Introduction
In January 2001, the famous English sportsman Randolph Adolphus Turpin was elected into America’s International Boxing Hall of Fame. The celebration marked fifty years since he had defeated Sugar Ray Robinson to win the world middle-weight boxing title in 1951.1 Older fans of boxing appreciated that Turpin would not be present at the US inauguration. He had committed suicide aged just 38, in 1966. Few, however, knew that the fatal decision to end his life had caused considerable controversy in British medical circles. His boxer’s brain became the subject of professional debates and medical research disputes between a coroner, pathologist, senior neurologists and heart specialists, as well as his family and the popular press. In 1966, the tragic events were opened up to public enquiry and exposed medico-legal tensions about who owned a body and its parts in death. In neglected archives, forgotten medical stories like that of Turpin reveal narratives of the dead that often question the global picture of a medico-scientific consensus which argued that the accumulation, deidentification and retention of human material was necessary for ‘progress’. We rediscover, instead, faces, people, families and communities whose loved ones became the unacknowledged bedrock of modern British medical research. These missing persons relocated in the historical record exemplify that medical breakthroughs could have been part of an important and ongoing public engagement campaign in a biomedical age.
On Friday 22 July 1966, the lead sports writer of the Daily Mail featured the sad death of Turpin. The ex-boxer ‘shot himself with a .22 pistol in an attic bedroom over his wife’s Leamington Spa café on May 17’.2 The case looked like a straightforward suicide, but was to prove to be more complicated and controversial. Turpin died ‘after wounding his daughter, Carmen, aged two’ (although critically injured, she survived the violent attack by her father). At the Inquest, medical evidence established how: ‘Turpin fired at himself twice. The first bullet lodged against his skull but was not fatal. The second passed through his heart.’ The coroner, however, came in for considerable criticism in the press about his conclusions. It was noted that ‘Dr. H. Stephens Tibbits did not call for the brain tests that could have decided if brain damage caused by Turpin’s 24 years of boxing (including his amateur days) might have contributed to his state of mind on the day he died’. The pathologist who conducted the post-mortem on behalf of the Coronial hearing expressed the prevailing medical view that: ‘An examination by a neuropathologist using a fine microscope could have disclosed any tell-tale symptoms of brain damage such as a boxer might suffer.’ In particular, more medical research would have pinpointed ‘traces of haemorrhage in the tiny blood vessels of his brain’. But Dr Barrowcliff (pathologist) was not permitted to proceed because Dr Tibbits (coroner) would not authorise him to do so. The pathologist regretted that: ‘There was a certain amount of urgency involved here’ because of the fame of the suicide victim ‘to which academic interest took second place’. The press thus noted: that ‘the opportunity had been missed to carry out this study was received with dismay from a physician concerned with the Royal College of Physicians Committee on Boxing’. Its ‘eight leading specialists on the brain, heart and eyes’ were very disappointed that the pursuit of medical research that was in the public interest had been overridden by a coroner’s exclusive powers over the dead. The family meanwhile were relieved to have been consulted at all, since it was not a legal requirement at the time. They were anxious that the Coronial hearing should take into account Turpin’s suicide note. His last words, in fact, revealed disagreement between medical personnel, the family and suicide victim about the cause of death and therefore the potential of his brain for further research. To engage with this sort of hidden history of the dead and its body parts dispute, which is normally neglected in the literature, we need to trace this human story in greater archival depth.
Thus, Turpin left a handwritten note which stated that the Inland Revenue were chasing him for a large unpaid tax bill. He claimed this was levied on money he had not actually earned, and this was the chief cause of his death – ‘Naturally they will say the balance of my mind was disturbed but it is not’, he wrote; ‘I have had to carry the can.’3 Money troubles since his retirement from boxing in 1958 certainly seemed to have mounted. Four years previously the Daily Mail had reported on a bankruptcy hearing which established that ‘Turpin who earned £150,000 from his boxing career, now tussles for £25 a bout as a wrestler’.4 At a tax hearing at Warwick it was reported that: ‘His main creditor is the Inland Revenue. It claims £17,126 tax for boxing earnings between 1949 and 1958.’ He still owed ‘£15, 225’ and could only offer to pay back the tax bill ‘at £2 per week’ – a repayment schedule which would take ‘153 years’. Turpin had earned about £750 in 1961–2, but paid back a loan to a friend of £450 and £300 to his wife in cash, rather than the taxman. He was essentially broke and a broken man. The press, however, did not let the matter of his perilous financial situation or mental health condition rest. And because they did not, we can retrace the human circumstances of a controversial Coronial case concerning his valuable brain material: an approach this book will be following in subsequent chapters. For the aim is to uncover the sorts of human faces that were subsumed inside modern British medical research cultures.
In a hard-hitting editorial, the Daily Mail insisted that: ‘two questions must be answered about Randolph Turpin’s wretched life whilst boxing – Was he the lingering victim of punch drunkenness? What happened to the £585,439 paid to see his four title fights?’ Here was a ‘back-street kid who was a wealthy champion at 23, bankrupt at 34, and demented and dead at 38’.5 His ‘first marriage broke up, there were stories of assaults all pointing to a diminishing sense of social responsibility. A second marriage was to bring him happiness but his career… never recovered’. The newspaper asked why his family GP was not called as a medical witness at the Inquest. When interviewed by the press, the family doctor said that although ‘I do not like using the phrase, I would say that Turpin was punch drunk. He was not the sort of man to worry about financial matters or about people who had let him down. In my opinion boxing was responsible for his death.’ It was revealed that Turpin was ‘part deaf from a childhood swimming accident’ and he became ‘increasingly deaf through the years’. The GP, however, believed his hearing impairment had not impacted on either his physical balance or the balance of his mind. His elder brother and a family friend, nevertheless, contradicted that statement, telling the press that Turpin had ‘eye trouble’ and ‘double vision’ from his boxing days. He often felt dizzy and disorientated. The difficulty was that only Turpin’s 4-year-old daughter, Charmaine, and his youngest child, Carmen, aged 17 months (she sustained ‘bullet wounds in her head and chest’6) really knew what happened at the suicidal shooting. They were too young and traumatised to give evidence in the coroner’s court.7 In the opinion of Chief Detective-Inspector Frederick Bunting, head of Warwickshire CID, it was simply a family tragedy.8 Turpin had risen from childhood poverty and fought against racial discrimination (his father was from British Guyana and died after being gassed in WWI; his mother, almost blind, brought up five children on an army pension of just 27s per week, living in a single room).9 Sadly, ‘the money came too quickly’ and his ‘personality did not match his ring skill’, according to Bunting. Even so, by the close of the case what was noteworthy from a medico-legal perspective were the overarching powers of the coroner once the corpse came into his official purview. That evidence hinted at a hinterland of medical science research that seldom came into public view.
It seems clear that the pathologist commissioned to do Turpin’s post-mortem was prepared to apply pressure to obtain more human material for research purposes. Here was a fit young male body from an ethnicity background that could provide valuable anatomical teaching and research material. This perspective about the utility of the body and its parts was shared by the Royal College of Physicians, who wanted to better understand the impact of boxing on the brain. This public interest line of argument was also highlighted in the medical press, notably the Lancet. The family, meanwhile, were understandably concerned with questions of dignity in death. Their priority was to keep Turpin’s body intact as much as possible. Yet, what material journeys really happened in death were never recounted in the Coronial court. For, once the Inquest verdict of ‘death by suicide’ was reached, there was no need for any further public accountability. The pathologist in court did confirm that he examined the brain; he said he wanted to do further research, but tellingly he stated that he did not proceed ‘at that point’. Crucially, however, he did not elaborate on what would happen beyond ‘that point’ to the retained brain once the coroner’s case was completed in court.
