Functional impairment in patients with bipolar disorder is common even during periods of euthymia. Reference Rosa, Reinares, Michalak, Bonnin, Sole and Franco1 Longitudinal and cross-sectional reports in patients with bipolar disorder confirm that neurocognitive and psychosocial functioning are related to each other Reference Martino, Marengo, Igoa, Scápola, Ais and Perinot2–Reference Martinez-Aran, Vieta, Torrent, Sanchez-Moreno, Goikolea and Salamero4 and that neurocognitive performance can predict functional outcome. Reference Bonnin, Martinez-Aran, Torrent, Pacchiarotti, Rosa and France3,Reference Tabares-Seisdedos, Balanza-Martinez, Sanchez-Moreno, Martinez-Aran, Salazar-Fraile and Selva-Vera5,Reference Lewandowski, Cohen, Keshavan, Sperry and Ongür6 Given the link between neurocognition and functional outcome Reference Bonnin, Martinez-Aran, Torrent, Pacchiarotti, Rosa and France3–Reference Lewandowski, Cohen, Keshavan, Sperry and Ongür6 the functional remediation programme was created with the objective of enhancing functioning in patients who are bipolar impaired. During the sessions, patients are trained in the use of neurocognitive skills (attention, memory and executive functions) to be applied during their daily routines to improve functional outcome. Reference Martinez-Aran, Torrent, Sole, Bonnin, Rosa and Sanchez-Moreno7,Reference Bonnin, Torrent, Vieta and Martínez-Arán8 A recent multicentre, randomised controlled trial (RCT) confirmed the short-term efficacy of functional remediation. Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9 Specifically, it was found that just after finishing the intervention, that is at 6-month follow-up after baseline, the functional remediation group had am improved functional outcome when compared with a treatment-as-usual (TAU) group, especially noted in occupational and interpersonal functioning. Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9 The present study is a continuation of the above-mentioned trial. Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9 In this regard, we analysed the functional outcome of the participants 6 months after finishing the therapy, that is 1 year after baseline, in order to study whether functional improvement is maintained over time. As a secondary objective, we aimed to analyse changes in neuropsychological performance.
Method
This is the 1-year follow-up study of a published RCT that analysed the efficacy of functional remediation at 6-month follow-up. Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9 The project is a multicentre, randomised, rater-masked out-patient trial conducted between 2009 and 2011. It included three parallel arms (1:1:1) to evaluate the efficacy of functional remediation as an add-on therapy compared with psychoeducation and TAU in bipolar disorder. Randomisation was accomplished with the use of a computer-generated sequence. The trial was registered with Clinicaltrials.gov: NCT01370668 and the current analyses were pre-planned in the original protocol.
Participants
As previously described in Torrent and colleagues, Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9 239 participants with euthymic bipolar I and II disorder were recruited in different centres across Spain. Participants were between 18 and 55 years old and presented a moderate to severe degree of functional impairment (Functioning Assessment Short Test (FAST) Reference Rosa, Sanchez-Moreno, Martinez-Aran, Salamero, Torrent and Reinares10 total score ≥18). All participants were euthymic for at least 3 months before study enrolment, assessed using the Hamilton Rating Scale for Depression (HRSD ≤8), Reference Hamilton11,Reference Ramos-Brieva and Cordero-Villafáfila12 and Young Mania Rating Scale (YMRS ≤6). Reference Young, Biggs, Ziegler and Meyer13,Reference Colom, Vieta, Martinez-Aran, Garcia-Garcia, Reinares and Torrent14 Participants were excluded if they presented any of the following conditions: (a) IQ <85; (b) any neurological or comorbid psychiatric condition affecting neuropsychological performance (patients with neurological diseases, such as epilepsy, or any Axis I comorbidity); (c) electroconvulsive therapy within the past year. All patients provided written informed consent. Ethical approval for the study was granted by the ethics committee at every hospital involved in the study.
