Introduction
Depressive and anxiety disorders have been associated with excess mortality. The relative risk is higher for depressive disorders compared to anxiety disorders but due to higher prevalence rates of anxiety disorders, the population attributable risk (PAR) hardly differs with 4.9 and 4.3%, respectively [Reference Walker, McGee and Druss1]. Calculation of PARs assumes that associations of depressive and anxiety disorders with mortality are causal. Nonetheless, meta-analysis of 293 studies has questioned causality due to pronounced publication bias, inadequate control for comorbid mental disorders, heterogeneity with respect to confounder control, and overrepresentation of studies in specific medical patient groups [Reference Miloyan and Fried2]. Miloyan and Fried [Reference Miloyan and Fried2] showed that meta-analysis of the four studies that met their quality criteria, that is, using a Diagnostic and Statistical Manual of Mental Disorders (DSM)-based structured interview to assess depressive disorder in a population-based sample and based on survival analysis methodology, revealed a non-significant pooled hazard ratio of 1.17 (95% confidence intervals [CI]: 0.75–1.60) [Reference Miloyan and Fried2].
Still some arguments can be made in favor of causation. First, meta-analysis has demonstrated a dose–response relationship regarding excess mortality in subthreshold and major depression [Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx3]. Whereas this meta-analysis was based on unadjusted estimates, findings were confirmed by a recent study adjusted for lifestyle and multimorbidity [Reference CSh, Jin, Nyunt, Feng and Ng4]. Moreover, excess mortality associated with depression gradually decays over time unless a recurrent episode occurs [Reference Gilman, Sucha, Kingsbury, Horton, Murphy and Colman5]. Secondly, several explanatory mechanisms are biologically plausible. Lifestyle characteristics may mediate this risk since patients with affective disorders generally have a less healthy lifestyle [Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx6,Reference Schuch, Vancampfort, Firth, Rosenbaum, Ward and Reichter7]. In some studies, excess mortality due to depression perished after adjustment for lifestyle characteristics [Reference Chwastiak, Rosenheck, Desai and Kazis8]. Other studies still demonstrated excess mortality due to depression controlled for lifestyle characteristics [Reference CSh, Jin, Nyunt, Feng and Ng4,Reference Gilman, Sucha, Kingsbury, Horton, Murphy and Colman5]. These latter findings suggest a role for specific pathophysiological mechanisms like neurohormonal and immune-metabolic dysregulations [Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx6,Reference Cuijpers and Smit9–Reference Juruena, Bocharova, Agustini and Young11]. Finally, indirect evidence stems from a decreasing secular trend for excess mortality in depression. This may be explained by better chronic disease management of depression-associated somatic morbidity [Reference Gilman, Sucha, Kingsbury, Horton, Murphy and Colman5,Reference Jeuring, Comijs, Deeg, Hoogendijk, Beekman and Stek12], as depression is associated with the onset of many chronic diseases as well as physical frailty [Reference Wang, Li, Shi, Que, Liu and Lappin13–Reference Scott, Lim, Al-Hamzawi, Alonso, Bruffaerts and Caldas-de-Almeida15]. More than half of the studies examining the association between depression and mortality have been conducted in patient samples with a chronic somatic disease [Reference Miloyan and Fried2]. These diseases and side-effects of their treatment share many symptoms with depression (e.g., insomnia and fatigue). This easily confounds the association between depression and mortality when using self-report depression scales (as most of these studies did) instead of applying formal DSM-IV criteria in which symptoms originating from a somatic disease are not counted Reference Miloyan and Fried[2].
Physical frailty is characterized by a decline in functioning across multiple physiological systems and marks a condition of older people who have an increased risk on adverse health outcomes when facing an arbitrary stressor [Reference Hoogendijk, Afilalo, Ensrud, Kowal and Fried16]. The diminished ability to respond to stress can be conceived as a loss of redundancy due to the accumulation of multiple deficits with aging [Reference Rockwood and Mitnitski17]. To the best of our knowledge, only one cohort study has examined whether the effect of depression on mortality might be explained by frailty. In this Australian cohort study, a crude mortality hazard of 4.3 for depression was reported among males aged 75 years and over which dropped to 1.8 after additional correction for frailty [Reference Almeida, Hankey, Yeap, Golledge, Norman and Flicker18].