As all good historians know, what is not said, is often as significant as what is. Today historians know to double-check on stories of safe storage by tracing what really happened to valuable human material once the public work of a coroner or pathologist was complete. The material reality was that Turpin’s brain was refrigerated, and it could technically be retained for many years. Whilst it was not subdivided in the immediate weeks and months after death, the fact of its retention meant that in subsequent years it could still enter a research culture as a brain slice once the publicity had died down. As we shall see, particularly in Chapter 6, this was a common occurrence from the 1960s onwards. At the time, it was normal for family and friends to trust a medico-legal system that could be misleading about the extra time of the dead it created with human research material. This neglected perspective therefore requires framing in the historiography dealing with bodies, body donations and the harvesting of human material for medical research purposes, and it is this task that informs the rest of the chapter.
The Long View
Historical studies of the dead, anatomisation and the use of bodies for research processes have become increasingly numerous since the early 2000s.10 Adopting theories and methodological approaches drawn from cultural studies,11 ethnography,12 social history, sociology, anthropology and intellectual history, writers have given us an increasingly rich understanding of cultures of death, the engagement of the medical professions with the dead body and the wider culture of body ethics. It is unfeasible (and not desirable) here to give a rendering of the breadth of this field given its locus at the intersection of so many disciplines. To do so would over-burden the reader with a cumbersome and time-consuming literature review. Imagine entering an academic library and realising that the set reading for this topic covered three floors of books, articles and associated reading material. It could make even the most enthusiastic student of the dead feel defeated. Two features of that literature, however, are important for the framing of this book.
First, we have become increasingly aware that medical ‘advances’ were intricately tied up with the power of the state and medicine over the bodies of the poor, the marginal and so-called ‘ordinary’ people. This partly involved the strategic alignment of medicine with the expansion of asylums, mental hospitals, prisons and workhouses.13 But it also went much further. Renewed interest in ‘irregular’ practitioners and their practices in Europe and its colonies highlighted how medical power and professionalisation were inexorably and explicitly linked to the extension of authority over the sick, dying and dead bodies of ‘ordinary’ people.14 More than this, the development of subaltern studies on the one hand and a ‘history from below’ movement on the other hand has increasingly suggested the vital importance for anatomists, medical researchers and other professionals involved in the process of death, of gaining and retaining control of the bodies of the very poorest and least powerful segments of national populations.15 A second feature of the literature has been a challenge to the sense and ethics of medical ‘progress’, notably by historians of the body who have been diligent in searching out the complex and fractured stories of the ‘ordinary’ people whose lives and deaths stand behind ‘great men’ and ‘great advances’. In this endeavour they have, inch by inch, begun to reconstruct a medico-scientific mindset that had been a mixture of caring and careless, clinical and inexact, dignified and disingenuous, elitist and evasive. In this space, ethical dilemmas and mistakes about medicine’s cultural impact, such as those highlighted in the Turpin case with which this chapter opened, were multiple. Exploring these mistakes and dilemmas – to some extent explicable but nonetheless fundamental for our understanding of questions of power, authority and professionalisation – is, historians have increasingly seen, much more important than modern ‘presentist’ views of medicine would have us believe.16
These are some of the imperatives for the rest of Parts I and II of this book. The remainder of this first chapter develops some of these historiographical perspectives. It does so by focussing on how trends in the literature interacted with social policy issues in the modern world. What is presented is not therefore a traditional historiographical dissection of the minutiae of academic debates of interest to a select few, but one that concentrates on the contemporary impact of archival work by historians as a collective. For that is where the main and important gap exists in the historical literature – we in general know some aspects of this medical past – but we need to know much more about its human interactions. Before that, however, we must engage with the question of definitions. Thus, around 1970 a number of articles appeared in the medical press about ‘spare-part surgery’ (today called organ transplantation). ‘Live donors’ and ‘donated’ cadavers sourced across the NHS in England will be our focus in this book too. To avoid confusion, we will be referring to this supply system as a combination of ‘body donations’ (willingly done) and ‘mechanisms of body supply’ (often involuntary). The former were bequested before death by altruistic individuals; the latter were usually acquired without consent. They entered research cultures that divided up the whole body for teaching, transplant and associated medical research purposes. This material process reflected the point at which the disassembling of identity took place (anatomical, Coronial, neurological and in pathology) into pathways and procedures, which we will be reconstructing. In other words, ‘pioneer operations’ in transplantation surgery soon ‘caught unawares the medical, legal, ethical and social issues’ which seemed to the media to urgently require public consultation in Britain.17 As one contemporary leading legal expert explained:
This is a new area of medical endeavour; its consequences are still so speculative that nobody can claim an Olympian detachment from them. Those who work outside the field do not yet know enough about it to form rational and objective conclusions. Paradoxically, those who work in the thick of it … know too much and are too committed to their own projects to offer impartial counsel to the public, who are the ultimate judges of the value of spare-part surgery.18
Other legal correspondents pointed out that since time was of the essence when someone died, temporal issues were bound to cause a great deal of practical problems:
For a few minutes after death cellular metabolism continues throughout the majority of the body cell mass. Certain tissues are suitable for removal only during this brief interval, although improvements in storage and preservation may permit a short delay in actual implantation in the recipient. Cadaver tissues are divided into two groups according to the speed with which they must be salvaged. First, there are ‘critical’ tissues, such as the kidney and liver, which must be removed from the deceased within a matter of thirty to forty-five minutes after death. On the other hand, certain ‘noncritical’ tissues may be removed more at leisure. Skin may be removed within twelve hours from time of death. The cornea may be taken at any time within six hours. The fact is, however, that in all cases action must be taken promptly to make use in a living recipient of the parts of a non-living donor, and this gives rise to legal problems. There is but little time to negotiate with surviving relatives, and waiting for the probate of the will is out of the question.19
Transplant surgeons today and anatomists over the past fifty years shared an ethical dilemma – how to get hold of human research material fast before it decayed too much for re-use. It was this common medico-legal scenario that scholars were about to rediscover in the historical record of the hidden histories of the body just as the transplantation era opened.
Ruth Richardson’s distinguished book, Death, Dissection and the Destitute, was first published in 1987. It pioneered hidden histories of disputed bodies.20 In it, she identified the significance of the Anatomy Act of 1832 (hereafter AA1832) in Britain, noting that the poorest by virtue of pauperism had become the staple of the Victorian dissection table. As Richardson pointed out, that human contribution to the history of medical science had been vital but hidden from public view. Those in economic destitution, needing welfare, owed a healthcare debt to society in death according to the New Poor Law (1834). Having identified this class injustice, more substantive detailed archive work was required to appreciate its cultural dimensions, but it would take another twenty-five years for the next generation of researchers to trace what exactly happened to those dying below the critical threshold of relative to absolute poverty.21 The author of this new book that you are currently reading for the first time (and three previous ones) has been at the vanguard of aligning such historical research with contemporary social policy issues in the medical humanities.
