1. Introduction
The increase in suicide rates in U.S. military personnel since 2003 has been dramatic [Reference Archuleta, Jobes, Pujol, Jennings, Crumlish and Lento1, Reference Nock, Stein, Heeringa, Ursano, Colpe and Fullerton2] even compared to the steady increase in suicide rates of the general U.S. population [Reference Kochanek, Murphy, Xu and Tejada-Vera3]. Much effort has been expended to identify risk factors for preventing suicide in the U.S. military [Reference Alexander, Reger, Smolenski and Fullerton4], and many prevention strategies have been employed. Some of the programs were quite successful as for example, a program implemented in the air-force [Reference Knox, Pflanz, Talcott, Campise, Lavigne and Bajorska5] and in other units [Reference Ramchand, Acosta, Burns, Jaycox and Pernin6]. However, the suicide rate in the US military as a whole is still fairly constant. In contrast, in the Israel Defense Forces (IDF) the suicide rate has declined for the last 6 years [Reference Rosenbaum7, Reference Shelef, Tatsa-Laur, Derazne, Mann and Fruchter8] by almost 50%. Understanding the reasons for these trends may help improve suicide prevention approaches in the military sector and may have implications for preventing civilian suicides.
In the IDF suicides and suicide attempts occur mostly 6 to 12 months after induction into military service [9–Reference Shelef, Tomer, Tatsa-Laur, Kedem, Bonne and Fruchter11]. One explanation for this timing of suicide attempts is that adjustment to military service, which is very different from civilian life, is a major stressor [Reference Bodner, Ben-Artzi and Kaplan12]. One expects this effect to be most obvious during the first six months of service, thus it is clear that additional factors are at work. Studies indicate that untreated psychiatric disorders play a critical role in suicidal behavior [Reference Joiner, Buchman-Schmitt and Chu13], among both, Israeli [Reference Shelef, Tatsa-Laur, Derazne, Mann and Fruchter8, Reference Shelef, Tomer, Tatsa-Laur, Kedem, Bonne and Fruchter11] and U.S. military personnel [14–Reference Nock, Dempsey, Aliaga, Brent, Heeringa and Kessler17].
Suicide risk assessment in both civilians [Reference Mann, Apter, Bertolote, Beautrais, Currier and Haas18, Reference Rudd and Nock19] and soldiers [Reference Nock, Deming, Fullerton, Gilman, Goldenberg and Kessler14] is one of the most challenging tasks in clinical practice. Suicide risk is dynamic [Reference Wolfe-Clark and Bryan20], fluctuating in response to both external events and internal subjective emotions and thoughts as well as over time. That makes predicting imminent risk of suicidal behavior difficult [Reference Bryan and Rudd21].
To date, few studies have focused on defining measures that can best differentiate those who make severe suicide attempts from those who make suicide attempts of mild-moderate severity [Reference Oquendo, Halberstam, Mann and First22]. A recent study found that the most powerful predictors of a first nonfatal suicide attempt among soldiers are: recent onset of ideation, presence and recent onset of a suicide plan, low control over suicidal thoughts and extreme risk-taking or “tempting fate.” The most innovative and interesting finding however, was “failure to answer questions about the characteristics of one’s suicidal thoughts [Reference Nock, Millner, Joiner, Gutierrez, Han and Hwang23].
The authors published recently a study reporting on three rating scales used in assessing soldiers who attempted suicide and soldiers with non-suicidal self-injury in the IDF [Reference Chiurliza, Gutierrez, Joiner, Hanson, Ben-Yehuda and Tatsa-Lauer24]. The tools used included the scale for suicide Ideation (SSI) [Reference Beck, Kovacs and Weissman25], the suicide intent scale (SIS) [Reference Beck, Schuyler, Herman, Beck, Resnick and Lettieri26] and the Columbia suicide severity rating scale (C-SSRS) [Reference Oquendo, Halberstam, Mann and First22, Reference Posner, Brown, Stanley, Brent, Yershova and Oquendo27]. The scales were analyzed using only data from soldiers’ medical files. The current study examines the association of these three scales with moderate vs. severe suicide attempts using live interviews with people in the military setting, 1–2 months after the suicide attempt. Examining the moderate and severe nonfatal attempts is crucial for suicide prevention since nonfatal suicide attempt severity indicates the risk for future suicide [Reference Bergen, Hawton, Waters, Ness, Cooper and Steeg28, Reference Borges, Nock, Haro Abad, Hwang, Sampson and Alonso29].