Clinical and psychosocial assessments
At baseline and at 1-year follow-up all participants were evaluated with the following rating scales: YMRS to assess manic symptoms; Reference Young, Biggs, Ziegler and Meyer13,Reference Colom, Vieta, Martinez-Aran, Garcia-Garcia, Reinares and Torrent14 HRSD to assess depressive symptoms; Reference Hamilton11,Reference Ramos-Brieva and Cordero-Villafáfila12 and the FAST scale Reference Rosa, Sanchez-Moreno, Martinez-Aran, Salamero, Torrent and Reinares10 to assess psychosocial functioning (a 24-item scale assessing disability in patients with bipolar disorder). FAST assesses six functional domains: autonomy (the capacity to make decisions and do things by oneself), occupational functioning (the capacity to maintain a paid job, efficiency of performing tasks at work, working in the field in which the patient was educated and earning according to the level of the employment position), cognitive functioning (the ability to concentrate, perform simple mental calculations, solve problems, and learn and recall new information), financial issues (the capacity to manage one's finances), interpersonal relationships (relations with friends and family, involvement in social activities, sexual relationships and the ability to defend one's own interests) and leisure time (the capacity to engage in sports or physical activities and to enjoy hobbies). Higher scores indicate a higher degree of functional impairment. The FAST total score was the primary outcome measure defined as the mean change on the total score from baseline to end-point (week 52).
Finally, clinical and demographic variables were collected at baseline and at the end-point through clinical interview and revision of clinical records. They included age, gender, education level, occupational status, body mass index, diagnosis, number and type of episodes, illness duration, age at first hospital admission, age at illness onset, number of admissions to hospital, number of suicide attempts, history of psychosis, pharmacological treatment and adherence, family psychiatric history, comorbidities and several course specifiers, such as rapid cycling, atypical symptoms, melancholia and psychotic depression.
Neuropsychological assessment
All individuals completed at baseline (week 0) and at follow-up (week 52) a comprehensive neuropsychological battery grouped into six cognitive domains: processing speed, working memory, executive functions, verbal learning/memory, visual memory and attention. For a more detailed description of the neuropsychological battery see Torrent et al. Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9
Interventions
Functional remediation
The functional remediation programme consisted of 21 weekly sessions, each lasting 90 min. This intervention addresses neurocognitive issues such as attention, memory and executive functions, but it focuses even more on enhancing functioning in daily routine. The content of the intervention is based on ecological tasks to be performed in two settings, in the clinic as well as at home. Participants receive training with exercises for memory, attention, problem-solving and reasoning, multitasking and organisation to improve their functional outcome. Most of the techniques were based on paper-and-pencil tasks and group activities. (For detailed information on the rationale of this intervention see Martinez-Aran et al Reference Martinez-Aran, Torrent, Sole, Bonnin, Rosa and Sanchez-Moreno7 and Bonnin et al. Reference Bonnin, Torrent, Vieta and Martínez-Arán8 ) A manual of the intervention has been published. Reference Vieta, Torrent and Martinez-Aran15
Psychoeducation
The psychoeducation also consisted of 21 weekly sessions of 90 min each, aimed at preventing recurrences of bipolar illness by improving four main issues: illness awareness, treatment adherence, early detection of prodromal symptoms of relapse and lifestyle regularity. Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea and Benabarre16
Treatment as usual
In the TAU group, participants received prescribed pharmacological treatment without any adjunctive psychosocial therapy.
Statistical analyses
Sociodemographic and clinical features, at baseline and at follow-up, were analysed using ANOVA for continuous variables and chi-square for categorical variables. Group×time effects for overall psychosocial functioning (FAST total score), which was the primary outcome of the study, was analysed using repeated-measures ANOVA. This analysis only takes into account complete cases; hence missing values because of loss to follow-up were not analysed.
