For many young people with depression their subsequent adult life is punctuated by recurrent episodes of depression and poor psychosocial functioning (Reference Harrington, Dubicka and GoodyerHarrington & Dubicka, 2001). Recurrence rates are estimated to be 60–70% (Reference Birmaher, Ryan and WilliamsonBirmaher et al, 1996). It is unclear which factors exert the most potent influence on the course of the illness. Methodological differences may partly explain this: some studies have not conducted diagnostic interviews in person at baseline and follow-up, most did not collect data continuously throughout the follow-up period, and impairment criteria may or may not have been implemented. To our knowledge, the longitudinal, catch-up study reported here is the first in the UK to carry out full diagnostic interviews, face-to-face, at baseline and follow-up, to apply strict criteria for impairment at both time points and record follow-up data continuously from baseline. Outcome is examined in terms of recovery from the index episode of depression and first recurrence in clinically referred and community populations.
METHOD
Sample
A sample of 193 young people aged 8–17 years was available for follow-up: 120 clinically referred, 35 from the community and 38 controls. All had participated in previous studies by our group in the 1990s. The control group was retained in this study to examine whether risk for recurrence might be influenced by periodicity effects (i.e. that there are unique features associated with adolescents ascertained in the 1990s).
Clinic and control groups
The clinic group comprised patients aged 8–16 years attending two child and adolescent mental health clinics in the Cambridge area: 92 were recruited in 1991–2 and 28 in 1995–6. The 38 well controls (no psychiatric disorder), from the same geographical area, were recruited through general practitioners in 1991–2 and were matched for age and gender to every third patient with depression. Participants were interviewed at study entry and 36 weeks later. For this study, information from these assessments, together with details from clinical notes, was pooled to designate the ‘index’ episode.
Community group
The 35 community participants, aged 12–17 years, were recruited from Cambridge-shire schools to participate in a large community depression study in 1994–5. All were illness-free at entry. After 1 year a proportion of these young people were either depressed or had been depressed in the interim: these provided the sample for follow-up.
Measures
Psychopathology
Baseline assessment. Original diagnoses were assigned according to DSM–III–R (American Psychiatric Association, 1987), using the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K–SADS) Present state (Reference Chambers, Puig-Antich and HirschChambers et al, 1985; Reference Kolvin, Barrett and BhateKolvin et al, 1991) for clinic patients and the K–SADS Present and Lifetime version (Reference Kaufman, Birmaher and BrentKaufman et al, 1997) for those from the community.
Follow-up assessment. Current and lifetime diagnoses were generated using the Structured Clinical Interview for DSM–IV Axis I Disorders (SCID–I; American Psychiatric Association, 1994), Patient Edition (Reference First, Spitzer and GibbonFirst et al, 1997). We screened for antisocial and borderline personality disorders using an adapted screen from the Structured Clinical Interview for DSM–IV Axis II Disorders (SCID–II; Reference Spitzer, Williams and GibbonSpitzer et al, 1990). Positive responses were followed up using the relevant section of the SCID–II interview.
Note ondiagnosis. At baseline, a proportion of people in the clinic group had experienced an episode of major depressive disorder within an episode of dysthymia (double depression). It was impossible to distinguish accurately the onset and offset of major depression within the dysthymic episode. Therefore, index episodes of depression are rated from onset to offset of significant depressive symptoms, with no attempt to delineate full major depressive disorder from dysthymia.
Self-reports
Baseline assessment. All participants completed the Mood and Feelings Questionnaire (MFQ; Reference Costello and AngoldCostello & Angold, 1988; Reference Wood, Kroll and MooreWood et al, 1995). This 33-item questionnaire covers the symptom areas specified in DSM–IV for major depressive disorder. Test–retest reliability (4 weeks) is highly satisfactory (r=0.85).
Follow-up assessment. Current level of depressed mood in adulthood was assessed using the Beck Depression Inventory (BDI; Reference Beck, Ward and MendelsonBeck et al, 1961).
Puberty
Baseline assessment. Participants in the clinic group were shown gender-appropriate sketches relating to the five standard Tanner stages of pubertal development (Reference TannerTanner, 1962) and asked to select which looked ‘most like them’. Participants were grouped as pre-/early puberty (Tanner stages I and II) or mid/late puberty (Tanner stages III–V). The stage of puberty was not assessed in the community group.