2. Methods
2.1 Settings and procedure
At recruitment, each candidate is assigned a medical profile, indicating physical and mental suitability for military service [Reference Joiner, Buchman-Schmitt and Chu13, Reference Goldberg, Fruchter, Davidson, Reichenberg, Yoffe and Weiser30]. Previous mental health history or mental disorders influence the determination of the soldier's suitability for service. The mental profile codes range from mild problems in functioning through moderate ones to major and debilitating disease (severe). While soldiers with severe previous psychiatric diagnoses (i.e. major depression, bipolar disorder, psychosis or suicidality) are excluded from service, soldiers with psychiatric disorders of mild or moderate severity are monitored by mental health professionals during their military service via mandatory periodic follow-up examinations [Reference Shelef, Laur and Fruchter10].
In addition the Military Adjustment Scale is used in order to assess the soldiers' ability to adjust to the difficulties of military service. This assessment is based on past experiences with adjustment to new environments, as for example in the context of schools. This scale is completed by a mental health professional, and assists in assigning the soldier to a suitable military placement [Reference Bodner, Ben-Artzi and Kaplan12]. In this context “adjustment difficulties” consist of a combination of personality traits, limited functionality and low adaptability to military service [Reference Shelef, Tomer, Tatsa-Laur, Kedem, Bonne and Fruchter11].
Following a suicide attempt, a soldier goes through a full psychiatric evaluation [Reference Shelef, Kaminsky, Carmon, Kedem, Bonne and Mann9] that includes: 1) categorizing the recent suicide attempt into mild, moderate or severe, based on the intent to die, medical lethality of the attempt, and assessed risk for another suicide attempt; 2) psychiatric diagnosis according to ICD-10 [Reference Goldberg, Fruchter, Davidson, Reichenberg, Yoffe and Weiser30, Reference World Health Organization31]; 3) assessment of level of functioning as a soldier (i.e. severe, moderate or mild impairment). It should be noted that following a suicide attempt, between 45–50% are discharged from military service [Reference Chiurliza, Gutierrez, Joiner, Hanson, Ben-Yehuda and Tatsa-Lauer24]. The others continue their military service supervised by a mental health officer.
2.2 Data collection
Data collection for the current study took place between June 2012 and October 2013 (16 months). Included were soldiers who had attempted suicide during the three months prior to completing the rating scales, were hospitalized for at least 24 h in wake of this attempt [Reference Beautrais32] and had been evaluated as being at high risk by a mental health officer [Reference Shelef, Kaminsky, Carmon, Kedem, Bonne and Mann9]. Each soldier was examined by a military psychiatrist immediately after returning to his or her regular military service, in order to reassess his or her mental state and functionality profile, whereby to determine a suitable military assignment [Reference Shelef, Kaminsky, Carmon, Kedem, Bonne and Mann9].
Data on the suicide attempters were retrieved using the Human Resource IDF database. The IDF computerized database provided the data on date of recruitment, military occupation, intelligence rating score and mental health. The retrieved health records included medical history of the soldier, as well as a summary of the medical examination results and the suggested treatment [Reference Shelef, Kaminsky, Carmon, Kedem, Bonne and Mann9].
2.3 Study population
Within the study period, 81 soldiers were hospitalized as a result of attempting suicide. Of those, 32 were immediately discharged as being unfit for further military service and therefore could not be included in the study. Of 49 soldiers who attempted suicide and stayed in the army for at least another month, in 39 the risk of another suicide attempt was defined as being moderate to severe. These 39 soldiers were included in the study and were divided into the two following groups based on the psychiatric evaluation:
a) Severe suicide attempters (n = 15, 38.5%): This categorization was based on a major psychiatric analysis and on inability to function as a soldier. When determining the lethality of a suicide attempt the psychiatric analysis included “potential lethality”, namely, in cases of threat of attempting suicide that was not realized, the potential for death if the suicidal attempt had been realized. For example, when a soldier points his weapon at himself but ultimately does not shoot [Reference Posner, Brown, Stanley, Brent, Yershova and Oquendo27].
b) Moderate suicide attempters (n = 24, 61.5%): This categorization was based on the lethality level of the suicide attempt and included potential lethality [Reference Posner, Brown, Stanley, Brent, Yershova and Oquendo27] as well as being unable to function as a soldier.