Secondary outcomes, such as neuropsychological changes were also analysed: verbal learning/memory, executive functions, processing speed, working memory, attention and visual memory. Working memory and processing speed changes were studied using the IQ index provided in the manual by Wechsler (Wechsler Adult Intelligence Scale-III). Reference Wechsler17 To study verbal memory, executive functions and attention, three composite scores were created. These variables were calculated by converting the participants' raw scores to standardised z-scores. In turn, these z-scores were summed and then averaged in each domain to provide a single score. The verbal memory composite score was composed of the variables of two tests: the California Verbal Learning Test Reference Delis, Kramer, Kaplan and Ober18 and the Logical Memory Scale (WMS-III) for learning/memory. Reference Wechsler19 The executive composite score was calculated based on four representative subtests measuring executive function: Stroop Interference, Wisconsin Card Sorting Test (WCST) Reference Heaton20 perseverative errors, WCST categories and Trail Making Test-part B. Reference Reitan21 Attention composite score was calculated based on several measures of the Continuous Performance Test (CPT-II) Reference Conners22 such as: omission and commission errors, d' attentiveness, beta and reaction time. Finally, exploratory Pearson correlations in each group were conducted to identify clinical and neuropsychological variables associated with functional change during 1-year follow-up. All analyses were two-tailed with alpha set at P<0.05 and were performed with the Statistical Package for Social Sciences version 18.
Results
Patient flow
Figure 1 represents a chart of the patient flow through the study, from the screening phase to the 12-month follow-up. Of 239 participants at baseline, 172 completed the follow-up phase (72%); hence, during the intervention (from week 0 to 21) 54 people discontinued treatment and at the end-point (at week 52) 13 further people withdrew from the study. Reasons were, particularly, lost to follow-up or refusing re-evaluation; however, analysis revealed that completers at the end of follow-up did not differ between groups (χ2 = 0.199, P = 0.9): functional remediation (n = 54), psychoeducation (n = 60) and TAU (n = 58). No significant differences between the three arms (functional remediation, psychoeducation and TAU) with regard to number of relapses were found at follow-up (F = 1.05, P = 0.349): for the functional remediation (mean 0.67, s.d. = 2.25), psychoeducation (mean 0.92, s.d. = 2.58) and TAU groups (mean 0.40, s.d. = 0.98). Finally, an additional analysis comparing missing cases with complete cases revealed that both groups did not differ in baseline characteristics; hence missing cases were considered ‘missing at random’.

Fig. 1 Flow chart of patients during the study.
TAU, treatment as usual.
Demographic and clinical features
As shown in Table 1, the three patient groups did not differ on demographic or clinical data at baseline, except for chronicity (illness duration) (F (2,230) = 3.2, P = 0.04). Tukey post hoc analyses revealed a significant difference when psychoeducation and TAU were compared (P = 0.02). In this regard, the TAU group presented with longer duration of illness when compared with the psychoeducation group. On average, at baseline, participants in the three groups were 40 years old (F (2,233) = 0.8, P = 0.4). They were equivalent in terms of educational level (F (2,231) = 0.2, P = 0.5) but estimated premorbid IQ showed a trend to be different in the three groups (F (2,231) = 2.4, P= 0.08). However, Tukey post hoc analyses revealed that there were no differences between the three groups, only a trend was detected when TAU and psychoeducation were compared (P = 0.07) with higher IQ in the TAU group.