Once that research was under way, it anticipated several high-profile human material scandals in the NHS. These included the retention and storage of children’s organs at Alder Hey Children’s Hospital, the clinical audit of the practice of Dr Harold Shipman, and the response to the inquiry into the children’s heart surgery service at Bristol Royal Infirmary. Such scandals brought to the public’s attention a lack of informed consent, lax procedures in death certification, inadequate post-mortems and substandard human tissue retention paperwork, almost all of which depended upon bureaucracy developed from Victorian times. Eventually, these controversies would culminate in public pressure for the passing of HTA2004 to ensure that a proper system of informed consent repealed the various Anatomy Acts of the nineteenth and twentieth centuries, as we will go on to see in Chapter 2. Recent legislation likewise provided for the setting up of a Human Tissue Authority in 2005 to license medical research and its teaching practices in human anatomy, and more broadly regulate the ethical boundaries of biomedicine. As the Introduction suggested, it seemed that finally the secrets of the past were now being placed on open access in the public domain. Or were they?
Today, studies of the cultural history of anatomy and the business of acquiring the dead for research purposes – and it has always been a commercial transaction of some description with remarkable historical longevity – have been the focus of renewed scholarly endeavours that are now pan-European and postcolonial, and encompass neglected areas of the global South.22 In part, what prompted this genre of global studies was an increasing focus on today’s illegal trade in organs and body parts that proliferates in the poorest parts of the world. The most recent literatures on this subject highlight remarkable echoes with the increasingly rich historical record. Scott Carney, for instance, has investigated how the social inequalities of the transplantation era in a global marketplace are prolific because of e-medical tourism. In The Red Market (the term for the sale of blood products, bone, skulls and organs), Carney explains that on the Internet in 2011 his body was, and is, worth $200,000 to body-brokers that operate behind an antivirus firewall to protect them against international law.23 He could also sell what these e-traders term ‘black gold’ – waste products like human hair or teeth – less dangerous to his well-being to extract for sale but still intrinsic to his sense of identity and mental health. Carney calculates that the commodification of human hair is a $900 billion worldwide business. The sacred (hair bought at Hindu temples and shrines) has become the profane (wigs, hair extensions and so on) whether it involves ‘black gold’ or ‘Red Market’ commodities, in which Carney’s original phrasing (quoted in a New York Times book review) describes:
an impoverished Indian refugee camp for survivors of the 2004 tsunami that was known as Kidneyvakkam, or Kidneyville, because so many people there had sold their kidneys to organ brokers in efforts to raise desperately needed funds. ‘Brokers,’ he writes, ‘routinely quote a high payout – as much as $3,000 for the operation – but usually only dole out a fraction of the offered price once the person has gone through it. Everyone here knows that it is a scam. Still the women reason that a rip-off is better than nothing at all.’ For these people, he adds, selling organs ‘sometimes feels like their only option in hard times’; poor people around the world, in his words, ‘often view their organs as a critical social safety net’.24
Having observed this body-part brokering often during his investigative journalism on location across the developing world, Carney raises a pivotal ethical question. Surely, he asks, in the medical record-keeping the term ‘organ donor’ in such circumstances is simply a good cover story for criminal activity? When the poorest are exploited for their body parts, eyes, hair and human tissues – dead or alive – the brokers that do this turn the gift of goodwill implied in the phrase ‘organ donor’ into something far more sinister, the ‘organ vendor’. This perspective, as Carney himself acknowledges, is deeply rooted in medical history.
In the past, the removal of an organ or body part from a dissected body involved the immediate loss of a personal history. Harvesting was generally hurried and the paperwork done quickly. A tick box exercise was the usual method within hours of death. Recycling human identity involved medical bureaucracy and confidential paperwork. This mode of discourse mattered. Clinical mentalities soon took over and this lesson from the past has considerable resonance in the present. Thus, by the time that the transplant surgeon talks to the potential recipient of a body donation ‘gift’, involving a solid organ like the heart, the human transaction can become (and often became) a euphemism. Importantly, that language shift, explains Carney, has created a linguistic register for unscrupulous body traders too. Thus, when a transplant surgeon typically says to a patient today ‘you need a kidney’ – what they should be saying is ‘you need someone else’s kidney’. Even though each body part has a personal profile, the language of ‘donation’ generally discards it in the desire to anonymise the ‘gift’. Yet, Carney argues, just because a person is de-identified does not mean that their organ has to lose its hidden history too. It can be summarised: male, 24, car crash victim, carried a donor card, liked sports – female, 35, washerwoman, Bangladeshi, 3 children, healthy, endemic poverty. It might be upsetting on a post-mortem passport to know about the human details, disturbing the organ recipient’s mental position after transplant surgery, but modern medical ethics needs to be balanced by declaring the ‘gift’ from the dead to the living too. Instead, medical science has tended to have a fixed mentality about the superior contribution of bio-commons to its research endeavours.
Historians of the body that have worked on the stories of the poorest in the past to learn their historical lessons for the future, argue that it would be a more honest transaction to know their human details, either post-mortem or post-operative. Speaking about the importance of the ‘gift relationship’ without including its human face amounts to false history, according to Carney and others. In this, he reflects a growing body of literature on medical tourism, which challenges the prevailing view that medical science’s neglected hidden histories do not matter compared to larger systemic questions of social, medical and life-course inequalities for the living. Instead, for Carney and his fellow scholars, the hidden histories of ‘body donations’ were a dangerous road to travel without public accountability in the material journeys of human beings in Britain after WWII. They created a furtive research climate that others could then exploit. Effectively, unintended consequences have meant that body-brokers do buy abroad, do import those organs and do pass them off as ‘body donations’ to patients often so desperate for a transplant that medical ignorance is the by-product of this ‘spare-part’ trade. Just then as the dead on a class basis in the past lost their human faces, today the vulnerable are exploited:
Eventually, Red Markets have the nasty social side effect of moving flesh upward – never downward – through social classes. Even without a criminal element, unrestricted free markets act like vampires, sapping the health and strength from ghettos of poor donors and funneling their parts to the wealthy.25
Thus, we are in a modern sense outsourcing human misery in medicine to the poorest communities in India, Africa and China, in exactly the same way that medical science once outsourced its body supply needs in the past to places of high social deprivation across Britain, America and Australia, as well as European cities like Brussels and Vienna.26 The dead (in the past), the living-dead (in the recent past) and those living (today) are part of a chain of commodification over many centuries. In other words, what medical science is reluctant to acknowledge and which historians have been highlighting for thirty years is that a wide variety of hidden histories of the body have been shaped by the ‘tyranny of the gift’, as much as altruism, and continue to be so.27
Unsurprisingly, then, the complexities surrounding this ‘gift relationship’ are an important frame for this book.28 Margaret Lock, for instance, has explored Twice Dead: Transplants and the Reinvention of Death (2002) and ‘the Christian tradition of charity [which] has facilitated a willingness to donate organs to strangers’ via a medical profession which ironically generally takes a secular view of the ‘donated body’.29 One reason she notes that public confidence broke down in the donation process was that medical science did not review ‘ontologies of death’ and their meaning in popular culture. Instead, the emphasis was placed on giving without a balancing mechanism in medical ethics that ‘invites an examination of the ways in which contemporary society produces and sustains a discourse and practices that permit us to be thinkers at the end-of-life’ and, for the purpose of this book, what we do with the dead-end of life too.30 Lock helpfully elaborates:
Even when the technologies and scientific knowledge that enable these innovations [like transplant surgery] are virtually the same, they produce different effects in different settings. Clearly, death is not a self-evident phenomenon. The margins between life and death are socially and culturally constructed, mobile, multiple, and open to dispute and reformulation. … We may joke about being brain-dead but many of us do not have much idea of what is implicated in the clinical situation. … We are scrutinising extraordinary activities: death-defying technologies, in which the creation of meaning out of destruction produces new forms of human affiliation. These are profoundly emotional matters. … Competing discourse and rhetoric on the public domain in turn influences the way in which brain death is debated, institutionalised, managed and modified in clinical settings.31
Thus, for a generation that donated their bodies after WWII questions of reciprocity were often raised in the press but seldom resolved inside the medical profession by co-creating in medical ethics with the general public. There remained more continuity than discontinuity in the history of body supply, whether for dissection supply or transplant surgery, as we shall see in Part II. The reach of this research culture hence remains overlooked in ways that this book maps for the first time. Meanwhile, along this historical road, as Donna Dickenson highlights, often ‘the language of the gift relationship was used to camouflage … exploitation’. This is the common situation today when a patient consents to their human tissue donation, but it is recycled for commercial gain into data-generation. For the donor is seldom part of that medical choice nor shares directly in the knowledge or profits generated.32 In other words: ‘Researchers, biotechnology companies and funding bodies certainly don’t think the gift relationship is irrelevant: they do their very best to promote donors’ belief in it, although it is a one-way gift-relationship.’33 Even though these complex debates about what can, and what should go for further medical research and training today can seem to be so fast moving that the past is another country, they still merit more historical attention. Consequently, the historical work that Richardson pioneered was a catalyst, stimulating a burgeoning field of medical humanities study, and one with considerable relevance for contemporary social policy trends now.