Aims of the study
The present study aims (a) to evaluate mortality risk of depressive and anxiety disorders, (b) to explore whether this risk is modified by age and sex, and (c) to evaluate whether the hypothesized mortality risk of depressive and anxiety disorders is independent of lifestyle characteristics and somatic health status within a large population-based study that met the quality criteria described by Miloyan and Fried [Reference Miloyan and Fried2].
Material and Methods
Lifelines
Lifelines is a multidisciplinary prospective population-based cohort study examining in a unique three-generation design the health and health-related behaviors of 167,729 persons aged from 6 months to 93 years living in the North of The Netherlands. It employs a broad range of investigative procedures in assessing the biomedical, behavioral, physical, and psychological factors which contribute to the health and disease of the general population, with a special focus on multimorbidity and complex genetics [Reference Scholtens, Smidt, Swertz, Bakker, Dotinga and Vonkd19].
The Lifelines Cohort Study is conducted according to the principles of the Declaration of Helsinki and in accordance with the research code of the University Medical Center Groningen (UMCG). All participants have signed informed consent prior to participation and the Lifelines study is approved by the medical ethical committee of the UMCG, The Netherlands.
Recruitment
People living in the Northern Netherlands were either invited by their general practitioner (GP) (in case aged 25–50 years) or self-registered at the Lifelines website (in case aged ≥18 years). People who had limited life expectancy due to severe illness, and who had insufficient knowledge of the Dutch language were excluded. After signing informed consent, participants received a baseline questionnaire and were invited for a physical examination and fasten blood collection at one of the Lifelines research sites. During these visits, participants were asked whether their family members would also be willing to participate. Overall, 49% of the participants (n = 81,652) were invited through their GP, 38% (n = 64,489) via participating family members, and 13% (n = 21,588) self-registered via the Lifelines website. Recruitment and baseline assessment of participants started in 2006 and were completed in 2013. The Lifelines adult study population is broadly representative for the adult population of the north of the Netherlands [Reference Klijs, Scholtens, Mandemakers, Snieder, Stolk and Smidt20]. Follow-up visits are scheduled every 5 years, and in between participants receive follow-up questionnaires.
For the present study, we a priori excluded participants aged below 18 years (n = 15,001) and those who had a Mini Mental State Examination score below 26 points, and therefore received a shortened assessment (n = 2,541), leaving a sample of 150,187 eligible participants.
Depressive and anxiety disorders
Current unipolar depressive disorder and anxiety disorders according to DSM-IV criteria were assessed at baseline with the Mini International Neuropsychiatric Interview (MINI). The MINI is a semi-structured interview with a good sensitivity and positive predictive value [Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller21]. In Lifelines, the sections on generalized anxiety disorder, panic disorder with or without agoraphobia, agoraphobia without panic disorder, social phobia, and depressive disorder were administered.
In addition, all participants were asked whether they ever had experienced a depressive and/or anxiety disorder during their lifetime.
All-cause mortality
Month and year of death up to October 2019 was retrieved by linkage with the national mortality data as collected in the database of Statistics Netherlands (see cbs.nl). This allowed us for all baseline participants to calculate survival rates by distracting the month and year of death by the month and year of the baseline assessment.
Covariates and explanatory variables
All covariates and explanatory variables were assessed at baseline. We included age, sex, and level of education as basic variables in all models. Education level was categorized in low (no or primary education), medium (lower/preparatory vocational education to intermediate vocational education/apprenticeship), and high education (higher secondary education to university) (included as dummies with low education as reference).
In subsequent models, we sequentially added lifestyle characteristics (model 1) and somatic health status (multimorbidity in model 2, and multimorbidity combined with frailty in model 3).
