6.1 Introduction
This chapter discusses a range of issues related to good clinical practice in psychopharmacology. It has been written to address the wide readership of care professionals who are involved in prescribing, monitoring and/or advising patients about psychiatric medication, which includes psychiatrists, pharmacists, psychiatric nurses, primary care physicians and hospital doctors.
Most people who are treated for a psychiatric disorder are managed in primary care by their primary care physician and never consult a psychiatrist. Those who do come under the care of a psychiatrist are also likely to see other mental healthcare professionals, including psychiatric nurses, clinical psychologists, social workers and occupational therapists. Often, they will have more frequent contact with these professionals than with their psychiatrist or primary care physician and so will tend to raise queries about medication with them. Within secondary care mental health services in the UK, care coordinators often have a formal role in monitoring the effectiveness of psychiatric medication and screening for potential adverse effects. Psychiatric nurses usually administer long-acting injectable (LAI/depot) antipsychotic preparations. Nurse-led clozapine and lithium clinics have been shown to be effective; the monitoring of the patients who attend includes relevant blood tests and assessment of side effects (Clark et al., Reference Clark, Wilton and Baune2014; Gage et al., Reference Gage, Family and Murphy2015; Shaw, Reference Shaw2004). Further, a significant proportion of patients under the care of secondary care physicians are likely to be prescribed psychotropic medication, partly because of the increased prevalence of depressive and anxiety disorders in patients with chronic medical conditions (Wells et al., Reference Wells, Golding and Burnam1988) and the increased prevalence of diabetes and cardiovascular disease in people with schizophrenia and bipolar disorder (Hoang et al., Reference Hoang, Stewart and Goldacre2011).
Non-medical prescribing is another reason why psychopharmacology is not just the province and interest of doctors. It was introduced in the UK in 1992, allowing healthcare professionals other than doctors or dentists to prescribe medicines after obtaining a prescribing qualification. In the UK, the largest group of non-medical prescribers are nurses, followed by pharmacists, with a third and much smaller group made up of miscellaneous health professionals (Cope et al., Reference Cope, Abuzour and Tully2016). Currently, nurses can be granted prescribing authority in many other countries, including Australia, Canada, New Zealand, various European countries and several states in the United States.
When medication is used to treat a psychiatric disorder, it is usually only one part of a wider treatment plan, which should be tailored to the individual and devised and agreed by the patient and prescriber working in collaboration. As such, pharmacotherapy is commonly accompanied by appropriate social and psychological treatments, the complexity of which can vary greatly. Such interventions may include simple lifestyle advice such as avoiding stress, reducing excess alcohol consumption and engaging in regular physical activity and exercise. Social treatment may encompass regular voluntary work, a support worker to provide assistance with practical activities, assessment by an occupational therapist regarding adaptations to the home or a social worker to help with the management of complex social issues. Psychological treatment can include interventions such as guided self-help, family therapy, cognitive behavioural treatment (CBT) and mindfulness.
6.2 Ensuring a Favourable Benefit-to-Risk Balance
Every time a prescriber starts a medication or initiates a pharmacological strategy such as a high-dose or augmentation regimen, it should be as an individual patient trial (Barnes et al., Reference Barnes, Dye and Ferrier2014; Maxwell, Reference Maxwell2009), the outcome of which is uncertain. There should be agreement between the prescriber and the patient on the goals of therapy, such as relief of acute symptoms or long-term prevention, and the rationale for the particular medication prescribed, including its expected risks and likely gains. It should be clear what will be required in terms of the frequency and nature of review appointments and monitoring in order to assess the effects of the treatment over an appropriate timescale. At review, the extent to which the treatment aims have been achieved and the extent to which these are offset by any harms should be assessed. On this evidence, a decision can be made to continue the medication, change the dose, or withdraw it, or possibly introduce some other treatment strategy, such as augmentation with another medication.
A core principle behind the choice of a drug treatment is that its likely benefits, in terms of clinical improvement, should outweigh the risk of adverse effects. Furthermore, this balance should be more favourable than for alternative treatments, whether these be other medications or psychological interventions, or, in the case of a mild disorder, monitoring progress without active treatment. For example, antidepressants are a first-line treatment for moderate and severe major depressive disorder (MDD) in adults but are not recommended for the treatment of short duration, subthreshold depression (i.e. depressive symptoms that do not meet the criteria for DSM-5 major depression) where low-intensity psychosocial and psychological interventions are preferable (Cleare et al., Reference Cleare, Pariante and Young2015). This is because the diagnostic threshold for DSM-5 major depression is an approximate marker for benefit from antidepressant medication over placebo, with the strongest evidence for antidepressant efficacy being when major depression is of at least moderate severity (Cleare et al., Reference Cleare, Pariante and Young2015). However, the adverse effects of antidepressants remain the same irrespective of the severity of the depression. Psychological treatments are less likely to cause adverse effects than antidepressants and have been shown to be effective in subthreshold depression (Cuijpers et al., Reference Cuijpers, Smit and van Straten2007). In summary, the risk–benefit ratio for antidepressant treatment is more favourable for major depression of moderate or greater severity than for short duration, subthreshold depression. The duration of depression, as well as its severity, should be considered when making treatment recommendations. The British Association for Psychopharmacology Guidelines recommend that antidepressant medication should be considered for subthreshold depression that has persisted for more than two to three months and for depression of any severity that has persisted for two years or more (Cleare et al., Reference Cleare, Pariante and Young2015).
Another example, that illustrates the importance of balancing benefit against risk, is the treatment of a moderate depressive episode in a person with epilepsy. In many cases, CBT will be preferred to an antidepressant because of concerns about an increased risk of seizures with such medication (Hill et al., Reference Hill, Coupland and Morriss2015) and possible pharmacokinetic interactions with anticonvulsant medication, whereas CBT carries no such risks but is equally effective for moderate depression (Cleare et al., Reference Cleare, Pariante and Young2015). If the depression were to fail to respond to CBT and/or worsen then the risk–benefit ratio might shift to favouring the prescription of an antidepressant. In such a case, a clinician would be likely to recommend starting treatment with a selective serotonin reuptake inhibitor (SSRI) antidepressant rather than a tricyclic antidepressant (TCA), as SSRIs have a lower liability for causing seizures (Maguire et al., Reference Maguire, Weston, Singh and Marson2014).