Timeline
Follow-up assessment. The use of a timeline proved invaluable in orienting participants to the lengthy follow-up period. A timeline was drawn from the date of the last interview to the current interview. Interviewee and interviewer chronologically mapped significant life events on the timeline, for example school leaving, examinations, relationships, losses, followed by episodes of illness, good health, treatment and medication.
Data collection
Tracing procedure
Recorded deaths since baseline were checked using the ‘list-cleaning’ service provided by the Office for National Statistics. Participants were contacted by letter through their family of origin or through their general practitioner by way of their strategic health authority.
Follow-up interview
Participants were interviewed as soon after their 22nd birthday as possible. The eldest were approached first, from July 2000. Follow-up interviewing lasted for 31 months. Follow-up time was calculated from the date of each participant's last baseline interview (in adolescence) to the date of their follow-up interview (as young adults). Interviews were conducted by four trained research staff, masked to baseline diagnoses and ascertainment group. Diagnoses were reached by consensus with a clinician (I.G.). Reliability was acceptable (κ > 0.8). Participants gave written consent to both the interview and access to clinical notes. Participants were seen either at home or at the Developmental Psychiatry Section in Cambridge. A small remuneration was offered. The study received the full approval of the local and regional ethics committees.
Statistical procedures
Analysis was carried out using the Statistical Package for the Social Sciences, version 10.0 for Windows. Mann–Whitney U-tests were used on non-parametric data and t-tests on parametric data. Time to full remission (defined as a minimum of 2 months free of depressive symptoms and functional impairment) of the index episode of depression and time from full remission to first depressive recurrence (defined as a new depressive episode following a period of full remission) were examined using Kaplan–Meier survival analysis. (This method takes into account the assessment periods of people for whom the event of interest has not occurred by the end-point of the study, defining them as ‘censored’. Here, these are participants whose index episode of depression had not fully remitted and those who had not experienced a depressive recurrence by the time of their follow-up interview.) As those interviewed were unable to reliably pinpoint onsets and offsets accurately, times were recorded and entered to the nearest 0.25 of a year. Survival curves were compared using the log-rank test. In the clinic group, Cox regression was used to examine baseline factors thought to influence time to full remission and time to first depressive recurrence.
RESULTS
Non-participants
Clinic patients proved significantly more difficult to follow up than young people from the community or controls (55% v. 71% and 79% respectively: χ2=8.47, d.f.=2, P=0.014). Participants and nonparticipants were compared on a number of baseline variables. Significant differences were found only within the clinic group: non-participants were significantly younger at the onset of their index episode of depression (mean 12.1 years v. 13.5 years, z=72.72, P=0.006), more likely to have been pre-pubertal or in the early stages of puberty (v. mid to late puberty) (28 (61%) v. 26 (35%), χ2=7.59, d.f.=1, P=0.006), have less psychiatric illness among first-degree relatives (27 (56%) v. 23 (36%), χ2=4.58, d.f.=1, P=0.032) and have parents who had completed their education by age 16 years: mothers 37 (64%) v. 15 (27%), χ2=15.16, d.f.=1, P<0.001; fathers 29 (63%) v. 22 (36%), χ2=7.65, d.f.=1, P=0.006.
Success of tracing, sample response and exclusions
Table 1 compares participation according to ascertainment group. Of the original 193 participants, 191 were traced (99%). Of these, 121 (63%) were interviewed, 29 (15%) refused, 38 (20%) did not respond and 3 (2%) were out of the UK. Of the 121 interviewed, 8 were subsequently excluded: 1 for medical reasons and 7 because their index episodes were nonaffective.
Table 1 Participation according to baseline ascertainment group
| Clinic group (n=120) n (%) | Community group (n=35) n (%) | Control group (n=38) n (%) | |
|---|---|---|---|
| Participants | 66 (55) | 25 (71) | 30 (79) |
| Exclusions | 8 | 0 | 0 |
| Non-participants | 54 (45) | 10 (29) | 8 (21) |
| Refused | 23 | 4 | 2 |
| No response | 27 | 6 | 5 |
| Travelling | 2 | — | 1 |
| No trace | 2 | — | — |
| Final sample | 58 | 25 | 30 |
Final sample
Data reported here are based on 113 participants: 58 clinic and 25 community participants all with depression (major depression, minor depression or dysthymia) in childhood or adolescence, and 30 depression-free controls. Mean follow-up times differed significantly between groups: 8.1 years (s.d.=1.3), 5.8 years (s.d.=0.6) and 9.2 years (s.d.=0.81) for clinic, community and control groups respectively (Kruskal–Wallis χ2=59.86, d.f.=2, P<0.001). Univariate comparisons (Mann–Whitney) showed differences were significant between all three groups (clinic v. controls z=3.78, P<0.001; clinic v. community z=6.43, P<0.001; community v. controls z=76.34, P<0.001).