Lifestyle characteristics
We included body mass index (kg/m2), use of alcohol, smoking, and physical activity as lifestyle characteristics which might independently contribute to mortality rates. Body mass index was calculated by dividing the body weight (kg) by the squared body length in meters. Use of alcohol was classified as “drinking no alcohol at all,” as “using problematic levels of alcohol (≥21 drinks a week),” or in case neither of these categories applied to a person as “using moderate/social levels of alcohol.” Physical activity was measured with the SQUASH questionnaire [Reference Wendel-Vos, Schuit, Saris and Kromhout22], which measure physical activity in Metabolic Equivalent of Task (MET) minutes based on light, moderate, and heavy physical activity in leisure time, household activities, and job. Participants were classified as having sufficient physical activity or not according to the current Dutch norm on physical activity [Reference Miloyan and Fried2 Reference Miloyan and Fried2]. Self-report smoking data were classified as never, ever, or current.
Somatic health status
We included multimorbidity as well as physical frailty.
Multimorbidity
Chronic diseases were based on a self-report questionnaire. We explored the following nine disease clusters: (a) lung diseases (asthma and chronic obstructive pulmonary disease), (b) heart disease (myocardial infarction, established coronary artery disease, arrhythmias, heart failure, and aneurysm), (c) brain disorders (migraine, epilepsy, multiple sclerosis, spasticity, and Parkinson’s disease), (d) cerebrovascular disease (stroke and clinically relevant carotid stenosis), (e) gastrointestinal diseases (Crohn’s disease, ulcerative colitis, hepatitis, and liver cirrhosis), (f) kidney diseases, (g) endocrine diseases (thyroid disease and diabetes mellitus), (h) musculoskeletal disease (arthrosis, rheumatoid arthritis, and osteoporosis), and (i) cancer (any type). A multimorbidity score was calculated based on the sum of positive clusters (range 0–9).
Frailty
Frailty was operationalized according to the deficit accumulation model. This model postulates that the proportion of aging-related health deficits, that is, the Frailty Index (FI), reflects biological age over chronological age [Reference Hoogendijk, Afilalo, Ensrud, Kowal and Fried16]. As described previously, we constructed a Lifelines-FI based on 64 items regarding chronic somatic diseases (15 items), physical measures (5 items), disabilities (6 items), subjective health measures (8 items), sensory function (2 items), mental health indicators (4 items), neuropsychological markers (4 items), and blood biomarkers (15 items) [Reference Oude Voshaar, Jeuring, Borges, van den Brink, Marijnissen and Hoogendijk23]. Following the guidelines for the construction of an FI by Searle et al. [Reference Searle, Mitnitski, Gahbauer, Gill and Rockwood24], these health deficits were included in the Lifelines–FI, because they (a) were biologically meaningful in representing several organ systems, (b) accumulate with age, but were not too prevalent at some younger age, and (c) had less than 5% missing values. Each deficit was coded as 0 (absence) or 1 (presence) or when clinically relevant, as any number between 0 and 1. This procedure has resulted in a baseline Lifelines-FI consisting of 64 items Reference Miloyan and Fried[2 Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx3]. In order to prevent confounding with either depressive or anxiety disorders, we have recalculated the FI excluding all mental health variables, that is, (a) feeling depressed in the past 2 weeks, (b) loss of interest/anhedonia in the past 2 weeks, (c) feeling happy, and (d) feeling nervous. This resulted in a 60-item FI used in the present paper.
Statistical analyses
Multivariable Cox proportional hazard models were fitted to study the association between depressive and anxiety disorders and all-cause mortality adjusted for age, sex, and level of education. Hazard ratios (HR) and 95% confidence intervals (95% CI) were calculated for each depressive and/or anxiety disorder. Survivors were censored at end of follow-up. The proportional hazard assumption was checked by inspecting whether the hazard plots showed approximately parallel and not-crossing lines. Three-way interaction terms with age and sex were tested, as well as two-way interaction terms with either age or sex in case of nonsignificant three-way interactions. In case of significant interaction terms, results were stratified by either sex, age, or both. Since the number of deceased persons was low in the younger age groups, age-stratified analyses were conducted using a cut-off value of 60 years.
Subsequently, we tested models additionally adjusted for (a) lifestyle characteristics as described above, (b) multimorbidity (disease count), and (c) frailty (60-item Lifelines-FI). Since the number of some specific anxiety disorders were rather small, we lumped all anxiety disorders into one category of the presence of “any anxiety disorder” in these latter analyses. All analyses were performed using SPSS version 25. Missing values on covariates (see Table 1) were excluded list wise. All p values were two-tailed, and significance level was set at p < 0.05.