Table 1 Demographic and clinical variables at baseline compared between groups

| Demographic and clinical variables | Functional
remediation group(n = 77) |
Psychoeducation group(n = 82) |
TAU
group (n = 80) |
F | χ2 | P |
|---|---|---|---|---|---|---|
| Age, years: mean (s.d.) | 40.59 (9.10) | 39.25 (8.85) | 40.47 (8.69) | 0.8 | 0.4 | |
| Educational level, years: mean (s.d.) | 12.64 (4.06) | 13.27 (3.66) | 13.22 (3.54) | 0.2 | 0.5 | |
| Estimated premorbid IQ, mean (s.d.) | 105.92 (12.51) | 103.20 (11.63) | 107.66 (14.31) | 2.4 | 0.08 | |
| Age at onset, years: mean (s.d.) | 25.76 (8.46) | 26.83 (8.61) | 24.29 (7.69) | 1.7 | 0.1 | |
| Chronicity, illness duration: mean (s.d.) | 14.83 (9.69) | 12.69 (8.63) | 16.38 (8.79) | 3.2 | 0.04 | |
| Total episodes, mean (s.d.) | 11.86 (12.54) | 9.93 (12.13) | 13.03 (12.27) | 1.3 | 0.2 | |
| Hospital admissions, mean (s.d.) | 2.79 (3.64) | 2.56 (2.51) | 2.51 (2.26) | 0.1 | 0.8 | |
| Hamilton Rating Scale for Depression score, mean (s.d.) | 4.09 (2.51) | 4.14 (2.68) | 4.32 (2.59) | 0.1 | 0.8 | |
| Young Mania Rating Scale score, mean (s.d.) | 1.43 (1.83) | 1.68 (2.12) | 1.32 (1.77) | 0.9 | 0.4 | |
| Women, n (%) | 44 (57.1) | 48 (58.5) | 46 (57.5) | 0.03 | 0.9 | |
| Lifetime psychotic symptoms, yes: n (%) | 47 (61) | 51 (62.2) | 55 (68.8) | 1.2 | 0.5 | |
| Lifetime rapid cycling, yes: n (%) | 12 (15.6) | 10 (12.2) | 15 (18.8) | 1.6 | 0.4 | |
| Family history of affective disorders, n (%) | 45 (58.4) | 50 (61) | 48 (60) | 0.01 | 0.9 | |
TAU, treatment as usual.
Group differences in longitudinal change
Primary outcome: change in psychosocial functioning
Longitudinal repeated-measures analyses addressing the treatment effect on the primary outcome measure showed significant differences between the three groups (Pillai's trace 0.032, F = 3.071, d.f. = 2, P = 0.049), suggesting an interaction between treatment allocation and time (from baseline to follow-up) and a positive effect of functional remediation over time if compared with psychoeducation and TAU. In Fig. 2, the FAST total score in the functional remediation group was significantly reduced from 30.94 (s.d. = 10.24) at baseline to 24.71 (s.d. = 13.60) (t = 4.26, P<0.01) at 12-month follow-up indicating a significant improvement in global functioning. Between-group effect sizes were small when functional remediation was compared with TAU (Cohen's d = 0.18). The within-group effect size in the functional remediation group was moderate (Cohen's d = 0.49).

Fig. 2 Functional improvement at 12-month follow-up: Functioning Assessment Short Test (FAST) total score.
Since baseline differences were detected in illness duration (chronicity) and a trend was detected in premorbid IQ, we decided to control for these two potential confounding variables. Repeated-measures ANCOVA comparing the three groups revealed that the model was still significant, showing that patients in the functional remediation group had a better outcome than patients in the psychoeducation or TAU group (Pillai's trace 0.036, F = 3.38, d.f. = 2, P = 0.036).
When analysing each of the FAST domains in detail, only one of them, autonomy, was found to be significantly different between groups in favour of the functional remediation group (F = 5.54, d.f. = 2, P = 0.005, Fig. 3).
