hormones. Finally, a change in the fatty acids composition of central nervous system membranes may alter their functions by changing fluidity and biophysical properties as well as neurotransmitters availability.
The first epidemiological evidence regarding the protective role of ω-3 fatty acids intake on depression comes from ecological studies. Hibbeln published the results of an ecological study, where an increment in fish consumption was correlated with a decreased annual prevalence of depression worldwideReference Hibbeln14. Hibbeln found similar negative correlation between total seafood consumption and the prevalence of post-partum depressionReference Hibbeln15.
Several case-control studies have also analysed the association between ω-3 fatty acid levels and depressive disorders. A nested case-control study was conducted within the Rotterdam cohort study. This population-based study showed that fatty acid composition of plasma phospholipids was associated with depressive disordersReference Tiemeier, van Tuijl, Hofman, Kiliaan and Breteler16. Subjects with depressive disorder had a significant lower percentage of ω-3 fatty acids in plasma phospholipids than did the group without depressive symptoms.
Recently, other case-control study found similar results in patients recovering from acute coronary syndromes. Major depression was associated with significantly lower plasma levels of ω-3 fatty acidsReference Frasure-Smith, Lesperance and Julien17.
However, only one cohort study has assessed the association between ω-3 fatty acids intake and the risk of depression. The study failed to find a statistically significant association between fish consumption or ω-3 fatty acids intake and the risk of depression among Finnish men after 9 years of follow-up. Depression was defined as a self-reported depressed mood and as the presence of a hospital treatment due to depression. None of the definitions of depression were related to the amount of fish or ω-3 fatty acids intakeReference Hakkarainen, Partonen, Haukka, Virtamo, Albanes and Lonnqvist18.
The results obtained from clinical trials are contradictory. Some of the trials fail to find a beneficial effect of the co-administration of ω-3 fatty acid supplements on depression treatment. On the other hand, several trials have suggested a positive role for these nutrients. In a clinical trial published in 2005 where the patients were randomly assigned to receive either olive oil or DHA-enriched fish oil, there were statistically significant differences in plasma ω-3 fatty acids levels between the two groups. However, both treatments achieved significant decreases in Hamilton scale scores after 2 weeks of interventionReference Silvers, Woolley, Hamilton, Watts and Watson19.
Mediterranean diet and the SUN Project
A growing body of research indicates a protective effect of different components of the Mediterranean diet on depression, like B vitamins or ω-3 fatty acids. In this context, it is necessary to introduce the SUN Project.
The SUN Project (Seguimiento Universidad de Navarra- Follow-up University of Navarra) is a prospective cohort study designed to establish the association between several dietary habits or lifestyle-related characteristics and the occurrence of several diseases and chronic conditions, including depressionReference Martínez-González, Sánchez-Villegas, De Irala, Marti and Martínez20. The recruitment of participants started in December 1999 and it is permanently ongoing as this is a dynamic cohort study. Information is collected using self-administered questionnaires sent by postal mail every two years.
Study subjects
The baseline questionnaires of 11 623 participants were coded, processed and ready for statistical analysis. Those participants who reported extremely low or high values for total energy intake (less than 600 and 400 Kcal day− 1 in men and women, respectively, or more than 4200 and 3500 Kcal day− 1 in men and women, respectively) (n = 1381), and subjects with a diagnosis of depression at an age prior to the age reported in the baseline questionnaire (n = 572) were excluded. Finally, data from 9670 participants (4211 men and 5459 women) remained available for the analysis.
Exposure assessment
The dietary exposure was ascertained through a semi-quantitative food frequency questionnaire (136 food items) previously validated in SpainReference Martín-Moreno, Boyle, Gorgojo, Maisonneuve, Fernández-Rodríguez, Salvini and Willett21. For the present analyses, we considered B12, B6, folic acid and ω-3 fatty acids intake as exposure factors.
B vitamins and ω-3 fatty acids intakes were adjusted for total energy intake using the residuals method. Then, the continuous variables were categorised in quintiles considering the first quintile as the reference category.
Outcome assessment
Depression was assessed though a question included in the baseline questionnaire. Participants responded to the following question: have you ever been diagnosed of depression by a health professional? The baseline questionnaire collected the use of regular antidepressant medication as well.
Recent depression was defined as the positive answer to either the question regarding physician-diagnosed depression or participant reporting of the use of antidepressant medication in baseline questionnaire.
Covariables assessment
The baseline assessment also included other questions (totally 46 items for men and 54 items for women) . Socio-demographic (e.g. gender, age, marital status and employment status), anthropometric (e.g. weight and height), lifestyle and health-related habits (e.g. smoking status, caffeine and alcohol intake and physical activity during leisure time), psychological characteristics (e.g. personality traits) and medical history variables (e.g. prevalence of chronic diseases and medication use) were also collected.
Results
We found no statistically significant associations between B vitamins intake and the prevalence of depression among men, although some point estimates for odds ratios (ORs) suggested an inverse association with folate intake. The multivariate-adjusted ORs (95% confidence intervals) for depression for successive quintiles of energy-adjusted folate intake were 1 (reference), 0.81 (0.51–1.28), 0.77 (0.48–1.25), 0.72 (0.43–1.20) and 1.01 (0.57–1.79). When the analyses were carried out according to several characteristics, we found an inverse association between energy-adjusted folate intake and the prevalence of depression among men who were current smokers. The ORs for depression in this group of men were 0.31 (0.12–0.82), 0.25 (0.08–0.75) and 0.52 (0.17–1.57) for the third to fifth quintiles, respectively, as compared to the reference quintile (Fig. 2).
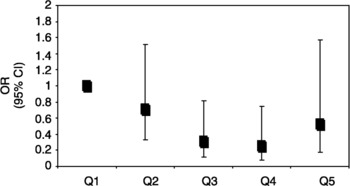
Fig. 2 Association between folate intake and depression prevalence in males who were current smokers in the SUN study. Q1, first quintile; Q2–Q5, second–fifth quintile
We found a significant inverse association between energy-adjusted vitamin B12 intake and prevalence of depression among women. ORs (95% CI) for successive quintiles of intake were 0.65, (0.46–0.91), 0.58 (0.41–0.84), 0.56 (0.38–0.82) and 0.68 (0.45–1.04), respectively. There were not statistically significant associations between folic acid or vitamin B6 intake and the prevalence of depression in females.
When the analyses were restricted to women who reported moderate physical activity level or to women who were current smokers, depression prevalence could be around 50% lower among whose vitamin B12 intake was in the Q2–Q5 than among women in the reference category of intake (Fig. 3).

Fig. 3 Association between B12 vitamin intake and depression prevalence among women who were current smokers and physically active in the SUN study. Q1, first quintile; Q2–Q5: second–fifth quintile
There were no statistically significant associations between ω-3 fatty acids intake and depression. However, there was a protective trend for women.
Conclusions
● There were no statistically significant associations between B6 vitamin intake and depression prevalence.
● Folate intake was inversely associated with depression prevalence among men, especially among smokers.
● B12 vitamin intake was inversely associated with depression among women, especially among smokers and physically active women.
● ω-3 fatty acids intake seems to be protective only among women.
● It is necessary to continue studying these associations in prospective analyses.





