Introduction
In the UK, more than 100,000 people experience a stroke annually, and there are currently over 1.2 million stroke survivors (Stroke Association, 2017). Although stroke usually occurs in older adults (median = 77 years), around 25% occur in those of working-age, leading to unemployment and loss of income (McKevitt et al., Reference McKevitt, Fudge, Redfern, Sheldenkar, Crichton, Rudd, Forster, Young, Nazareth and Silver2011; Stroke Association, 2017). Given the sudden and life-altering nature of a stroke, adjustment difficulties are common (Maaijwee et al., Reference Maaijwee, Rutten-Jacobs, Schaapsmeerders, Van Dijk and de Leeuw2014). For instance, approximately 31% of stroke survivors experience depression (Hackett and Pickles, Reference Hackett and Pickles2014) and 20–25% experience anxiety disorders/symptoms at any time (Burton et al., Reference Burton, Murray, Holmes, Astin, Greenwood and Knapp2013). Additionally, fatigue, emotionalism, low self-efficacy, low self-esteem, altered self-concept and post-traumatic stress are also common following a stroke (Morris, Reference Morris2020). These adjustment difficulties are associated with poorer quality of life (Bays, Reference Bays2001; Jeong et al., Reference Jeong, Kang, Bae, Kim, Kim, Shin, Kim, Park, Cho and Yoon2012), worse functional recovery (West et al., Reference West, Hill, Hewison, Knapp and House2010) and greater health care costs (Gillham et al., Reference Gillham, Carpenter and Leathley2012).
The UK National Stroke Strategy (Department of Health, 2007) emphasised the central role of psychological care in supporting post-stroke rehabilitation. Accordingly, the National Institute for Health and Clinical Excellence (NICE, 2010) and the Royal College of Physicians National Clinical Guidelines for Stroke (Royal College of Physicians, 2016) recommend routine assessment and treatment of psychological difficulties following a stroke. Although randomised controlled trials have shown some support for psychological interventions after stroke (i.e. Ahrens et al., Reference Ahrens, Shao, Blackport, Macaluso, Viana, Teasell and Mehta2023; Hill et al., Reference Hill, House, Knapp, Wardhaugh, Bamford and Vail2019; Majumdar and Morris, Reference Majumdar and Morris2019; Niu et al., Reference Niu, Sheng, Chen, Ding, Li, Shi and Ye2022; Nguyen et al., Reference Nguyen, Wong, McKay, Rajaratnam, Spitz, Williams and Ponsford2019; Thomas et al., Reference Thomas, Walker, Macniven, Haworth and Lincoln2013; Watkins et al., Reference Watkins, Auton, Deans, Dickinson, Jack, Lightbody and Leathley2007), a recent narrative review suggests evidence for the efficacy of psychological interventions for post-stroke anxiety and depression remains limited (Chun et al., Reference Chun, Ford, Kutlubaev, Almeida and Mead2022). As such, further exploration of psychological interventions for stroke survivors is needed.
Acceptance and commitment therapy (ACT) has been shown to be efficacious in improving well-being and recovery outcomes in a range of long-term conditions, such as chronic pain (Hughes et al., Reference Hughes, Clark, Colclough, Dale and McMillan2017), brain injury (Sander et al., Reference Sander, Clark, Arciniegas, Tran, Leon-Novelo, Ngan, Bogaards, Sherer and Walser2020; Whiting et al., Reference Whiting, Deane, McLeod, Ciarrochi and Simpson2019), multiple sclerosis (Han, Reference Han2021), and cancer (Li et al., Reference Li, Li, Guo, Li and Yang2021). Emerging evidence indicates that ACT may also be an efficacious treatment approach for post-stroke adjustment difficulties (Graham et al., Reference Graham, Gillanders, Stuart and Gouick2015; Large et al., Reference Large, Samuel and Morris2019; Majumdar and Morris, Reference Majumdar and Morris2019, Niu et al., Reference Niu, Sheng, Chen, Ding, Li, Shi and Ye2022; Rauwenhoff et al., Reference Rauwenhoff, Bol, Peeters, van den Hout, Geusgens and van Heugten2023). For example, a recent randomised controlled trial demonstrated that group-based ACT was efficacious in reducing depression, improving self-report health status and increasing hopefulness in stroke survivors (Majumdar and Morris, Reference Majumdar and Morris2019). Qualitative interviews with the participants from this study revealed that ACT was helpful in facilitating the acceptance of a changed reality and the adjustments to impairments resulting from stroke (Large et al., Reference Large, Samuel and Morris2019). Indeed, in the recent update of the National Clinical Guideline for Stroke for the UK and Ireland, ACT was included as one of the recommended psychological interventions for stroke survivors at risk of developing post-stroke anxiety or depression (Intercollegiate Stroke Working Party, 2023).
One of the basic assumptions of ACT is that psychological suffering is a core feature of being human (Hayes et al., Reference Hayes, Strosahl and Wilson2011). Habitual human responses to suffering, including experiential control and avoidance, when applied in an unworkable manner, are regarded as ineffective due to the inevitability of recurrent suffering (Luoma et al., Reference Luoma, Hayes and Walser2017). Paradoxically, ACT does not aim to reduce distress by getting rid of it, rather by helping the client make contact with unwanted experiences without excessive or rigid attempts to transform the experiences, when doing this is in the service of moving the client towards a life they value (Hayes et al., Reference Hayes, Luoma, Bond, Masuda and Lillis2006; Luoma et al., Reference Luoma, Hayes and Walser2017). Essentially, ACT is not about changing distress in itself, but rather modifying how one relates to their distress. Accordingly, the development of psychological flexibility is a central therapeutic process in ACT, defined as the ability to consciously contact the present moment, and to adapt or persist in behaviours in accordance with personal values (Hayes and Smith, Reference Hayes and Smith2005).
Majumdar and Morris (Reference Majumdar and Morris2019) highlighted several features of ACT that suggest its suitability in managing post-stroke adjustment difficulties. For example, they suggest that ACT’s focus on acceptance of distress and ‘getting on with life’, as well as seeking to change the function of or context around unwanted cognitions (rather than the form or content as in traditional cognitive behaviour therapy), may be more appropriate for responding to stroke symptoms which can be real, persistent and therefore difficult to cognitively challenge. They go on to suggest that the promotion of contact with the present moment and openness to experience might allow an individual to engage with experiences beyond distress or disability. Additionally, they suggest that the exploration of values may help the process of goal setting which is a common practice in stroke rehabilitation.