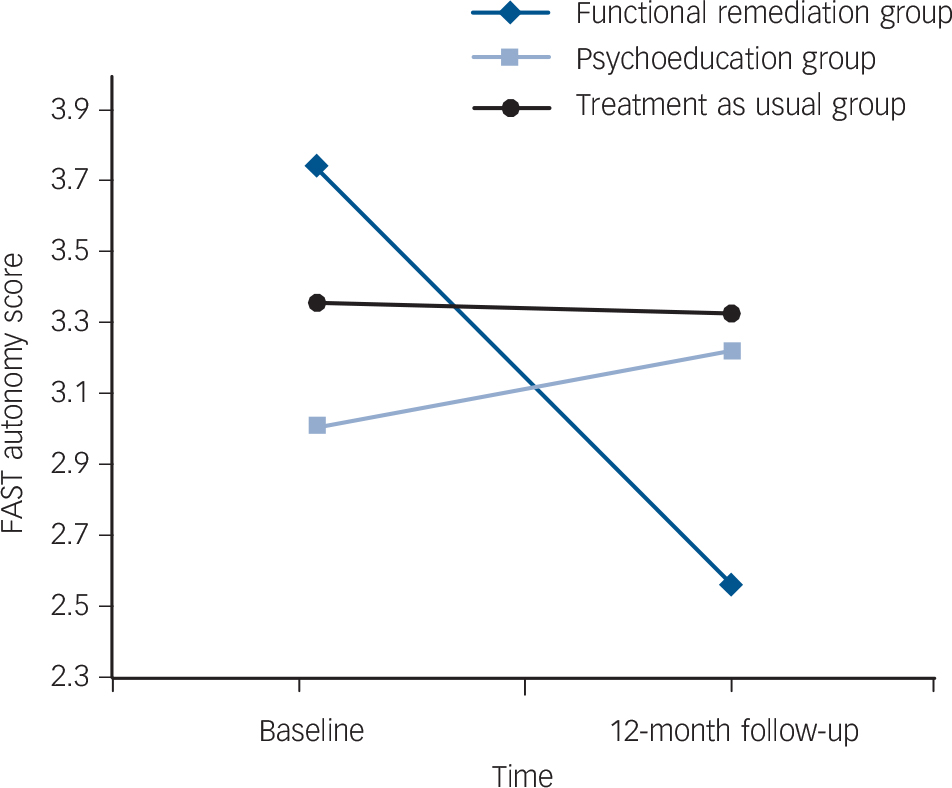
Fig. 3 Improvement of the score in the Functioning Assessment Short Test (FAST) autonomy domain at 12-month follow-up.
Even though subsyndromal depressive symptoms did not differ significantly between the three groups at follow-up, it was found that at the end of follow-up, 35 people had subsyndromal symptoms at the time of the assessment presenting scores of between 9 and 16 on the HRSD and between 7 and 11 on the YMRS. Moreover, seven people at the end of follow-up fulfilled criteria for an acute episode, and one of these refused to continue the study. As a consequence of this, we decided to apply repeated-measures ANCOVA controlling for the potential confounding effect of subsyndromal symptomatology on functioning. It was found that the improvement in autonomy was still significant; however, changes in the FAST total score were no longer significant after controlling for subthreshold depressive symptoms.
Secondary outcome: neuropsychological changes
Concerning neuropsychological performance, repeated-measures analyses showed an improvement in verbal memory (verbal memory composite score) in participants who were enrolled in the functional remediation group compared with the other two treatment groups (F = 5.31, d.f. = 2, P = 0.006). Once again, we repeated the same analyses controlling for those potential confounding variables identified at baseline (chronicity and premorbid IQ), and we found that the difference in the verbal memory composite score was still significant, favouring the functional remediation group when compared with psychoeducation and TAU (Pillai's trace 0.087, F = 7.64, d.f. = 2, P = 0.001).
Finally, no differences were found in the remaining neuropsychological variables such as composite executive score (F = 0.03, d.f. = 2, P = 0.96); processing speed (F = 0.4, d.f. = 2, P = 0.66); working memory (F = 1.18, d.f.= 2, P= 0.30) or attention composite score (F = 0.6, d.f. = 2, P = 0.52).