Assessing the risk–benefit balance of pharmacological treatment involves the prescriber having a good knowledge of the evidence base for different treatments and also being able to judge the risks of not offering treatment. Box 6.1 summarizes relevant factors that should be considered in making safe prescribing decisions. Ensuring that a medication has a favourable risk–benefit balance for an individual patient also dictates that medication should be withdrawn if it proves to be ineffective after an adequate trial in terms of dose, duration and adherence; it is not good practice to continue an ineffective medication. However, in clinical practice, ineffective medication is sometimes continued, and new medication added, thereby contributing to unnecessary and persistent polypharmacy.
Box 6.1 Factors to consider in making safe prescribing decisions
Patient age
elderly and children/adolescents are more vulnerable to many side effects
in these groups use lower doses and slower titrations.
Is the patient pregnant or likely to become pregnant? If yes:
obtain expert advice
avoid known teratogens (e.g. lithium, valproate, carbamazepine)
choose a drug where there is evidence of safety in pregnancy
consider adverse effects on fetus and newborn other than teratogenesis (e.g. impairment of IQ with valproate)
consider risk to newborn if breastfeeding while maternal prescribing continues
consider risks to mother and unborn child if psychiatric illness is not treated pharmacologically.
Are there coexisting medical disorders? In particular consider:*
cardiovascular disease
epilepsy
renal impairment
hepatic impairment
respiratory disease
gastrointestinal disorders
dementia and cerebrovascular disease.
Is there a potential for drug interactions?*+
with other prescribed medication
with over-the-counter medication
with alcohol
with illicit drugs
with smoking.
Is the patient at risk of overdose?
consider prescribing a less toxic drug
consider dispensing in limited quantities
consider asking a relative to give out medication (if the patient agrees).
Is there a history of drug allergies or serious drug side effects?
if so, avoid the drug or similar drugs.
* Co-morbidity and pharmacodynamic interactions with co-prescribed drugs may increase susceptibility to adverse effects and require dose reduction or avoidance of certain drugs. + Pharmacokinetic interactions with co-prescribed medication may necessitate either dose reduction or dose decrease.
Reproduced with permission from Haddad PM and Wieck A (2016). Prescribing in clinical practice. Chapter 10 in Fundamentals of Clinical Psychopharmacology (editors Ian M Anderson, RH McAllister-Williams), 4th ed. British Association for Psychopharmacology.
6.3 Shared Decision Making and Prescribing
Shared decision making (SDM) has been defined as ‘an approach where clinicians and patients share the best available evidence when faced with the task of making decisions, and where patients are supported to consider options, to achieve informed preferences’ (Elwyn et al., Reference Elwyn, Coulter and Laitner2010). SDM is encouraged and supported in the UK and many other countries, both in mental health and health care in general (National Institute for Health and Care Excellence, NICE, 2011). The justification is partly ethical and partly clinical. SDM respects patient autonomy, a fundamental principle of medical ethics, and this alone warrants its promotion.
While SDM is widely considered to be associated with better clinical outcomes, for example in terms of patient understanding of the disease area, patient satisfaction, symptom reduction and medication adherence, there is only limited evidence to support such positive outcomes. The reality is that SDM is under-researched in both mental health and general medicine. A 2010 Cochrane review of SDM in mental health identified only two randomized controlled trials (RCTs), one conducted in people with schizophrenia and the other in depression (Duncan et al., Reference Duncan, Best and Hagen2010). SDM was associated with greater patient satisfaction in the depression study but no difference was seen in the schizophrenia study. There was no evidence that SDM was associated with harm and the authors highlighted the need for further research. A subsequent study, conducted among patients in community mental health teams, showed that SDM (in this case, involving the use of an electronic decision aid) was associated with greater patient satisfaction with care planning (Woltmann et al., Reference Woltmann, Wilkniss, Teachout, McHugo and Drake2011). A systematic review of RCTs that compared SDM with care as usual in people with mood disorders concluded that SDM was associated with significant improvement in depression outcomes or medication adherence (Samalin et al., Reference Samalin, Genty and Boyer2018).
Where possible, decisions about medication should be made through SDM. The clinician will need to provide the patient with information about their illness and different treatments, answer any questions that the patient may have and address any concerns and misconceptions. Depending on the psychiatric disorder and its severity, the treatment plan may include psychological treatment as an alternative, or adjunct, to drug treatment or the option of no active treatment with a period of ‘watchful waiting’. In practice, the resources available to deliver an evidence-based psychological intervention may be insufficient and waiting lists can be long, which may limit this as a viable treatment choice. The prescriber should try to offer choice from a range of alternative medications. While some patients will wish to follow the prescriber’s recommendation, others will be keen to take a more active role in deciding which medication to take (Paton & Esop, Reference Paton and Esop2005).
As a general rule, individual antidepressants used in the treatment of MDD show little difference in efficacy (Cleare et al., Reference Cleare, Pariante and Young2015). Similarly, in the management of acute schizophrenia, antipsychotics show only minor differences in efficacy (Leucht et al., Reference Leucht, Cipriani and Spineli2013). The only exception is clozapine, which has superior efficacy to other antipsychotics in treatment-resistant schizophrenia and is therefore the treatment of choice for this condition (Siskind et al., Reference Siskind, McCartney, Goldschlager and Kisely2016). Both antidepressant and antipsychotic medications are heterogeneous in their adverse effect profiles (Cleare et al., Reference Cleare, Pariante and Young2015; Leucht et al., Reference Leucht, Cipriani and Spineli2013). For this reason, the relative liability of medications for particular adverse effects and patients’ tolerability of side effects are often major determinants of choice of an antidepressant or antipsychotic medication (Zimmerman et al., Reference Zimmerman, Posternak and Friedman2004). However, individuals vary greatly in their susceptibility to and tolerance of side effects and clinical data on the relative risk of particular side effects across the medications being considered may be incomplete (Pope et al., Reference Pope, Adams, Paton, Weaver and Barnes2010). In some cases, adverse effects may be turned to therapeutic advantage, e.g. when using a sedating antidepressant such as mirtazapine in people whose depression is associated with significant insomnia.
6.4 Acute and Long-Term Drug Treatment
The pharmacological treatment of many psychiatric disorders can be divided into two phases, acute treatment and long-term treatment. However, in clinical practice the distinction between the two phases is often less than clear. Acute treatment refers to the use of medication to treat symptoms of an illness, for example an episode of depression, mania or psychosis. There is no fixed duration for acute treatment and in theory it continues until all acute symptoms have resolved; this is termed remission. If one medication is ineffective in eradicating symptoms it will often be switched to an alternative or combined with a new medication. Despite this, in practice incomplete remission is common and so acute treatment often merges into long-term treatment.