Since the onset of the COVID-19 pandemic, telerehabilitation has emerged as an alternative to in-person care. Accordingly, the National Clinical Guideline for Stroke for the UK and Ireland recommended that telerehabilitation should be considered for stroke survivors to augment conventional in-person rehabilitation (Intercollegiate Stroke Working Party, 2023). A recent systematic review demonstrated that telerehabilitation for stroke survivors may be as effective as usual care on a range of outcomes including self-efficacy, independence, activities of daily living, and motor function (Appleby et al., Reference Appleby, Gill, Hayes, Walker, Walsh and Kumar2019). Specifically, telephone-based telerehabilitation has been found to improve global functioning, post-traumatic symptoms, sleep quality and depressive symptoms relative to usual care in traumatic brain injury survivors (Ownsworth et al., Reference Ownsworth, Arnautovska, Beadle, Shum and Moyle2018). Notably, with regard to psychological interventions, existing evidence on telerehabilitation has focused on cognitive behavioural therapy in a traumatic/acquired brain injury population (Boulos et al., Reference Boulos, Colella, Meusel, Sharma, Peter, Worthington and Green2023; Fann et al., Reference Fann, Bombardier, Vannoy, Dyer, Ludman, Dikmen and Temkin2015). To the best of our knowledge, the efficacy of ACT delivered via telerehabilitation for stroke survivors has yet to be explored.
Given this gap in the literature, the present case study aims to explore whether ACT is an efficacious approach in managing post-stroke adjustment difficulties in a working-aged man, when therapy was delivered via telerehabilitation. It describes the assessment, formulation, treatment and outcome following six sessions of ACT. The efficacy of the intervention is evaluated on measures of psychological flexibility and psychological distress.
Presenting problem
Reason for referral
John (pseudonym) was a man in his early-40s who, following a diagnosis of a partial anterior cerebral circulation stroke (PACS) was seen at home by an Early Supported Discharge (ESD) team. As recommended by the NICE (2010) and the Royal College of Physicians (2016) guidelines, John was screened for post-stroke cognitive impairment and mood difficulties. Whilst John reported some minor cognitive changes following his stroke (i.e. shorter attention span, reduced processing speed, greater distractibility), he explained that these symptoms were not significant. Indeed, John’s performance on the Oxford Cognitive Screen (Demeyere et al., Reference Demeyere, Riddoch, Slavkova, Bickerton and Humphreys2015) revealed no clear impairments in the cognitive domains that are frequently affected by stroke (i.e. language, attention, memory, praxis, numerical abilities, visual abilities, etc.). John also passed the Rookwood Driving Battery (McKenna, Reference McKenna2009) indicating no cognitive concerns in relation to driving. However, assessment of John’s mood using the Clinical Outcomes Routine Evaluation-Ten Item Version questionnaire (see ‘Assessment measures’ section below) yielded a total score of 23, indicating moderate to severe levels of distress. Indeed, John reported feeling highly anxious and low in mood following his stroke which was impairing his daily functioning. He also experienced sleep disturbance and difficulties chewing his food, in the absence of any dysphagia (i.e. acquired swallowing difficulties). Given John’s mood difficulties, coupled with no physical or medical explanations for his difficulties with chewing, he was referred to clinical psychology for further assessment.
Assessment
John lived with his wife and two children. At the onset of his stroke symptoms, John experienced severe headaches and dizziness, and sought medical assistance from various services (i.e. General Practitioner, Accident & Emergency, Neurology) but was misdiagnosed as having a migraine. After 4 weeks of repeated consultations, he was eventually diagnosed with a stroke. However, the headache, dizziness and fatigue symptoms continued to be problematic thereafter, causing him to spend much of his time in his house reportedly sitting with his head in his hands. He described how he struggled to initially access a referral for rehabilitation, although he was eventually referred to the ESD team. These experiences left him feeling let down by medical professionals, which led to him ruminating on the dangers of his misdiagnosis given that he was subsequently driving long distances for his job. Moreover, these experiences led John to think that he was wasting medical professionals’ time which contributed to a belief that ‘people look at me and think, you’re fine’, as well as a sense of having to be self-sufficient in his recovery. Despite this, he felt conflicted over the fact that he had questions about the cause of his stroke that he wished to discuss with his stroke medical consultant.
As stated, prior to the stroke, John worked as a transport worker, driving at least 500 miles per day. He enjoyed his job and was worried about whether he would be able to continue working and the financial implications of this. He went on to express concerns around his ability to provide for his family and the impact of not earning on their lifestyle. Accordingly, he spent a lot of time problem-solving how he would be able to support his family in the event of being unable to return to his job. Indeed, John identified family life as being important and whilst he previously drove longer distances for his job, he decided to work closer to home when his children were young so that he could spend more time with his family.
John reported feeling guilty about currently being unable to share parenting and household responsibilities with his wife due to his symptoms. For instance, he described feeling lethargic, unmotivated and overwhelmed by family situations (e.g. the children’s morning routine, conversations with the children about household chores, etc.) that were previously manageable prior to the stroke. As such, he avoided potential conflict by staying in bed until the children had left for school and spent more time alone in his bedroom. Aside from the routine and necessary parenting responsibilities that John felt unable to do, he also expressed guilt at being unable to play and engage in pleasurable activities with his children. Given that his wife had now taken over these roles, this had an impact upon how he saw himself as a partner, reporting a sense of failure.
John reported that he had ‘always been a worrier’ but had not experienced any significant mental health difficulties in the past. He reported that prior to his stroke, his typical way of responding to emotional content was to avoid it via distraction or displace it with positive thoughts and emotions. Specifically, he was worried about having a further stroke and reported predictions that any further strokes may result in more severe disability. This caused him to avoid leaving the house on his own through the fear of not being able to summon medical assistance. This meant that he was not engaging in preferred pleasurable activities such as walking his dog with his wife, and cycling with his family.
John also reported difficulties with his eating and sleep. Despite having a healthy appetite prior to the stroke, John felt that he did not have the energy to chew his food and was taking a long time to finish his meals. Accordingly, he began eating on his own, away from his family. He also reported difficulties falling asleep and waking throughout the night. For example, he was spending about 3 hours most nights ruminating on his worries in bed before falling asleep and waking up intermittently during his 4 to 5 hours of sleep. He also reported feeling isolated as his stroke occurred during the coronavirus pandemic, meaning that he was not able to have much contact from friends or family.