2.4 Measures
2.4.1 Demographic variables
Socioeconomic status was determined by location of residence (low, medium and high).
Intelligence rating score (IRS) [Reference Bodner, Ben-Artzi and Kaplan12]: also referred to as Scholastic Ability (SA) score, is an independent scale that includes a cognitive test composed of four sub-tests measuring intellectual ability. The total score is a highly valid measure of general intelligence and is equivalent to a normally distributed IQ score [Reference Goldberg, Fruchter, Davidson, Reichenberg, Yoffe and Weiser30]. The soldiers were divided into three groups according to their SA score (low, average and high).
2.4.2 Psychological variables
Psychiatric diagnoses-a psychiatric diagnosis is given, when needed, by a military psychiatrist prior to enlistment or during the military service as described above. Mental health diagnosis is based on the ICD-10 [Reference Shelef, Kaminsky, Carmon, Kedem, Bonne and Mann9, Reference Shelef, Tomer, Tatsa-Laur, Kedem, Bonne and Fruchter11]. This diagnosis is translated into a medical profile to which is added the ability to function as a soldier (classified into one of three levels of severity: mild, moderate or severe). Those diagnosed with high severity illness are not inducted into military service or are discharged from it. Those diagnosed with a mild or moderate psychiatric diagnosis continue the induction process. Despite IDF service being compulsory, people with severe mental disorders (major depression, psychosis or suicidality) are not enlisted. People with mild mental disorders (e.g. anxiety, depression, eating disorders), however, are recruited into military service but are monitored by military mental health professionals [Reference Shelef, Kaminsky, Carmon, Kedem, Bonne and Mann9, Reference Shelef, Laur and Fruchter10]. Additional data that was collected from medical records included: past psychological therapy, previous suicide attempts, alcohol use, past unauthorized absence from service, number of primary care physician (PCP) visits and number of mental health officer visits.
2.4.3 Suicidal measures
2.4.3.1 Scale for suicide ideation (SSI) [Reference Beck, Kovacs and Weissman25]
The SSI is a 19-item self-report measure designed to assess suicidal thoughts, plans, and intent to die by suicide. The first five items are screening items, and the last two are items assessing past attempts and intent. Each item's scoring ranges from 0 to 2 on a three-point scale, resulting in an overall score in the range of 0 to 38. The SSI has shown strong psychometric properties in previous studies [Reference Beck, Kovacs and Weissman25]. Cronbach’s alpha coefficient α = 0.90 was previously reported [Reference Beck, Steer and Ranieri33].
In interpreting the SSI's results, the higher the total score the greater the risk of future suicide [Reference Beck, Kovacs and Weissman25]. In adults, a score of 6 or more has been used as a cutoff point for clinically significant suicidal ideation [Reference Holi, Pelkonen, Karlsson, Kiviruusu, Ruuttu and Heila34, Reference Sokero35].
2.4.3.2 The suicide intent scale (SIS) [Reference Beck, Schuyler, Herman, Beck, Resnick and Lettieri26]
This scale has 15 items. A factor analysis identified two factors: objective intent and subjective intent. Items 1–9 are about the circumstances related to suicidal attempt, and deal mainly with observable aspects of the attempt and the events surrounding the individual. Items 10–15 are self-reported and are used to score thoughts and feelings at the time of the attempt [Reference Beck, Schuyler, Herman, Beck, Resnick and Lettieri26]. The final score is the total of all individual item scores. Cronbach’s alpha coefficient is high: α = 0.95 [Reference Beck and Steer36].
2.4.3.3 The Columbia suicide severity rating scale (C-SSRS)
This scale quantifies both, suicidal ideation and behaviors. A higher score indicates greater severity. The C-SSRS was administered as a semi-structured interview. Evidence of reliability and validity can be found in publications by Posner and colleagues [Reference Posner, Brown, Stanley, Brent, Yershova and Oquendo27]. The first 5 items of the scale refer to suicide ideation and have binary yes/no responses. The next 5 items deal with the intensity or level of suicidal ideation. Their responses range from 0 (suicidal ideation denied) to 5 (suicidal ideation with a plan, i.e. severe suicidal ideation). These items assess frequency, duration, controllability and deterrents of ideation as well as reasons for ideation. The total score reflects only the items whose scoring is bigger than 0 and it thus ranges from 1 to 25.