Long-term treatment refers to continuing a drug beyond the point at which acute symptoms have resolved in order to reduce the likelihood of a relapse or recurrence of the underlying psychiatric disorder. The effectiveness of long-term or maintenance treatment in reducing relapse, following successful use of the same drug for acute treatment of an illness, has been demonstrated by meta-analyses of RCTs in various disorders. These include antipsychotic medication in schizophrenia (Leucht et al., Reference Leucht, Tardy and Komossa2012), antidepressants in MDD (Geddes et al., Reference Geddes, Carney and Davies2003) and lithium and several other drugs in bipolar disorder (Miura et al., Reference Miura, Noma and Furukawa2014). Figure 6.1 shows the efficacy of maintenance antipsychotic medication versus placebo in schizophrenia, from the meta-analysis by Leucht et al. (Reference Leucht, Tardy and Komossa2012). The data are from 65 trials (n = 6493) and show that the number needed to benefit in terms of preventing relapse is 3 and to prevent hospitalization is 5. These data also show that there is a ‘cost’ for this benefit. Compared with those study participants assigned to placebo, those treated with antipsychotic medication have a higher risk of adverse effects including movement disorder, weight gain and sedation, as well as being more likely to be prescribed an anticholinergic drug (a proxy for extrapyramidal symptoms).

Figure 6.1 Efficacy of maintenance antipsychotic medication versus placebo in schizophrenia (65 trials, n = 6493).
We have highlighted the distinction between acute and long-term treatment as many patients, their relatives and healthcare professionals who are new to psychiatry may question why a person, who is apparently well, continues to be prescribed medication. Many patients find it difficult to accept the need for long-term medication, especially if they have made a full recovery from an acute episode of illness.
The duration of long-term treatment will be influenced by various factors that include the nature of the underlying psychiatric disorder, the number and severity of previous episodes of illness, whether the person has totally recovered from the last episode or has residual symptoms, the presence of adverse drug effects and the potential impact of a recurrence. Individuals with MDD who have responded to antidepressant treatment are generally recommended to continue antidepressant medication for six to nine months after full remission (Cleare et al., Reference Cleare, Pariante and Young2015). Most schizophrenia treatment guidelines recommend continuing antipsychotic treatment for at least one to two years after the resolution of a first episode of psychosis (Barnes et al., Reference Barnes2011). In both depression and schizophrenia, a longer period of treatment is recommended if there is judged to be a higher risk of relapse, with the duration being tailored to the individual relapse risk.
Decisions on the duration of long-term treatment should be made jointly by the prescriber and the patient. Essentially, the benefits of continuing medication in terms of reducing the risk of relapse need to be weighed against the downsides, which include the inconvenience of taking medication and adverse effects. Given the potentially harmful consequences of relapse, a careful assessment and joint discussion is essential before a decision to withdraw maintenance medication in any disorder is made. As a general rule, medication that has been prescribed long term is best withdrawn gradually and followed by a period of monitoring to facilitate the early detection of relapse. Patients should be aware of the particular signs and symptoms that have characteristically heralded past episodes of relapse and know how to access help urgently if these early signs emerge, their health deteriorates or a crisis develops.
6.5 Off-Label Prescribing
Patients should be treated, whenever possible, with medicines that have an appropriate marketing authorization rather than with off-label or unlicensed medicines. However, off-label medicines and, less commonly, unlicensed medicines may sometimes be necessary to provide the best treatment for patients, although they should only be used if there is a clear clinical justification and relevant evidence of safety and efficacy.
A drug is within licence, or label, when it is prescribed in accordance with the marketing authorization (previously termed a product licence) in the country concerned. The marketing authorization is intended to guarantee the quality, safety and efficacy of the drug and states the clinical indication, dose and route of administration as well as the age group of the patients for whom the drug may be used. It also includes other relevant information, including a list of the known adverse effects. Licensing is the remit of the Medicines and Healthcare products Regulatory Agency (MHRA) in the UK and the Food and Drug Administration (FDA) in the USA. Marketing authorization, or approval, is only granted when a rigorous review of all the relevant data (animal studies and clinical trials) concludes that the benefits of using the drug for a particular indication outweigh the potential risks.
‘Off-label’ prescribing refers to using a drug outside of the terms of its marketing authorization, in relation to the indication, age group, dosage or duration. It also includes unapproved forms of administration, for example crushing a tablet before it is taken. It follows that using a drug outside the terms of its marketing authorization may involve some uncertainty, in that the licensing authority will either not have examined any data on the benefits and risks of using the drug in that way or, if they have, the evidence provided did not meet the requirement for approval. Prescribers can legally prescribe medicines outside the licensing terms with certain caveats but when they do so they take on a greater professional responsibility and liability. In the UK, general guidance on off-label prescribing is provided by the General Medical Council (General Medical Council, 2013). The term ‘near label’ prescribing is sometimes encountered in the literature to refer to a drug being used off-label but in a way that is close to the terms of the licence.
Off-label prescribing needs to be distinguished from the use of an unlicensed drug, i.e. a drug that has no licence for use in the country concerned. This includes the use of drugs that have a licence in another country or have no licence in any country. An example of the latter would be a drug that is in development and still undergoing clinical trials.
Prescribing drugs within label does not guarantee their safety or efficacy. The fact that drugs are occasionally withdrawn from the market due to the identification of serious adverse effects after licensing is the clearest demonstration of this. An example in psychiatry is nomifensine which was first marketed in the UK in 1977 for the treatment of depression. A series of reports of haemolytic anaemia and hepatotoxicity led to its worldwide withdrawal in 1986 (Committee on Safety of Medicines, 1986). Conversely, using a drug off-label does not necessarily imply that treatment is ineffective or unsafe. Off-label prescribing can be appropriate or inappropriate depending on the supporting evidence and clinical circumstances. Where a patient’s condition has failed to respond to all approved treatments (or approved treatment options are contraindicated), then prescribing a drug off-label on the basis of supportive clinical trial evidence may be appropriate. Rigidly adhering to the licence may limit patient choice, reduce the chance of recovery and deny a patient a treatment which is supported by a reasonable evidence base. In contrast, poorly thought out off-label prescribing can be ineffective and dangerous.
