Objectives
The objectives of this chapter are to:
Discuss the rationale for airway assessment.
Outline a pre-anaesthetic patient assessment.
Evaluate methods of airway assessment.
Identify patients who may be difficult to ventilate and/or intubate.
Identify patients that may require a different airway intervention.
Introduction
During elective anaesthesia a failed airway (‘cannot intubate, cannot oxygenate’) occurs in 0.01–0.03% of cases. Difficult intubation, defined as the need for more than three attempts, occurs in 1.15–3.8% of elective surgical cases, and is usually related to a poor view at laryngoscopy. However, the characteristics of patients requiring intubation or assisted ventilation outside the operating room are different to those undergoing elective surgical procedures, and the incidence of difficult intubation is significantly higher in emergency departments, as demonstrated by the Royal College of Anaesthetists’ Fourth National Audit Project (NAP4). More importantly, a failed airway may occur at least ten times more frequently in the emergency setting; in the United States, 0.5% of intubations recorded in the National Emergency Airway Registry (NEAR) required a surgical airway. In a recent Scottish study, 57/671 (8.5%) of patients undergoing rapid sequence induction in the emergency department had Cormack and Lehane grade 3 or 4 views at laryngoscopy (see below), and two (0.3%) required a surgical airway.
Given these data, difficulties with the airway must be expected in all emergency patients, and appropriate preparation undertaken. Some features may indicate a particularly high likelihood of airway difficulties, and in these cases modification of practice may reduce complications and improve outcome.
Definition of a difficult airway
A difficult airway is categorized by:
Difficult mask ventilation. Difficult mask ventilation occurs when the patient’s anatomy or injuries make it impossible to maintain adequate ventilation and oxygenation with a facemask and simple airway adjuncts alone.
Difficult intubation. Difficult intubation is defined when an experienced laryngoscopist, using direct laryngoscopy, requires:
1. more than two attempts with the same blade or;
2. a change in the blade or an adjunct to a direct laryngoscope (e.g. bougie) or;
3. use of an alternative device or technique following failed intubation with direct laryngoscopy.
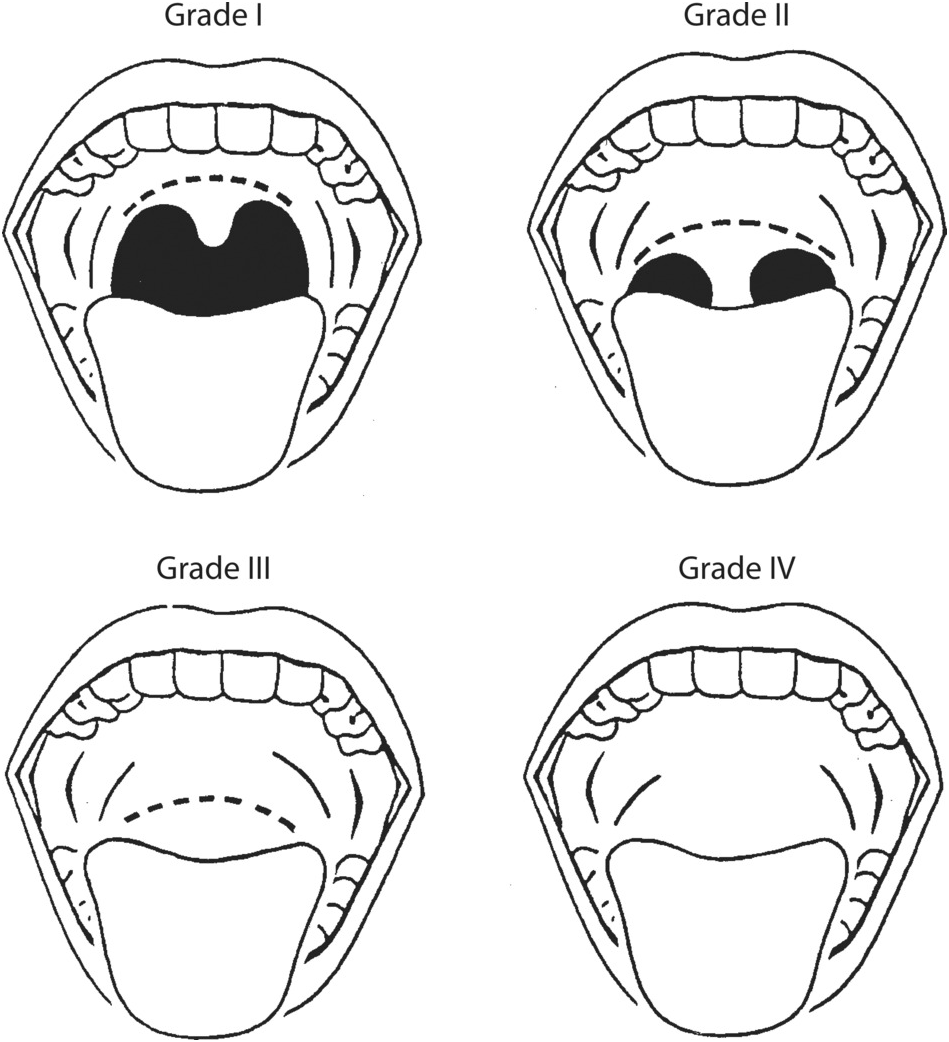
Difficult view at laryngoscopy. The view at direct laryngoscopy has been classified by Cormack and Lehane (Figure 5.1). A difficult view is defined as being unable to see any portion of the vocal cords with conventional laryngoscopy (Cormack and Lehane grades 3 and 4). These views are associated with more difficult or even impossible intubations under direct vision. Although this may not help at initial presentation, the grade of view at laryngoscopy must be recorded because it may influence the approach to future airway management by other healthcare professionals.
Grade 1 The vocal cords are visible
Grade 2 The vocals cords are only partly visible
Grade 3 Only the epiglottis is seen
Grade 4 The epiglottis cannot be seen
Difficult cricothyroidotomy. Failure to intubate the trachea combined with an inability to oxygenate the patient using a bag-mask or supraglottic airway device will necessitate a surgical airway. Occasionally, patient-specific features may render the cricothyroid membrane inaccessible. This makes induction of anaesthesia particularly risky because if the airway is lost it may be irretrievable, and oxygenating the patient will be impossible
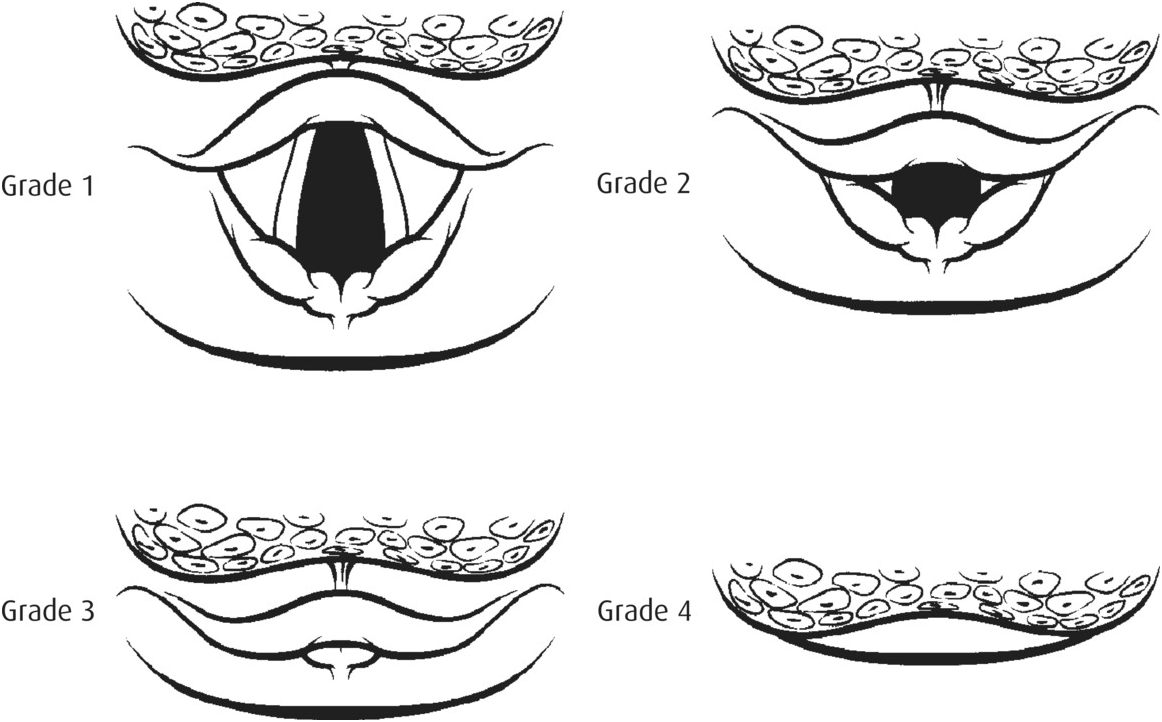
Figure 5.1 The Cormack and Lehane classification of laryngeal view.
