Introduction
The 11th version of the international classification of diseases (ICD-11) [1] introduced complex post-traumatic stress disorder (CPTSD). PTSD and CPTSD represent distinct diagnostic entities [1, Reference Brewin2]. CPTSD commonly arises following exposure to prolonged and repetitive interpersonal traumas, where escape is difficult or impossible [Reference Herman3]. These may include sexual, physical, and emotional abuse in childhood and adolescence, torture, genocide, prolonged domestic violence, and/or institutional abuse [Reference Cloitre, Stolbach, Herman, Kolk, Pynoos and Wang4–Reference Nickerson, Cloitre, Bryant, Schnyder, Morina and Schick6]. Compared to chronic PTSD, a CPTSD diagnosis requires disturbances of self-organization (DSO), namely emotional dysregulation; a negative self-concept; and impaired interpersonal relationships [1, Reference Brewin2] alongside core PTSD symptoms, that is, re-experiencing through flashbacks and intrusive memories, avoidance of trauma-related reminders, and heightened threat sensitivity. Early evidence suggests an impairment in the neural circuitry involved in threat processing [Reference Bryant, Felmingham, Malhi, Andrew and Korgaonkar7] and response inhibition [Reference Bryant, Tran, Williamson and Korgaonkar8] in individuals with CPTSD, reflecting the additional emotion dysregulation, compared to those with PTSD without complex symptoms. Finally, patients with ICD-11 CPTSD show higher levels of suffering, comorbidity, and functional impairment than those with ICD-11 PTSD [Reference Cloitre, Garvert, Brewin, Bryant and Maercker9–Reference Karatzias and Cloitre15] and DSM-5 PTSD [Reference Hyland, Shevlin, Fyvie and Karatzias16, Reference Powers, Fani, Carter, Cross, Cloitre and Bradley17].
International guidelines on CPTSD management [Reference Cloitre, Courtois, Charuvastra, Carapezza, Stolbach and Green18, 19] recommend a phase-based psychotherapeutic approach [Reference Herman20, Reference Cloitre, Courtois and Ford21]. Meta-analyses also support the effectiveness of psychological interventions in patients with symptoms of CPTSD [Reference Karatzias, Murphy, Cloitre, Bisson, Roberts and Shevlin22–Reference Cusack, Jonas, Forneris, Wines, Sonis and Middleton24]. Trauma-focused cognitive behavioral therapy (TF-CBT) and eye movement desensitization and reprocessing (EMDR) have the strongest evidence base for core PTSD symptoms [Reference Karatzias, Murphy, Cloitre, Bisson, Roberts and Shevlin22–Reference Cusack, Jonas, Forneris, Wines, Sonis and Middleton24]. TF-CBT consists of prolonged and/or narrative exposure through imaginal reliving with rescripting and cognitive restructuring [Reference Ehlers, Clark, Hackmann, McManus and Fennell25]. EMDR consists of attending to memories and associations while simultaneously engaging in bilateral physical stimulation, such as eye movements, taps, or tones [Reference Shapiro26]. Research on CPTSD across all its domains in adults is limited due to the novelty of the formal diagnosis, with only two recent studies identifying prolonged exposure [Reference Hoeboer, de Kleine, Oprel, Schoorl, van der Does and van Minnen27, Reference Voorendonk, De Jongh, Rozendaal and Van Minnen28] and EMDR [Reference Voorendonk, De Jongh, Rozendaal and Van Minnen28] as effective for adults with CPTSD. Furthermore, there are a lack of studies from real-world clinical settings.
Aims of study
We sought to evaluate the treatment model of a specialist inner-London CPTSD service and its effectiveness in patients with CPTSD. Our first aim was to identify whether the package of trauma-focused psychotherapy (TF-P) offered (TF-CBT, EMDR, or a TF-CBT plus EMDR) within the phased model approach was effective at reducing PTSD symptom severity in a real-world setting. Our secondary outcomes were the change in depressive symptoms, CPTSD using a proxy measure, and functional impairment. Further exploratory aims of this study were (a) to compare differences between groups receiving TF-CBT, EMDR, and TF-CBT plus EMDR and (b) to identify whether baseline clinical severity of PTSD and depressive symptoms influenced treatment response.