Why do marketing authorizations sometimes exclude evidence-based indications for a drug? A drug’s marketing authorization will normally only be extended if the relevant pharmaceutical company makes an application. The application process is expensive and time-consuming, partly because comprehensive data relating to the new indication will be required by the regulator. If existing trials that supported the new indication did not meet the specific requirements of the regulatory authority, new and costly clinical trials would need to be conducted. Further, if a drug were near the end of its patent life, or already available as a generic, financial considerations would mean that a company would be highly unlikely to apply for a revised marketing authorization, even if convincing data for its effectiveness and safety were available.
A recent study examined off-label prescribing of antidepressants in primary care in Canada in adults (Wong et al., Reference Wong, Motulsky and Abrahamowicz2017). Overall, 29% of all antidepressant prescriptions were for an off-label indication. TCAs were the antidepressant class with the highest prevalence of off-label indications (81%). The authors highlighted that these findings largely reflected amitriptyline being prescribed for pain, insomnia and migraine (note: in the UK, some formulations of amitriptyline are licensed to treat neuropathic pain in adults and for migraine prophylaxis in adults). The most frequent use of an off-label antidepressant was trazodone, being prescribed for insomnia and accounting for 26% of all off-label prescriptions. Examining the scientific rationale for this off-label prescribing of antidepressant medications, the researchers concluded that only 16% of all such prescriptions were supported by strong evidence. In 40% of off-label prescriptions, the prescribed drug lacked strong supportive evidence for the indication for which it was prescribed but another antidepressant in the same class had strong evidence for that indication (irrespective of whether on-label or off-label). In the remaining 45% of off-label prescriptions, neither the prescribed antidepressant nor any other antidepressant in its class had robust evidence for efficacy for the clinical indication. An accompanying editorial highlighted that, when it comes to making prescribing decisions, the ‘strength of evidence matters more than presence or absence of a specific licence’ (Morales & Guthrie, Reference Morales and Guthrie2017).
As a general rule, off-label prescribing of psychotropic drugs should only be commenced or recommended by a psychiatrist with appropriate experience. The corollary is that a non-specialist prescriber should ensure that psychiatric drugs are prescribed within the terms of their licence unless there is clear advice to the contrary from an appropriate senior colleague. There should always be an evidence-based rationale to support off-label prescribing and it should be fully discussed with the patient (Baldwin & Kosky, Reference Baldwin and Kosky2007; Royal College of Psychiatrists, 2017). The report by the Royal College of Psychiatrists (2017) on the Use of licensed medicines for unlicensed applications in psychiatric practice recommends that the agreement of the patient to the proposed intervention is recorded and if the patient is ‘unable to provide consent to a necessary treatment, document that it has not been possible to obtain formal consent’. If a medication is used for an off-label indication and subsequently proves ineffective then it should be withdrawn. Similarly, if the off-label use relates to an increase in dosage above the maximum recommended for that disorder in the marketing authorization, and the higher dose confers no additional benefit, then the dose should be reduced so that it is again within the licensed dose range. Marketing authorizations often differ between countries and a drug may have different approved dose ranges for different indications. Licences can change over time. The best source of information on drug indications and doses in the UK is the SPC (Summary of Product Characteristics) for the particular medication. The British National Formulary (BNF) is a useful source of abbreviated information, the data for each drug reflecting that in the SPC.
6.6 Polypharmacy
Polypharmacy refers to prescribing multiple medications for a person at the same time, though beyond this there is no uniformly accepted or more specific definition. A helpful distinction is between polypharmacy that may be considered clinically appropriate and that which may be problematic (Duerden et al., Reference Duerden, Avery and Payne2013). Appropriate polypharmacy occurs when the potential benefits of the co-prescribed medications outweigh their potential harms. It can result from co-morbid conditions, each of which requires medication to be prescribed, or from a single medical disorder that requires several drugs for optimal management. Problematic polypharmacy occurs when the drug combination is inappropriate, for one or more of the following reasons:
There is a lack of robust evidence for the potential risks and benefits of the combination.
The benefits of the combination are outweighed by the risk of harm, including drug interactions.
A drug is being used to treat the side effects of another medication but other solutions exist that would reduce the number of prescribed medications.
The demands of the medication regimen make it unacceptable to the patient.
Prescribed drugs account for most polypharmacy but over-the-counter products, including herbal remedies, can also contribute. Before considering polypharmacy in psychiatry it is helpful to briefly consider polypharmacy in medicine generally. Polypharmacy is common worldwide, is becoming more prevalent and occurs in both primary and secondary care. The greater use of polypharmacy may be partly explained by an ageing population with increasing co-morbidity and the introduction of new medications for conditions that were previously untreatable. While appropriate polypharmacy may improve quality of life and life expectancy, inappropriate polypharmacy can be associated with poor medication adherence, a greater risk of drug interactions and an increased burden of adverse effects, which at their most serious can be fatal (Bourgeois et al., Reference Bourgeois, Shannon and Valim2010; Maher et al., Reference Maher, Hanlon and Hajjar2014). Inappropriate polypharmacy can lead to greater financial costs, partly due to the prescription of unnecessary medication but also due to the costs of treating the resultant medical complications. A final problem with polypharmacy is that it can be difficult for the prescriber to know which of several medications a patient is taking is responsible for any perceived benefit or emergent side effects.
Various attempts have been made to categorize psychiatric polypharmacy, including the following system from the National Association of State Mental Health Program Directors (NASMHPD) (2001):
1. Same-class polypharmacy: this refers to using two or more medications with the same basic pharmacology, e.g. using two benzodiazepine receptor hypnotic drugs to treat insomnia or two SSRIs to treat depression.
2. Multi-class polypharmacy: this refers to using medications from two different pharmacological classes to manage the same symptom cluster, e.g. combining valproate and an antipsychotic to treat mania.
3. Adjunctive polypharmacy: this refers to a medication being used to treat the side effects of a medication from a different class, e.g. an antimuscarinic agent (e.g. procyclidine) is used to treat parkinsonism caused by an antipsychotic drug.
4. Augmentation polypharmacy: this refers to adding a medication from one pharmacological class, sometimes at a lower dose than would be used in monotherapy, to a full therapeutic dose of a drug in another class that has proved only partially effective. The combination aims to treat a single symptom cluster. An example would be adding a serotonin-dopamine antagonist (i.e. second-generation) antipsychotic to an SSRI for the treatment of MDD.