How then do the hidden histories of this book relate to what is happening today in a biotech age? The answer lies in the immediate aftermath of WWII when medical schools started to reform how they acquired bodies for dissection and what they intended to do with them. Seldom do those procedures and precedents feature in the historical literature. This author studied in-depth older legislation like the Murder Act (running from 1752 to 1832) and the first Anatomy Act (covering 1832–1929) in two previous books. Even so, few studies move forward in time by maintaining those links to the past that continue to have meaning in the post-1945 era in the way that this study does.34 That anomaly is important because it limits our historical appreciation of medical ethics. It likewise adds to the problem of how science relates its current standards to the recent past. Kwame Anthony Appiah (philosopher, cultural theorist and novelist) conducting the Reith Lectures for the BBC thus reminds us: ‘Although our ancestors are powerful in shaping our attitudes to the past’ – and we need to always be mindful of this – we equally ‘should always be in active dialogue with the past’ – to stay engaged with what we have done – and why.35 Indeed, as academic research has shown in the past decade, the policing of the boundaries of medical ethics that involve the sorts of body disputes which are fundamental to us as a society also involves the maintenance of long-term confidence and public trust that have been placed in the medical sciences. This still requires vigilance, and in this sense the investigation and production of a seamless historical timeframe is vital. Such a process demands that we engage in an overview of the various threshold points that created – and create – hidden histories in the first place.
This is the subject of the next section, but since hidden histories of the body in the post-war period – stories like that of Randolph Turpin – are the product of, reflect and embody the powerful reach of intricate networks of power, influence and control, it is first necessary to engage briefly with the field of actor-network studies. Helpfully, Bruno Latour wrote in the 1980s that everything in the world exists in a constantly shifting network of relationships.36 The human actors involved operate together with varying degrees of agency and autonomy. Retracing and reconstructing these actor networks therefore involves engaged research and engagement with research, argue Michel Callow, John Law and Arne Rip.37 This approach to historical studies can enhance our collective understanding of how confidence and public trust change over time, as well as illuminate mistrust in the medical sciences. Latour argues we thus first need to ‘describe’ the network of actors involved in a given situation. Only then can we investigate the ‘social forces acting’ that shape the matrix of those involved. Latour along with Michel Callow hence prioritised the need to map the dynamic interactions of science and technology since these disciplines have come to such prominence in Western society. How the sociology of science operates in the modern world was likewise an extension of their work. Actor network theory and its study are therefore essentially ‘science in action’ and are one of the foundational premises of the case studies in Part II of this book.
Latour pioneered this novel approach because he recognised that science needed help to rebuild its reputation and regain its authority in the modern period, at a time when the ethical basis of so much medical research and claims to be in the public good became controversial in the global community. In 1999, John Law and John Hassard outlined a further development of actor network theory, arguing that if it was to become a genuine framework for transdisciplinary studies then it had to have five basic characteristics:
It does not explore why or how a network takes the form its does.
It does explore the relational ties of the network – its methods and how to do something within its world.
It is interested in how common activities, habits and procedures sustain themselves.
It is adamantly empirical – the focus is how the network of relationships performed – because without performance the network dissolves.
It is concerned with what conflicts are in the network, as well as consensus, since this is part of the performative social elements.38
Michael Lee Scott’s 2006 work further refined this model.39 He pointed out that those who defend the achievements of science and its research cultures too often treat its performance like a car. As long as the car travels, they do not question the performance of the results, the function of its individual components or its destination. Only when science stumbles or breaks down, is its research apparatus investigated. When society treats science like a well-performing car, ‘the effect is known as punctualisation’. We need medical mistakes and/or a breakdown of public confidence, argues Scott, to ‘punctuate’ our apathy about the human costs of the medical sciences to society as a whole. In other words, belief in science and rationalism is logical, but human beings are emotional and experiential too. If science has encapsulated our cultural imaginations for good healthcare reasons, we still need to keep checking that its medical performance delivers for everybody and is ethical. This notion of ‘encapsulation’, Scott explains, is important for understanding how the research cultures of the medical sciences really work. A useful analogy is computer programming. It is common for programmers to adopt a ‘language of mechanism that restricts access to some of the object’s component’. In other words, when a member of the general public then turns a computer on, most people are generally only concerned that the computer works today in the way that the car-owner does when they turn on the ignition key in the morning to go to work. Even so, those simple actions hand over a considerable part of human agency to new technology. On the computer, we do not see the language of algorithms (the mechanisms of the system) that have authority over us and conceal their real-time operation. Science operates in an equivalent way to computer programmes, according to Scott, because it has hidden and privileged research objectives, written into its code of conduct and a complex, interrelated and often hidden set of actors. This book takes its lead from this latest conceptual thinking in actor network studies, but it also takes those methods in a novel research direction too. We begin by remodelling the sorts of research threshold points created inside the system of so-called body bequests and what these ‘donations’ meant for the way that the medical sciences conducted itself, networked and performed its research expertise in post-war Britain.