General assessment of patients before inducing anaesthesia
Few patients require immediate induction of anaesthesia and intubation. Some time is usually available for a clinical assessment and, where possible, a comprehensive evaluation of the patient is required before inducing anaesthesia (see Table 5.1).
Table 5.1 Pre-anaesthetic assessment of emergency patients where time allows
Comprehensive history
Cardiorespiratory status
Conscious level
Focal/global neurological signs
Assessment of face and neck
Assessment for pneumothorax
Abdominal and pelvic assessment for surgical signs
Body morphology
When time allows, obtain a good history including current medication and allergies, previous medical and surgical problems, last oral intake, and details of the patient’s current condition. If available, previous medical records can be invaluable. Patients and relatives may have been informed about any serious problems, including airway difficulties, occurring during previous anaesthetics. A MedicAlert bracelet system has been advocated for patients with difficult airways, and may be carried by some.
Document clearly the pre-anaesthetic findings and communicate them to the team responsible for the patient’s continuing care.
Once a patient is anaesthetized some physical signs will be lost, e.g. abdominal guarding or abnormal neurology. Before inducing anaesthesia, pay attention to:
the Glasgow Coma Scale (GCS);
focal neurological signs;
evidence of pathology in the chest, abdomen or pelvis.
Positive pressure ventilation may convert a simple pneumothorax into a tension pneumothorax. Examine the patient and look for signs of a pneumothorax. Consider obtaining a chest x-ray before induction of anaesthesia in patients at particular risk, e.g. trauma, asthma and chronic obstructive pulmonary disease (COPD). A pneumothorax will sometimes require drainage before or immediately after induction of anaesthesia.
Most intravenous anaesthetics are cardiovascular depressants and these effects will be compounded by positive pressure ventilation. Concurrent rapid infusion of intravenous fluid, combined with a vasopressor if necessary, will reduce the risk of cardiovascular collapse during induction of anaesthesia.
Airway assessment
Predicting difficulty in bag-mask ventilation (BMV)
In elective anaesthesia profound difficulty in maintaining adequate BMV occurs in 1.4% of the population and is impossible in 0.16%. If intubation is difficult or impossible, ventilation with a bag-mask can maintain oxygenation until the airway is secured. Difficulty with facemask ventilation is a serious problem, and every effort should be made to anticipate this complication. The combination of difficult mask ventilation and difficult laryngoscopy occurs in 0.4% of the general anaesthesia population. In many cases, difficulty with facemask ventilation may be resolved by use of simple airway manoeuvres, adjuncts or a change in technique. If these fail, insertion of a supraglottic airway device may enable oxygenation and ventilation until a definitive airway is established.
Difficult facemask ventilation will occur if it is not possible to establish a good seal, if airway patency is difficult to maintain, if airway resistance is high, or if lung and chest wall compliance is poor. A study of patients undergoing elective surgery identified five criteria that were independent predictors of difficult mask ventilation: age > 55 years, body mass index > 26 kg m–2, beard, lack of teeth, and a history of snoring. Combinations of these factors significantly increase the likelihood of difficulties during BMV.
Features likely to cause difficulty in achieving a good seal with a facemask
a beard or moustache; this may be rectified by the application of petroleum jelly or aqueous lubricant, although the resulting slippery conditions may cause additional difficulty;
significant cachexia, missing molar teeth or missing dentures causing sunken cheeks; where possible, leave well-fitting dentures in place; when this is not feasible, pad the cheeks out with dressing gauze, but ensure that all gauze is subsequently removed to avoid inadvertent airway occlusion following later extubation;
facial trauma, particularly through and through cheek lacerations and unstable bony injuries.