Relationship between clinical variables and outcome variables
To investigate the candidate variables associated with functional changes across time, exploratory correlations were run in each of the patient groups. Specifically, correlations were conducted between changes in the FAST total score, changes in neurocognitive domains (verbal memory composite score, executive composite score, working memory index, and processing speed index and attention) and clinical changes (current symptomatology, number of relapses) during 1-year follow-up. Since not all participants were euthymic at the end of the study and in order to avoid confounding effects of symptomatology, the correlations were run only with asymptomatic patients at the end of the study. Hence, the distribution of euthymic participants, defined as HRSD ≤8 and YMRS ≤6, in each group was as follows:
Table 2 Outcome variables measured at baseline and at 12-month follow-up

| Mean (s.d.) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Functional remediation group | Psychoeducation group | Treatment as usual group | Repeated measures ANOVA | |||||
| Outcome variables | Baseline (n = 77) | 1 year (n = 54) | Baseline (n = 82) | 1 year (n = 60) | Baseline (n = 80) | 1 year (n = 58) | F | P |
| FAST total score | 30.62 (9.87) | 24.71 (13.60) | 29.63 (10.64) | 26.87 (13.46) | 29.63 (9.38) | 27.28 (13.77) | 3.07 | 0.049 |
| FAST autonomy | 3.74 (5.59) | 2.56 (3.07) | 3.01 (2.61) | 3.22 (3.03) | 3.36 (2.65) | 3.33 (2.83) | 5.54 | 0.005 |
| FAST occupational | 10.15 (5.18) | 8.77 (6.61) | 9.88 (5.54) | 9.38 (6.21) | 9.69 (5.38) | 9.45 (5.94) | 0.01 | 0.38 |
| FAST cognitive functioning | 7.44 (2.80) | 5.97 (3.78) | 7.56 (2.76) | 6.40 (3.46) | 7.55 (2.53) | 6.55 (3.59) | 0.003 | 0.76 |
| FAST interpersonal relationships | 6.05 (3.13) | 4.55 (3.03) | 5.40 (3.21) | 4.46 (3.39) | 4.90 (3.13) | 4.57 (3.47) | 0.014 | 0.26 |
| Verbal memory composite score | −0.04 (5.89) | 1.41 (5.66) | −0.80 (5.50) | −1.9 (6.33) | 0.17 (6.21) | 0.46 (5.56) | 5.31 | 0.006 |
| Executive composite score | 0.16 (2.02) | 0.29 (1.93) | −0.14 (2.02) | −0.08 (2.06) | −0.17 (2.04) | −0.14 (2.01) | 0.03 | 0.96 |
| IQ processing speed | 95.54 (12.62) | 101.58 (14.06) | 92.65 (14.15) | 96.97 (14.81) | 96.37 (21.75) | 100.39 (15.01) | 0.4 | 0.66 |
| IQ working memory | 95.42 (18.15) | 98.23 (14.49) | 91.75 (12.45) | 91.43 (12.90) | 93.37 (14.46) | 93.88 (15.47) | 1.18 | 0.30 |
| Attention composite score | −0.07 (0.49) | −0.10 (0.50) | 0.02 (0.67) | 0.08 (0.59) | 0.07 (0.68) | 0.03 (0.59) | 0.6 | 0.48 |
FAST, Functioning Assessment Short Test.
functional remediation n = 49, psychoeducation n = 48 and TAU n = 52.
A significant correlation was found between change in the FAST total score (FAST baseline – FAST end-point) and change in verbal memory composite score (verbal composite baseline – verbal composite end-point) in the functional remediation group (r = −0.32, P= 0.039). With regard to the psychoeducation group, a positive correlation (r = 0.47, P = 0.001) was found between changes in the FAST total score and changes in HRSD scores (from 0 to 8). Finally, in the TAU group no significant correlations were found between changes in psychosocial functioning and the above-mentioned variables.
Discussion
Main findings
The main finding of this study is the confirmation that functional remediation remains effective over time, particularly after 6 months of no further therapy. The participants enrolled in the functional remediation group showed better psychosocial performance than participants in the psychoeducation and TAU groups after 1-year follow-up from baseline. The FAST total score was reduced at the end-point (52 weeks) from baseline indicating a clinically and statistically significant improvement in general functioning in the functional remediation group.