Remapping Disputed Bodies – Missing Persons’ Reports
The quotation ‘volenti non fit iniuria’ – no wrong is done to one who is willing – encapsulates modern attitudes towards ethical conduct in the dissection room, transplant operation theatre and more widely towards the use of human tissue and body parts for research purposes.40 In practice, however, things are rarely this simple. Bronwyn Parry, a cultural geographer, has described this defensive position as follows:
New biotechnologies enable us, in other words, to extract genetic or biochemical material from living organisms, to process it in some way – by replicating, modifying, or transforming it – and in so doing, to produce from it further combinations of that information that might themselves prove to be commodifiable and marketable.41
In other words, the patient consents, is willing, and soon becomes the ‘other’, whether in life or death. A new cell-line, blood-product or genome sequence erases an original body identity. The ‘donor’ and ‘donated human part’ or ‘tissue’ are re-designated – ‘Out there’.42 As Margaret Lock explains – ‘first a dead body must be recognised as alienable … legally available for transfer or sale. Current policies in North America and Europe treat cadavers and body-parts as “quasi-property”, thus making them alienable, but their transfer may not involve payment’ or at least not a direct payment.43 Often there is (for instance) a refund of petty cash expenses to suppliers, as a way of working around regulations. The law of medical negligence on both sides of the Atlantic states in case law that the body is ‘abandoned’ into these recycling schemes – known as bio-commons. If the person has consented to this, then it is a transparent process. Yet, often, and particularly under the Human Tissue Acts of 1961 and 1984, this was not the case (which Chapter 2 explains in greater detail). During the various government enquiries into NHS organ scandals, the conclusion was that all the original paperwork to reconstruct what really happened had been cursory, destroyed or never created in the first place. Generic figures covering the scale of organ retentions are thus often cited routinely in the historical literature, without checking their material pathways inside the research culture of the time. This book argues that the human material was traceable, provided we begin by reconstructing the threshold points of medical research. Thus, after 1945, the anatomical sciences, coroners and pathologists formed actor networks inside the research community of the medical sciences in Britain. They passed human material along a chain of human supply from operating theatre (amputated part or dead person) to hospital morgue or pathology laboratory, from the teaching lecture theatre or dissection room, to burial or cremation. Together they performed a series of research thresholds in disputed bodies and hidden histories of the dead. In remapping these, it is feasible to trace a whole series of what effectively became missing persons’ reports, acknowledged by HTA2004. Conceptually, we need thus to start modelling a process that was hidden from public view.
The first research threshold point of the historical process for each individual ‘body donation’ was the need to put pressure on people to think more about giving. The second threshold point is usually then the approach made by a medical professional to obtain that tissue or organ when the time is right. The third threshold point normally comes with the medical decision to use that tissue or organ for a particular purpose. These threshold points go on being crossed until the human donor ‘disappears’ in terms of their whole body identity (see Chapter 4), but crucially their body part or human material does not. In point of fact, it is capable under certain circumstances of being recycled multiple times. A human heart transplanted from a young to an older person could (in theory) for instance be reutilised again, provided, that is, it remains healthy enough to be taken from one transplant recipient and given to another patient on a waiting list (see Chapter 5). Sometimes recipients need two hearts in their lifetime because each operation is time-limited by the effectiveness of immunosuppressant drugs. Mortality rates are much higher in such cases, but they are occasionally medically feasible. Tissue that is cultured or brain slices likewise could be recycled many times for different purposes under a myriad of medical research circumstances (see Chapter 6). This means that crossing these threshold points in modern science will always involve the potential for ambiguity, dispute, dilemma and resolution. Nothing is fixed, little is certain. Yet, medical science does two critical things with and around these threshold points which are in turn crucial for this book.
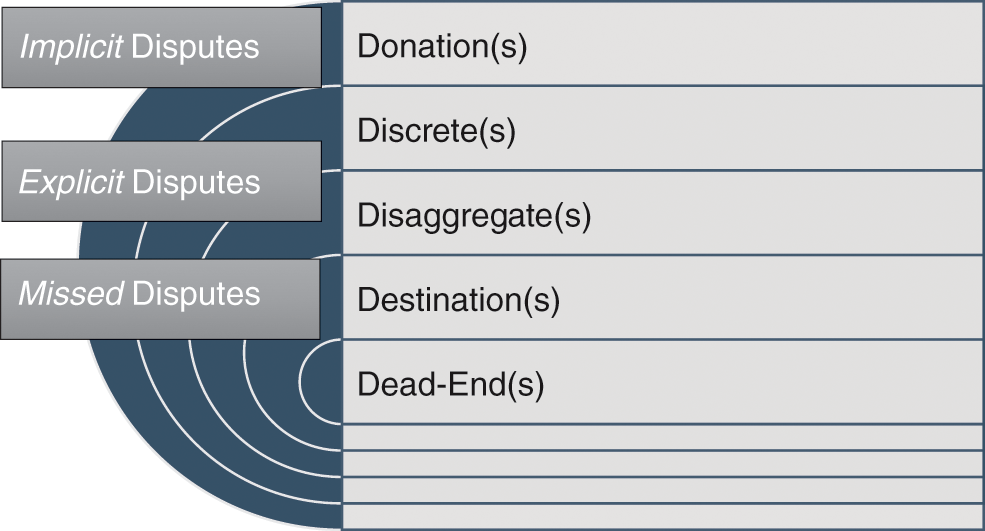
The first is that it treats each one of the threshold points described above as discrete. This is deliberate because such an approach distracts public attention from potential disputes about the fuzziness that surrounds medical ethics as each research threshold is crossed. The breaking up of a whole body history into parts across discrete moments on a research pathway is essential to disaggregate the human being from their ‘body donation’ point. In mapping, therefore, its historical process, we find – donation(s), discrete(s), disaggregate(s) and destination(s) – all to push past – dead-end(s) (see Figure 1.1). In other words, to become the ‘other’ you need a ‘donation mechanism’ that separates the ‘gift’ from its eventual destination, often called ‘out there’ or ‘abandoned’ as bio-commons in medical case law.
The second aspect is that medical science effectively treats each threshold point as ahistorical. The history of the person and the body or body part is there but it does not matter or is not central to the crossing of a threshold. To add to the confusion, the keeper of the record of what is happening at each threshold point is one step removed from the clinical bench of medical science itself. The regulator does not take an overview of the entire research recycling process but concentrates instead on monitoring each threshold point: essentially the modus operandi of the Human Tissue Authority and older legislation in the past (see Chapter 2). Regulators tend to wait until medical science reports to them the need for a license to use human material. This is a matter of professional trust, but it also distances that official oversight from the whole body of the donor from which in principle a wide variety of human material disappears from public view. Essentially, medical science’s ‘body donation mechanism’ was (and is) given the capacity to act in a series of discrete steps in terms of its actor-network performance, and because its research professionals did just that, acts of bequest and donation move seamlessly into hidden histories of dead bodies and body parts. However, at each threshold point, relevant choices about its component activities and parts can become controversial – a drug development was judged worth the investment return – a specific treatment became commercialised – an experiment that was externally fundable was prioritised – and so on. In this sense, a set of related ethical questions arises that tends to remain unresolved in the historiography because few study them in-depth. What happens if these threshold points are not considered discrete in popular culture, and as a donor you regard them as one whole – as many people did around the time of the NHS scandals in 1999? What happens if this complete history does matter in certain cases, as it did in the case of Randolph Turpin at the start of this chapter? By way of further example, although there are rigorous screening protocols in place for cancer patients in full remission who donate, some recent transplant cases have been reported of a donor giving recipients undetected breast cancer at the point of transplantation.44 Surgeons estimate the chances of this happening are ‘between 1 in 10,000 and 5 in 10,000’; even so, the discrete history of each organ does matter to those living patients reliant on the dead for their healthy survival. Likewise, what happens when you have a whole set of body disputes that emerges in time to undermine public confidence and trust? These are complex issues, but ranging widely over the historiographical literature and primary materials, we can see that dealing in discrete thresholds generates three sorts of tensions (or disputes) between medical science broadly defined and ‘ordinary’ people and those (like the press) who represented them. These stress points are crucial to this volume.