Features likely to cause difficulty in maintaining an airway without intubation
a short jaw or inability to bring bottom incisors in front of top incisors (prognath);
immobilized neck;
unstable facial bony injuries;
upper airway obstruction, e.g. blood or vomit, retropharyngeal swelling such as haematoma or infection;
obesity;
macroglossia;
history of snoring.
Features likely to make it difficult to ventilate the lungs
abdominal distension/diaphragmatic splinting;
lower airways obstruction, e.g. asthma, pneumothorax;
obesity.
Predicting difficult intubation
Most tests used to predict difficult intubation have poor sensitivity and specificity, particularly in the emergency patient when it can be difficult to obtain a comprehensive evaluation. If a particular feature associated with difficult intubation is present, whilst more likely, it does not necessarily mean that the patient will be difficult to intubate. Likewise if a feature is absent it does not rule out the possibility of a difficult intubation.
Features that have some value in predicting difficult intubation include:
Previous history of a difficult airway
Look for a MedicAlert bracelet or similar. Ask about previous anaesthetic events and access patient medical records if available.
Body morphology
Facial features
Poor mouth opening – less than 4–5 cm or three finger breadths incisor to incisor (or gum to gum in edentulous patients) will reduce access and view of the larynx.
Prominent upper incisors will restrict view and access. Jagged teeth may puncture the cuff of a tracheal tube.
A high-arched palate reduces the space inside the mouth, compromising access during laryngoscopy.
Receding mandible (see thyromental distance below).
An inability to move the lower teeth in front of the upper teeth.
Macroglossia reduces space within the mouth and makes the tongue harder to move.
Facial trauma causing deranged facial anatomy. Bleeding into the soft tissues may distort the anatomy and normal colouration of the pharynx and larynx, making landmarks more difficult to identify. Fractures involving the temporomandibular joints may be particularly dangerous as they can prevent any mouth opening even after a neuromuscular blocker has been given. Paradoxically, unstable, and therefore mobile, facial bony injuries may facilitate laryngoscopy and subsequent intubation.
Neck
Thyromental distance < 6–7 cm, or four finger breadths, from the top of the thyroid cartilage to the anterior border of the mandible with the neck in full extension implies a short mandible and/or a high larynx; both may impair the view at laryngoscopy or make intubation very difficult.
Trauma – blunt trauma may rarely fracture the larynx, altering the anatomy and making it difficult to identify structures during laryngoscopy.
Penetrating trauma may cause haematomas that displace the larynx, making the view and access difficult, yet are not visible externally.
Infection causing either generalized swelling (e.g. pharyngitis, laryngitis, epiglottitis) or focal swelling (retropharyngeal abscess or quinsy) may cause obstruction.
Tumours, previous surgery or radiotherapy may all alter normal anatomy and reduce soft tissue mobility.
Reduced skeletal mobility will worsen the view of the larynx. The best views are obtained in adults with the head in extension and the neck in flexion. This is the ‘sniffing the morning air’ position, which aligns the airway axes and makes it easier to see the glottis (see Chapter 3). Reduced neck mobility may be present in presumed or actual cervical spine injury, the elderly, in patients with arthritis of the cervical spine, and in patients with previous neck injuries or surgery. During laryngoscopy with in-line stabilization of the neck and pressure applied to the cricoid cartilage the view of the glottis will be Cormack and Lehane grade 3 or 4 in 20% of cases. The use of videolaryngoscopy will reduce this incidence. In obese patients, women with large breasts or patients with severe fixed flexion neck deformities (e.g. ankylosing spondylitis), it may be difficult to get the laryngoscope blade into the mouth whilst mounted on the handle. In these cases the blade may have to be inserted separately or a specialist laryngoscope used (such as a polio blade or a fibre optic scope).