Materials and Methods
Treatment setting and process
The traumatic stress clinic (TSC) is a local outpatient service within the UK National Health Service. The service assesses and treats adult patients with multiple, severe traumas and PTSD, and other comorbid difficulties. The TSC has specialist expertise in working cross-culturally with refugees, asylum-seekers, torture, developmental trauma survivors, victims of trafficking, and complex presentations. Referral criteria include a primary PTSD or CPTSD diagnosis, and readiness to talk about past traumas in treatment without experiencing high levels of emotional dysregulation. The service is unable to accept patients who cannot tolerate TF-P, that is, with significant difficulties with self-harm, drug and alcohol dependence, or other harmful ways of responding to distress.
Patient referrals and treatment
Treatment at the TSC follows a phase-based approach [Reference Cloitre, Courtois, Charuvastra, Carapezza, Stolbach and Green18–Reference Herman20]. In phase 1, up to five sessions of stabilization occur individually or in a group, and include PTSD psychoeducation, grounding techniques for flashbacks and nightmares, and exercises to improve anxiety and sense of safety. Clinicians may signpost clients for practical problems, for example, regarding finances and housing. Subsequently, patients are placed on a waitlist for TF-P.
Phase 2 involves processing traumatic memories to re-appraise associated emotions and meanings and integrate them into adaptive representations of the self, relationships, and world. Three TF-P options are offered: TF-CBT, EMDR, and TF-CBT combined with EMDR. Choice of therapy was influenced by clinician availability, expertise, and patient preference. TF-CBT at the TSC also draws on evidence-based treatments for multiple and complex traumas, such as narrative exposure therapy [Reference Schauer, Schauer, Neuner and Elbert29] and compassion-focused therapy [Reference Lee and James30]. Depending on clinical presentation, some patients are invited to attend a compassion-focused therapy group before, during, or after individual therapy [Reference Lee and James30, Reference Karatzias, Hyland, Bradley, Fyvie, Logan and Easton31]. Unfortunately, we had insufficient information to incorporate this in our analysis. Phase 3, re-integration, builds on the hopes and goals of patients during treatment, encouraging the re-establishment of social and cultural connection. While we did not study this treatment phase, re-integration begins to be considered during phase 2 TF-P.
Participants and procedures
Our sample included all TSC discharges between July 2016 and June 2019, satisfying the “selection” criterion in the assessment of methodological quality of case reports [Reference Murad, Sultan, Haffar and Bazerbachi32]. Eligible patients were all adults, had sustained multiple and prolonged traumata and had completed outcome measures at assessment, start of treatment, and end of treatment. Using a pseudonymized list of yearly discharges, we classified patients as meeting ICD-11 diagnostic criteria for CPTSD retrospectively through standardized psychological measures, file review and consultation with expert treating clinicians, fulfilling criteria for “ascertainment” in the evaluation of the methodological quality of case reports [Reference Murad, Sultan, Haffar and Bazerbachi32]. Patients had to meet CPTSD criteria across all three steps to be included in the study.
First, the presence of symptoms based on items of the Post-traumatic Checklist (PCL)-5 [Reference Weathers, Litz, Keane, Palmieri, Marx and Schnurr33], Patient Health Questionnaire (PHQ)-9 [Reference Kroenke, Spitzer and Williams34], and Work and Social Adjustment Scale (WSAS) [Reference Mundt, Marks, Shear and Greist35] corresponding to the ICD-11 diagnosis of CPTSD (see Table 1) were evaluated.
Table 1. Items used to assess for ICD-11 complex PTSD.

Note. A score of >2 was required for a symptom to be considered endorsed for the PCL-5 and PHQ-9, and a score of >4 for the WSAS.
Abbreviations: CPTSD, complex post-traumatic stress disorder; ICD-11, International Classification of Diseases; PCL, Post-traumatic Checklist; PHQ, Patient Health Questionnaire; WSAS, Work and Social Adjustment Scale.