Table 1. Baseline characteristics of study sample (n = 141,337).

* Number of missing values: Level of education, n = 369 (0.3%); social phobia, n = 1 (<0.1%); any anxiety disorder, n = 1 (<0.1%); smoking, n = 719 (0.5%); sufficient physical activity, n = 11,175 (7.9%); body mass index, n = 43 (<0.1%).
Abbreviation: SD, standard deviation.
Results
Sample characteristics
Of the 150,187 eligible Lifelines participants, a total of 7,157 persons were excluded due to missing values with respect to the FI index and another 2,653 due to missing data on the psychiatric interview (MINI), leaving a final study sample of 141,377 persons. These study participants (58.4% females) were on average 44.5 (standard deviation 12.8) years old. Table 1 presents all other baseline characteristics.
Mortality
A total of 2,068 (1.5%) participants died during a mean follow-up up of 8.3 years (standard deviation 1.5; range 3.0–13.7 years). Among younger people <60 years, a total of 449/49,777 (0.9%) males and 459/71,990 (0.6%) females died during follow-up. Among older people, 704/9,013 (7.8%) males died and 456/10,597 (4.3%) females during follow-up.
We did not find significant three-way interaction terms of age by sex with either any of the current or lifetime depressive and/or anxiety disorders. Subsequently, we tested two-way interaction terms of all affective disorders with age as well as with sex separately. Whereas sex did not interact with any affective disorder on the prediction of mortality, we found significant interaction terms between age and each affective disorder, except social phobia (p = 0.064) and panic disorder (p = 0.655).
Table 2 shows the hazard rate of affective disorders for mortality for younger and older people separately. Adjusted for age, sex and level of education, depressive disorder, and all anxiety disorders were associated with an increased risk of premature mortality in younger people (<60 years). When all psychiatric disorders were tested simultaneously in one model, only depressive disorder and panic disorder remained statistically significant.
Table 2. Hazard ratios of current and life-time affective disorders for younger (n = 121,643) and older (n = 19,365) persons for mortality, adjusted for age, sex, and level of education.
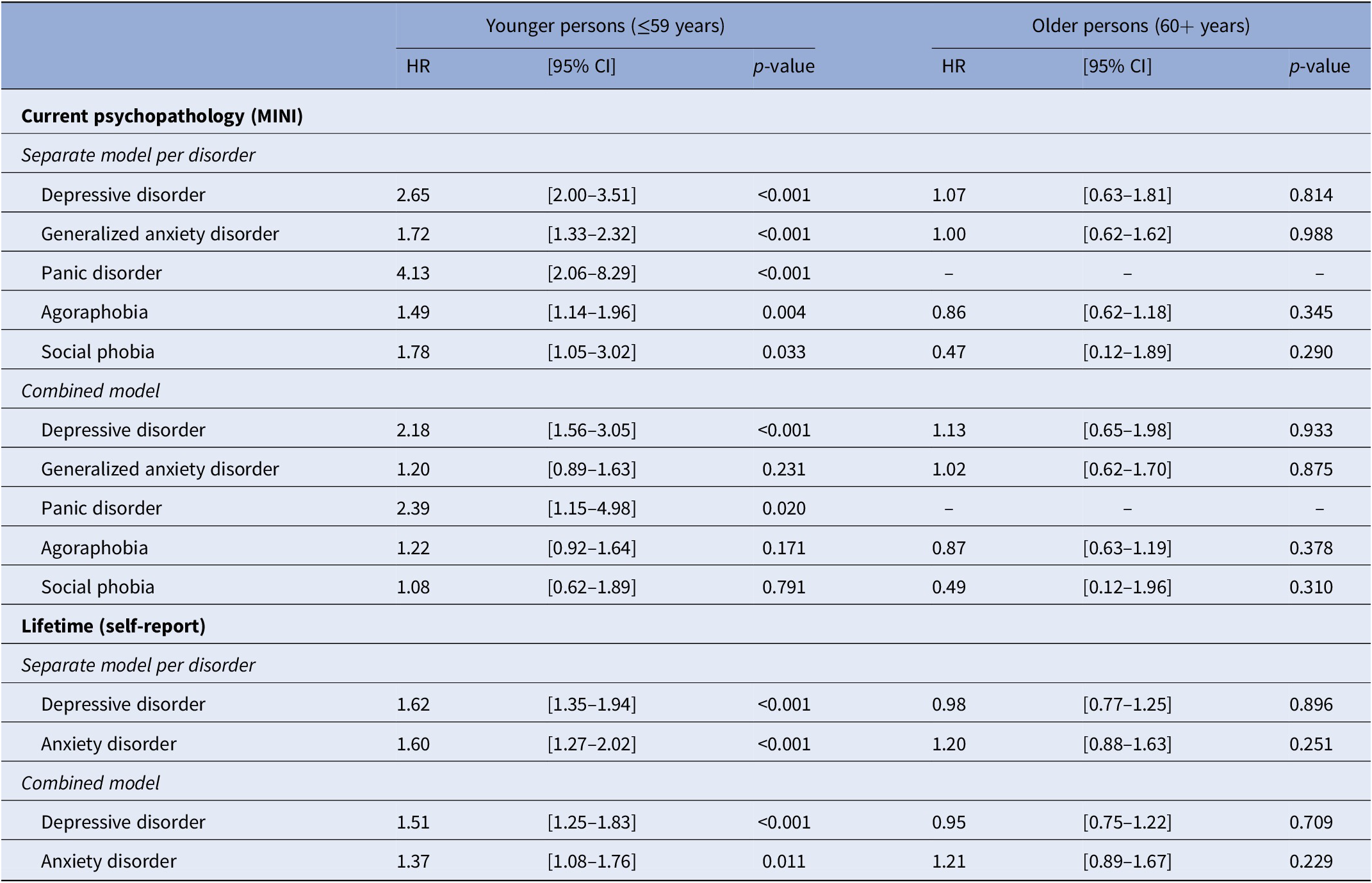
