Book contents
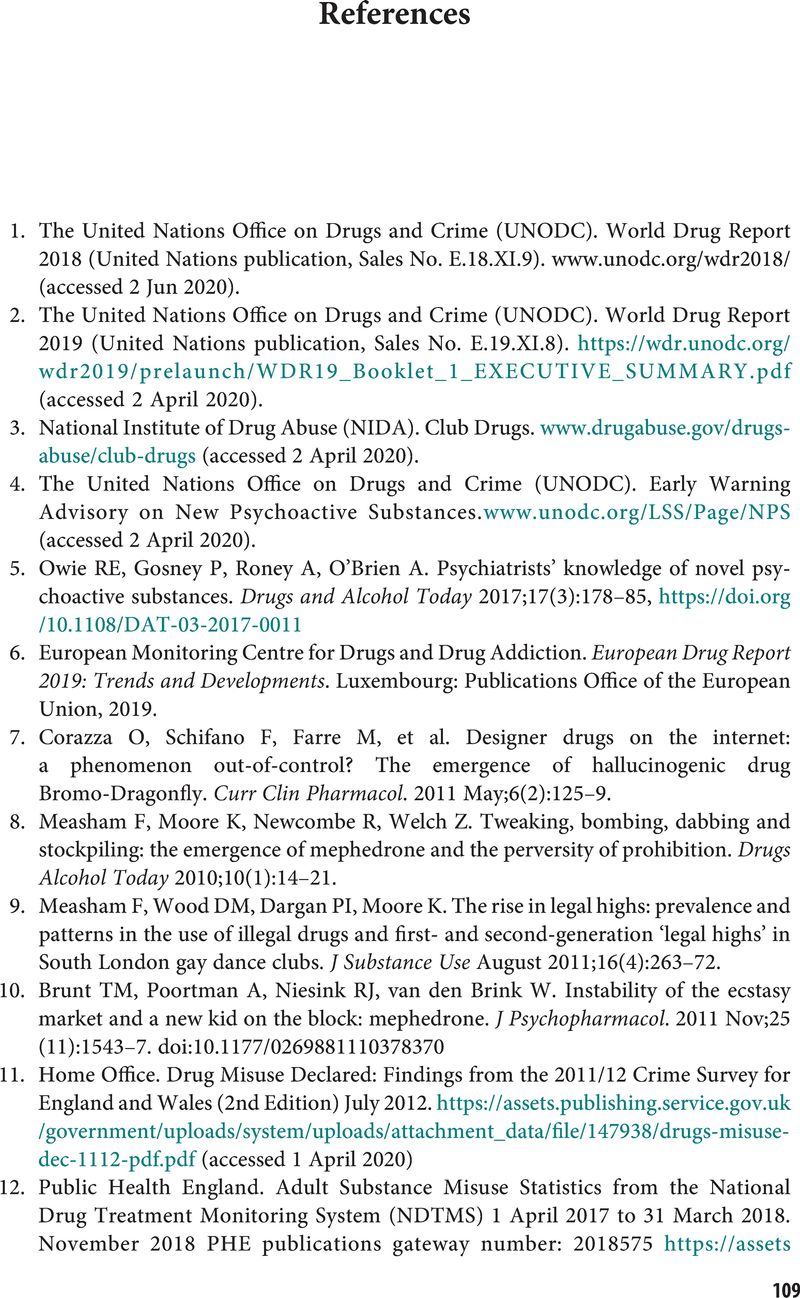
References
Published online by Cambridge University Press: 21 September 2020
Summary
- Type
- Chapter
- Information
- Club Drugs and Novel Psychoactive SubstancesThe Clinician's Handbook, pp. 109 - 123Publisher: Cambridge University PressPrint publication year: 2020