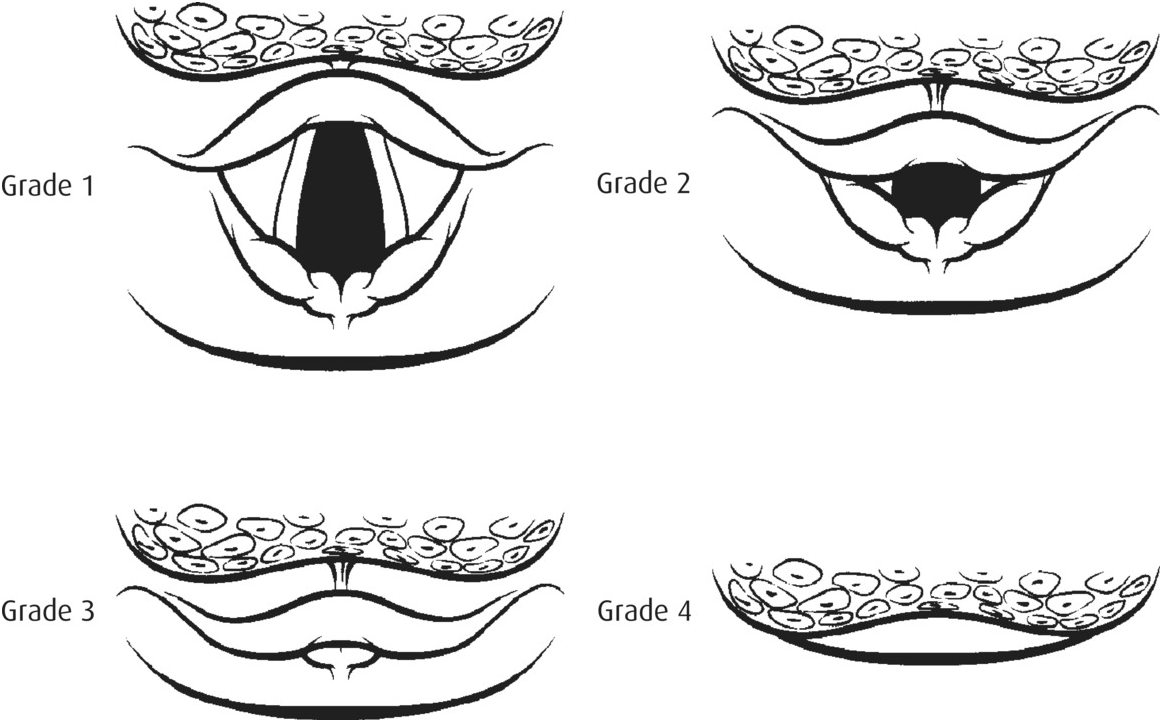
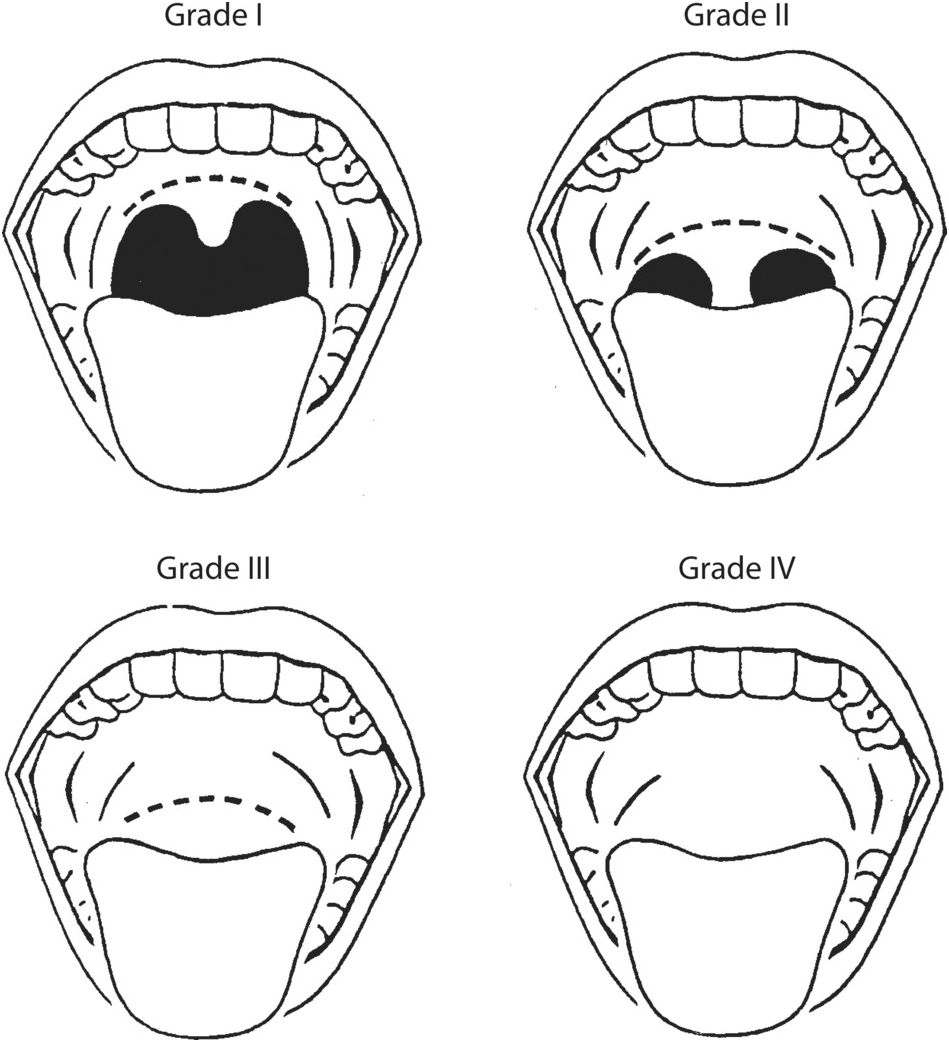
Mallampati and other scoring systems
A Mallampati score of I to IV is used to describe the view of the patient’s tongue, faucial pillars, uvula and posterior pharynx (Figure 5.2). Scores of III or above are associated with limited views at laryngoscopy. To be valid, the assessment is undertaken with the patient seated in front of the practitioner with the head extended on a flexed neck. The patient is asked to open their mouth wide and protrude their tongue.
Other scoring systems (for example, the Simplified Predictive Intubation Difficulty Score (SPIDS), and the Simplified Airway Risk Index (SARI)) have been advocated. These use a combination of features in an attempt to improve the sensitivity and specificity of predicting a difficult airway, but they have had limited success. SARI uses a score derived from seven risk factors (mouth opening, thyromental distance, Mallampati score, neck mobility, ability to prognath, weight and history of difficult intubation) and is currently being evaluated in the elective anaesthesia population in an attempt to validate this form of assessment for predicting difficulty with intubation and BMV.
All these scoring systems require time, a compliant patient able to mobilize, and often prior knowledge of the patient. None of this may be available when dealing with an emergency airway, and they therefore have a limited role in pre-intubation airway assessment in this context.
Predicting a difficult cricothyroidotomy
Performing a surgical or needle cricothyroidotomy is a rescue procedure that may enable oxygenation of a patient in a ‘can’t intubate, can’t oxygenate’ situation. These techniques rely on the cricothyroid membrane being accessible, which may not always be the case.
Features that may cause difficulty in accessing the cricothyroid membrane
Obesity. A layer of subcutaneous tissues makes the anatomical landmarks ill-defined and difficult to locate.