The second step involved reviewing clinical case notes to confirm that the patient fulfilled all CPTSD domains. Affect dysregulation was endorsed when clinicians described emotional reactivity, dissociation, high levels of anger, aggression, and/or emotional numbing [Reference Maercker, Brewin, Bryant, Cloitre, Reed and Ommeren36]. Negative self-concept was operationally defined as persistent negative beliefs about the self, and feelings of guilt and shame related to the event. Interpersonal disturbances included social isolation, avoidance of family, friends, intimate relationships; estrangement; and difficulty with emotional intimacy [Reference Maercker, Brewin, Bryant, Cloitre, Reed and Ommeren36].
In the third step, we consulted clinicians involved in patients’ care to ascertain whether patients fulfilled the criteria for CPTSD at assessment. Clinicians were blind to the rating derived from clinical notes and questionnaires, and reported whether each ICD-11 CPTSD symptom was present.
Measurements
Sociodemographic characteristics and The Life Events Checklist (LEC) [Reference Weathers, Blake, Schnurr, Kaloupek, Marx and Keane37] were collected at baseline. Outcome measurements were collected at assessment, start of treatment, and end of treatment.
PTSD symptoms
The PCL-5 [Reference Weathers, Litz, Keane, Palmieri, Marx and Schnurr33] is a 20-item self-report measurement of PTSD based on the DSM-5 [38]. Scores range from 0 to 80 and refer to the past month. A 10-point reduction represents clinically significant change, and a cut-off of 33 indicates a PTSD diagnosis [Reference Wortmann, Jordan, Weathers, Resick, Dondanville, Hall-Clark, Foa, Young-McCaughan, Yarvis, Hembree, Mintz, Peterson and Litz39]. It has been reported to have good psychometric properties [Reference Wilkins, Lang and Norman40].
Depressive symptoms and functional impairment
The PHQ-9 [Reference Kroenke, Spitzer and Williams34] is a self-report instrument measuring nine DSM-IV [41] criteria for depression. Scores range from 0 to 27, with higher scores reflecting depression severity. It is well-validated [Reference Kroenke, Spitzer and Williams34] with good sensitivity to change [Reference Löwe, Kroenke, Herzog and Gräfe42]. A five-point reduction on the PHQ-9 [Reference Kroenke and Spitzer43] reflects clinically significant change and a score of less than 5 reflects loss of diagnosis [Reference Kroenke, Spitzer, Williams and Löwe44].
The WSAS is a five-item self-report rating scale, measuring perceived impairment in functioning in the domains of work, home management, social leisure activities, private leisure activities, and relationships with others. A WSAS score above 20 suggests at least moderately severe impairment from psychopathology [Reference Mundt, Marks, Shear and Greist35].
Proxy for the International Trauma Questionnaire (ITQ) to measure CPTSD
We calculated total scores for items used to screen for CPTSD, mapping onto symptom dimensions of CPTSD based on the ICD-11 and the ITQ [Reference Cloitre, Shevlin, Brewin, Bisson, Roberts and Maercker45] (see Table 1). PHQ-9 and WSAS item responses were converted to a five-item scale comparable to the ITQ and PCL-5.
Adverse and no treatment effects
We recorded hospitalizations, suicide attempts, serious self-harm resulting in presentation to hospital, or severe deterioration in functioning and symptomatology due to treatment as documented in clinical notes. Symptom deterioration was measured through reliable change on the PCL-5 and PHQ-9 using the reliable change index (RCI) (see below).
Statistical analysis
Linear multilevel mixed-effects models examined treatment effects on outcomes over time. The random component included a random subject intercept term to account for correlations between repeated measurements [Reference Molenberghs, Verbeke, Verbeke and Molenberghs46]. Fixed effects included: age, sex, the dummy variable of treatment period (assessment, start of treatment, and end of treatment), treatment time, and number of sessions. The fixed effects assessing change in the PTSD scores included baseline depression scores, treatment period, and depression interaction. The exploratory models assessing change in depression scores included baseline PTSD scores and their interaction with treatment period, and the model assessing change in functional impairment included baseline PTSD and depression scores. To explore clinical change in the treatment phases, we compared symptom change during stabilization and waiting versus during individual TF-P (i.e., pre-to-post phase 1 symptom change versus pre-to-post phase 2 symptom change) on primary and secondary outcomes using paired samples t-tests. Rates of reliable change [Reference Jacobson and Truax47] were calculated for all outcomes in both treatment phases. For each outcome, the standard error of measurement (SE meas) was calculated using the scale’s Cronbach’s alpha and the standard deviation of a normative sample. Subsequently, the pre-treatment and post-treatment differences were divided by the standard error of the difference (S diff), with the absolute value reflecting the RCI. A change index score of over 1.96 was considered reliable [Reference Jacobson and Truax47]. Independent samples t-tests were used to assess for differences between treatment groups, for each outcome of interest across timepoints. Analyses were conducted using IBM SPSS Statistics 22 and STATA v16.1 MP 4.