5. Total polypharmacy: this refers to the total number of medications taken by an individual.
This categorization illustrates that psychiatric polypharmacy can arise in different ways. However, the subdivisions proposed above may not always be clear in clinical practice. The authors (NASMHPD, 2001) highlighted that ‘class’ refers to mechanism of action but the categorization of polypharmacy will be very different if this is ignored and drugs are classified by indication. For example, reboxetine and fluoxetine are both traditionally classified as ‘antidepressants’ but have different mechanisms of action, reboxetine is an inhibitor of noradrenaline reuptake and fluoxetine is an inhibitor of serotonin reuptake. The newly proposed Neuroscience-based Nomenclature (NbN) aims to overcome some of the problems inherent in the traditional classification of psychiatric drugs (see Editor’s Note on Nomenclature). Although NbN has much to commend it, the reality is that clinicians are likely to continue to use traditional terminology in some of their work. In practice, the division of polypharmacy into appropriate and inappropriate may have most clinical utility.
Polypharmacy is common in psychiatry. A study of office-based psychiatric practice in the United States showed that in 2005–6 approximately a third of patients were taking three or more medications, a percentage that had nearly doubled over the preceding 10 years (Mojtabai & Olfson, Reference Mojtabai and Olfson2010). Data from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study, the largest randomized trial of antipsychotic treatment in schizophrenia (and also conducted in the United States), showed that for those patients at baseline who were prescribed at least one psychotropic medication, the mean number of psychotropic medications prescribed for each was 2.03 (SD ±1.1): 38% were prescribed antidepressant medications, 22% anxiolytics, 4% lithium and 15% other mood stabilizers, while 6% were prescribed two antipsychotics (Chakos et al., Reference Chakos, Glick and Miller2006). Psychiatric polypharmacy has been found to be more commonly prescribed for men than women and for those with a diagnosis of schizophrenia (De las Cuevas & Sanz, Reference De las Cuevas and Sanz2004).
Several practical steps can help reduce inappropriate polypharmacy (see Box 6.2). Medicine management, also termed medicines optimization, centres on improving medication use, one aspect of which is reducing inappropriate polypharmacy.
Box 6.2 Some practical strategies to help reduce inappropriate polypharmacy
Consider whether non-pharmacological treatments (e.g. cognitive behavioural treatment) may be more appropriate than adding a new drug.
Explore adherence to current medication before increasing dosages or adding new drugs.
Be clear on the goals of treatment before medication is started
record the treatment targets clearly to assist future reviews especially if these will be by other healthcare professionals
review treatment targets periodically and stop medication if it proves to be ineffective.
Consider drug interactions when adding a new medication.
Keep medication regimens simple, ideally medication to be taken once or twice daily.
Try to substitute rather than add medicines.
Ask patients about over-the-counter products they may be taking including herbal remedies.
Review medication regimens regularly especially in patients with long-term co-morbid conditions.
Involve patients in prescribing decisions and medication reviews.
6.7 Managing Adverse Effects and Drug Interactions
The adverse effects of medication are clinically important as they can cause suffering, impair quality of life, stigmatize patients and lead to poor adherence to medication, which may result in a relapse of the underlying psychiatric disorder (Haddad & Sharma, Reference Haddad and Sharma2007). In some cases, they may also confound the clinical assessment of the psychiatric illness. Minimizing adverse effects involves several steps: (i) discussing potential adverse effects with the patient prior to commencing medication; (ii) avoiding excessive doses; (iii) considering the potential for drug interactions; (iv) systematically screening for adverse effects during treatment; and (v) appropriately managing adverse effects when they occur.
Discussing potential adverse effects with patients prior to starting treatment is important for several reasons. Talking about the relative liability for adverse effects of the possible medications is an important part of SDM and medication choice. If a person is prone to develop a certain adverse effect then a drug with a lower risk of causing that problem can be selected. Furthermore, patients who have been warned about potential adverse effects are less likely to unilaterally stop a medication if they subsequently develop an adverse effect they have been informed about. Their trust and confidence in the prescriber are likely to be increased.
While most psychiatric drugs have a therapeutic dose range, the dose within this range at which an individual will respond may be difficult if not impossible to predict. Many adverse effects become more frequent and severe as the dosage is increased. Tolerance for some adverse effects can develop over a period of days or weeks and in some cases a slow increase in dose initially can reduce their severity and frequency. As a general rule, doses should be increased gradually, especially in the elderly who are more prone to adverse effects for a variety of pharmacological and physiological reasons (see Chapter 18). Most antidepressants, other than TCAs, and most antipsychotics can be started at a therapeutic dose, though there are exceptions. For example, the SPC recommends that quetiapine immediate release is started at a subtherapeutic dose in the treatment of schizophrenia before being titrated to a therapeutic dose. Similarly, clozapine needs to be gradually titrated to a therapeutic dose. Although a licence may permit a drug to be commenced at a therapeutic dose, it is sometimes advisable to start at a subtherapeutic dose when treating patients who are judged to be more prone to adverse effects. Examples include patients with a history of poor tolerance to the class of drug that is to be used, the elderly, children, and those with hepatic or renal impairment or who are taking other drugs with which there is a potential interaction. However, it is important that this principle does not inadvertently result in a patient being left permanently on a subtherapeutic dose of medication.
To avoid potentially serious drug interactions, history taking should include documenting all currently prescribed and over-the-counter medications (including herbal remedies). Drug interactions may be due to pharmacokinetic or pharmacodynamic interactions. Examples of drugs used in psychiatry where there are well-documented and potentially serious drug interactions include the following (please note that this list is not extensive and merely describes a few examples):
Lithium: Lithium has a narrow therapeutic index. Consequently, drugs that interact pharmacokinetically to elevate the serum level of lithium, even to a minor degree, can lead to lithium toxicity. Examples of such drugs are non-steroidal anti-inflammatory drugs (NSAIDs), thiazide diuretics, loop diuretics, angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor antagonists (Finley, Reference Finley2016).
Serotonergic antidepressants: If two drugs that increase serotonergic transmission in the central nervous system are co-prescribed, especially if they increase serotonin transmission through different mechanisms, there is a risk of serotonin toxicity. This occurs on a spectrum of severity and at its gravest can be life-threatening. Most serious cases of serotonin toxicity involving antidepressants have occurred when monoamine oxidase inhibitors (MOAIs) have been co-prescribed with another serotonergic medication.