Methodology
Case study design
This case study employed a case-controls design where John’s scores on measures of distress and ACT processes were compared with normative data. Data from non-clinical samples was chosen for comparison to assess whether John’s scores were in the ‘normal’ ranges at selected time points.
Assessment measures
Accordingly, weekly measures on the Valuing Questionnaire (VQ; Smout et al., Reference Smout, Davies, Burns and Christie2014) were taken during a 4-week baseline period (i.e. B1 to B4), during six sessions of active therapy (i.e. S1 to S6) and during a 4-week post-therapy period (i.e. P1 to P4), as well as at 3-month (3M) and 6-month (6M) follow-up. Measures on the Clinical Outcomes in Routine Evaluation (CORE-10; Barkham et al., Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013) and Comprehensive Assessment of Acceptance and Commitment Therapy Processes (CompACT; Francis et al., Reference Francis, Dawson and Golijani-Moghaddam2016) were also taken at B1, S1, S6, P4, 3M and 6M.
Clinical Outcomes in Routine Evaluation
The CORE-10 is a 10-item self-report measure which assesses psychological distress (Barkham et al., Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013). The items are rated on a 5-point Likert scale ranging from 0 (not at all) to 4 (most or all of the time), with higher total scores indicating greater distress. The CORE-10 has strong internal consistency with a Cronbach’s alpha of .90. The 95% reliable change index for this measure is 8 (Barkham et al., Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013). The cut-off score for clinically significant change between clinical and non-clinical populations is 10/11 (where 10 is in the non-clinical range and 11 is in the clinical range), while a cut-off score of 13 yields sensitivity and specificity values of .92 and 0.72, respectively, against a diagnosis of DSM-IV depression (Barkham et al., Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013; Connell and Barkham, Reference Connell and Barkham2007; Jacobson and Truax, Reference Jacobson and Truax1991).
Comprehensive Assessment of Acceptance and Commitment Therapy Processes
The CompACT is a 23-item self-report measure of psychological flexibility (Francis et al., Reference Francis, Dawson and Golijani-Moghaddam2016). The CompACT consists of three subscales: Openness to Experience (OE) and detachment from literality capturing the ACT processes of acceptance and diffusion; Behavioural Awareness (BA) or self-awareness and perspective capturing the ACT processes of present moment awareness and self as context; and Valued Action (VA) capturing the ACT processes of values and committed action (Francis et al., Reference Francis, Dawson and Golijani-Moghaddam2016). Items are rated on a 7-point Likert scale ranging from 0 (strongly disagree) to 6 (strongly agree), with higher CompACT total scores indicating greater psychological flexibility. The CompACT has demonstrated adequate internal consistency, with a Cronbach’s alpha of .91 (Francis et al., Reference Francis, Dawson and Golijani-Moghaddam2016) and .90 (Gallego et al., Reference Gallego, McHugh, Villatte and Lappalainen2020) for the overall 23-item scale. Means and standard deviations for the CompACT and its subscales were not reported for the sample used in the original CompACT development study by Francis et al. (Reference Francis, Dawson and Golijani-Moghaddam2016). However, Gallego et al. (Reference Gallego, McHugh, Villatte and Lappalainen2020) reported CompACT total and subscale scores in a sample of university students (52.6% female) where CompACT total: M=88.13, SD=19.93, VA: M=35.89, SD=7.07, OE: M=34.80, SD=10.84 and BA: M=17.43, SD=5.97. Furthermore, Trindade et al. (Reference Trindade, Ferreira, Mendes, Ferreira, Dawson and Golijani-Moghaddam2021) reported the CompACT total score of M=86, SD=20.79, in a UK general population sample (81% female). However, subscale scores for the 23-item questionnaire were not reported in this latter study. Using the Cronbach’s alpha and standard deviation scores for the CompACT total values from Francis et al. (Reference Francis, Dawson and Golijani-Moghaddam2016) and Trindade et al. (Reference Trindade, Ferreira, Mendes, Ferreira, Dawson and Golijani-Moghaddam2021) (i.e. .91 and 20.79, respectively), we calculated a reliable change index (RCI) of 17 (95% CI) and for the CompACT total score (Evans et al., Reference Evans, Margison and Barkham1998; Jacobson and Truax, Reference Jacobson and Truax1991). It was not possible to calculate a cut-off score for clinically significant change due to the absence of any known normative data on the CompACT from a clinical sample of stroke survivors experiencing mental health difficulties.
Valuing Questionnaire
The VQ is a 10-item self-report measure which assesses the extent of personal values enactment (Smout et al., Reference Smout, Davies, Burns and Christie2014). Items are rated on a 7-point Likert scale ranging from 0 (not at all true) to 6 (completely true). The VQ consists of two subscales: Progress and Obstruction. Higher Progress subscale scores represent greater enactment of values including clear awareness of what is personally important and perseverance. In contrast, higher Obstruction subscale scores represent greater disruption of valued living due to avoidance of unwanted experience and distraction from values by inattention to values or attention to other psychological experiences (Smout et al., Reference Smout, Davies, Burns and Christie2014). Norms for both a clinical and non-clinical populations for both subscales are as follows: Progress: clinical: M=12.80, SD=6.91; non-clinical: M=17.20, SD=6.44; Obstruction; clinical: M=18.90, SD=6.49; non-clinical: M=12.10, SD=6.88 (Smout et al., Reference Smout, Davies, Burns and Christie2014). Cronbach’s alpha internal consistency values for both the Progress and Obstruction subscales were .87 (Smout et al., Reference Smout, Davies, Burns and Christie2014). Using Smout et al.’s (Reference Smout, Davies, Burns and Christie2014) clinical norms, we calculated a RCI score of 13 (95% CI) for the Progress scale and 19 (95% CI) for the Obstruction scale and a cut-off score between clinical and non-clinical populations of 15 for the Progress scale and 16 for the Obstruction scale (Evans et al., Reference Evans, Margison and Barkham1998; Jacobson and Truax, Reference Jacobson and Truax1991).
Treatment
Formulation
A formulation of John’s psychological adjustment to stroke using the six core processes underlying psychological flexibility (Hayes et al., Reference Hayes, Luoma, Bond, Masuda and Lillis2006) is presented in Fig. 1. As indicated in the baseline psychometric measures, John had a clear awareness of his personal values (i.e. connecting with family, equality in parenting and household responsibilities, fun). However, he was engaging in unworkable actions that served as barriers to valued living, such as avoiding family situations that may trigger unwanted feelings (e.g. eating meals without family due to chewing difficulties, avoiding challenging conversations with his children, avoiding his children’s morning routine). He was also avoiding leaving his house alone, and not engaging in pleasurable activities (i.e. limited committed action).