Results
Figure 1 presents the screening of patients and reasons for exclusion, with 59 patients included in the study. Socio-demographic and clinical characteristics are presented in Table 2. Patients were aged between 25 and 63 years old [mean (SD) = 45.66 (9.19)] and 64% (n = 38) of them were female. Most patients reported psychiatric comorbidity (54.24%, n = 32) and received psychotropic medication (69.49%, n = 41). Most patients experienced developmental trauma and multiple traumatic events. Moreover, 84% endorsed directly experiencing at least three traumatic events on the LEC, with a mean of 5.09 (SD = 3.07) events directly experience. The sample was ethnically diverse, and 49.15% (n = 29) were of non-UK origin. whereas 35.60% (n = 21) were refugees or asylum seekers.
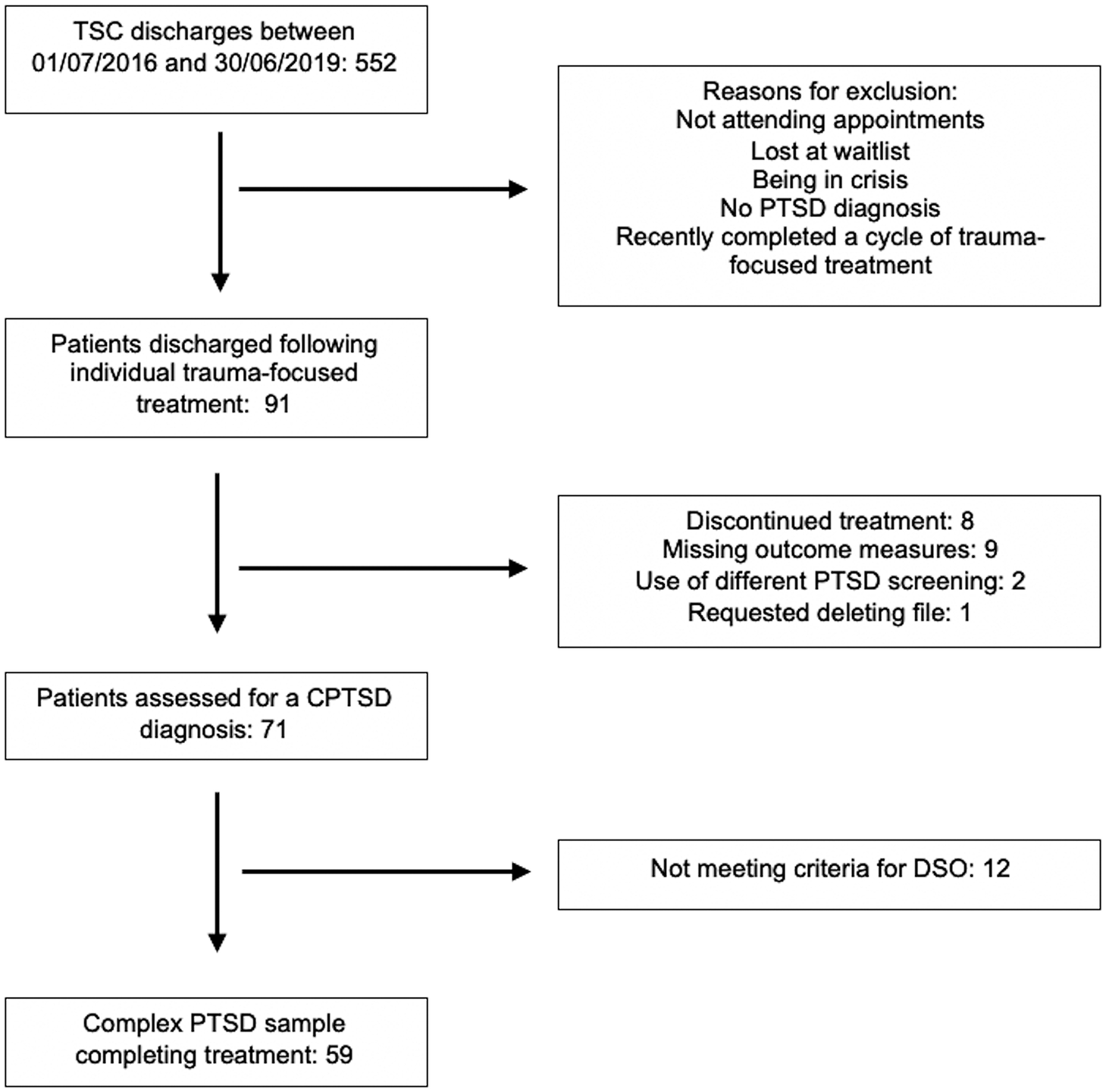
Figure 1. Flow diagram of participant classification with a complex post-traumatic stress disorder (CPTSD) diagnosis (DSO, disturbances of self-organization).