Mean age at follow-up interview was 23 years (s.d.=1.66), 22 years (s.d.=0.79) and 23.5 years (s.d.=1.6) for the clinic, community and control groups respectively (clinic v. community t=2.88, P=0.005; community v. controls t=4.07, P<0.001).
Baseline characteristics
Table 2 gives the characteristics of the sample at baseline. Compared with the community group, participants in the clinic group were more severely impaired, had higher rates of attempted suicide and self-harm, more psychotic symptoms, were significantly younger at onset of depression, received more treatment and medication and had significantly more psychiatric illness among first-degree relatives. Self-report depression scores were no different between the clinic and the community groups; both were significantly higher than controls.
Table 2 Characteristics of groups at baseline
| Variable | Clinic group (n=58) | Community group (n=25) | Control group (n=30) | Significance |
|---|---|---|---|---|
| Gender, n (%) | ||||
| Male | 19 (33) | 6 (24) | 15 (50) | |
| Female | 39 (67) | 19 (76) | 15 (50) | NS |
| Age, years; mean (s.d.) | ||||
| Age at entry into study | 14 (1.6) | 14 (1) | 13.8 (2.3) | NS |
| Age at index depression (n=82) | 13.5 (1.7) | 15.4 (1.2) | z=-4.5, P<0.0011 | |
| Age at first episode (n=82) | 11.6 (3.6) | 14.8 (2.3) | z=-4.7, P<0.0011 | |
| Any depression (no comorbidity) n (%) | 16 (28) | 12 (48) | 0 (0) | |
| Depression with comorbidity, n (%) | 42 (72) | 13 (52) | 0 (0) | |
| Anxiety disorder | 18 | 5 | ||
| Eating disorder | 4 | 4 | ||
| Behavioural disorder2 | 9 | 2 | ||
| Multiple comorbidity | 11 | 2 | ||
| Psychotic symptoms, n (%) | 6 (10) | 0 | 0 | |
| Serous suicide attempt (n=81), n (%) | 16 (28) | 0 | 0 | P=0.0023 |
| Self-harm (n=78), n (%) | 19 (35) | 1 (4) | 0 | P=0.0043 |
| MFQ score: mean (s.d.) | 36.1 (14.8) | 35.1 (6.7)6 | 11.7 (7.2) | z=-6.4, P≤0.0014 |
| z=-4.9, P<0.0015 | ||||
| GAF score (n=72), n (%) | ||||
| 60-51 moderate impairment | 15 (20) | 25 (100) | P<0.0013 | |
| ≤50 serious/severe impairment | 43 (80) | 0 | ||
| Puberty stage at onset (n=65), n (%) | ||||
| Pre/early | 12 (21) | |||
| Mid/late | 46 (79) | |||
| Treatment sought (n=82), n (%) | 58 (100) | 4 (17) | 0 | P<0.0013 |
| Medication prescribed (n=81), n (%) | 26 (46) | 0 | 0 | P<0.0013 |
| Regular substance use (sub-threshold for misuse), n (%) | 7 (12) | 3 (12) | NS3 | |
| Family psychiatric history (in first-degree relatives) (n=107), n (%) | 42 (78) (n=54) | 11 (46) (n=24) | 13 (45) (n=29) | χ2=11.96, d.f.=2, P=0.003 |
Subsequent disorder
Figure 1 compares subsequent psychiatric illness in the ascertainment groups. By the time of their follow-up interview 24 of 30 controls (80%) had remained illness-free compared with 16 of 58 clinic patients (28%) (Fisher's exact test P=0.001) and 10 of 25 young people from the community (40%) (Fisher's exact test P=0.005). As the focus of this report is depression we do not report on those who had exclusively non-affective illness.