Abbreviations: CI, confidence intervals; HR, hazard ratio.
None of the affective disorders was associated with an increased mortality risk among older people (≥60 years).
Regarding the lifetime diagnoses, similar age-effects were found. In younger people the presence of depressive disorder and of any anxiety disorder were independent of each other associated with an increased mortality risk (see Table 2).
Explanatory models for excess mortality in depression
Table 3 presents three different statistical models: model 1 is adjusted for socio-demographic characteristics as well as lifestyle characteristics; model 2 is additionally adjusted for multimorbidity, and finally model 3 is additionally adjusted for frailty. To facilitate interpretation, multimorbidity had a HR of 1.22 (95% CI: 1.17–1.27; p < 0.001) for mortality adjusted for demographic and lifestyle characteristics, which became non-significant after additional adjustment for frailty (HR = 1.04 [95% CI: 0.99–1.09]; p = 0.142). In this latter model, the FI significantly predicted mortality (HR = 1.05 [95% CI: 1.04–1.06]; p < 0.001). These results did not differ by age.
Table 3. Hazard ratios of depression and anxiety (current and lifetime) for mortality in younger persons (n = 111,954) and in older persons (n = 17,886).

Abbreviations: CI, confidence intervals; HR, hazard ratio; MDD, major depressive disorder.
a Adjusted for age, sex and level of education, and lifestyle (alcohol, smoking, physical activity, and BMI).
b Adjusted for same covariates as model 1, including multimorbidity.
c Adjusted for same covariates as model 1, including multimorbidity and frailty.
In younger people, the hazard ratio of a current depressive disorder for mortality, adjusted for socio-demographics and comorbid anxiety disorders, hardly changed when adjusted for lifestyle characteristics, but decreased slightly when additionally adjusted for multimorbidity and even more when adjusted for frailty. In the latter model, a current depressive disorder remained independently associated with mortality (HR = 1.56 [95% CI: 1.12–2.19]; p = 0.010), whereas the presence of a lifetime depressive disorder did not. The impact of anxiety disorders on mortality in younger people was not significant anymore after adjustment for lifestyle characteristics.