First, they involve implicit disputes of the sort explored in Chapter 4. Here we encounter the stories of people who allowed use of their bodies by default rather than design, largely a reflection of the fact that nobody explained to them all the research steps properly. Second, we encounter explicit disputes of the sort explored in Chapter 5, where, for instance, coroners co-operating with transplant teams had the right to remove more than they declared officially after, say, road-traffic accidents, discovery of which brings them into direct conflict with families, the law or both. Finally, we can find missed disputes of the sort that underpin Chapter 6. Here, people were not able to dispute the use of dead bodies and their brain material because the discrete thresholds, layered onto complex actor-network relationships, kept them uninformed, such as at Alder Hey Children’s Hospital when pituitary glands of dead children were taken as ‘bio-extras’. In other words, it is true that ‘no harm is done to someone that was willing’ (as the Latin quotation stated at the start of this section). However, many people might have been unwilling to consent to the extent of what was about to be done to them or their deceased loved one, but they did not know this at the time, and these hidden histories matter to everybody. For, paradoxically, the medical profession prefers piecemeal methodologies that are untraceable, since these are not easily legally accountable. By pausing briefly to engage with a human story, this scenario can be poignantly and powerfully illustrated.
In the late 1950s, a distinguished and decorated hero of WWII died under tragic circumstances. For ethical reasons, this book does not identify this individual because they may still have living relatives. The 100-year rule has been applied to ensure that any distant kin who could not be consulted to give informed consent are still treated with the utmost dignity in this study, despite the fact that some of this information has been in the public domain for sixty years. Detailed record-linkage work reveals that the person in question had worked on mine sweepers in the Atlantic during WWII. Their career ladder was impressive. They were promoted after being ‘Mentioned in Despatches’ (MID) for bravery and eventually awarded the Distinguished Service Order (DSO). Once the war finished, like many service personnel, they were not discharged for some years after 1945. Even by the early 1950s, there was still a lot of cleaning up to do and de-militarisation of equipment to co-ordinate from the War Office in London. Thus, the war hero transferred to the regions, was allocated a new logistics job. Soon they were ‘overworked’, according to contemporary accounts. They had to process a large amount of paperwork in what became a busy semi-civilian job. As they were a diligent person, eventually the excessive workload triggered ‘depression’. Since they had never had an experience of mental ill-health, they booked an appointment with a local doctor under the new NHS. That GP signed the person off work for a time, but then ‘allowed [his patient] to return to work because he considered [the patient] was worrying so much about [the] paperwork piling up’ that a leave of absence was counter-productive to the war hero’s mental well-being.45 By now, the individual was middle-aged, had a settled home life, was married in a stable relationship, but still they found it hard to cope at work. Eventually, they drove their family car one Sunday evening to a remote side-road near the coast in the South of England and attached a tube from the exhaust pipe into the passenger side, and then rolled up the window. At a subsequent Coronial hearing: ‘the cause of death was stated as asphyxia due to the inhalation of carbon monoxide gas … while the balance of [name withheld by this book’s author] mind was disturbed’. The individual in question did not donate their body to medical science in their will. Nonetheless, what happened next does indicate the research threshold points that this dead body was now about to cross in the hands of medical science.
The first threshold point was that by virtue of the physical fact of a suicide, the body in question became the responsibility of a coroner whose public duty it was to perform a post-mortem and report to an Inquest Jury. At this point, the coroner had two legal options: to extensively cut open the body and examine the lungs and heart and/or test the carbon monoxide levels in the tissue; or, examine the external appearance of the body and use his powers of discretion to declare a death by suicide. Historically, this latter option, a ‘non-Jury’ case, came under Coroners’ Regulations. Since the early 1830s, when coroners started to be medically, not legally qualified, they had the discretion to save the costs of a post-mortem if a death was obvious, for example, in drowning cases. In other words, at this first threshold point, the body might be cut a little, some, or a lot. It all depended on the decision of the coroner, whether he was legally or medically qualified (or both) and the local political temperature, shaped by events surrounding an unexplained death. Today this practice continues with paper inquests, and it has always been part of Coronial discretionary justice.
The second threshold point that is then noteworthy is that despite a lack of bequest, this body went next to St Bartholomew’s Hospital in London. The records indicate that the person died, there was a quick Coronial hearing and the body arrived at the dissection room within a total of two days. It is likely some testing had been done on its CO2 levels and heart/lung tissue samples were removed for examination, but the body itself was substantially intact at this handover given the speed of delivery. It was now about to fall under the official jurisdiction of the dissection room because Coronial offices often had close working relationships with medical schools needing a steady supply of the dead to train students in anatomy in the 1950s. It had therefore travelled about 100 miles by van. In other words, the whole body had started to become the ‘other’ on that journey – literally and metaphorically moving by means of a medical bypass – but it was not, as yet, not ‘out there’ in parts – where its ultimate destination would be diverted to the cul-de-sac of history (as the Introduction outlined) until this book remapped it.
Crossing a third threshold point, the body of the dead person passed into the dissection room jurisdiction to underpin further teaching and research. It is evident from the original records that this phase took one and a half years in total, from entry to leaving the dissection room for the final time to be buried (cremation was not yet commonplace as it is today). In other words, this body was cut up extensively and no opportunity to learn missed. On entry, it was refrigerated and embalmed. This involved first washing the body. Then embalmers made initial small cuts at the neck in the carotid artery area and injected preservation chemicals into the inner thigh. The embalmer on duty pumped embalming fluid (a mixture of ethanol and formalin) into the arteries. About 25 to 40 litres was the normal level. Bodies were always refrigerated and checked regularly to see that the process was working. Additional fluid injected directly into areas of the body not responding to the chemical processes to fix the human material was likewise the usual procedure. Once preserved, cadavers, placed on a metal table in a temperature-controlled dissection room, were covered with a shroud until ready for teaching. The head was shaved for cleanliness too, akin to the sort of shorn-head appearance of all serving recruits in the armed forces. As the procedures for dissection were methodical on site, we can proceed to the fourth threshold point.
Allowing for the fact that the heart was still present (in some cases, coroners removed it as a precaution in suspected homicides, but this does not seem to have been so here), then medical students on site spent a concerted amount of time dissecting it. The lungs likewise were always the focus of intense interest, as would be the major organs like the liver and kidneys. The separated skin and each body part were prepared as prosthetics. The head generally was the focus of a month of teaching sessions too. Of importance here were the age, general condition of the body and its gender. The coroner’s report said the deceased ‘enjoyed reasonably good health’ despite a recent episode of ‘depression’. The person was middle-aged and had led an active life; therefore, the human remains were very good teaching aids. They were also useful for further research into mental ill-health in the brain, provided the pathologist had frozen below –20 degrees centigrade (rather than embalmed) that body part after a post-mortem. Consequently, the crossing of thresholds three and four technically represented a research opportunity to learn more about the potential physical manifestations of a suicide case and its neurology. Each threshold point was self-evidently a discrete step in which a whole body history was being dis-assembled into a series of hidden histories where the physical reality of completeness and the history of the person were eroded.
What happened then to each body part, organ, tissue or brain slice tends to fade from view into the jurisdiction of the pathologist and medical research community, as we shall see in the following chapters. After eighteen months, the body was buried with a Christian ceremony, complying with legislation. A family of undertakers in the employ of the dissection room at St Bartholomew’s for almost 100 years did the internment (see Chapter 4). Consequently, here, as the ethnographer Marie Andree Jacob puts it: ‘What deserves particular attention is the very creative ways actors [in this case, coroner, pathologist, dissector, student, medical researcher, lab technician and scientist] go around the law while going through the legal processes: for this is how legality is experienced.’46 In other words, it is important not to be distracted by the medical sciences’ insistence on the ‘global’ over the ‘local’. Indeed, this reunification does require a lot more concerted effort in the archives. Nonetheless, what historical research has to do is ‘privilege the microscope over the telescope’ to trace each threshold point, engaging with its hidden histories of the dead and potential body disputes (explicit, implicit and missed).47 That endeavour will provide a checking mechanism in respect of the success story of the ‘body donation mechanism’ of the medical sciences since WWII, testing in context the maintenance of public confidence and trust (or not) in actor networks and their achievements.