Lamotrigine: There are a range of potential drug interactions with lamotrigine. Focusing on the interaction between lamotrigine and valproate, if these two medications are co-prescribed, lamotrigine plasma levels may be elevated because of inhibition of its metabolism (glucuronidation) by valproate. Lamotrigine can cause skin reactions especially early in treatment. These vary in severity but at their most serious include Stevens–Johnson syndrome and toxic epidermal necrolysis which are potentially life-threatening. The risk of skin rashes is much higher when the dose of lamotrigine is escalated more rapidly than the drug licence dictates. When lamotrigine is started in a patient who is already prescribed valproate, it is recommended that the starting dose for lamotrigine is lower, the dose is increased more gradually and the final recommended target dose is lower than it would be for a patient not taking valproate.
After a new drug is initiated, the clinician should enquire about adverse effects rather than simply waiting for the patient to volunteer information. However, the answers to simple questions to a patient about how their medication is suiting them or if they have noticed any problems are likely to underestimate the extent of their side effects (Yusufi et al., Reference Yusufi, Mukherjee and Flanagan2007). Patients may not report adverse effects for a variety of reasons; for example, they may not have attributed them to medication or may be reluctant to discuss problems they find embarrassing. For a patient prescribed antipsychotic medication, the use of a comprehensive rating scale, such as the Antipsychotic Non-Neurological Side Effects Rating Scale (ANNSERS) (Ohlsen et al., Reference Ohlsen, Williamson and Yusufi2008), administered with sensitive and systematic questioning is perhaps the only way to determine a patient’s full side-effect burden. Several patient-completed checklists and/or rating scales are also available to aid detection of adverse effects, depending on the medication that is prescribed. An example is the Glasgow Antipsychotics Adverse-effect Scale (GASS) (Waddell & Taylor, Reference Waddell and Taylor2008). A patient can complete this before a consultation and it can form the basis for a discussion with the clinician. The discussion is essential as what is recorded on a patient-completed checklist/rating scale as an apparent adverse effect may have another cause including being a symptom of psychiatric illness or a concurrent medical disorder. Even if it is an adverse effect, discussion will be necessary in those prescribed more than one medication to identify which drug is most likely to be responsible.
Assessment of potential adverse effects may require physical examination and appropriate blood tests in addition to taking a history. For example, monitoring of weight and fasting serum lipids and glucose is recommended during treatment with antipsychotic medication given the risk of associated weight gain and metabolic abnormalities. With lithium, serial assessment of renal and thyroid function is required (lithium can cause thyroid and renal impairment) as well as monitoring of the serum lithium level, given lithium’s low therapeutic index.
If adverse effects are detected, their consequences for the patient should be explored and options for treatment should be discussed. These will depend on the nature and severity of the adverse effect, whether it is likely to be transient or persistent, its impact on the patient and the results of a careful assessment of both the benefits and drawbacks of the current medication versus alternatives. Some adverse effects may be managed by simple lifestyle changes (e.g. sipping water if an antidepressant causes a dry mouth) but some may require a dose reduction or switch of medication. Management may be aided by the time course of the adverse effect in relation to prescribing. Some adverse effects, for example nausea with SSRIs and serotonin and noradrenaline reuptake inhibitors (SNRIs), are usually transient and spontaneously resolve over the first few weeks of treatment (Demyttenaere et al., Reference Demyttenaere, Albert and Mesters2005; Greist et al., Reference Greist, McNamara, Mallinckrodt, Rayamajhi and Raskin2004). Some adverse effects, for example sexual dysfunction with antidepressants, tend to persist, while others tend to become more marked with time, for example weight gain with antipsychotic medication (Bushe et al., Reference Bushe, Slooff, Haddad and Karagianis2012).
6.8 Medication Adherence
Medication adherence can be defined as the extent to which a patient’s medication taking matches that agreed with the prescriber. Poor medication adherence is a common problem in all chronic conditions, both psychiatric and physical. A comprehensive literature review reported that the mean amount of prescribed medication taken was 58% for antipsychotics, 65% for antidepressants and 76% for a range of medications prescribed for physical disorders (Cramer & Rosenheck, Reference Cramer and Rosenheck1998). Adherence is influenced by multiple patient, clinician, illness, medication and service factors (Figure 6.2). Non-adherence is a particular challenge in schizophrenia due to the impact of positive and negative symptoms, lack of insight, depression and cognitive impairment, as well as the association between the illness and social isolation, stigma and co-morbid substance use (Haddad et al., Reference Haddad, Brain and Scott2014). A useful distinction is between intentional and unintentional non-adherence though both can occur simultaneously in the same person. Intentional non-adherence is when a patient decides not to take their medication as prescribed, usually because they perceive its disadvantages as outweighing its benefits. Unintentional non-adherence occurs when practical problems interfere with medication taking, for example a person does not understand the instructions that they were given about taking their medication or forgets to take it.
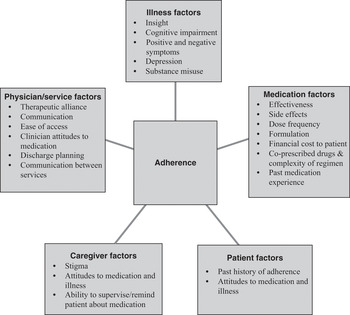
Figure 6.2 Factors associated with adherence. This figure has been adapted from Haddad PM et al. (Reference Haddad, Brain and Scott2014), Patient Related Outcome Measures, 5, 43–62.
Non-adherence leads to poorer clinical outcomes. Observational studies demonstrate a strong association between poor medication adherence and relapse and rehospitalization in schizophrenia (Novick et al., Reference Novick, Haro and Suarez2010) and in bipolar disorder (Hong et al., Reference Hong, Reed and Novick2011). As non-adherence is often covert (i.e. unrecognized by the prescriber) it is a common reason for an apparently poor response to medication. Thus, covert non-adherence may lead to inappropriate prescribing decisions such as a dose increase, switching or augmentation. Non-adherence has significant economic implications, especially in terms of increased inpatient costs, in both schizophrenia and bipolar disorder (Dilla et al., Reference Dilla, Ciudad and Alvarez2013; Hong et al., Reference Hong, Reed and Novick2011; Knapp et al., Reference Knapp, King, Pugner and Lapuerta2004). Figure 6.3 summarizes the potential consequences of nonadherence to antipsychotic medication in schizophrenia.