In older people, depressive disorder, both current and lifetime, were not associated with mortality in any of the models. A small protective effect was seen for the presence of any anxiety disorder when adjusted for lifestyle characteristics, multimorbidity and frailty (HR = 0.97 [95% CI: 0.95–1.00]; p = 0.029).
Discussion
Main findings
Within a population-based sample of 141,337 people, we confirmed that depressive and anxiety disorders according to DSM criteria are associated with increased mortality rates in younger people. Our data shed more light on some gaps and inconsistencies in the literature. First, we did not find any sex differences [Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx6]. Secondly, the impact of depressive and anxiety disorders on mortality disappeared after the age of 60 years [Reference Machado, Veronese, Sanches, Stubbs, Koyanagi and Thompson25]. Thirdly, regarding explanatory mechanisms, we found that among younger persons the hazard ratios decreased but remained statistically significant when adjusted for lifestyle characteristics and multimorbidity [Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx6]. After additional adjustment for frailty, only a current but not a lifetime depressive disorder remained significantly associated with excess mortality in younger people.
Age- and sex specific effects of affective disorders on mortality
Age-effects in the association between affective disorders and mortality have not yet been examined by meta-regression [Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx3,Reference Machado, Veronese, Sanches, Stubbs, Koyanagi and Thompson25–Reference Miloyan, Bulley, Bandeen-Roche, Eaton and Gonçalves-Bradley27]. Individual studies examining age-effects in samples with both younger and older people are scarce and inconsistent. Among patients with severe depression the association with mortality was highest in younger people [Reference Laursen, Musliner, Benros, Vestergaard and Munk-Olsen28], whereas among patients with diabetes mellitus, the association between depressive disorder and mortality was highest in older people [Reference Kimbro, Mangione, Steers, Duru, McEwen and Karter29]. Furthermore, among diabetes patients, meta-regression of nine studies showed that neither age nor sex interacted with comorbid depression on cardiac mortality [Reference Farooqi, Khunti, Abner, Gillies, Morriss and Seidu30]. An individual patient data (IPD) meta-analyses among older persons (≥65 years), however, revealed an interaction between age and depressive symptoms on mortality with highest mortality rates in the youngest old [Reference Eurelings, van Dalen, Ter Riet, Moll van Charante, Richard and van Gool31]. Two explanations might have contributed to the discrepancy with our data. First, the IPD meta-analysis was not adjusted for lifestyle characteristics. Second, only studies who had assessed depression with the self-report Geriatric Depression Scale (GDS) were included. The GDS score may be falsely inflated due to underlying (sometimes subthreshold) somatic diseases [Reference Eurelings, van Dalen, Ter Riet, Moll van Charante, Richard and van Gool31,Reference Benedetti, Wu, Levis, Wilchesky, Boruff and Loannidis32].
We did not find any impact of current affective disorders on excess mortality in later life. One explanation may be that people with affective disorders have died earlier and that the background rate of mortality among older people without mental illness starts to catch up with people with affective disorders as the whole sample ages. In line with this reasoning, meta-regression has shown that the mortality rate associated with mental disorders decreases with a longer duration of follow-up [Reference Walker, McGee and Druss1]. Another explanation might be excessive use of antidepressants beyond the presence of current affective disorders. Among 121,252 patients with heart failure, both a clinical diagnosis of depression as well as antidepressant drug use were independently associated with increased mortality rates, whereas only 13.3% patients receiving antidepressants suffered from a diagnosis of clinical depression [Reference Brouwers, Christensen, Damen, Dennollet, Torp-Pedersen and Gislason33]. Finally, due to the large age range of the Lifelines cohort generational differences (cohort effects) cannot be excluded. A secular trend of increased life-expectancy may also explain age differences, in particular a secular trend due to increased awareness and improved treatment of depression in more recent calendar periods. In