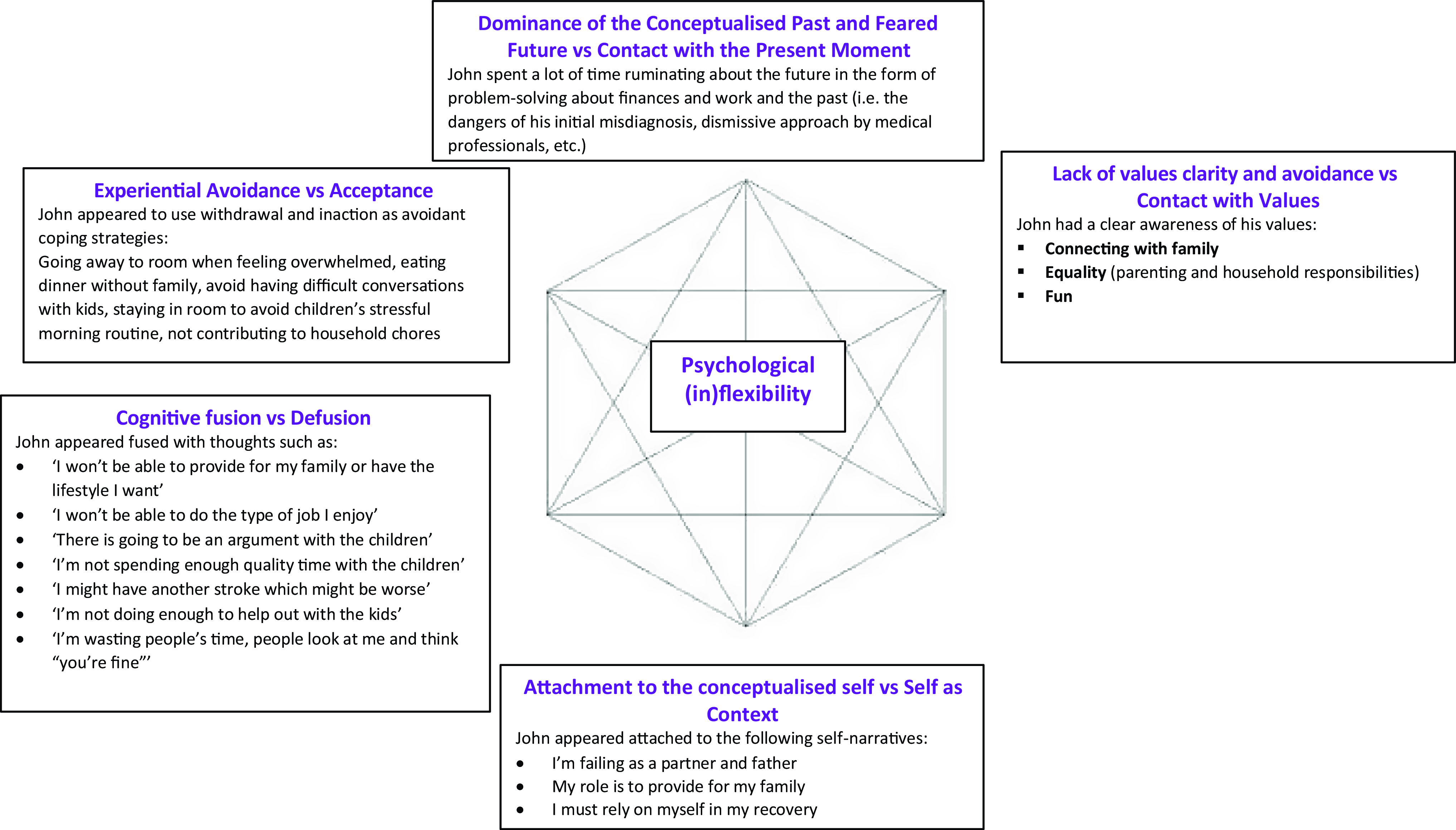
Figure 1. Formulation of John’s difficulties at assessment based on the Hexaflex (Hayes et al., Reference Hayes, Luoma, Bond, Masuda and Lillis2006).
John’s avoidance of behaviours that were more consistent with his values were hypothesised as being due to (a) having not previously developed formal skills in the acceptance of difficult emotions (e.g. anxiety, guilt, feeling overwhelmed) and physical sensations (e.g. headaches, dizziness), (b) often getting ‘hooked’ by rumination about his past misdiagnosis and problem-solving predicted future work and finance difficulties preventing contact with the present moment, (c) often becoming fused with thoughts related to his finances, work, parenting, health, and his role as a partner and (d) struggling to separate self-narratives (e.g. ‘I’m failing as a partner and father’) from the perspective of an observing self (i.e. attachment to the conceptualised self).
Goals for therapy and treatment rationale
John’s goals for therapy were to (1) gain a better understanding of his condition, (2) to manage his mood difficulties and (3) improve his sleep. Based on John’s formulation and goals, an ACT treatment approach was adopted. It was hypothesised that reducing the barriers to committed action (e.g. avoidance and ineffective coping strategies) as well as developing acceptance and mindfulness skills could help to reduce John’s experiential avoidance and, consequently, the dissonance between his behaviours and values. It was suggested that this would help him commit to approaching the stroke consultant to find out more about his condition (goal 1) and better manage his mood difficulties (goal 2). Moreover, it was hypothesised that cognitive defusion techniques and increasing access to a more stable sense of self (e.g. noticing the ‘observer self’) could help him manage the rumination, worries and associated mood difficulties (goal 2), that may have been interfering with his ability to sleep. This, coupled with increased values-based action which would intensify John’s physical activity in a paced way (to manage fatigue levels), was also hypothesised as having the potential to improve John’s sleep (goal 3). Indeed, sleep difficulties can be common after stroke and cognitive behavioural interventions have been suggested which are consistent with those outlined here (Baylan et al., Reference Baylan, Griffiths, Grant, Broomfield, Evans and Gardani2020; Herron et al., Reference Herron, Farquharson, Wroe and Sterr2018). This rationale, along with an explanation of ACT, was discussed with John and he consented to the intervention.