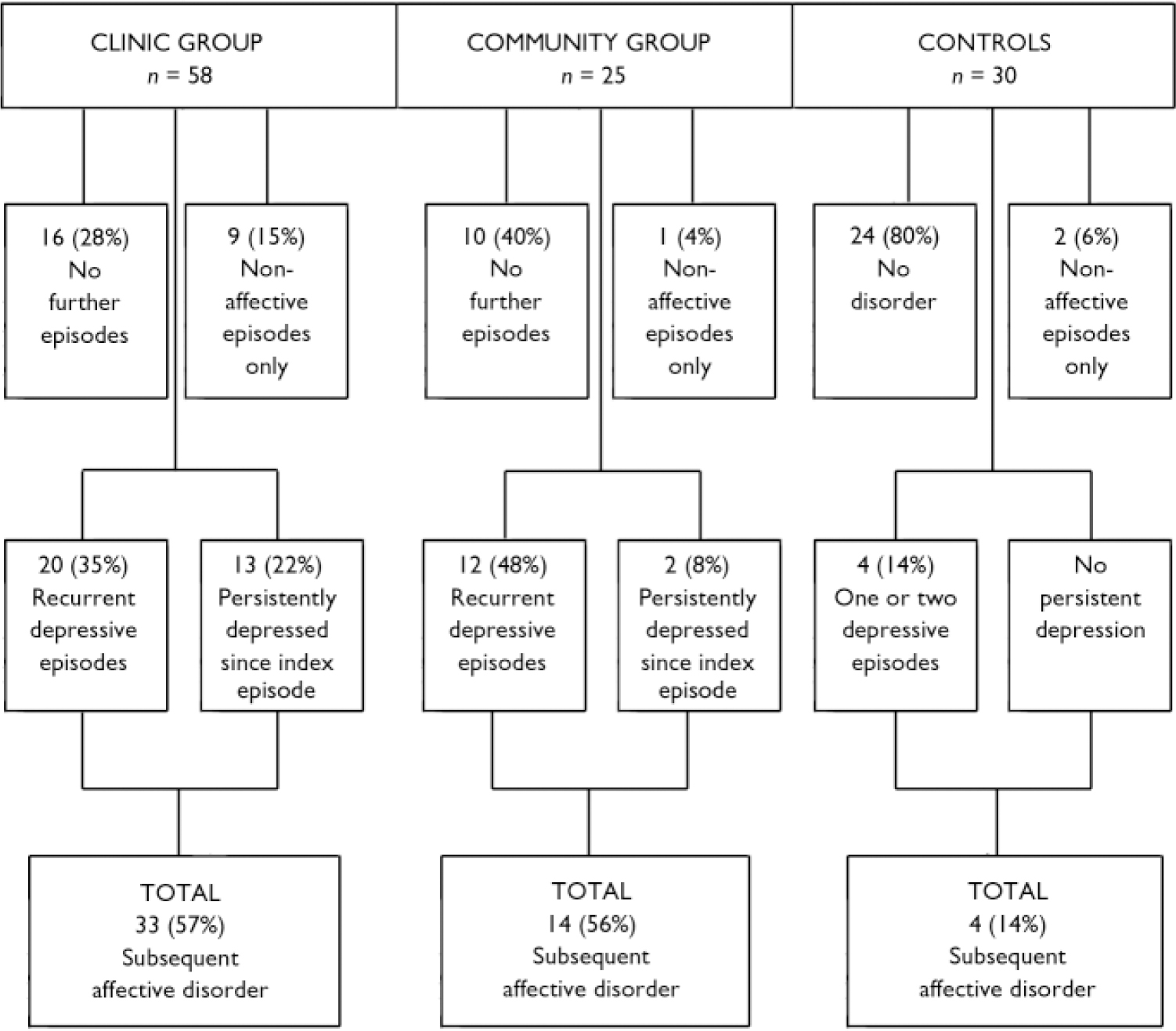
Fig. 1 Subsequent psychiatric illness in study sample throughout follow-up period.
Recurrent episodes of depression (one to three further episodes) were experienced by 20 people in the clinic group (35%) and 12 in the community group (48%), whereas 13 (22%) and 2 (8%) respectively had persistent depression since the index episode. Four people in the control group (14%) experienced first depressive episodes.
In the clinic group with subsequent affective disorder (33, consisting of 10 men and 23 women), men were more likely than women to be persistently depressed: 7 (70%) v. 6 (26%); whereas women were more likely to have recurrent episodes, 17 (74%) v. 3 (30%): (Fisher's exact test P=0.026).
No completed suicide was recorded during the follow-up period. There was a trend for more suicidal ideation and attempts in the intervening years among the clinic group (19 of 58; 33%) compared with the community group (3 of 25; 12%); Fisher's exact test P=0.06. In the control group, one person experienced suicidal ideation but there was no suicide attempt.