Table 2. Sociodemographic and clinical patient characteristics.

a Sex, geographical region of origin, psychiatric comorbidity, types of trauma, and information on medication were recorded based on each patient’s clinical case notes.
b Ethnicity categories were determined using the ethnic groups recommended for England and Wales, as described by the Office of National Statistics.
Mean phase 1 duration was 13.6 (8.1) months and TF-P duration was 17.60 (12) months. Mean (SD) number of phase 2 treatment sessions was 28 (10) (range: 7–60 sessions). In total, 57.60% (n = 34) received TF-CBT, 13.60% (n = 8) received EMDR, and 28.80% (n = 17) received TF-CBT plus EMDR. Outcome measurements by treatment group are presented in Table 3 and Table 4.
Table 3. Means, standard deviations, median, and maximum scores across TF-CBT, EMDR, and TF-CBT plus EMDR treatment groups.

Abbreviations: EMDR, eye movement desensitization and reprocessing; PCL, Post-traumatic Checklist; TF-CBT, trauma-focused cognitive behavioral therapy; TF-P, trauma-focused psychotherapy.
Table 4. Means and standard deviations across measurement points, and frequencies of clinical status at end of trauma-focused psychotherapy (TF-P).

Abbreviations: PCL, Post-traumatic Checklist; PHQ, Patient Health Questionnaire; WSAS, Work and Social Adjustment Scale.
PTSD symptoms
Patient outcomes across time are presented in Table 4. PCL-5 scores significantly improved following TF-P (coefficient −14.44; 95% CI −25.89 to −10.16) (see Table 2), with a large effect size (Cohen’s d = 0.89). PCL-5 scores did not significantly change during phase 1 (p = 0.162). Change in PCL-5 scores was significantly greater during TF-P [mean (SD) = −14.44 (16.21)] versus during phase 1 [mean (SD) = 3.37 (11.35)], t(58) = −3.99, p < 0.001 (Cohen’s d = 0.52) (see Figure 2). In total, 28.81% (n = 17) demonstrated positive reliable change during phase 1 and 54.24% (n = 32) demonstrated positive reliable change during phase 2. In total, 54.24% (n = 32) showed clinically significant change on the PCL-5 during phase 2 (see Table 2). Visually inspecting changes across domains of the PCL-5 showed a consistent reduction.

Figure 2. Individual post-traumatic stress disorder (PTSD checklist [PCL-5]) and depressive (Patient Health Questionnaire [PHQ-9]) symptom severity and psychosocial functioning (Work and Social Adjustment Scale [WSAS]) scores across measurement points. Error bars indicate standard error of measurement. TF-P, trauma-focused psychotherapy.
Baseline depression significantly and positively affected PCL-5 scores (coefficient 0.97; 95% CI 0.41 to 1.54) at the 5% level. There was no treatment period and baseline depression interaction (p > 0.49). No differences were observed in PCL-5 scores between patients receiving TF-CBT, EMDR, and TF-CBT plus EMDR, at any measurement point (all p > 0.42). There was no association between sex, age, number of sessions, time, and PCL-5 scores (all p > 0.57).