Course of therapy
The intervention was carried out by the primary author (J.O.), a trainee clinical psychologist who had completed the online ACT for Beginners course by Russ Harris and was working in a specialist stroke placement as part of a doctorate in clinical psychology training. The work was supervised by T.S., a clinical psychologist with seven years of experience using ACT with people who have had a stroke.
After the initial assessment session, John attended six sessions of individual ACT spread over a 2-month period. Weekly hour-long sessions were scheduled for the first 4 weeks, followed by fortnightly sessions for the final two sessions. As face-to-face work became more difficult when treatment commenced due to social distancing measures during the coronavirus pandemic, the intervention was carried out via telerehabilitation. Here, John opted for telephone calls rather than videocalls. Worksheets (i.e. Choice Point; see below) were sent to John via email, which were printed out and completed during the sessions.
Session 1 – Formulation and values
A formulation was mapped out collaboratively with John during the initial session and elaborated throughout treatment using the Choice Point Model (Ciarrochi et al., Reference Ciarrochi, Harris and Bailey2015) as outlined in Fig. 2 below. This summarised the “away moves” (or ineffective, values-incongruent actions) that were discussed in the assessment session (i.e., avoiding situations, sitting with his heads in his hands, not eating with his family etc) and went onto explore “towards moves” or effective, values-congruent actions. Here, John further reinforced his clear sense of his values (i.e., connecting with family, equality, fun) and goals for therapy which guided his definition of towards moves. Specifically, these were outlined as being more present with his family (i.e., helping children with homework, cycling with his family, having difficult discussions with children), leaving the house and driving on his own again, increasing his physical activity with the aim of improving his sleep and seeking information about his condition from medical professionals.

Figure 2. Formulation shared with John based on the Choice Point (Ciarrochi et al., Reference Ciarrochi, Harris and Bailey2015).
Session 2 – Creative hopelessness, defusion, contact with the present moment, acceptance
John’s formulation indicated that he was avoidant of difficult thoughts, emotions and physical sensations which were acting as a barriers to valued living. Therefore, this session initially focused on creative hopelessness, which involves recognising that excessive experiential avoidance is unworkable in the longer term and that learning different ways of managing them may be more adaptive (Harris, Reference Harris2019). John completed the ‘Join the D.O.T.S.’ exercise (Harris, Reference Harris2019), which is a semi-structured interview used to explore the types of experiential avoidance strategies he was engaging in and their longer-term impact. This is with a view to exploring certain circumstances in which alternative acceptance-based methods of responding to distress may be more workable. Here, John identified that the short-term strategies he had engaged in to avoid unpleasant experiences (i.e. avoiding/withdrawing from stressful family situations, rumination, suppression of unwanted internal thoughts) were away moves because they were acting as longer-term barriers to him being more present with his family.
As part of this, John was introduced to a thought suppression exercise in which he was instructed to not think about ice-cream, designed to demonstrate the paradoxical effects of thought suppression (Wenzlaff and Wegner, Reference Wenzlaff and Wegner2000). Here, he initially reported that he was not thinking about ice-cream because he was distracting himself by thinking about chocolates, but then moved onto thinking about chocolate ice-cream. He drew parallels from this exercise to his rumination, having to exert increasing effort to distract himself from the unpleasant experiences which he reported was often ineffective and resulted in further rumination.
In further discussing John’s rumination, he was asked to identify the thoughts that were typically present. Here, John reported: ‘I’m not able to have the patience I used to have to follow through with difficult discussions with my child like I was able to before’, ‘Eating is something I should be able to do’, ‘I want to get back to work right now’ and ‘I’m not able to have the lifestyle or do the things I find pleasure in’. The defusion technique, Naming the Story (Harris, Reference Harris2019) was then used where the client is asked to imagine that these thoughts made up a documentary or autobiography of their life. The client is asked to give that story a name and practise noticing when it becomes activated. Here, John identified these thoughts as his ‘Not Able To’ story.
During this session, John also identified that he often felt anxious and frustrated for not being able to do certain activities following his stroke and due to the coronavirus pandemic. An Acceptance of Emotions exercise (Harris, Reference Harris2019) was then undertaken in which John was asked to engage with and ‘open up’ to bodily feelings and sensations. Although John was able to use this exercise in relation to physical sensations, he found it much harder to contact emotions in session. This fitted with John’s reported tendency to generally avoid difficult emotions via distraction or displacement with positive thoughts and emotions. Accordingly, the workability of John’s different ways of responding to emotional content via the creative hopelessness exercise was revisited.
Session 3 – Acceptance, contact with the present moment, committed action
In this session, John reported greater acceptance of the unpleasant physical sensations (e.g. dizziness, headache, fatigue) he was experiencing, which allowed him to be more engaged in valued living over the previous week. He also managed to learn more about the specifics of his stoke during an appointment with a stroke medical consultant. He felt a sense of achievement when he was able to resolve stressful situations/discussions with his children instead of withdrawing to his room. He noticed that his daughter approached him for help with homework when he was in greater contact with the present moment. He also enjoyed spending time with his children, preparing a surprise birthday celebration for his wife.
This session focused on increasing John’s contact with the present moment and expanding his committed action. During the session, John was able to describe being more attuned to noticing physical sensations related to feeling overwhelmed (i.e. back pain, headache, sweating), which previously led to him ‘sitting with my head in my hands’. Additionally, John identified ‘fun’ as a value that was important to him given that part of his ‘Not Able To’ story related to being unable to do pleasurable activities during the pandemic. As such, he identified kicking a football in his garden with his dog and going for walks with his daughter as pleasurable activities to increase fun activities and time with his family.
Session 4 – Values and committed action, defusion, self as context
Over the previous week, John began noticing that he was able to engage in more towards moves that were congruent with his values, such as going cycling with his family, building Lego with his daughter, and playing football with his son. He felt a sense of achievement because he was able to reciprocate care for his wife by making her feel appreciated on her birthday. He was also proud that he was able to engage in acceptance and committed action (i.e. driving his daughter to a medical appointment despite feeling slightly anxious), given that it was the first time after his stroke that he had to drive a long distance. Additionally, he also noticed that he was engaging in fewer away moves such as withdrawing to his room. He noticed being less occupied with worries about having another stroke, ruminated less frequently about his ‘Not Able To’ story and described being more present with his thoughts. We discussed how he was developing the skills to notice, take perspective on and describe his private and explicit experiences, as well as changes in his behaviours.