Index depression
The index episode of depression fully remitted in 45 clinic patients (78%) and 23 from the community (92%). Kaplan–Meier survival analysis was carried out to examine predictors of time to full remission. The 13 clinic patients (22%) and the 2 from the community (8%) in whom the index episode did not remit are censored in the analysis. (‘Full remission’ refers to depression; comorbid symptoms might have persisted.)
Figure 2 compares the cumulative survival times to full remission. The median time to full remission in clinic patients was 2 years (95% CI 0.83–3.17) v. 3 months in the community. By 3 months after onset, remission had occurred in 3 clinic patients (5%) compared with 17 (68%) in the community. By the end of the first year numbers in remission were 16 (28%) and 22 (88%) and by 2 years 29 (50%) and 23 (92%) for clinic and community groups respectively. Remission rates were clearly different (log-rank test χ2=25.1, d.f.=1, P<0.001) and so further analysis was made of the two groups separately.
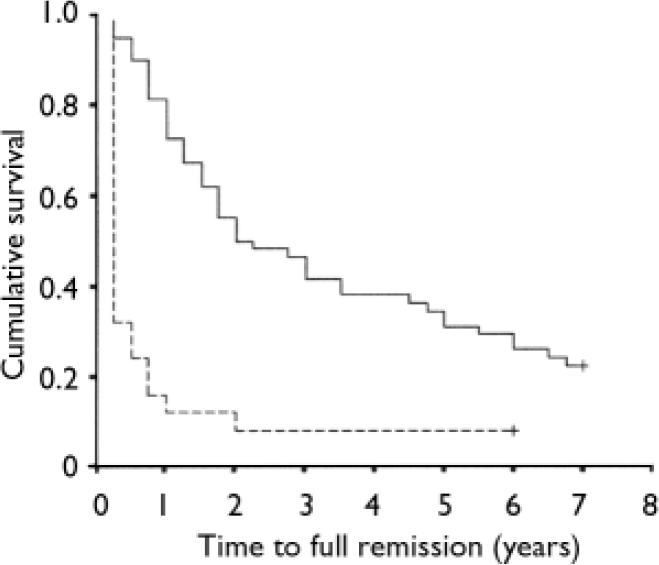
Fig. 2 Time to full remission of index depression: comparison of clinic group (![]() , n=58, 45 remitted (78%), 13 (22%) censored/unremitted at 7–13.7 years) and the community group (-------, n=25, 23 remitted (92%), 2 (8%) censored/unremitted, both at 6 years).
, n=58, 45 remitted (78%), 13 (22%) censored/unremitted at 7–13.7 years) and the community group (-------, n=25, 23 remitted (92%), 2 (8%) censored/unremitted, both at 6 years).
Cox regression (clinic patients only)
Eight baseline variables were entered into a Cox regression (backwards linear regression): gender, pubertal stage at onset, MFQ score, age at onset of index episode of depression, age at first psychiatric episode, comorbidity at index episode, severity of impairment at index episode and number of months with depression before starting treatment. The best-fit model incorporated three variables. The longest times to remission were found in those most severely impaired at index (hazard ratio (HR)= 3.27, 95% CI 1.6–6.65, Wald=10.62, d.f.=1, P=0.001), those who were depressed for longer (months) before starting treatment (HR=0.95, 95% CI 0.92–0.99, Wald=5.51, d.f.=1, P=0.019) and those with early psychiatric episodes (HR=1.12, 95% CI 1–1.24, Wald=4, d.f.=1, P=0.046).
Owing to small numbers, missing data and skewed distribution, Cox regression analysis of the community sample was not possible.
First recurrence of depression
Clinic group
Survival analysis explored time from full remission to first recurrence of depression, necessarily including only those whose index episode of depression had remitted (n=45). Of these, 20 (44%) experienced at least one recurrence of depression. The 25 (56%) whose depression did not recur are censored in the analysis. Figure 3 shows the cumulative recurrence rate. The median time to first recurrence was 9.25 years (95% CI 8.64–9.86). By 1 year after remission only 1 (2%) had experienced recurrence, after 2 years 5 (11%), after 3 years 8 (18%), 4 years 9 (20%), 5 years 13 (29%) and 6 years 15 (34%). In 3 instances the person was well for 9 years before the depression recurred. Recurrence peaked at 9% in years 1–2 and 4–5.