the three cohorts of the Sterling County Study, the association between depressive disorder and mortality among adults has indeed decreased in more recent cohorts, with a HR of 2.90 in the 1952 cohort, 1.97 in the 1970 cohort, and 1.52 in the 1992 cohort [Reference Gilman, Sucha, Kingsbury, Horton, Murphy and Colman5]. Finally, the number of older participants might have been too small in our sample to identify small effects. A recent population-based cohort study based on Danish registries including over 7 million people showed that mortality rates are higher for people with a mental disorder registered in a hospital, outpatient, and/or emergency setting compared to people without a mental disorder [Reference Plana-Ripoll, Pedersen, Agerbo, Holtz, Erlangsen and Canudas-Romo34]. This study, however, showed that the highest mortality rates ratios and largest sex-differences were found among people aged 30–40 years Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx[3 Reference CSh, Jin, Nyunt, Feng and Ng4]. Since we had only few events (deaths) in this age-range, our statistical power was too low to detect a sex-difference. Interestingly, in this registry study, the mortality rate ratios for people with mental disorders declined with increasing age, in line with our findings and those of a Spanish cohort study (n = 4,583 people aged 18+) who also did not find any impact of depressive disorder on mortality in people aged above 65 years [Reference Cabello, Borges, Lara, Olaya, Martín-Maria and Moreno-Agostino35]. Nonetheless, in the Danish registry study, the mortality rate ratio of mood disorders remained elevated up to the age of 95 years. Explanatory variables like lifestyle are not available in registry-based studies Reference Cuijpers, Vogelzangs, Twisk, Kleiboer, Li and Penninx[3 Reference CSh, Jin, Nyunt, Feng and Ng4]. The lower mortality rates with increasing age and the lack of any association with excess mortality among older persons as we found, also fits with findings of the Netherlands Study of Depression in Older persons, one of the largest clinical cohort studies on late-life depression. In that study, 6-year mortality rates were significantly higher among 378 extensively phenotyped depressed patients compared to 132 never depressed controls. While this association lost statistical significance after correction for lifestyle and physical functioning [Reference Jeuring, Stek, Huisman, Oude Voshaar, Naarding and Collard36,Reference van den Berg, Wiersema, Hegeman, van den Brink, Rhebergen and Marijnissen37], which may partly be due to lack of statistical power, the frailty phenotype still predicted excess mortality in this cohort of depressed patients [Reference Arts, van den Berg, Marijnissen, de Jonge, Hegeman and Collard38].
Differential and/or independent effects of depression and anxiety disorders on mortality
While comorbidity between affective disorders is rather the rule than the exception, studies on mental multimorbidity lag behind knowledge on somatic multimorbidity. Interestingly, only 16 out of 293 studies on the association of depression with mortality have adjusted their results for at least one comorbid mental condition [Reference Miloyan and Fried2]. Meta-analyses of these 16 studies did not find an association between depression and excess mortality.
Meta-analysis on the association between anxiety disorders and excess mortality demonstrated a significant association, but this association lost significance after correction for publication bias [Reference Miloyan, Bulley, Bandeen-Roche, Eaton and Gonçalves-Bradley27]. Even without correction for publication bias, neither population-based samples nor studies that adjusted for depression could demonstrate any association between anxiety and excess mortality. This is in line with our findings, as only lifetime anxiety disorders were independent of depressive disorder associated with increased mortality rates among younger persons, but this effect was lost after correction for lifestyle characteristics. Nonetheless, a large registry-based population study showed that many psychiatric comorbidity patterns were associated with excess mortality compared to pure psychiatric diseases. Although anxiety disorders were grouped within the larger subgroup of neurotic/stress/somatoform disorders, this subgroup as well as the mood disorder subgroup were independently associated with excess mortality and had increased mortality rates when comorbid to each other [Reference Plana-Ripoll, Musliner, Dalsgaard, Momen, Weye and Christensen39].