John continued to identify further pleasurable activities to do with his family, such as setting up a table football/pool table and supporting his daughter’s interest in cars by working together on his own car. John explained that his main difficulty at this point was his disrupted sleep and this session focused more explicitly on this goal. He still spent about 1.5 hours in bed before falling asleep, although he no longer ruminated about his difficulties during that time. He then slept for 4–5 hours, waking up intermittently. In keeping with cognitive behavioural interventions to improve sleep after stroke (Herron et al., Reference Herron, Farquharson, Wroe and Sterr2018), John decided to increase his physical activity gradually over the next few weeks (i.e. increasing the distance of his daily walks by 1 mile per week), whilst managing the effect of this on his fatigue levels with pacing.
Sessions 5 and 6 – Committed action, acceptance
John managed to increase his physical activity to walking 5 miles each day by session 6, which resulted in improved sleep. It took no longer than 30 minutes for him to fall asleep and he was able to get 5–6 hours of uninterrupted sleep each night, comparable to the amount of sleep he had before the stroke. John reported having a greater acceptance of his stroke and was no longer noticing worries of having another one. He was also able to focus on adjusting to the outcomes of the stroke (e.g. taking on a different job role). He also reflected on his growing confidence about his ability to cope with difficult situations relating to his health. Specifically, an echocardiogram revealed a patent foramen ovale (PFO), which could be linked to his stroke. He was surprised at how well he coped with the diagnosis and was able to continue valued living whilst waiting for further tests and treatment. He also reported no longer ruminating on his ‘Not Able To’ story and was looking forward to the future by purchasing a new car and booking a family holiday. He also felt able to manage difficult discussions with his children and no longer felt overwhelmed in such situations. His eating had also returned to pre-stroke levels. He continued to engage in pleasurable activities such as going on walks with his wife and building Lego car models with his daughter.
Review session – ending treatment
John recognised that he managed to achieve all his therapy goals at the end of treatment. In reviewing the Choice Point model, he reflected on his progress throughout treatment, especially in relation to the reduction in away moves and the increase in towards moves. He found exploring pleasant activities particularly helpful in guiding his valued living. He was more accepting of his recovery progress and felt a reduced sense of urgency to return to work before he was ready. He agreed to wait another 6–8 weeks before starting a phased return to work as recommended by his occupational therapist and did not mind waiting until further tests and procedures (i.e. the fitting of a cardiac monitoring device) were completed before returning. He planned to continue monitoring his physical activity and sleep, and to engage in pleasant activities involving his family on a regular basis.
Follow-up: 3 and 6 months
Brief follow-up telephone calls were completed with John at 3 and 6 months by the second author (T.S.). At both intervals he agreed to fill in further outcome measures by post. At 3 months, John reported that he was continuing to make progress and had started a phased return to work although in a different role. At 6 months, he reported that he was back to work for 40 hours per week and had applied to get his driving licence back. He was hopeful of this being returned as well as getting through a date for the surgery on his PFO. He reported that things were generally going ‘in the right direction’.
Outcome
To evaluate the outcome of the intervention, the Singlims_ES.exe programme was used to compare John’s scores (CORE-10, CompACT and VQ) with those of control samples. This methodology produces effect size estimates, significance tests and percentile scores for each measure. The effect size estimate offers an analogue of Cohen’s d by calculating the average difference in standard deviation units between John’s score and a score of a randomly chosen member of the control sample.
Clinical Outcomes Routine Evaluation (CORE-10)
Figure 3 shows John’s response to treatment on the CORE-10 and Table 1 shows his scores in relation to a non-clinical sample. John’s baseline score on the CORE-10 was 22, reliably above the cut-off score for depression. When compared with a non-clinical sample (n=535, 49.8% female, M=4.70, SD=4.80) (Connell and Barkham, Reference Connell and Barkham2007), this baseline score was estimated to be at the 99th percentile. Results also indicated that John’s psychological distress at baseline was significantly higher than the control sample average, with a large effect size.

Figure 3. CORE-10 total scores at baseline, therapy and post-Intervention. Baseline: B1 to B4; therapy sessions: S1 to S6; post-intervention: P1 to P4; 3M: 3-month follow-up; 6M: 6-month follow-up. Higher CORE-10 scores indicate greater psychological distress.
Table 1. John’s CORE-10 scores compared with a non-clinical sample

B1, baseline 1; S6, end of therapy; 6M, 6-month follow-up; control sample: Connell and Barkham (Reference Connell and Barkham2007); M=4.70, SD=4.80, n=535.
However, his scores at S6 and 6M were below the control group mean at the 44th and 36th percentiles and had small and medium effect sizes, respectively. These differences were also no longer statistically significant, indicating that John’s distress levels were comparable with the control group average both immediately after the intervention and at follow-up. Following therapy (i.e. at S6, P4, 3M and 6M, respectively), his distress scores had reduced to the non-clinical range (i.e. <11) and were below the cut-off for depression (<13). The reduction in John’s distress scores from baseline to end of therapy (B1 – S6 = 18 points) and from baseline to 6-month follow-up (B1 – 6M = 19 points) shows reliable change over time (95% RCI for CORE-10 = 8).
Comprehensive Assessment of Acceptance and Commitment Therapy Processes (CompACT)
Figure 4 shows John’s response to treatment on the CompACT and Table 2 shows John’s CompACT scores compared with a non-clinical sample. John’s baseline score on the CompACT total scale was 56. When compared with a non-clinical sample in the UK (Trindade et al., Reference Trindade, Ferreira, Mendes, Ferreira, Dawson and Golijani-Moghaddam2021), this baseline score was estimated to be at the 7th percentile. This suggested that his psychological flexibility at baseline was significantly lower than the control sample mean, with a large effect size. Furthermore, in relation to Gallego et al.’s (Reference Gallego, McHugh, Villatte and Lappalainen2020) non-clinical sample, John’s baseline scores showed low willingness to experience internal events without attempting to avoid or control them (OE: 4th percentile) and low levels of mindful attention to current actions (BA: 5th percentile). In contrast, John reported better levels of engagement in meaningful activities (VA: 39th percentile).

Figure 4. CompACT total and subscale scores at baseline, therapy and post-intervention. Baseline: B1 to B4; therapy sessions: S1 to S6; post-intervention: P1 to P4; 3M: 3-month follow-up; 6M: 6-month follow-up. Higher CompACT total and subscale scores indicates greater psychological flexibility.