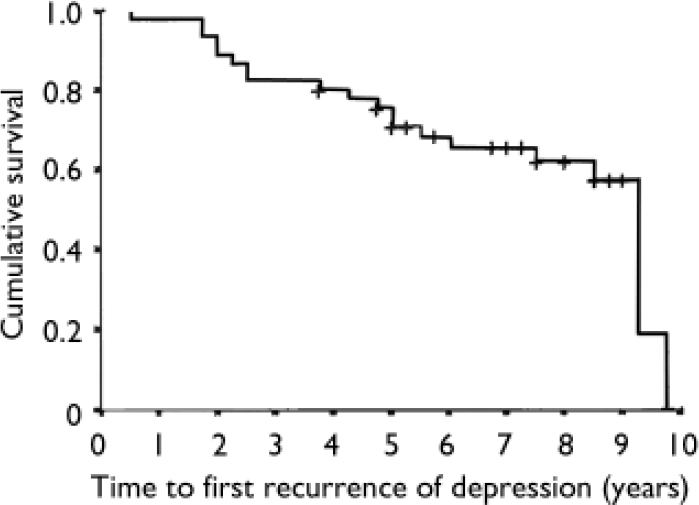
Fig. 3 Clinic group: time to first recurrence of depression from onset of full remission (n=45: 20 recurrences (44%), 25 (56%) censored (no recurrence); first censored observation (+)3.75 years, last 9 years).
The following baseline predictors of time to recurrence were entered in a Cox regression (backwards linear regression): gender, MFQ score, comorbidity, severity of impairment, pubertal stage and age at onset. The best-fit model was obtained with three variables: earlier recurrence was associated with being female (HR=5.4, 95% CI 1.12–25.73, Wald=4.42, d.f.=1, P=0.036), higher self-report depression scores (MFQ) at index episode (HR=1.04, 95% CI 0.999–1.1, Wald=3.73, d.f.=1, P=0.053) and comorbid symptoms at index episode (HR=3.3, 95% CI 0.952–11.3, Wald=3.54, 3.54, d.f.=1, P=0.06). There was no interaction. Mean duration of first recurrence was 45 weeks (s.d.=36.5) with a mean age at onset of 20 years (s.d.=1.8).
Community group
Small numbers made survival analysis impossible. Calculated in the standard way, mean time to first recurrence (n=12) was 3.4 years (s.d.=1.5). The mean duration of first recurrence was 44 weeks (s.d.=53.3) with a mean age at onset of 19.5 years (s.d.=2).
Controls
The mean age at onset of new episodes was 19 years, and the mean duration was 41 weeks (s.d.=42.2).
Group with persistent depression
The mean duration of depression, from onset in adolescence through to follow-up in young adult life, was 9.6 years (s.d.=2, range 7–13.8). The original diagnoses of the 15 people with non-remitted depression were 3 (20%) pure depression, 7 (47%) depression/anxiety, 5 (33%) multiple comorbidity. Most had complex diagnostic profiles with persistent depression remaining a core feature. One individual was subsequently diagnosed as having schizophrenia; one had bipolar affective disorder (also substance dependency); three people experienced other psychotic episodes (two also substance-dependent); three became dysthymic (one also substance-dependent); three had persistent anxiety symptoms (one also substance-dependent); and four had ‘pure’ persistent depression. Five participants (33%) had repeated in-patient stays during the follow-up period. Non-adherence to treatment (defined as a pattern of missed appointments, withdrawal from treatment, discharging self from hospital and refusing prescribed medication) was significantly higher in this group than among those with recurrent depression: 8 of 15 (53%) compared with 6 of 31 (19%; Fisher's exact test P=0.04).
There were significantly more suicide attempts and suicidal ideation among the group with persistent depression than among the recurrent depression group: 13 of 15 (87%) v. 6 of 32 (19%; Fisher's exact test P=0.001).
Substance and alcohol use
During follow-up
Recreational use or no use of substances and alcohol was reported by 36 (63%), 19 (76%) and 23 (77%) of the clinic, community and control groups respectively. However, many of these reported regular, high levels of recreational use. Commonly, cannabis, amphetamines and/or alcohol were used 2–3 times per week, with use increasing over time. However, little or no functional impairment was reported. Dependence was coded according to DSM–IV criteria. At least one episode of prolonged, daily (or near-daily for more than 6 months) substance or alcohol misuse was reported by 15 people in the clinic group (26%), 4 in the community group (16%) and 7 in the control group (23%) (NS). Prolonged polysubstance/alcohol misuse or dependence was absent in the control group but was reported by 6 (11%) of the clinic sample and 2 (8%) of the community sample (missing data on 1 clinic patient; n=57).