Figure 6.3 Consequences of non-adherence to antipsychotic medication in schizophrenia. Reproduced from Haddad P, Lambert T and Lauriello J (Reference Haddad, Lambert, Lauriello, Haddad, Lambert and Lauriell2016). The role of antipsychotic long-acting injections in clinical practice. Chapter 15 in Antipsychotic Long-Acting Injections (editors P Haddad, T Lambert and J Lauriello), 2nd ed. Oxford University Press.
Before a new medication is prescribed, the prescriber needs to try to understand the patient’s beliefs and concerns about their illness and medication so that potential barriers to adherence can be identified and tackled (NICE, 2009). This will involve providing the patient with information about their illness and treatment. Adherence is likely to be improved by some of the principles of good practice already discussed in this chapter, including SDM when choosing medication, adverse effect monitoring and the avoidance of unnecessary polypharmacy. Other generic strategies to enhance adherence include keeping the medication regimen simple and maintaining a positive therapeutic alliance between the prescriber and patient. Medication adherence should be enquired about, in a non-judgemental way, whenever the patient is seen.
When non-adherence is identified its causes should be explored and addressed, for example, managing adverse effects, enhancing efficacy and countering misperceptions associated with the medication and the underlying illness. More specific approaches to tackle non-adherence include psychosocial interventions, service interventions (e.g. intensive case management), electronic reminders, financial incentives and in the case of antipsychotics switching from an oral to a depot/LAI preparation. Sometimes several interventions will need to be combined. It is crucial that interventions are tailored to the individual patient and chosen in collaboration with them. In the rest of this section we review some strategies that have been used to improve antipsychotic adherence in schizophrenia.
Psychosocial interventions to improve medication adherence in schizophrenia include adherence therapy, behavioural interventions, cognitive adaptation training (CAT), motivational interviewing and psychoeducation. The distinction between these interventions is not absolute and studies have often combined elements of several models. Psychoeducation programmes are more effective in improving adherence when the focus is on adherence and environmental or behavioural interventions are included (Barkhof et al., Reference Barkhof, Meijer, de Sonneville, Linszen and de Haan2012).
Adherence or compliance therapy utilizes motivational interviewing, psychoeducation and cognitive behavioural approaches to highlight the benefits of treatment to an individual, modify their illness and treatment beliefs, and resolve ambivalence towards medication. Many of the elements build on what would be regarded as good practice when discussing antipsychotic medication with a patient. However, a systematic review of four trials of adherence therapy failed to show an improvement in antipsychotic adherence compared with treatment as usual or a control intervention (Hegedüs & Kozel, Reference Hegedüs and Kozel2014), leading to guideline recommendations that it should not be used (Barnes et al., Reference Barnes2011; NICE, 2014). In the studies reviewed by Hegedüs and Kozel (Reference Hegedüs and Kozel2014) baseline adherence was high, which may create a ceiling effect, i.e. it is difficult for such studies to demonstrate an improvement. The findings of a subsequent meta-analysis of six studies of adherence therapy in schizophrenia spectrum disorders suggested that although there was no significant effect on medication adherence, the intervention was associated with a significant reduction in psychiatric symptoms compared to treatment as usual (Gray et al., Reference Gray, Bressington and Ivanecka2016).
One of the main advantages of LAI antipsychotic preparations is that they make antipsychotic adherence transparent. There is increasing evidence that LAIs can improve outcomes in schizophrenia compared with oral antipsychotic medication (OAPs) though this derives largely from observational studies rather than RCTs. In the most recent meta-analysis of RCTs, pooled LAIs did not reduce relapse compared with OAPs in people with schizophrenia (Kishimoto et al., Reference Kishimoto, Robenzadeh and Leucht2014). This may partly reflect selective recruitment of adherent patients into RCTs plus the design of RCTs distorting the ecology of treatment as used in clinical practice. Since this meta-analysis was conducted, the results of three RCTs, with designs that better reflect real-world practice, have been published and each showed superiority of LAIs to OAPs (Alphs et al., Reference Alphs, Mao, Rodriguez, Hulihan and Starr2014; Schreiner et al., 2015; Subotnik et al., Reference Subotnik, Casaus and Ventura2015). It is notable that two of the three trials recruited people early in the course of schizophrenia (Alphs et al., Reference Alphs, Mao, Rodriguez, Hulihan and Starr2014; Subotnik et al., Reference Subotnik, Casaus and Ventura2015).
Observational studies have the advantage of studying patients that are representative of clinical practice and include mirror-image studies and parallel group cohort studies. A meta-analysis of mirror-image studies showed reduced hospitalization with LAIs compared with prior use of oral antipsychotics (Kishimoto et al., Reference Kishimoto, Nitta, Borenstein, Kane and Correll2013). Cohort studies are methodologically stronger than mirror-image studies. A database study of all adult patients in Sweden with a schizophrenia diagnosis assessed the risk of rehospitalization and treatment failure (i.e. psychiatric rehospitalization, suicide attempt, stopping or switching medication, or death) for various antipsychotic medications (Tiihonen et al., Reference Tiihonen, Mittendorfer-Rutz and Majak2017). The highest rates of relapse prevention were seen with LAI antipsychotics and clozapine. Compared with equivalent oral formulations, LAIs were associated with a 20% to 30% lower risk of rehospitalization.
A meta-analysis of retrospective and prospective cohort studies showed that LAIs were superior to OAPs for hospitalization rate, i.e. number of hospitalizations per person-year (Kishimoto et al., Reference Kishimoto, Hagi and Nitta2018). There was no significant difference between treatment with LAIs and OAPs for hospitalization risk (i.e. proportion of patients experiencing ≥1 hospitalizations) and total hospital days. Interpreting these findings should take account of the naturalistic treatment selection (indication bias) and that illness severity/chronicity was greater for those treated with LAIs compared with OAPs. Furthermore, the impact of LAIs on the hospitalization rate may not be due to better adherence; patients prescribed a LAI antipsychotic will usually have more clinical contact (from the healthcare professional administering the injections) than those on oral medication, and therefore potentially greater support, more regular review of mental state and side effects and enhanced adherence monitoring. Nevertheless, the authors’ overall conclusion was that LAIs were superior to OAPs (Kishimoto et al., Reference Kishimoto, Hagi and Nitta2018).
