Book contents
- Frontmatter
- Contents
- List of contributors
- Preface
- Section 1 History and general issues
- Section 2 Cell biology and pathobiology
- Section 3 Evaluation and treatment
- 12 Pharmacokinetic, pharmacodynamic, and pharmacogenetic considerations
- 13 Acute lymphoblastic leukemia
- 14 Relapsed acute lymphoblastic leukemia
- 15 B-cell acute lymphoblastic leukemia and Burkitt lymphoma
- 16 Acute myeloid leukemia
- 17 Relapsed acute myeloid leukemia
- 18 Myelodysplastic syndrome
- 19 Chronic myeloproliferative disorders
- 20 Leukemias in patients with Down syndrome
- 21 Treatment of adolescents and young adults with acute lymphoblastic leukemia
- 22 Hematopoietic stem cell and natural killer cell transplantation
- 23 Treatment of acute leukemia in countries with limited resources
- 24 Antibody-targeted therapy
- 25 Adoptive cellular immunotherapy
- 26 Gene transfer: methods and applications
- 27 Development therapeutics
- 28 Minimal residual disease
- Section 4 Complications and supportive care
- Index
- Plate Section
- References
18 - Myelodysplastic syndrome
from Section 3 - Evaluation and treatment
Published online by Cambridge University Press: 05 April 2013
- Frontmatter
- Contents
- List of contributors
- Preface
- Section 1 History and general issues
- Section 2 Cell biology and pathobiology
- Section 3 Evaluation and treatment
- 12 Pharmacokinetic, pharmacodynamic, and pharmacogenetic considerations
- 13 Acute lymphoblastic leukemia
- 14 Relapsed acute lymphoblastic leukemia
- 15 B-cell acute lymphoblastic leukemia and Burkitt lymphoma
- 16 Acute myeloid leukemia
- 17 Relapsed acute myeloid leukemia
- 18 Myelodysplastic syndrome
- 19 Chronic myeloproliferative disorders
- 20 Leukemias in patients with Down syndrome
- 21 Treatment of adolescents and young adults with acute lymphoblastic leukemia
- 22 Hematopoietic stem cell and natural killer cell transplantation
- 23 Treatment of acute leukemia in countries with limited resources
- 24 Antibody-targeted therapy
- 25 Adoptive cellular immunotherapy
- 26 Gene transfer: methods and applications
- 27 Development therapeutics
- 28 Minimal residual disease
- Section 4 Complications and supportive care
- Index
- Plate Section
- References
Summary
- Type
- Chapter
- Information
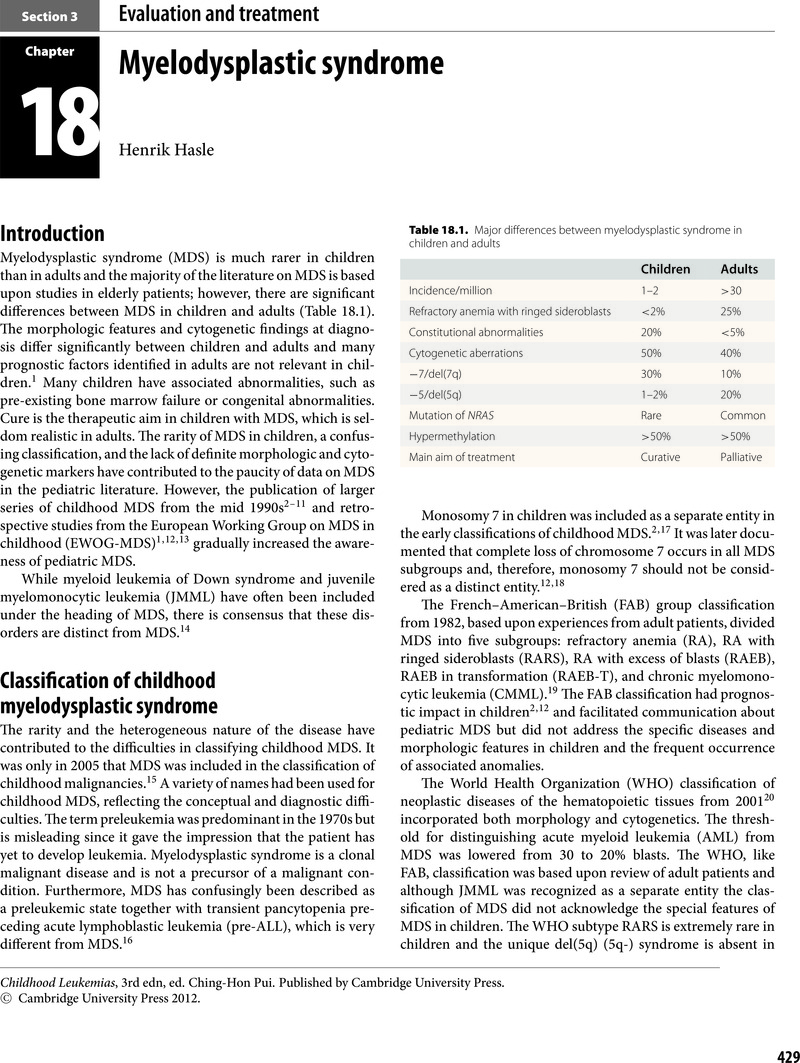
- Childhood Leukemias , pp. 429 - 443Publisher: Cambridge University PressPrint publication year: 2012



