Introduction
Detecting recidivous cholesteatoma following surgical treatment continues to be a challenge of otological practice. Published literature suggests that cholesteatoma recidivism occurs in 5–17 per cent of canal wall down and 9–70 per cent of canal wall up procedures.Reference Tomlin, Chang, McCutcheon and Harris1
The methods of surveillance for cholesteatoma have evolved, with diffusion-weighted magnetic resonance imaging (MRI) becoming the modality of choice over second look surgery. Diffusion-weighted MRI has been demonstrated to be reliable for detecting cholesteatomas as small as 2–3 mm.Reference Corrales and Blevins2,Reference Lingam, Nash, Majithia, Kalan and Singh3 A systematic review by Jindal et al. showed that non-echoplanar imaging MRI ‘has a sensitivity, specificity, and positive and negative predictive value of 91 per cent, 96 per cent, 97 per cent, and 85 per cent, respectively’.Reference Jindal, Riskalla, Jiang, Connor and O'Connor4
Non-echoplanar diffusion-weighted imaging is preferred to other MRI sequences because it is advantageous in distinguishing cholesteatoma from inflammation by providing thinner cuts, higher resolution and less artefact. This translates into a reduced risk of undertaking unnecessary second look procedures.Reference Lingam, Nash, Majithia, Kalan and Singh3,Reference Jindal, Riskalla, Jiang, Connor and O'Connor4,Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5
When compared with second look surgery, diffusion-weighted MRI is favoured because it is lower in risk and cost, especially when there is no evidence of cholesteatoma in around 52–67 per cent of cases.Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5
False positive diffusion-weighted imaging findings can result in unnecessary revision surgery, which places patients in danger of unnecessary complications and produces additional healthcare costs.Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5 False positive diffusion-weighted imaging findings are poorly described in the literature with reference to cholesteatoma surveillance.Reference Lingam, Nash, Majithia, Kalan and Singh3,Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5
We describe the cases of two patients with cartilage grafts producing false positive findings mimicking cholesteatoma with genuine diffusion restriction on diffusion-weighted MRI who had no evidence of disease at second look surgery.
Case reports
Patient 1
The first patient was a 59-year-old female who underwent a routine diffusion-weighted MRI to exclude residual disease two years after clearance of a left-sided cholesteatoma prior to discharge from further follow up. At the time of scanning, she was asymptomatic and clinical examination was normal, with no evidence suggestive of residual disease. She had undergone a left attico-antrostomy in 2017 to remove a left attic cholesteatoma that extended into the mastoid antrum. The attic defect had been closed with a tragal cartilage graft.
The diffusion-weighted MRI showed a 2-mm area of restricted diffusion in the left epitympanum (Figure 1), which corresponded to a low area on the apparent diffusion co-efficient map.

Figure 1. Coronal plane magnetic resonance imaging (non-echoplanar diffusion-weighted imaging) showing an area of restricted diffusion in the left epitympanum.
On further clinical examination, no attic defect or keratin was detected. However, there was evidence of fullness in the left attic, and therefore a high-resolution non-contrast computed tomography (CT) scan of the temporal bones was requested to further evaluate the area. The CT scan (Figure 2) demonstrated a small focal opacity in Prussak's space, consistent with the MRI findings.
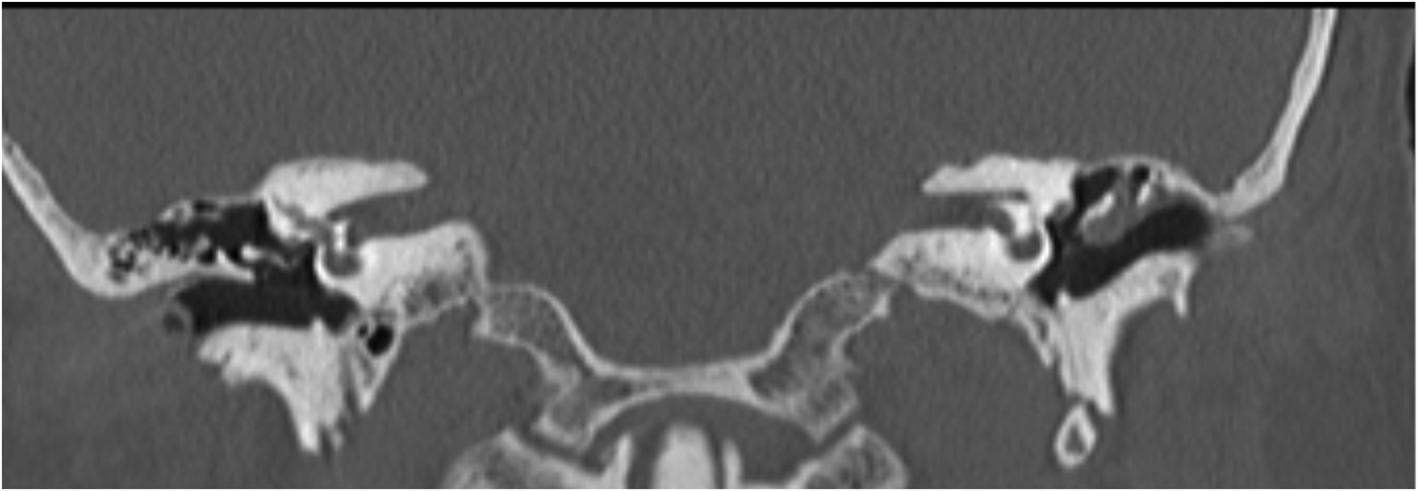
Figure 2. Axial plane computed tomography of temporal bones showing a left-sided intermediate density opacity in Prussak's space.