Depressive symptoms, functional impairment, and CPTSD
The PHQ-9 had good internal reliability (a = 0.81). PHQ-9 scores significantly reduced following TF-P (coefficient −5.38; 95% CI −7.50 to −3.25) with a large effect size (Cohen’s d = 0.96). PHQ-9 scores did not significantly change during phase 1 (p = 0.51). Change in PHQ-9 scores during TF-P [mean (SD) = −5.07 (5.47)] was significantly greater than during phase 1 [mean (SD) = 0.56 (5.17)], t(58) = −4.41, p < 0.001 (Cohen’s d = 0.57) (see Figure 2). In total, 18.64% (n = 11) demonstrated positive reliable change during phase 1 and 40.68% (n = 24) demonstrated positive reliable change during phase 2. In total, 49.15% (n = 29) of patients showed clinically significant change on the PHQ-9 during phase 2.
Baseline PCL-5 score had a significantly positive effect at the 5% level on PHQ-9 scores (coefficient 0.14; 95% CI 0.02 to 0.25). The effect of baseline PTSD scores was consistent across measurement points, presenting no interaction with treatment period (all p > 0.337). Sex, age, number of sessions, or time was not associated with PHQ-9 scores (all p > 0.433). PHQ-9 scores did not differ between patients receiving TF-CBT, EMDR, or TF-CBT plus EMDR, at any measurement point (all p > 0.105).
The WSAS showed good internal reliability (a = 0.80). WSAS scores significantly decreased following TF-P (coefficient −5.11; 95% CI −8.52 to −1.71) with a moderate effect size (Cohen’s d = 0.54). WSAS scores did not significantly change during phase 1 (p = 0.580). Change in WSAS scores was significantly greater following treatment [mean (SD) = −5.21 (9.49)] than following phase 1 [mean (SD) = 0.33 (5.63)], t(58) = −2.26, p = 0.028 (Cohen’s d = 0.424) (see Figure 2). In total, 7.01% (n = 4) demonstrated positive reliable change during phase 1 and 34.48% (n = 20) demonstrated positive reliable change during phase 2. PHQ-9 (coefficient 0.51; 95% CI 0.06 to 0.97), but not PTSD (p = 0.195), scores had a significant effect on WSAS scores.
Sex, age, number of sessions, or time were not associated with WSAS scores (all p > 0.170). WSAS scores did not differ between patients receiving TF-CBT, EMDR, and TF-CBT plus EMDR, at any timepoint (all p > 0.185). In total, 59.3% (n = 35) continued to experience at least moderately severe impairment from psychopathology at the end of treatment.
There was no significant reduction in CPTSD severity during phase 1, p = 0.168. There was a significant reduction in CPTSD symptom severity from the start of treatment [mean (SD) = 34.49 (7.26)] to the end of treatment [mean (SD) = 25.47 (10.98)], t(58) = 7.18, p < 0.001 (Cohen’s d = 1.04). Change in CPTSD severity was significantly greater following treatment [mean (SD) = −9.05 (9.60)] than during phase 1 [mean (SD) = 1.36 (7.46)], t(58) = 4.69, p < 0.001.
Adverse treatment effects
Regarding adverse effects, no hospitalizations, increased suicidality, or self-harm were reported to have occurred during treatment. Reliable worsening on the PCL-5 was observed in 11.86% (n = 7) of patients during phase 1 and 3.39% (n = 2) during phase 2. Reliable worsening on the PHQ-9 was observed in 8.48% (n = 5) of patients during phase 1 and 1.70% (n = 1) during phase 2. Reliable worsening on the WSAS was observed in 6.78% (n = 4) of patients during phase 1 and 3.39% (n = 2) during phase 2.
Discussion
This is one of the first studies on the effectiveness of TF-P in improving PTSD symptoms in patients with CPTSD based on the ICD-11 criteria in a real-world setting. Depression, functional impairment, and CPTSD also improved significantly after treatment. Interestingly, higher depression scores were predictive of higher PTSD and impaired functioning across timepoints, and a smaller association was established with baseline PTSD and depression scores across timepoints.