Two scores are created for each patient, one for ideation and one for intensity. Next, the two means for these characteristics are calculated within each of the attempt-severity groups (i.e. moderate attempt and severe attempt) and a comparison is done between the means of each characteristic (Table 2). Cronbach's alpha coefficient was previously reported as being α = 0.80 for severity ideation and α = 0.67 for intensity [Reference Chiurliza, Gutierrez, Joiner, Hanson, Ben-Yehuda and Tatsa-Lauer24].
2.4.4 Statistical analyses
Analyses were done using IBM SPSS, version 21.
The analyses consisted of three statistical procedures: (1) A one dimensional analysis of all characteristics in the severe and the non-severe suicide attempter groups. Fisher’s Exact Test was used to assess differences in categorical variables between the severe attempters and the non-severe attempters. The ordinal Scale Score means (C-SSRS, SSI, SIS etc.) were tested with more than two groups of categorical variables. Each group was compared to the other groups by Scheffe's Post-Hoc Multiple comparison. Where results were significant, post-hoc tests were used to examine the source of the differences. (2) Mantel-Haenszel Common Odds Ratio Estimate and Relative Risk were determined for each characteristic. (3) Kendall's tau-b correlation with Bootstrap was used to compare the performance of the three scales. All significance levels were two-tailed. An exploratory analysis evaluated each of the items in the three scales searching for significant correlations with severity of suicide attempt, by using Kendoll's Tau-b test for dichotomous variables (0 = non-severe,1 = severe).
Due to the sample size, (n = 39) the tests could not be done using a multivariate model and were thus carried out using a single-level variable approach. Kendall's tau-b correlation with 500 Bootstrap was used in order to reduce the possibility of statistical error. For stability of Kendall's tau b correlation, testing was done between each of the indices "risk of suicide" and "socio-demographic" and between the dependent variable "severity of suicidal attempt".
2.4.5 Ethical approval
The IDF Medical Corps Institutional Review Board approved the study and all participants singed an informed consent form after the nature of the study was explained to them.
3. Results
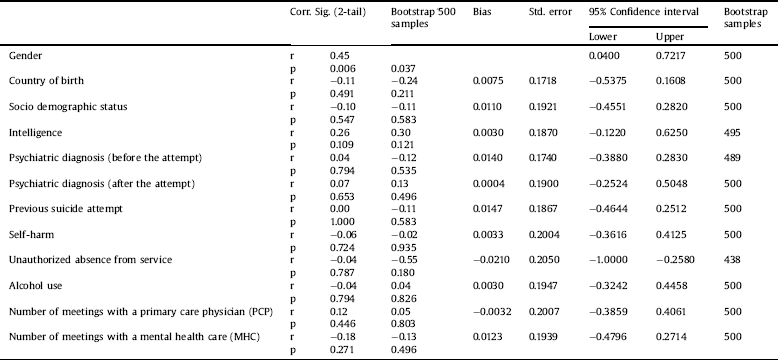
Demographic and clinical characteristics of the two study groups (n = 39) are presented in Table 1. The groups did not differ in any of the characteristics assessed except for gender ratio, namely, as expected more males were in the serious suicide attempt group (p = 0.008).
Suicidal soldiers from both groups served an average of 12.5 months (SD = 8.3) prior to the suicide attempt. Most (n = 34, 87.1%) were born in Israel, 12.8% served in combat units, 74.3% had low to average intelligence scores and 54.1% came from low to average socio demographic background. Before the suicide attempt 18.1% had a psychiatric diagnosis and 33.3% had attempted suicide previously. Non-suicidal self-injury was reported by 43.6% of the soldiers.
Table 1 Demographic and clinical characteristics of moderate vs. severe suicide attempters in a military setting.

* Fisher’s Exact Test: p < 0.05.