The material reality is that this suicide could have had many different types of threshold points. These would have shaped the sorts of disputes that could arise. The individual might have made a body bequest in a particular way that led to a medical breakthrough. If so, their bereaved family may have wanted to participate in its knowledge formation as a consolation after death but missed an opportunity to do so. On being opened up (even without this happening voluntarily), it is entirely feasible that a war hero would have a good physiology that a medical researcher was waiting on. Certainly, one cannot rule out the possibility that this body in the 1950s contributed to the development of crime scene forensic science. It could also have been used for new research into cancers caused by the presence of asbestos in the lungs, as the person had worked on mine sweepers in the war that would later prove to be of importance for the study of painful mesothelioma. As yet, Crick and Watson’s discovery of DNA at Cambridge was just four years old. Had the war hero died ten years later, the potential was there in the cells for early genetic study. Even so, human tissue culture work took place at the Strangeways laboratory in Cambridge at the time of death and St Bartholomew’s Hospital had shared training facilities and dissected cadavers with Oxbridge since the war. All of these possibilities and their potential thresholds could have created material afterlives. Speaking about them in this way is not about ‘moral pronouncements’ in which there have traditionally been ‘two camps’ – one defending science’s achievements, the other doing the opposite – but instead focusses historical attention onto the nature, scope and meaning of body ethics in both a historical and modern sense.48 And of course there is an irony here. Because the importance of discrete threshold points and their potential for generating dispute has rarely been acknowledged, medical science has gone about the Enlightenment project in a rather contradictory manner. Combating ignorance with reason, rationality and science has been dependent on the ignorance of donors about what was going on to achieve the ultimate goal called ‘progress’. Should the combatting of medical ignorance rely on generating cultural ignorance to this extent, is a thought-provoking question and one with wide-ranging ethical implications. Soon it gave rise to public criticism and a demand that the human story must be restored to the relationship between medical researchers and teachers and the bodies that they relied upon. It is to this medical humanities issue that the chapter finally turns.
Everybody – ‘Who Must Own the Organs of My Body?’
I think it is self-centred of the public to feel they have a right to other people’s organs without offering their own, and I think the present system, under which hundreds of kidney patients die each year while many more useful organs are destroyed is … inefficient. And yet, I cannot go along with the suggestion one’s body, even after death, should be considered the property of the state. Perhaps this is a libertarian view, or perhaps it is simply the greatest irony of the transplant problem. The period of this great scientific advance has coincided with a decline in a sense of collective responsibility, and the advance itself, by making us think we can postpone death indefinitely, has discouraged us from making arrangements for our own demise.49
In many respects this short extract from a feature article in the Independent on Sunday in the early 1990s denoted the start of a public discussion about body disputes. It recognised controversial human harvesting issues that the general public may have wanted to raise about the regulation of organ donation, transplant surgery and ‘body donation’ bequests, but did not have the full information to do so. The rise of doctoring in British society as a profession over several hundred years had created a set of expectations for fee-paying patients that ‘death’s door’ would be held shut for as long as possible by the medical sciences.50 After 1948, NHS consumers became taxpayers with a stake in the best that medical science could share with everybody. It had once been the view that, as George Steiner, the moral philosopher, explains: ‘Death has its history. The history is biological, social and mental. … Every historical era, every society and culture has had their own understanding, iconography and rites of mortality.’51 In Western cultures, by the modern era, however, the way that people had traditionally edified ‘the House of the Dead’ (to use Steiner’s analogy) was starting to change shape, and radically so. It no longer had in the popular imagination a clearly defined deadline – the metaphysical belief that this is your time, and date, and you must enter here after the traditional lifespan of three score years and ten – for that biblical timetable had eroded slowly with secularism and science. Patients now expected to push past the dead-end of life, and indeed, in many respects that so-called deadline seemed more alive than dead in emergency rooms that had lower mortality rates from improved resuscitation facilities. For Steiner this has created nonetheless what he calls ‘the barbarism of specialisation’ and with it the inability to see material things including the human body ‘in its totality’. The real problem is that it has also tended, in his view, to misrepresent scientific invention as human creativity. It is important to reflect on this philosophical perspective because it has often been excluded from historical accounts of the ‘success story’ of the medical sciences in the modern era.
Steiner points out that science seldom looks back. Its mentality is to cancel a drug, medical procedure or surgical innovation and move on to the next big breakthrough.52 Why study Newton when Einstein has taken a leap forward, was a rational position to take by the twentieth century; the new displaces the old. But this, Steiner believes, is contrary to the history of the creative arts over centuries. Creativity links the whole to each part – one artwork to another, one novel to a series of writings and so on. It is rare for new knowledge to cancel out old mind-sets and perspectives altogether. Knowledge is often compartmentalised for a time, retains the potential to re-join a creative conversation, may keep changing emphasis, and often productively so. What has tended to happen over a century of innovation in science that is worrying, for Steiner and philosophers of the body, is that the public have come to expect medical science to do the editing of information for them. This neglects the creative potential of knowledge formation, reinvention and retrieval in which everyone should be involved. Science instead will typically develop a new drug and work to lessen its side-effects because of the expense of clinical trials. Even if the drug is not really fit for purpose for some patients, the medical sciences will keep using it despite its downsides; until, that is, their lack of creative imagination to revisit their research agendas is held to public account. Occasionally we glimpse this sort of scenario, most notably in the case of thalidomide, which illustrates this key point succinctly.
Thalomid [sic] was the original name of the drug developed and sold in Germany in 1957 under the trade name Contergan.53 It was marketed without proper clinical safeguards for nausea and morning sickness in pregnancy, then banned. Later, its chemical interaction that stunted human growth in the limbs persuaded some governments to issue it under special license for cancer and leprosy treatments to inhibit tumours. The ‘dark remedy’ had thus a ‘one-track’ scientific history, until a public outcry caused its creative potential to be unlocked. This is exactly the sort of predicament that troubled Rhoda Koenig (the journalist) in her 1990s short piece on organ donation that opened this section. The ‘postponement of death’, as she put it, makes everyone’s eventual ‘demise’ not just difficult to talk about but there is an endemic cultural denial about difficult situations. ‘Edit me down so that I survive longer’ is all very well, as she explains, but it also disempowers the patient. Further complicating that situation was the reluctance of the medical profession to speak openly about the successes and failures of their clinical work, as the thalidomide controversy showed. Indeed, seldom was the legislative framework regulating laboratory practice, the development of drug rejection therapies or human tissue experiments, set out clearly in print in the immediate post-WWII era (see Chapter 2 for a more detailed discussion of the legalities). Innovations were publicised in the medical press like the Lancet and British Medical Journal, but almost never was the cohort of bodies or human tissue research activities acknowledged openly. It was not a legal requirement and thus omitted. Any publicity tended to be about promoting a new breakthrough and accrediting it to a doctor or scientist on their career path. A cultural fissure consequently started to open up after 1945 in Britain. The public thought they were being fully informed, when they were not; and the medical sciences assumed that the general public did not want to know what they did not know about!