As a second finding, a significant enhancement in autonomy was observed at 1-year follow-up, but only in those receiving functional remediation. Autonomy refers to the capacity of patients to do things alone and making their own decisions with more self-responsibility. This includes a basic management of the household, the ability to live alone, to do the shopping and to organise a list of products without requiring additional help. Of note, the psychoeducation group did not improve on functional outcomes significantly, but the main aim of psychoeducation is to prevent relapses, not to improve functioning. The psychoeducation group was used as an intensity-matched comparator to the functional remediation. Although psychoeducation may improve functioning over the long term, because it is effective in preventing recurrences according to Colom and colleagues, Reference Colom, Vieta, Martinez-Aran, Reinares, Goikolea and Benabarre16 a 1-year follow-up may be too short a time to detect improvement in functional outcome in those who received psychoeducation. Moreover, the present study selected patients who were highly impaired at baseline with a FAST total score ≥18, and psychoeducation may be much more effective in patients who are not functionally impaired.
Improvements in autonomy
With the functional remediation intervention we aimed to reduce the difficulties that people with bipolar disorder present in their daily life because of their illness, providing them with some tools to improve their ability to solve daily problems. In the primary 6-month end-point analysis patients improved in their adaptation and occupational performance as well as in their interpersonal relationships. Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9 Six months after finishing the intervention, the improvement in these two areas (occupational and interpersonal relationships) disappeared and only autonomy was found to be significant at 12-month follow-up. There are a number of reasons this may be the case: the most likely one is that because of loss to follow-up the study is statistically underpowered, at least, to detect differences when analysing the different FAST domains. Another possible reason is that functional remediation needs booster sessions to maintain the effects of the intervention in the long term, since it seems that results were stronger at 6-month follow-up than at 12-month follow-up.
Improvements in verbal memory
Regarding neurocognitive performance after 1 year, significant improvement in verbal memory was detected. Our data suggest that there is a positive relationship between improved verbal memory and psychosocial functioning that was confirmed with the significant correlation found between changes in the FAST total score and verbal memory in the functional remediation group. This is important since verbal memory and executive functions have been identified as predictors of global functioning. Reference Martino, Marengo, Igoa, Scápola, Ais and Perinot2,Reference Bonnin, Martinez-Aran, Torrent, Pacchiarotti, Rosa and France3,Reference Laes and Sponheim23 Therefore, by improving these cognitive processes patients are better equipped with the necessary underlying skills to find greater success in their daily activities that most often require adequate cognitive functioning. Functional remediation can target, as a secondary objective, the cognitive deficits of patients with bipolar disorder, yielding not only better neuropsychological skills but also a generalised improvement in functional abilities, such as the before-mentioned autonomy. However, results have to be interpreted with caution as a learning effect in the tests related to verbal memory cannot be excluded either, because of a lack of parallel tests. However, verbal memory improvements were observed only in the functional remediation group.
Findings from other studies
Despite the well-characterised association between neurocognitive deficits and functional outcome in patients with euthymic bipolar disorder, only three trials so far have addressed the efficacy of neurocognitive-based psychosocial interventions. The first one is a small, uncontrolled trial of 18 participants with bipolar disorder showing an improvement in psychosocial and occupational functioning. Reference Deckersbach, Nierenberg, Kessler, Lund, Ametrano and Sachs24 The second study is a multicentre, randomised, rater-masked clinical trial showing the efficacy of functional remediation in improving psychosocial functioning, which is the first part of the present study. Reference Torrent, Bonnin, Martinez-Aran, Valle, Amann and González-Pinto9 Recently, another randomised trial has been registered aiming to evaluate the effects of cognitive remediation in 40 participants with bipolar disorder in full or partial remission with persistent cognitive difficulties, but results are still not available. Reference Demant, Almer, Vinberg, Kessing and Miskowiak25 Similarly, Bauer and colleagues Reference Bauer, McBride, Williford, Glick, Kinosian and Altshuler26 found that collaborative care, a psychosocial intervention, showed a positive effect on functioning in the long term. However, this intervention was not based on a neurocognitive intervention; instead it was based on three different components that addressed the patient, provider and systems aspects of care. This suggests that there might be different paths to achieve functional improvement in patients with bipolar disorder, ranging from neurocognitive-based interventions to community-care programmes. Altogether, it highlights the need to study the long-term efficacy of the programmes aiming to improve functional outcome in those with bipolar disorder. Reference Fuentes-Dura, Balanza-Martinez, Ruiz-Ruiz, Martínez-Arán, Girón and Solé27
Future directions
The above-mentioned studies, and particularly the functional remediation studies, have just started to be explored in bipolar disorder, so that the cognitive domains to be trained; the feasibility of the programme, including number and frequency of session; duration and intensity of the intervention warrant further investigation. Moreover, other relevant variables may influence results, such as age of patients, chronicity or severity of illness (such as number of episodes). Patients included in this study were chronic, with an average age of 40 years. Probably younger patients, earlier in the course of the illness, may have greater potential for cognitive and functional improvement. For these reasons, the development of interventions aiming at preventing neurocognitive and functional impairment in the early stages of the illness are urgently needed.