3.1 Correlations with severe suicide attempt
Kendall's tau-b correlations between the individual scale items and severe suicide attempt found the following:
In the SSI scale, 7 significant items correlated with severe suicide attempts: Item No. 2 – “Wish to die” (r = 0.305, p = 0.046); Item No. 3 – “Reasons for living/dying” (r = 0.31, p = 0.044); Item No. 5 – “Passive suicidal desire” (r = 0.30, p = 0.05); Item No 6. – “Time dimension: Duration of suicide ideation/wish” (r = 0.345, p =.05); Item No 10. – “Deterrents to active attempt (e.g., family, religion, irreversibility)” (r = 0.36, p = 0.05); Item No 15. – “Expectancy/anticipation of actual attempt“(r = 0.432, p = 0.015); and Item No 16. – “Actual preparation for contemplated attempt” (r = 0.489, p = 0.007) [Reference Chiurliza, Gutierrez, Joiner, Hanson, Ben-Yehuda and Tatsa-Lauer24].
The SIS scale includes 2 items that correlated with severe suicide attempts: Items No. 6 – “Active Preparation for Attempt” (r = 0.348, p = 0.031) and item No. 14 “Conception of medical Reachability” (r = 0.409, p = 0.011).
In the C-SSRS scale only the first item was found to be significantly correlated with severe suicide attempt – (1) want/wish to be dead (r = 0.394, p = 0.017).
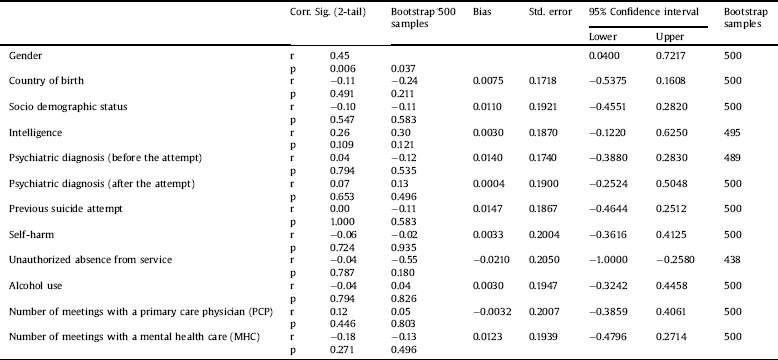
500 Bootstrap sampling was performed when calculating Kendall’s tau-b correlation due to the small sample size and in order to test the stability of dependent variable-“The severity of suicidal experience” (Table 3). Each sample included 7 random cases of the total sample (n = 39), Correlation Coefficients (r) and significance (p) were calculated. Bootstrap test found that in the SSI, 17 out of 19 items of SSI were significant, 7 of 15 items of the SIS were significant and 10 items from C-SSRS were significant.
SSI – 4 additional items were significantly correlated with sever suicide attempts: Item No. 4 – “Desire to make active suicide attempt” (r = 0.26, p = 0.084); Item No. 9 – “Control over suicidal action/acting-out wish” (r = 0.34, p = 0.06); item No. 12 – “Method: Specificity/planning of contemplated attempt” (r = 0.29, p = 0.104); Item No. 14 – “Sense of "capability" to carry out attempt” (r = 0.30, p = 0.095).
SIS – 2 additional items were significantly correlated to severe suicide attempts: Item No. 7 – “Suicide Note” (r = 0.27, p = 0.80); Item No. 9 – “purpose of attempt” (r = 0.30, p = 0.59).
C-SSRS – 2 items were additionally correlated with severe suicide attempts: Item No. 4 – “Active Suicidal Ideation with Some Intent to Act, without Specific Plan” (r = 0.29, p = 0.091); item No. 15 – “Interrupted Attempt” (r = 0.29, p = 0.079).
4. Discussion
Seven Item of the SSI, were found to be associated with severe suicide attempts. Comparable results were found for two items of the SIS and one item of the C-SSRS – (wishing to be dead which reflects passive ideation). Those findings indicate that severity of suicidal ideation is more strongly associated with serious suicide attempt than with suicidal intent. This finding contradicts approaches arguing that suicidal intent carries a critical weight in the assessment of suicidality risk. A possible explanation is that while intent to die may diminish after a serious suicide attempt (may be due to related mechanisms such as repression, denial or dissociation), suicide ideation remains strong [Reference Gothelf, Apter, Brand-Gothelf, Offer, Ofek and Tyano37]. Alternatively, retrospective measurement of intent may have limited validity [Reference Mcauliffe38] and is different after an attempt [Reference Wolfe-Clark and Bryan20, Reference Rudd and Ellis39], while suicidal ideation is potentially more persistent after a suicide attempt [Reference Mcauliffe38]. Yet another explanation may be that the suicide attempt causes a cathartic effect that reduces the involvement with death [Reference Matsuishi, Kitamura, Sato, Nagai, Huh and Ariyoshi40, Reference Sarfati, Bouchaud and Hardy-Bayle41].