Current use
At follow-up, dependency rates in the clinic and community groups were 5 (9%) and 1 (4%) respectively: in the clinic group 2 persons were dependent on heroin, 2 on prescribed medication (with substantial overuse) and 1 on alcohol; the person from the community group was alcohol-dependent. All were depressed. There was no dependence among the controls. A further 3 clinic (5%), 1 community (4%) and 2 control (7%) participants reported current, daily cannabis use or alcohol use for at least 6 months, but only one of the clinic group met impairment criteria.
Current psychiatric status
Clinic group
At follow-up, 22 (38%) from the clinic group had a current diagnosis: 17 affective disorder (11 major depressive disorder, 4 dysthymia, 2 bipolar disorder); 1 schizophrenia (also with depression); 1 attention-deficit hyperactivity disorder; 3 probable personality disorders disorders (1 antisocial and 2 borderline; both with depression and 1 alcohol-dependent). In 17 instances (29%) the participant was receiving treatment (9 out-patient care, 1 counselling, 6 general practitioner care, 1 other) and 15 participants (26%) were taking psychotropic medication. The mean BDI score was 11 (s.d.=0.3, range 0–37).
Community group
Eight participants (32%) had a current diagnosis at follow-up interview: 6 affective disorder (4 major depressive disorder, 1 dysthymia, 1 bipolar disorder) and 2 anxiety disorder. In 3 instances (12%) the participant was currently receiving treatment (1 out-patient care, 2 general practitioner care) and were taking psychotropic medication. The mean BDI score was 8 (s.d.=5.6, range 0–19). Community participants were as likely as clinic patients to have a current diagnosis.
Controls
Three people in the control group (10%) were diagnosed with an affective disorder at follow-up interview: 1 bipolar disorder, 1 depression and 1 minor depression with comorbid eating disorder symptoms (eating disorder not otherwise specified). Both those with bipolar and major depression were receiving psychiatric treatment and psychotropic medication. The mean BDI score was 5 (s.d.=5.1, range 0–25).
DISCUSSION
Continued affective disorder was present in over half those with childhood/adolescent depression from both clinic and community groups. For a substantial proportion (40%) depression was recurrent with significant periods of remission. A small but significant subgroup (18%) of individuals remained persistently unwell into adulthood. In the clinic group, those whose index episode remitted took significantly longer to recover than those from the community. Females were more liable to recurrence, males to persistence.
Persistent depression
To our knowledge, previous studies have not identified a group whose adolescent depression continued, unabated, into young adulthood. This may be for methodological reasons. For example, Weissman et al (Reference Weissman, Wolk and Goldstein1999a , Reference Weissman, Wolk and Wickramaratne b ) left an arbitrary gap of 12 months between baseline and follow-up in an attempt not to confuse index and subsequent episodes. Similarly, others, whose primary focus was adult recurrence, recorded baseline data at around 13 years and follow-up data from 17 years (Reference Harrington, Fudge and RutterHarrington et al, 1990; Reference Fombonne, Wostear and CooperFombonne et al, 2001). This strategy runs the risk of misclassification, with persistent depression being incorrectly classified as recurrent. Our study overcame this by collecting data continuously from baseline throughout the follow-up period. The result is the identification of a small group (more males than females) with unremitting mental illness. These patients are characterised by more severe impairment than those described in previous studies, in which partial remissions occurred with ongoing residual symptoms (reviewed by Reference Birmaher, Arbelaez and BrentBirmaher et al, 2002).
For most of those with persistent depression (80%), the index episode of depression was accompanied by at least one comorbid disorder. Complex diagnostic profiles evolved, including high rates of psychotic illness (30%), dependence (30%) and suicidal thoughts or attempts (87%). In over half (53%), the patient regularly did not adhere to treatment. The Cox regression suggested that, as adolescents, these individuals had been depressed for long periods before starting treatment and had been severely impaired. Within the clinic group, first-onset depression may exert a more deleterious effect on males compared with females, but neither age nor pubertal status at first episode contributed to the outcome. These patients might benefit from early, long-term and more intensive clinical intervention than is currently given.