Moreover, further studies should address the identification of the moderators and mediators in the prediction of functional outcome because this may help to disentangle the complex network of variables that contribute to functional outcome in bipolar disorder. Reference Vieta28 In fact, a recent study found that patients' composite verbal memory score explained partially the variability of functional outcome (measured by means of FAST) at 6-month follow-up. Verbal memory had a significant indirect effect on functional outcome, partly mediating the relationship between depressive symptoms and functional status. Reference Bonnin, Gonzalez-Pinto, Sole, Reinares, González-Ortega and Alberich29 Another line of future research is that further studies will have to confirm the duration of the effects of the intervention and to evaluate whether or not the inclusion of some regular booster sessions may help to maintain the effects of the intervention longer term. Finally, computerised neurocognitive training is also needed. So far, little evidence exists of neuropsychological computerised programs for patients with bipolar disorder. A recent study with a sample of affective patients including some with bipolar disorder has been published with positive results (improvement neuropsychological and clinical outcome). Reference Preiss, Shatil, Cermakova, Cimermanová and Ram30 In this regard, functional remediation may be a promising tool in combination with other psychosocial interventions to improve functional outcome.
Strengths and limitations
The most relevant limitations of the study are that the follow-up is still relatively short and the study lost power because of the small sample size; in light of this, missing cases were excluded for the analyses and considered ‘missing at random’. However, the study provides strong evidence that improvements in psychosocial functioning can be achieved and maintained beyond the end of a structured psychological intervention with emphasis on neurocognitive strategies. The randomised, rater-masked design and the presence of not only a TAU but also a psychoeducation arm provides further strength to the findings. Establishing how to adjust and implement interventions such as functional remediation for people with bipolar disorder in the community and how to make them cost-effective is the next step forward.
Acknowledgements
The CIBERSAM Functional Remediation Group consists of: Analucía Alegría, Susana Al-Halabi, Silvia Alonso-Lana, Celia Anaya, Jesus Valle, Vicent Balanzá-Martínez, Francesc Colom, Sara Barbeito, Julio Bobes, Ana Calvo, Esther Cerrillo, Patricia Correa, Núria Custal, Patricia Fernández, Miryam Fernández, Inmaculada Fuentes-Durá, Gonzalo Galván, Sandra Isella, Ramon Landín-Romero, María Mayoral, José Manuel Menchón, Jessica Merchan-Naranjo, Esther Jiménez, Jordi Ortiz-Gil, Isabella Pacchiarotti, Adriane R Rosa, Marta Rapado-Castro, José-María Rodao, Pilar A Saiz, Jose Sánchez-Moreno, Bárbara Segura, Gabriel Selva, Jerónimo Saiz-Ruiz, Marta Subirá, Imma Torres, Amaia Ugarte, Patricia Vega.








eLetters
No eLetters have been published for this article.