This study's findings are in line with other reports of a difference in the reporting of suicide intent and ideation prior to and following a suicide attempt [Reference Oquendo, Halberstam, Mann and First22, Reference Matsuishi, Kitamura, Sato, Nagai, Huh and Ariyoshi40]. Prior to the attempt participants often reported suicidal thoughts as well as intentions to die but after the suicide attempt they reported only suicide ideation while denying any intention to die [Reference Oquendo, Halberstam, Mann and First22]. Therefore, in the severe suicide attempt group, ideation might persist more than reported intent following the attempt.
Mann et al. [Reference Mann, Apter, Bertolote, Beautrais, Currier and Haas18] suggested a model by which suicide ideation turns into a suicidal act with mediating factors such as availability of means for suicide. A recent systematic review reinforced the importance of such availability [Reference Zalsman, Hawton, Wasserman, van Heeringen, Arensman and Sarchiapone42]. Moreover, it was shown that the risk of suicide is two to five times greater in households with firearms [Reference Miller, Azrael and Barber43]. In a military setting, availability of firearms is critical, and constitutes a major risk factor for suicide amongst army soldiers [Reference Anglemyer, Miller, Buttrey and Whitaker44, Reference Reisch, Steffen, Habenstein and Tschacher45]. In the U.S. this is a major risk factor for civilians too [Reference Mann and Michel46]. In the IDF, as in other military settings, guns are prevalent, especially for combat soldiers, and those are mostly males [Reference Lubin, Werbeloff, Halperin, Shmushkevitch, Weiser and Knobler47]. It is also a well-established fact that a third of youngsters with suicide ideation will go on to attempt suicide within 1 year [Reference Nock, Green, Hwang, McLaughlin, Sampson and Zaslavsky48].
Table 2 Scores of suicide ideation and intent in moderate vs severe suicide attempters in a military setting (mean and standard deviations).

SSI = Scale for Suicide Ideation; SIS = Suicide Intent Scale.
a C-SSRS = Columbia Suicide Severity Rating Scale.
* p < 0.05.
Table 3 Coloration bootstrap method to prove stability of the scale of suicide ideation (n = 39 Bootstrap, n = 28).
These findings fit the model described in Mann et al.’s review [Reference Mann, Apter, Bertolote, Beautrais, Currier and Haas18]. Soldiers are often young people who find themselves in highly stressful situations, with high availability of weapons, as military settings tend to be, especially combat situations. Thus suicidal acts are more apt to happen and thresholds for depression and intent are potentially lower. This understanding becomes critical when assessing soldiers' potential die by suicide. Support for our conclusions can be found in a recent study among IDF soldiers which showed that despite all the soldiers in the study performing an act that was lethal enough to result in death it seems that the intent of the subjects without depression was not as high as the intent of those with depression [Reference Shelef, Korem, Yavnai, Yedidya, Ginat and Shahar49]. The group without depression was more impulsive, and scored lower on the SIS questionnaire [Reference Conner50].
4.1 Limitations
The current study has several limitations. The sample size is relatively small however a Bootstrap method was used to test the stability of the Kendall's tau b correlation and lower the statistical error. Additionally, this was an opportunistic study and the group that was discharged immediately from military service after the suicide attempt was not examined. That group may constitute the most serious suicide attempter group but it lacked the measures of ideation, intent and lethality that were used in this study.
4.2 Conclusions
This study's findings have important clinical implications. “Current” or post-attempt suicidal ideation following a suicide attempt may be a more reliable indicator than previous suicide intent when assessing the risk for future suicides. Future studies need to test this finding prospectively to determine its predictive properties.
Funding support
None.
Acknowledgment
The authors thank Mrs. Michaela Gerchak for editing the final version.







Comments
No Comments have been published for this article.