PTSD, depressive, and CPTSD symptoms
Positive reliable and clinically significant changes during TF-P were observed in more than half the sample. Comparing this to phase 1, where a third of patients reliably improved on PTSD symptoms, we see that in most patients PTSD symptoms do not tend to spontaneously improve over time in the absence of active TF-P. As we compared treatment with stabilization plus waiting, we cannot infer whether stabilization alone is effective. In two recent studies [Reference Hoeboer, de Kleine, Oprel, Schoorl, van der Does and van Minnen27, Reference Van Vliet, Huntjens, Van Dijk, Bachrach, Meewisse and De Jongh48], patients with CPTSD did not benefit more from the addition of affective and interpersonal skills training to prolonged exposure [Reference Hoeboer, de Kleine, Oprel, Schoorl, van der Does and van Minnen27] and EMDR [Reference Van Vliet, Huntjens, Van Dijk, Bachrach, Meewisse and De Jongh48]. However, earlier research [Reference Cloitre, Petkova, Su and Weiss49] had found additional skills training to improve outcomes for women with more severe difficulties in emotion regulation. It is therefore necessary for future research to elucidate the relative benefit of using a phase-based approach [Reference Karatzias, Murphy, Cloitre, Bisson, Roberts and Shevlin22]. Additionally, as the PCL-5 is based on the DSM-5 diagnosis of PTSD [Reference Weathers, Litz, Keane, Palmieri, Marx and Schnurr33], improvements in the DSM-5 domain “Negative alterations in cognition and mood” [38] may reflect changes in DSO.
Depression scores decreased significantly more during TF-P than during phase 1, in line with previous meta-analyses [Reference Bisson, Roberts, Andrew, Cooper and Lewis23]. Approximately, half of the patients exhibited clinically significant change and 40.68% exhibited reliable improvement following TF-P. TF-CBT uses cognitive restructuring to change negative thinking patterns about the self and the world, such as negative thinking biases and dysfunctional core beliefs [Reference Ehlers, Clark, Hackmann, McManus and Fennell25] also relevant in depressive symptoms, which have developed because of severe, repeated, and often chronic traumatic experiences.
The role of baseline depression on the trajectory of PTSD and functioning scores is noteworthy, as patients with CPTSD are known to experience worse levels of depression [Reference Hyland, Shevlin, Fyvie and Karatzias16] and comorbid depression can negatively affect CPTSD treatment outcome [Reference Cloitre, Garvert and Weiss50, Reference Ehlers, Grey, Wild, Stott, Liness and Deale51]. Putative explanations involve the way negative schemata and shame can interfere with the re-processing of trauma memories [Reference Karatzias, Shevlin, Hyland, Brewin, Cloitre and Bradley52], but also how reduced motivation and hopelessness could make elements of treatment difficult to engage with. Depressive symptoms can be targeted through a multimodal approach [Reference Karatzias and Cloitre15], and in stabilization, especially if they significantly increase the risk of harm to self [19].
The statistically significant improvement in our proxy CPTSD score during TF-P needs to be interpreted with caution, given the retrospective and non-validated measurement. Treatment groups did not differ on symptoms across timepoints, consistent with meta-analyses comparing the effectiveness of TF-CBT to EMDR on both PTSD and depression scores [Reference Karatzias, Murphy, Cloitre, Bisson, Roberts and Shevlin22, Reference Bisson, Roberts, Andrew, Cooper and Lewis23]. No sociodemographic characteristics were associated with clinical outcomes across timepoints. Although females have higher risk of CPTSD in population studies [Reference Karatzias, Cloitre, Maercker, Kazlauskas, Shevlin and Hyland53], the multiple and diverse range of traumas, and comorbidities observed in our sample may explain the consistent symptom severity.
Adverse effects
Most past studies fail to describe adverse effects [Reference Cusack, Jonas, Forneris, Wines, Sonis and Middleton24], despite the risk of increased PTSD symptoms, particularly re-experiencing, following TF-P [Reference Foa, Zoellner, Feeny, Hembree and Alvarez-Conrad54, Reference Pitman, Altman, Greenwald, Longpre, Macklin and Poiré55]. No adverse effects were reported by clinicians, but a small number of patients experienced reliable worsening on PTSD, depression, or functional impairment during treatment. The exclusion of patients dropping out of treatment could introduce selection bias to this finding.