Second look tympanoplasty was undertaken with superior tympanomeatal and conchomeatal flaps elevated for access. The attic was visualised well and was also inspected with a 30° otoendoscope. Cartilage filler was present at the site corresponding to the diffusion restriction on the MRI, with no evidence of recidivous cholesteatoma.
Patient 2
The second patient was a 53-year-old female who had undergone a left mastoidectomy in 1977, followed by a right atticotomy with cartilage graft in 2017 to reduce the size of the cavity.
She had presented to the ENT department acutely in 2020 with right-sided post-auricular pain; there was no discharge, hearing loss, vertigo or tinnitus. On examination, the right attic was retracted, and although the full depth of the retraction was not fully visualised, there was no evidence of keratin or discharge. There were no concerns regarding the left ear.
A high-resolution CT scan of the temporal bones was performed (Figure 3a), demonstrating non-specific opacification within the right aditus ad antrum and the mastoid antrum. Non-echoplanar diffusion-weighted MRI demonstrated an area of diffusion restriction (Figure 3b) consistent with the area of opacification on the CT scan.

Figure 3. (a) Axial plane computed tomography of temporal bones showing evidence of bilateral mastoidectomies with non-specific opacities in the surgical cavities. (b) Coronal plane magnetic resonance imaging (non-echoplanar diffusion-weighted imaging) showing evidence of bilateral diffusion restriction.
Right revision atticotomy was undertaken; however, at operation, no cholesteatoma was encountered, and the area of diffusion restriction corresponded to the cartilage graft that had been used in the original procedure to reduce the size of the mastoid cavity.
Discussion
There are a number of published cases of false positive non-echoplanar imaging findings that include malignancy (external auditory canal squamous cell carcinoma), structures containing fluid (e.g. abscess cavity, cyst or cholesterol granuloma, or encephalocele), iatrogenic causes (e.g. cartilage or bone grafts; bone dust, pâté or powder; silastic sheet and dental brace artefact) and incidental findings (e.g. non-specific inflammation, cerumen and tympanosclerosis).Reference Lingam, Nash, Majithia, Kalan and Singh3,Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5
Lingam et al. described methods to negate pitfalls in specificity, such as multi-disciplinary discussion of questionable high diffusion-weighted imaging signals between otologists and radiologists in order to corroborate information such as the operative approach, location and type of materials used, confidence of successful clearance, extent of disease, current clinical status of the ear, and examination findings, which are useful factors for determining the risk of recidivism. They also suggested that additional imaging, such as further MRI sequences, apparent diffusion co-efficient values and fusion with high-resolution CT images, is a good adjunct to diffusion-weighted imaging and apparent diffusion co-efficient mapping to interrogate potentially spurious results.Reference Lingam, Nash, Majithia, Kalan and Singh3
Diffusion-weighted imaging relies upon the measurement of Brownian motion of water molecules because diffusion restriction occurs as a result of limited motion of water molecules within tissues. Cellular tissue contains fluid, giving it a lower diffusion co-efficient in comparison with non-cellular structures and therefore producing high signal intensity in material such as keratin.Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5 Apparent diffusion co-efficient mapping quantifies the diffusion of water molecules in tissue and can be used to cross-examine areas of diffusion restriction, distinguishing between true restriction and T2-weighted shine-through.Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5
Interestingly, in the case of patient 1, despite multiple modalities of imaging, the cartilage filler was not identifiable as a false positive finding. The area of diffusion restriction from the cartilage filler corresponded to the same point on the apparent diffusion co-efficient map and was consistent with the high-resolution CT temporal bone imaging. Patient 2 had also undergone high-resolution CT of the temporal bone in addition to non-echoplanar imaging MRI, and again, even with additional imaging techniques, the false positive finding was not discernible through imaging alone. We ask whether re-look surgery could be avoided with repeat scanning in patients who have diffusion restriction in the presence of features that favour a false positive finding over recidivous cholesteatoma.