Neck immobility. Being unable to extend the head on the neck may restrict access, particularly in the obese or short-necked patient.
Local trauma. Significant blunt or penetrating trauma may distort the anatomy, as may burns over the anterior neck.
HAVNO
A simple reminder for assessing predictors of a difficult airway is:
H History – including previous airway problems.
A Anatomy – features of the face, mouth, and teeth that may suggest intubation will be difficult.
V Visual clues – trauma, obesity, facial hair, age.
N Neck mobility and accessibility, including the presence of in-line stabilization.
O Opening of the mouth – less than three fingers suggests potential difficulty with intubation.
What to do if a difficult airway is predicted
Airway management in an emergency is more difficult than in elective practice, so the emergency airway practitioner must always be prepared for difficulty, even if not predicted. By using the approach described above, a difficult airway can often be anticipated so that, time allowing, rapid sequence induction is not undertaken in the absence of the most experienced available assistance unless the patient has life-threatening hypoxaemia or is deteriorating despite all possible basic airway interventions. The management of difficult and failed airway is described in Chapter 9.
Summary
Always be prepared for a difficult airway.
No single airway assessment tool is sufficiently sensitive or specific to reliably predict a difficult or easy airway.
In some cases features of the patient’s morphology and pathology enable a difficult airway to be predicted.
Rarely, patients with no predictive features may be difficult or impossible to intubate using conventional techniques.
Intubation is rarely so urgent that airway assessment is not possible; aim to undertake a pre-anaesthetic assessment in all but the most unusual cases, and document the findings.