Table 2. John’s CompACT total scores compared with a non-clinical sample

B1, baseline 1; S6, end of therapy; 6M, 6-month follow-up; control sample: Trindade et al. (Reference Trindade, Ferreira, Mendes, Ferreira, Dawson and Golijani-Moghaddam2021): M=86, SD=20.79, n=665.
However, by the end of treatment, John’s scores at S6 and 6M were at the 85th and 96th percentiles, respectively. These scores were significantly higher than the control sample means, resulting in a large effect size. This suggests that John’s psychological flexibility went from being below average before treatment, to above average following treatment. The increase from John’s psychological flexibility scores from baseline to end of treatment (B1 – S6 = 52 points) and from baseline to 6-month follow-up (B1 – 6M = 67 points) shows reliable change over time (95% RCI for CompACT = 17).
As only Gallego et al. (Reference Gallego, McHugh, Villatte and Lappalainen2020) provided normative data from the CompACT subscales (see above) analysis of John’s CompACT subscale scores in relation to this sample were carried out. At B1, John’s VA, OE and BA scores were at the 40th, 4th and 4th percentiles, respectively. At S6, these had increased to the 87th, 64th and 88th percentiles, respectively; and at 6M, John’s scores VA, OE and BA scores were at the 94th, 94th and 88th percentiles, respectively, suggesting overall improvement across all CompACT subscales.
Valuing Questionnaire (VQ)
Figure 5 shows John’s response to treatment on the VQ. Baseline VQ Progress scale measurements (i.e. B1 to S1) were all above the cut-off score of 15 and therefore in the non-clinical range. These scores showed good levels of Progress (i.e. enactment of values including clear awareness of what is personally important and perseverance) and are largely consistent with John’s pattern of responding on the CompACT (i.e. adequate values-based processes). At S6, 3M and 6M, these scores remained in the non-clinical range. Although John’s scores on the VQ Progress scale increased from baseline to end of treatment (B1 – S6 = 12 points), it was slightly below the reliable change threshold (95% RCI for VQ Progress scale = 13).

Figure 5. Valuing Questionnaire subscale scores at baseline, therapy and post-intervention. Baseline: B1 to B4; therapy sessions: S1 to S6; post-intervention: P1 to P4; 3M: 3-month follow-up; 6M: 6-month follow-up. Higher Progress subscale scores indicate greater awareness and enactment of personal values. Lower Obstruction subscale scores indicate reduced disruption to valued living.
Table 3 shows John’s VQ Progress scores in relation to a non-clinical sample. In relation to a non-clinical sample described by Smout et al. (Reference Smout, Davies, Burns and Christie2014), his B1 score of 17 was estimated to be at the 49th percentile and comparable to the control average. However, his scores at S6 and 6M were estimated to be at the 97th and 98th percentiles, respectively, resulting in significantly higher progress scores than the control average, showing large effect sizes. These findings show that whilst John’s VQ progress score was similar to the control group at baseline, it moved above the control group average at the end of treatment and 6-month follow-up, indicating increased enactment of values, awareness of what is personally important and perseverance (Smout et al., Reference Smout, Davies, Burns and Christie2014).
Table 3. John’s Valuing Questionnaire Progress subscale scores compared with a non-clinical sample

B1, baseline 1; S6, end of therapy; 6M, 6-month follow-up; control sample: Smout et al. (Reference Smout, Davies, Burns and Christie2014), M=17.2, SD=6.44, n=630.
Figure 5 shows that baseline measurements (i.e. B1 to S1) for John’s VQ Obstruction scores ranged from 14 to 19, where cut-off scores of ≥16 are in the clinical range. These scores showed somewhat problematic levels of Obstruction (i.e. disruption of valued living due to avoidance of unwanted experience and distraction from values by inattention to values or attention to other psychological experiences) and are largely consistent with John’s pattern on responding on the CompACT (i.e. less well-developed mindfulness and acceptance processes). However, at S6, 3M and 6M, John’s scores reduced to the non-clinical range (i.e. 3, 1 and 0, respectively). Although John’s scores on the VQ Obstruction scale reduced from baseline to end of treatment (B1 – S6 = 16 points), it was slightly below the reliable change threshold (95% RCI for VQ Obstruction scale = 19).
Table 4 shows John’s VQ Obstruction scores in relation to a non-clinical sample. Whilst there was a large effect size differentiating John’s score above the control sample mean (Smout et al., Reference Smout, Davies, Burns and Christie2014) at B1, where John’s VQ Obstruction score of 19 was estimated to be at the 84th percentile, his scores at S6 and 6M showed favourable large effect sizes below the control group average. That is, he was at the 9th and 4th percentiles at S6 and 6M, respectively, showing that his VQ Obstruction score moved further away from the control average as time went on. This shows decreased disruption to valued living due to avoidance of unwanted experience or attention to other psychological experiences (Smout et al., Reference Smout, Davies, Burns and Christie2014).
Table 4. John’s Valuing Questionnaire Obstruction subscale scores compared with a non-clinical sample

B1, baseline 1; S6, end of therapy; 6M, 6-month follow-up; control sample: Smout et al. (Reference Smout, Davies, Burns and Christie2014), M=12.1, SD=6.88, n=630.
Discussion
In the present case study, ACT appeared to be an efficacious treatment for post-stroke adjustment difficulties in a working-age male, even when delivered via telerehabilitation. Here, following treatment John no longer met the clinical cut-offs for psychological distress and depression, which was maintained at 3- and 6-month follow-ups. Additionally, John’s psychological flexibility also improved following treatment and remained well developed at follow-ups.
Specifically, the work on values and committed action appeared to be particularly helpful for John. Whilst sessions 1–3 generally focused on mindfulness and acceptance work, sessions 4–6 focused more on behavioural aspects. Indeed, the initial assessment and formulation showed that John had a generally clear idea of his values but appeared to be struggling to live consistently with them, whilst managing the symptoms caused by his stroke. This dissonance was a source of distress for John. By engaging in ACT, alongside his stroke recovery and rehabilitation, John was able to develop skills in becoming more aware of the cognitive factors that may have been holding him back (e.g. the ‘Not Able To’ story) and distance himself from them whilst engaging in value-based actions. This finding is supported by MacQueen and Fisher (Reference MacQueen and Fisher2019) who suggested that ACT may be particularly helpful for men following neurological injury due to the potential consequences of associated changes on masculine identity in the domains of, for example, family role and occupational status. Here, ACT was proposed as being helpful for encouraging flexibility around such roles/narratives through exploration of values. Indeed, this appeared to be helpful for John.