The timing of post-operative surveillance scanning remains a point of debate in terms of both length of follow up and frequency of imaging. Steens et al. found that 14 of 45 (31 per cent) of post-operative patients with a normal clinical assessment and no disease on their first follow-up diffusion-weighted imaging had positive or equivocal findings on repeat scanning 6 months later, and 5 of 45 (11 per cent) had cholesteatoma confirmed during re-look surgery.Reference Steens, Venderink, Kunst, Meijer and Mylanus6
Muhonen et al. discussed the only other four reported cases of false positive non-echoplanar diffusion-weighted imaging results associated with cartilage grafts. The authors were confident in all cases that complete cholesteatoma clearance was achieved during the initial surgical procedures. One patient underwent revision surgery with no evidence of disease encountered. The other three patients were assessed with clinical examination and repeat imaging with stable or resolved scan findings and no cholesteatoma recurrence on follow up at 52–84 months. On the basis of their experiences, they recommended further non-echoplanar diffusion-weighted imaging to be undertaken at 6 to 12 months where scan findings are suspicious for a false positive.Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5
• Diffusion weighted magnetic resonance imaging (MRI) is a trusted method for assessing post-operative cholesteatomas, but it is not infallible
• Cartilage grafts can produce diffusion restriction on diffusion-weighted imaging sequences, mimicking cholesteatoma
• False positive diffusion-weighted imaging findings should be considered in cases where cholesteatoma clearance is strongly assured
• Clear documentation of the location of cartilage grafts can aid in identifying a false positive MRI finding of cholesteatoma
• When considering false positive diffusion restriction in the context of cholesteatoma, a high index of suspicion for recurrence should be maintained along with a low threshold for second look surgery
Features that may raise concern for false positive diffusion restriction are reduced size and intensity of the lesion on repeat imaging and presence of diffusion restriction away from the initial cholesteatoma location. Conversely, non-resolving lesions, those that increase in size or intensity, and development of symptoms or clinical signs suggestive of recidivism are features that warrant consideration of a further procedure.Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5
We acknowledge that it is difficult to provide definitive advice because there is limited evidence in the medical literature to support the validity of our recommendations; however, we suggest careful documentation of the cholesteatoma location and confidence of clearance in the operation notes. The location of any bone, cartilage or silastic used for grafting should also be noted clearly. In cases where clinical suspicion of recidivism is low, findings of diffusion restriction should be discussed in detail between the otologist and the radiologist. If the clinical and radiological features favour a false positive finding, further surveillance scanning with non-echoplanar diffusion-weighted imaging at 6–12 months may be appropriate because both Muhonen et al. and Steens et al. have published cases demonstrating resolution of abnormal diffusion restriction in subsequent re-imaging.Reference Muhonen, Mahboubi, Moshtaghi, Sahyouni, Ghavami and Maducdoc5,Reference Steens, Venderink, Kunst, Meijer and Mylanus6 The caveat to this recommendation is to ensure that close clinical follow up is observed, maintaining a high suspicion for cholesteatoma recurrence and a low threshold for consideration of second look surgery. We advise that the presence of adverse features, such as clinical signs of cholesteatoma, presence of diffusion restriction at the location of the original site and evidence of progression on serial imaging are indications for revision surgery.
Conclusion
The presence of cartilage grafts can produce false positive non-echoplanar diffusion-weighted imaging findings. This is poorly documented in the literature and must be considered where there is high confidence of complete cholesteatoma clearance, presence of diffusion restriction away from the location of the original disease, and diminishing intensity or dimensions on repeat imaging.
Where a false positive is considered, we recommend close clinical follow up and repeat imaging at 6–12 months, with a low threshold for consideration of revision surgery where new symptoms or clinical signs suggestive of recidivism develop.
Competing interests
None declared