Anatomists, clinicians and pathologists thus found themselves in a bad self-validating prophecy of their making: the public do not understand what we do, and we do not understand their attitude to us – ergo, we cannot work or co-create together. What exacerbated this situation was how talented doctors and scientists – ones genuinely working to improve the public good – made assumptions that laws in the past superseded present-day regulations. Soon it became clear that they were still working with outdated laws, broken down, tinkered with and rehashed, but never repealed. In stressing patient confidentiality (a legitimate legal concern), they seldom thought to look at the legal basis of their paperwork on bequests, post-mortems and so on. In other words, the methodologies of the medical sciences with their threshold points in human dissection and further research, done in discrete stages, ironically matched the way that the law itself had been revised in bits and pieces instead of in its entirety for the living and the dead. This cultural stand-off (for that is what it amounted to by the end of the 1990s) was further exacerbated by the medical sciences’ scepticism about the value of human stories to their research endeavours. This scepticism is misplaced, argue moral philosophers and poets such as John Glenday; his poetic satire is biting about medical science’s proverbial rubble from this recent past:
To disassemble might be a necessary and inevitable part of research, but to forget is not. This book thus builds on philosophies of the body and science since it challenges, resituates and rediscovers the human ‘rubble’ of a bio-commons.
Conclusion: ‘No Decisions about Me, without Me’
HTA2004 reflected a wide range of reactions to a recent (and not so recent) history of disputed bodies that has included – anger, blame, disappointment, frustration, regret and sadness. In many respects, it follows that the fallout of that history was always going to be far-reaching but not necessarily in the ways that the medical sciences would have anticipated. After 2005, body donations did not decline dramatically, and more people were willing to donate their organs in the first decade of the new legislation because of the work of the Organ Donation Task force set up by the government in 2008.55 Rebuilding public trust can nonetheless be a complicated process. Often it is damaged far quicker than the long time it takes to be established. What continues to be at issue is the cultural fissure opened up by NHS scandals in 1999. These have been exemplified by the ongoing public stand-off over compulsory organ donation. On 17 July 2007 BBC News, for instance, reported that Sir Liam Donaldson (former Chief Medical Officer at the time of the NHS organ retention controversy) had done a volte face, despite his support for the principle of inclusiveness embedded into the new HTA2004 statute. He had embraced a system of ‘presumed consent’ because of long waiting lists for organs.56 Yet, as the Shadow Health Secretary at the time, Andrew Lansley, replied: ‘The state does not own our bodies, or have the right to take organs after death’ – echoing the prescient journalism of Rhoda Koenig in the 1990s touched on early in this chapter. That concept of state ownership has been rejected in Scotland (for now), though adopted in Wales from 2015. In England, meantime, what remains the subject of lively debate is the ethical principle of ‘No decisions about me, without me’, as it embraces in 2020 a new organ donation scheme based on the Welsh opt-out facility for the living and presumed consent for the dead. This proposal to change the law prompted lively discussion at a meeting of the Royal Society of Medicine (hereafter RSM) convened on 23 June 2016 to reflect on twelve years after ‘the good, the bad and the ugly’ of HTA2004.57
What remains palpable in bioethics is that if a person (alive or dead) gives (or has given) consent – whether for human tissue, cell-line, biopsy or organ – and if a medical researcher makes an invention or innovation that proves to be of commercial value from that human material – then that outcome distorts the ‘goodwill’ of the bequest. If we have moved from ‘proprietorial’ to ‘consensual’ medical ethics after HTA2004, then that legal emphasis has yet to become a medical reality in working practices. Moreover, there remains the difficult question of what happens when human tissue becomes recycled into computer data. Hugh Whittall, Director of the Nuffield Council on Bioethics, thus explained at the recent RSM conference in June 2016 that:
The long-term challenge is the issue of tissue banking. The value of a tissue sample, he says, is beginning to reside more ‘in the huge amount of data it can deliver once you put it through any kind of biochemical or genetic analysis’.
‘So to some extent, tissue banks could become redundant once you have got the data or information in the tissue. We then move from the framework of human tissue regulation into the framework of data and information regulation.’ The interaction of regulatory control and legal and ethical frameworks is going to be very difficult, he thinks, because ‘the two areas have not necessarily matched up completely’.
The current legislation … should be capable of working for ‘another 10 or 15 years, because we quite deliberately introduced a degree of flexibility and discretion that could be exercised by the HTA’.58
The rising cost of regulation, the bureaucracy involved, the question of how far systems of medical research are streamlined enough to be inspected uniformly and, above all, the fast-moving e-globalisation of all our personal information, remain uncertain. ‘Hack-work’ was once pejorative slang for medical students cutting open corpses. Now to be ‘hacked’ involves breaches in data protection privacy laws and ‘goodwill’ needing a better firewall to protect the biomedical boundaries being broken down in medical science.
Looking back, leaping forward, it remains apparent that when the medical sciences had ‘a degree of flexibility and discretion’ in the past (to quote Hugh Whittall’s phrasing above) they proved incapable of handling it. To build ‘deliberately’ therefore the same discretionary powers into HTA2004 to ensure it has longevity as a piece of legislation in terms of a Human Tissue Authority management culture, is dubious from a historical standpoint, however well intended its work. For it negates any historical sense of the research processes and their threshold points in the pieces of a medical mosaic. Indeed, it is striking that no historian of the body was (or is) invited to sit on the Human Tissue Authority. Such observations suggest that scientists, doctors, anatomists, coroners and pathologists continue to take a proprietorial view of the bodies and body parts in their professional hands. Few voluntarily adopted the mentalities of custodianship, and arguably this hidden history is still having important ramifications in scientific research circles today. As Sir Jeremy Farrar, Director of the Wellcome Trust, highlighted in his recent blog post on 10 September 2019:
The emphasis on excellence in the research system is stifling diverse thinking and positive behaviours. As a community we can rethink our approach to research culture to achieve excellence in all we do. The UK’s research sector is powering ahead, with our world-leading universities generating knowledge and innovations that are improving lives around the world. But in the engine room of this great enterprise, warning lights are blinking on. The relentless drive for research excellence has created a culture in modern science that cares exclusively about what is achieved and not about how it is achieved. As I speak to people at every stage of a scientific career, although I hear stories of wonderful support and mentorship, I’m also hearing more and more about the troubling impact of prevailing culture. People tell me about instances of destructive hyper-competition, toxic power dynamics and poor leadership behaviour – leading to a corresponding deterioration in researchers’ wellbeing. We need to cultivate, reward, and encourage the best while challenging what is wrong.59
Perhaps one of the greatest ironies is that the heritage sector may have better working practices in terms of the custodianship of our national assets than the medical sciences, which dominate public spending by government. Maybe because the heritage sector has always had a charitable status defined by trusteeship, its ethics were co-created in conversations with the entrance-fee-paying public. Yet, in medicine, people do pay their equivalent entrance fee in taxes to fund the NHS; its medical research base from patient case-histories is a national asset too: as the Covid-19 pandemic is highlighting. It is a point of view worth considering that whereas voters want politicians to protect the physical public ownership of the natural landscape of the environment, seldom are the insides of human nature seen as needing the same public property safeguards. One thing remains certain. This is a history not simply in our keeping, but in our collective making too. For, as Farrar emphasises, the medical sciences still need a more caring culture – ‘not exclusively about what is achieved’ but ‘how it is achieved’ too. The disputed bodies that have been missed and mislaid, exemplify the need for vigilance about the ethical basis of pushing back all our deadlines. We next therefore examine the legal framework of the messy business of these muddled research threshold points of the modern era.