The NICE schizophrenia guideline (NICE, 2014) recommends considering a LAI antipsychotic for people with schizophrenia who would prefer such a treatment after an acute episode or where avoiding covert non-adherence (either intentional or unintentional) to antipsychotic medication is a clinical priority.
Electronic reminders have been used to improve medication adherence in several illness areas. A systematic review of electronic reminders to improve patients’ adherence with long-term medication in physical health disorders identified 13 controlled studies that used short message service (SMS) reminders, audio-visual reminders or pager messages (Vervolet et al., Reference Vervloet, Linn and van Weert2012). It found evidence for the short-term effectiveness of all three electronic reminders, especially SMS reminders, but the authors highlighted that their long-term effectiveness was unknown. In a study by Montes et al. (Reference Montes, Medina, Gomez-Beneyto and Maurino2012), SMS reminders improved patient-rated adherence to antipsychotic medication compared with a control group, over a three-month period. Although not widely used at present, electronic medication dispensers can be wirelessly linked to a central server to allow real-time electronic medication monitoring for individual patients. The dispensers register when a daily medication compartment is opened and convey this information wirelessly to a server. This can be programmed to allow various interventions, e.g. sending a ‘medication reminder’ text message to the patient if the dispenser is not opened within a specified time frame or alerting staff (Velligan et al., Reference Velligan, Mintz and Maples2013).
In 2017 the FDA approved aripiprazole tablets with an embedded Ingestible Event Marker or ‘sensor’ (‘Abilify MyCite’) (Otsuka America Pharmaceutical, 2018). Following ingestion of the tablet, the sensor is activated by gastric acid and transmits a signal to a skin patch monitor worn by the patient. The skin patch monitor records the date and time of ingestion and the patient’s rest and activity level and transfers the data wirelessly to an application (app) on the patient’s smartphone which in turn relays it to a secure web-based portal (the ‘dashboard’). This ‘dashboard’ allows healthcare professionals, with the patient’s consent, to monitor the data including that on medication ingestion. The patient can view their data on their smartphone app and scroll through information for past months. The final design of this digital medicine system (DMS) incorporated feedback from patients and healthcare professionals (Peters-Strickland et al., Reference Peters-Strickland, Hatch, Adenwala, Atkinson and Bartfeld2018). The acceptability and effectiveness of the system, and whether it improves adherence and clinical outcomes, in real-world practice remains to be determined. The ingestible sensor can be embedded within most tablets. Outside of psychiatry, small feasibility studies have assessed this technology in patients with various disorders including hypertension, heart failure and tuberculosis (Au-Yeung et al., Reference Au-Yeung, Moon and Robertson2011; Belknap et al., Reference Belknap, Weis and Brookens2013).
One RCT has investigated financial incentives to improve adherence with LAI antipsychotic medication (Priebe et al., Reference Priebe, Yeeles and Bremner2013). The study was conducted in the UK and recruited patients prescribed LAIs who had shown poor adherence in the preceding year. Over the one-year trial period, the intervention group, who received £15 (€17; $22) per LAI administered, had significantly better adherence to the LAI and better patient-rated quality of life than the control group who received treatment as usual. However, the two groups did not differ in terms of clinician ratings of clinical improvement. When the trial ended, and the incentive stopped being paid, adherence returned to approximately baseline level (Priebe et al., 2016). The finding that a modest financial incentive can improve adherence to LAI antipsychotics is consistent with studies that show that financial incentives can improve medication adherence in general medicine as well as improve health behaviours in a range of areas, for example reducing the use of alcohol and illicit drugs, decreasing smoking and assisting weight loss (Petry et al., Reference Petry, Rash, Byrne, Ashraf and White2012). However, despite a growing evidence base, the use of financial incentives in health care is controversial and raises ethical and logistical issues (Petry et al., Reference Petry, Rash, Byrne, Ashraf and White2012).
6.9 Role of Audit as a Tool to Enhance Good Practice
Clinical audit can be an effective tool to improve the quality of prescribing in psychiatric services (Paton & Barnes, Reference Paton and Barnes2014) and has been defined as a ‘quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change’ (NICE, 2002). The collection and feedback of data relevant to the performance of clinicians and clinical teams against evidence-based practice standards can stimulate and support reflection on actual clinical practice. In an organization with a supportive, quality-improvement culture, this can then spur the implementation of change interventions and subsequent monitoring for continuing improvement. A range of change interventions may be considered; these may be implemented at an organizational level, targeted at clinicians (provision of educational material, reminders and knowledge support tools) or targeted at patients (educational materials). Barriers to such behavioural change may best be overcome with multifaceted interventions (Robertson & Jochelson, Reference Priebe, Bremner and Pavlickova2006).
A standard in this context may be considered as a ‘definable measure against which existing structures, processes or outcomes can be compared’ (National Clinical Effectiveness Committee, 2015). The practice standards derived for clinical audit should be recognized by the clinicians taking part as defining optimal prescribing practice, being universally applicable, and realistic to achieve in routine care. They commonly relate to the quality of pretreatment screening and monitoring and review of continuing treatment.
The audit data collected will focus on measures of compliance with the practice standards. But other contextual data should be collected to provide some indication of the organizational, administrative and clinical factors that may be associated with variation in clinical performance and thus inform the change interventions. Clinicians’ interpretation of the audit findings relating to their own clinical service may be enhanced by providing benchmarked performance data, allowing comparison with other, similar services. For local clinical audit, this may involve benchmarked data across clinical teams. For national, audit-based quality improvement programmes like those run by the Prescribing Observatory for Mental Health (POMH-UK; Barnes & Paton, Reference Barnes and Paton2012), use of a standard data collection tool by all the participating clinical services allows for local performance to be compared with equivalent data on performance from other services nationally. Topics addressed by POMH-UK quality improvement programmes tend to focus on discrete, defined aspects of prescribing practice, and have included high-dose and combined antipsychotic medication (Paton et al., Reference Paton, Barnes, Cavanagh and Taylor2008), screening for the metabolic side effects of antipsychotic medication (Barnes et al., Reference Barnes, Bhatti, Adroer and Paton2015), monitoring of lithium treatment (Paton et al., Reference Paton, Adroer and Barnes2013), prescribing valproate for bipolar disorder (Paton et al., Reference Paton, Cookson and Ferrier2018) and the pharmacological management of acute behavioural disturbance, including rapid tranquillisation (Paton et al., Reference Paton, Adams and Dye2019).