Underlying pathways linking affective disorders to excess mortality
The mechanisms by which affective disorders are related to mortality are unknown. Conceivably, both causal and noncausal effects may play a role. In our study, the associations could not be fully explained by an adverse lifestyle of depressed people. One explanation for excess mortality in affective disorders is that these disorders might exacerbate outcomes particularly among individuals with poorer health. For example, anxiety as well as depression is associated with increased risk of incident cardiovascular and metabolic diseases [Reference Roest, Martens, de Jonge and Denollet40,Reference Scott41]. Moreover, most previous studies on the impact of depression on mortality have been conducted in medical populations [Reference Miloyan and Fried2]. Reverse causality cannot be ruled out in medical patients, as recently demonstrated for cancer patients [Reference Wang, Li, Shi, Que, Liu and Lappin13]. In our study, the impact of life-time depression on mortality lost significance after adjustment for a simple disease count as measure for multimorbidity, where the associations with current depressive disorders decreased but remained statistically significant when additionally adjusted for multimorbidity and frailty. This is in line with the only cohort adjusting the association between depressive disorder and excess mortality for frailty, which still found an independent effect of depression [Reference Almeida, Hankey, Yeap, Golledge, Norman and Flicker18]. Since frailty and depression are reciprocally related [Reference Soysal, Veronese, Thompson, Kahl, Fernandes and Prina42] and depression is assumed to emerge earlier in life (mean age of onset around 30 years), it is likely that frailty is a mediating pathway by which depression leads to increased mortality rates. This might also explain why a lifetime diagnosis is not significantly associated with mortality when adjusted for frailty, whereas a current depressive episode might be.
Methodological considerations
A strength of the Lifelines cohort study is the large sample size which is representative for the Dutch population in the Northern Netherlands [Reference Klijs, Scholtens, Mandemakers, Snieder, Stolk and Smidt20]. In the present study, 141,337 people of the 150,187 eligible people were included (94.1%). Another strength of our study is the assessment of depressive and anxiety disorders with a semi-structured interview, which may be more valid compared to self-report data and/or registries. Nonetheless, a weakness may be that we only assessed current disorders, whereas most epidemiological studies are based on a past-year diagnosis of either anxiety or depressive disorders. Whereas anxiety disorders are based on 6-month periods (except panic disorder), a depressive episode requires only 2 weeks. While this may have underestimated the effect of current disorders, bias might be minor as depressive episodes in the general population have a median duration of 6 months [Reference ten Have, Penninx, Tuithof, van Dorsselaer, Kleinjan and Spijker43]. Secondly, lifetime diagnoses were based on self-report data. This may differentially impact on younger and older patients due to recall bias as well as due to more accurate mental health diagnostics over the years. Nonetheless, the null finding in the older age group was found for both, a current as well as a lifetime diagnosis. Thirdly, multimorbidity was operationalized as a disease count instead of having two or more diseases. Although this operationalization does not reflect multimorbidity by definition, it precludes residual confounding due to dichotomization. Finally, the duration of follow-up (range 3–13.7 years) was relatively short which has resulted in a low overall mortality rate. This may have reduced the power for the three-way interaction effects and may have masked some minor sex-differences.
Conclusions
Depressive and anxiety disorders, in particular depression, are associated with excess mortality in younger adults, independent of lifestyle characteristics. Since the effect of a current depressive disorder substantially decreases after adjustment for multimorbidity and frailty and of a lifetime diagnosis even lost statistical significance, may suggest that the onset of somatic morbidity and frailty are mediating pathways. Whether depression in a medical context should be considered a comorbid disorder interacting with a patients’ physical state that results in excess mortality or whether depression is simply an indicator of a more severe somatic condition deserves further study. Regarding the numerous studies on the association between affective disorders and excess mortality, meta-regression to study these associations in specific subgroups defined by age and relevant somatic comorbidity may shed some light on this clinically important distinction.
Acknowledgments
The authors wish to acknowledge the services of the Lifelines Cohort Study, the contributing research centers delivering data to Lifelines, and all the study participants.
Conflicts of Interest
The authors have no personal or financial conflicts of interest.
Financial Support
The Lifelines Biobank initiative has been made possible by subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen (UMCG the Netherlands), University Groningen and the Northern Provinces of the Netherlands.
Author Contributions
All authors satisfy the four conditions of the ICMJE for an authorship by having substantially contributed to the concept of the study, interpretation of the data, critical revision of the article, approval of the final version, and agreed to be accountable for all aspects of the work. Data analysis: R.C.O.V., M.K.B., and R.H.S; Drafting the first version of the manuscript: R.C.O.V. and I.A. Research supervision: H.W.J.
Data Availability Statement
The data that support the findings of this study are available by Lifelines (see www.Lifelines.nl/researchers). Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the corresponding author with the permission of Lifelines.






Comments
No Comments have been published for this article.