A key strength of the present case study is the delivery of ACT via telerehabilitation. Existing evidence highlights the benefits of telerehabilitation in addressing barriers to accessing rehabilitation, including geographical isolation, limitations in time/resource, and compliance with rehabilitation (Appleby et al., Reference Appleby, Gill, Hayes, Walker, Walsh and Kumar2019). For John, some barriers to accessing in-person rehabilitation were infection control during COVID-19 lockdown and being unable to drive due to his stroke. Delivering his treatment via telerehabilitation enabled him to receive support throughout lockdown without disruption, and without having to arrange alternative transport for hospital visits. However, it is worth noting that some stroke survivors may experience barriers that impact on their ability to engage in telerehabilitation, including cognitive and language impairment, digital literacy, and access to equipment and connectivity (Tyagi et al., Reference Tyagi, Lim, Ho, Koh, Cai, Koh and Legido-Quigley2018).
Additionally, the case study adopted a single-case design involving baseline, post-intervention, and follow-up assessments. In line with recommended standards (i.e. Tate et al., Reference Tate, McDonald, Perdices, Togher, Schultz and Savage2008), the present case study measured more than 3 points at baseline across multiple outcomes (i.e. distress, psychological flexibility and engagement with values) to ensure greater reliability in baseline measurement. The case study has also used inferential statistics to determine the degree of change relative to large samples of non-clinical participants.
In terms of limitations, one of the potential difficulties with the statistical methods used to compare John’s scores to their respective samples and calculate reliable and clinically significant change scores is that they assume the CORE-10, CompACT and VA scores in the samples used are normally distributed. Unfortunately, none of the papers used to take normative sample data cite skewness or kurtosis values. To overcome this, we sought sample sizes of a least 50 or more (Crawford and Howell, Reference Crawford and Howell1998). However, even in very large non-clinical samples, the distribution of scores on common mood questionnaires can still be positively skewed (Crawford et al., Reference Crawford, Henry, Crombie and Taylor2001). We therefore suggest cautions in interpreting these values. Notwithstanding this, visual inspection of Figs 3, 4 and 5 show clear changes in the direction of improvement.
A further limitation is the narrow range of outcome measures used which focused on distress and ACT processes. Further work could consider the impact of ACT on a wider range of outcomes related to adjustment difficulties such as fatigue, confidence, quality of life, activities of daily living and illness perceptions.
Furthermore, whilst there are clear limitations on the generalisability of findings from single case studies, being in his early-40s, John experienced his stroke at a younger age than the national average for males in England (i.e. 68 years; Public Health England, 2018). He also experienced relatively mild cognitive and physical symptoms, retaining sufficient cognitive and language skills to engage in telerehabilitation. These factors are likely to have contributed to a more favourable prognosis, compared with someone experiencing greater cognitive and/or language impairments who may not be able to engage in telerehabilitation. Indeed, John exhibited several of the factors that have been found to be associated with post-traumatic growth after acquired brain injury such as his age (i.e. being in the ‘mid stages’ of life), being employed and being in a relationship (Grace et al., Reference Grace, Kinsella, Muldoon and Fortune2015). Conversely, John did not experience any significant difficulties which have been shown to be predictors of increased post-stroke distress including communication, cognitive or physical difficulties and a serious history of mental health difficulties prior to his stroke (Ayerbe et al., Reference Ayerbe, Ayis, Wolfe and Rudd2013; Mitchell et al., Reference Mitchell, Sheth, Gill, Yadegarfar, Stubbs, Yadegarfar and Meader2017; Thomas and Lincoln, Reference Thomas and Lincoln2006, Reference Thomas and Lincoln2008).
Although further research exploring psychological therapies such as ACT after stroke are warranted, we also encourage development of a process-based therapy approach to further research (Hayes and Hofmann, Reference Hayes and Hofmann2018; Hayes et al., Reference Hayes, Hofmann and Ciarrochi2020; Hofmann and Hayes, Reference Hofmann and Hayes2019). Here, key mediators and moderators of psychological functioning are incorporated into testable formulations of psychological phenomena as opposed to comparing one type of existing therapy against another (i.e. ACT vs cognitive behaviour therapy). This is with the aim of disentangling which specific processes targeted by different therapies may be useful for the various respective psychological challenges after stroke. Indeed, whilst distress was assessed via the CORE-10 in this study, we were equally interested in the impact of an ACT intervention on the processes of psychological flexibility (e.g. acceptance/mindfulness and values/committed action) that were being directly targeted by the intervention. To this end, it appeared that these processes did improve over the course of the six months John was assessed. Further exploration is needed to examine the types of psychological processes that are likely to facilitate adjustment after stroke and build these into models of adjustment (e.g. Gracey et al., Reference Gracey, Evans and Malley2009) which can be empirically tested and directly promoted through psychological therapy.
Key practice points
-
(1) ACT appeared to be an efficacious treatment for post-stroke adjustment difficulties in a working-aged man, even when delivered via telerehabilitation.
-
(2) Six sessions of ACT resulted in a reduction in psychological distress and depression, and greater psychological flexibility even at 6 months following treatment.
-
(3) By engaging in ACT, John developed skills in noticing and managing difficult thoughts and feelings that were acting as barriers to value-based actions.
-
(4) At 6-month follow-up, John had returned to work (40 hours per week) and reported that things were going ‘in the right direction’ for him.
Data availability statement
Data are available on request due to privacy/ethical restrictions.
Acknowledgements
A very special thanks to John for his immense patience and generosity in supporting our study throughout his recovery, and for permission to publish his treatment journey.
Author contributions
Jinnie Ooi: Conceptualization (equal), Data curation (equal), Formal analysis (equal), Funding acquisition (equal), Investigation (equal), Methodology (equal), Project administration (equal), Visualization (equal), Writing – original draft (equal), Writing – review & editing (equal); Tom Steverson: Conceptualization (equal), Formal analysis (equal), Methodology (equal), Supervision (equal), Writing – review & editing (supporting).
Financial support
This research was completed as part of J.O.’s Doctorate in Clinical Psychology (ClinPsyD) training. It did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
The authors declare none.
Ethical standard
All authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS. The service user described in this case study has seen this submission in full and agreed to it going forward in publication. The therapy was provided as part of routine care at an Early Supported Discharge service in the East of England. Written informed consent was gained from John for the publication of this case study, who has read the manuscript and agreed that the details were sufficiently anonymised.












Comments
No Comments have been published for this article.