Strengths and limitations
Our study is novel in evaluating treatment in a sample meeting ICD-11 CPTSD diagnostic criteria in a real-world clinical setting with an ethnically and culturally diverse civilian sample. Our research on treatment following multiple traumas highlights the greater level of need compared to studies on single event traumas, providing a valuable addition to the current trauma literature. Finally, in contrast to previous research [Reference Bisson, Roberts, Andrew, Cooper and Lewis23, Reference Cusack, Jonas, Forneris, Wines, Sonis and Middleton24], we considered adverse effects.
Limitations include a retrospective design and the absence of a separate control group. Adding to this the length of waiting time and treatment we need to consider the possibility of spontaneous remission. Varying levels of detail in clinical notes may have limited the retrospective ability to capture the clinical nature of a symptom, for example, depressive symptoms versus the negative self-concept and world view as part of DSO. However, our stringent process of participant selection by triangulating evidence from different sources would have provided some protection against this, increasing the internal validity of our measurement. Treatment comparison results could be explained by unadjusted confounding variables, as there was no randomization, and the sample size was small. The non-random provision of treatment modality may have been influenced by clinician availability, expertise, and preference. Another limitation is that we only included treatment completers with all outcome measures and without follow-up.
Clinical implications
A clear clinical implication from our study concerns treatment length. More than half of the patients still met clinical diagnosis criteria after an average of 28 sessions, which is almost three times the number suggested by NICE clinical guidelines for PTSD [19]. This finding demonstrates that it is critical for specific CPTSD guidelines to be developed. Clinically, this population may present with shame and lack of trust arising from interpersonal traumas and require longer periods of time for engagement and the formation of a good enough therapeutic relationship [19]. A recent study [Reference Hoeboer, de Kleine, Oprel, Schoorl, van der Does and van Minnen27] supported the view that longer treatment is needed, as some patients with CPTSD continue to present with elevated symptoms after therapy. We need to adapt treatments and available resources to fit these higher levels of complexity and severity [Reference Lehrner and Yehuda56].
Finally, although we did not record current life events that could interfere with treatment, more functional impairment is observed in CPTSD than in PTSD [Reference Herman3, Reference Cloitre, Hyland, Bisson, Brewin, Roberts, Karatzias and Shevlin11, Reference Bondjers, Hyland, Roberts, Bisson, Willebrand and Arnberg13, Reference Karatzias and Cloitre15, Reference Hoeboer, de Kleine, Oprel, Schoorl, van der Does and van Minnen27, Reference Coventry, Meader, Melton, Temple, Dale and Wright57]. This includes socioeconomic, relational, and housing difficulties. Consistent with meta-analyses [Reference Coventry, Meader, Melton, Temple, Dale and Wright57], our sample maintained high levels of functional impairment following treatment. It is therefore essential to move beyond the narrow measurement of symptomatic change, to promoting wellbeing in all life domains affected by the debilitating experience of CPTSD.
Suggestions for future research
Further research should determine the comparative efficacy and optimal sequence of different treatments with randomized controlled trials, and designs to identify personal markers of treatment effectiveness for CPTSD. Psychotherapeutic approaches that can improve one’s attachment organization and adaptive self and interpersonal schemata should be explored [Reference Karatzias, Shevlin, Hyland, Brewin, Cloitre and Bradley52], and for whom which TF-P is most appropriate and safe.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author M.B. upon reasonable request.
Acknowledgments
We are grateful to all the patients and our colleagues at the Traumatic Stress Clinic.
Author Contributions
E.M., M.B., M.R. and J. Blumberg participated in formulating research questions, designing the research, carrying it out, and writing the article. EM and RG participated in analyzing the research. J. Blumberg, E.D., K.E., J.G., H.K., T.K., L.O., E.W., R.G., C.B., J. Billings, and M.B. participated in carrying out the research and writing the article.
Funding Statement
M.B. was funded by a UKRI Future Leaders Fellowship (MR/V025945/1), a UCL Excellence Fellowship and the NIHR University College London Hospitals Biomedical Research Centre.
Conflicts of Interest
The authors declare none.
Ethical Standards
This retrospective study, which was part of a service evaluation using archival data, was registered with the Camden and Islington NHS Foundation Trust audit committee.









Comments
No Comments have been published for this article.