Remission and recurrence in the community group
The adolescents ascertained from the community on the whole achieved remission from their first depressive episode: 68% by 3 months and 92% by 3 years. This may be explained by less severe index episodes characterised by the absence of suicide attempts and psychotic features, a near-absence of self-harm and only moderate impairment. Despite this, almost half (48%) experienced recurrence of their depression, which is consistent with the 45% recurrence rate reported by Lewinsohn et al (Reference Lewinsohn, Rohde and Klein1999). First recurrences were similar in length to those experienced in the clinic group. The small size of this community group means that the results should be treated with caution. They suggest that the probability of recurrence is high despite the moderate nature of the original depressive episode. A small proportion of individuals from the community may suffer persistent depression, with no remission, into young adulthood. Young people in the community with depression, therefore, might benefit from early detection and robust intervention.
Remission and recurrence in the clinic group
Remission of the index episode of depression was slower among clinic patients: only 5% had achieved remission by 3 months, less than a third by 12 months and only half by 3 years. Median time to full remission was 2 years, with 13 (22%) having no remission by follow-up. This contrasts with previous studies which have reported rates of 92% remission by 18 months (Reference Kovacs, Feinberg and Crouse-NovakKovacs et al, 1984)–our 18-month figure was 38% – and 80% after 12 months (Reference McCauley, Myers and MitchellMcCauley et al, 1993). This may be a result, in part, of our not differentiating between dysthymia and major depressive disorder at the index assessment. Kovacs et al (Reference Kovacs, Feinberg and Crouse-Novak1984) reported a pattern in dysthymia that more closely resembles that reported here: a median duration of around 3 years, low annual remission rates and a maximal remission of 89% after 6 years.
Longer index episodes were associated with more severe impairment, being depressed for longer before starting treatment and having an early psychiatric episode. In those with higher self-report depression (MFQ) scores and comorbidity at index assessment the depression tended to recur sooner, and recurrence was earlier in females than in males. There was no effect of puberty or age. Confidence intervals were wide in our Cox regression, indicating a less-than-perfect fit which could be a result of the wide distribution of times to first recurrence (6 months to 9.75 years) and the small number of males (n=3) who experienced recurrence compared with females (n=17).
Females with depression were more likely to have a recurrent pattern of depressive disorder, whereas more males developed persistent mental illness. The non-participants in the follow-up constituted 45% of the original clinic group, were younger and had less psychiatric illness among first-degree relatives. Thus, the above findings should be treated cautiously.
Substance and alcohol use
The 9% dependency rate in the clinic group (all participants currently depressed and 3 with psychotic illness) was lower than the 29% reported by Fombonne et al (Reference Fombonne, Wostear and Cooper2001). This may be owing to our comparatively young follow-up age (mean 23 years), compared with a mean of 35 years in the Fombonne study. The high thresholds we set for diagnosis might have resulted in an underestimate.
Deaths during follow-up
Although 46% of those from the clinic group had either self-harmed or attempted suicide at the time of the index episode, there was no recorded suicide during the follow-up period. This is somewhat surprising as the strongest predictor of suicide is previous self-harm (Reference Safinofsky, Hawton and Van HeeringenSafinofsky, 2000; Reference Hawton, Zahl and WeatherallHawton et al, 2003). Other studies have reported moderate suicide rates. For example, Weissman et al (Reference Weissman, Wolk and Goldstein1999a ) reported a 7.7% suicide rate; Harrington et al (Reference Harrington, Fudge and Rutter1990) reported 4 deaths (3%), 3 of which were suicide; and Fombonne et al (Reference Fombonne, Wostear and Cooper2001) reported 8 deaths (3%), 6 of which were suicide. Our absence of suicides may be explained by our cohort being relatively young at follow-up: mean age 23 years, compared with means of 26 years, 31 years and 35 years respectively in the other studies.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Depression in the community requires early detection and psychiatric assessment.
-
▪ A significant proportion of young people with depression continue to be depressed into young adult life.
-
▪ Among clinically referred youngsters, course and outcome may differ between the genders, with males showing increased risk of persistence and females of recurrence.
LIMITATIONS
-
▪ The small sample size limits the power of statistical analysis.
-
▪ A significant proportion of the original group with pre-pubertal onset and younger clinic patients were lost to follow-up.
-
▪ The lengthy follow-up time may have resulted in selective recall or recall bias.
Acknowledgements
We thank Carole Lack, Gillian Barker and Cessie Johannsson for data collection; the staff at the Office for National Statistics; Sarah Vowler at the Centre for Applied Medical Statistics, University of Cambridge; and Alison Tamplin for advice. The study was funded by a grant from the Wellcome Trust.








eLetters
No eLetters have been published for this article.