Introduction
Health authorities and governments worldwide address older adults as a risk group for facing more serious and possibly fatal illness associated with SARS-CoV-2 (COVID-19) (Brooke and Jackson, Reference Brooke and Jackson2020). Worldwide, governments are warning people at high risk of infection and severe progression of the disease to be particularly strict in following social distancing measures, as evidence grows that older adults are more likely to need critical care or to experience a fatal outcome in case of an infection (Fuellen et al., Reference Fuellen, Liesenfeld, Kowald, Barrantes, Bastian, Simm, Jansen, Tietz-Latza, Quandt, Franceschi and Walter2020; Jordan et al., Reference Jordan, Adab and Cheng2020; Wang et al., Reference Wang, Pan, Zhang, Han, Fan, Zhao, Miao, Xu, Guan, Deng, Chen and Shen2020). Recent studies have concluded that old age is significantly associated with a higher probability of COVID-19-related death (Bezzio et al., Reference Bezzio, Saibeni, Variola, Allocca, Massari, Gerardi, Casini, Ricci, Zingone, Amato, Caprioli, Lenti, Viganò, Ascolani, Bossa, Castiglione, Cortelezzi, Grossi, Milla, Morganti, Pastorelli, Ribaldone, Sartini, Soriano, Manes, Danese, Fantini, Armuzzi, Daperno and Fiorino2020) and showed that, after controlling for background variables, age and the number of chronic underlying diseases were risk factors of more severe illness (Dong et al., Reference Dong, Li, Bai, Liu, Zhou, Gao, Li and Zhang2020).
Indeed, the overall mortality of older adults during the COVID-19 pandemic has been striking so far (Shahid et al., Reference Shahid, Kalayanamitra, McClafferty, Kepko, Ramgobin, Patel, Aggarwal, Vunnam, Sahu, Bhatt, Jones, Golamari and Jain2020): in Austria, where the present study is based, 75 per cent of COVID-19-related deaths occurred in adults over the age of 75. In Germany, 86 per cent of total deaths caused by COVID-19 were among people over 70 years old (Robert Koch-Institut, 2020) and in Europe, people over the age of 65 account for 90 per cent of the total COVID-19-related deaths (World Health Organization, 2020). There is overwhelming evidence suggesting that older adults bear a higher risk of COVID-19 infection and fatal outcome associated with it, which is one reason why older age groups have been framed as a COVID-19 risk group throughout the pandemic.
In addition to these medical risks that have been placed on older adults during the pandemic, research in social gerontology has raised significant concerns about age-based categorisations of SARS-CoV-2 risk groups and their social and psychological effects on older adults, arguing that while it might help to protect older age groups from COVID-19 infection, classifying older adults as a risk group for coronavirus disease bears the risk of reinforcing ageism and negative images of ageing (Ayalon et al., Reference Ayalon, Chasteen, Diehl, Levy, Neupert, Rothermund, Tesch-Römer and Wahl2020; Colenda et al., Reference Colenda, Reynolds, Applegate, Sloane, Zimmerman, Newman, Meeks and Ouslander2020; Jimenez-Sotomayor et al., Reference Jimenez-Sotomayor, Gomez-Moreno and Soto-Perez-de-Celis2020; Monahan et al., Reference Monahan, Macdonald, Lytle, Apriceno and Levy2020; Rahman and Jahan, Reference Rahman and Jahan2020). Ageism, the ‘stereotyping, prejudice, and discrimination against people on the basis of their age’ (Officer et al., Reference Officer, Schneiders, Wu, Nash, Thiyagarajan and Beard2016: 710), might become more visible during the COVID-19 pandemic, as older people are represented in the current public discourse surrounding the pandemic as a homogenous and vulnerable group that is in need of care and protection (Fraser et al., Reference Fraser, Lagacé, Bongué, Ndeye, Guyot, Bechard, Garcia, Taler, Adam, Beaulieu, Bergeron, Boudjemadi, Desmette, Donizzetti, Éthier, Garon, Gillis, Levasseur, Lortie-lussier, Marier, Robitaille, Sawchuk, Lafontaine and Tougas2020).
Indeed, as one of the first empirical studies on the topic, the study on tweets related to age and ageing during COVID-19 found that a quarter of the tweets analysed included ageist and potentially offensive content towards older adults (Jimenez-Sotomayor et al., Reference Jimenez-Sotomayor, Gomez-Moreno and Soto-Perez-de-Celis2020). A study on newspaper coverage of the pandemic in three different countries showed that despite divergent policies in different countries, ageism in response to the COVID-19 pandemic took similar forms and included name-calling of older adults, blame, and ‘so-be-it’ reactions when ageing was discussed (Lichtenstein, Reference Lichtenstein2020). Many social gerontologists have therefore argued that addressing older adults as a COVID-19 risk group and related policies lead to an increased prevalence of ageism in society, contribute to the diffusion of negative images of ageing that position old age as a vulnerable and risky stage of life, and connect concepts of insecurity, instability and risk to images of later life and ageing (Ayalon et al., Reference Ayalon, Chasteen, Diehl, Levy, Neupert, Rothermund, Tesch-Römer and Wahl2020; D'cruz and Banerjee, Reference D'cruz and Banerjee2020; Fraser et al., Reference Fraser, Lagacé, Bongué, Ndeye, Guyot, Bechard, Garcia, Taler, Adam, Beaulieu, Bergeron, Boudjemadi, Desmette, Donizzetti, Éthier, Garon, Gillis, Levasseur, Lortie-lussier, Marier, Robitaille, Sawchuk, Lafontaine and Tougas2020; Klusmann and Kornadt, Reference Klusmann and Kornadt2020; Monahan et al., Reference Monahan, Macdonald, Lytle, Apriceno and Levy2020).
However, even though there is considerable debate in the literature on the manifold social and psychological challenges of the COVID-19 pandemic that have been imposed upon older adults, there is hardly any evidence on how older adults perceive and negotiate COVID-19-related risk in their everyday lives and which consequences this has for their images of age and ageing. It is such a perspective on the subjective experiences of older adults during the COVID-19 pandemic and its related risks that this paper uses as its starting point. It adds to current debates by exploring how feeling at risk of severe illness associated with COVID-19 influences the daily lives of older adults and influences their perceptions, experiences and images of ageing. In doing so, the study contributes to the scholarly discourse about the role of ageism during the COVID-19 pandemic.
Older adults as a COVID-19 risk group
While previous research as well as commentaries from the field of social gerontology have provided arguments as well as some empirical evidence on the social effects that perceived COVID-19 risk has on older adults, significant gaps in the literature remain. First, while scientific commentaries have widely noted that classifying older adults as a COVID-19 risk group based on chronological age potentially reinforces ageism (Ayalon et al., Reference Ayalon, Chasteen, Diehl, Levy, Neupert, Rothermund, Tesch-Römer and Wahl2020; Fraser et al., Reference Fraser, Lagacé, Bongué, Ndeye, Guyot, Bechard, Garcia, Taler, Adam, Beaulieu, Bergeron, Boudjemadi, Desmette, Donizzetti, Éthier, Garon, Gillis, Levasseur, Lortie-lussier, Marier, Robitaille, Sawchuk, Lafontaine and Tougas2020; Rahman and Jahan, Reference Rahman and Jahan2020), there is a significant lack of evidence on how such ageist assumptions and language affect older adults and how they relate to subjective images of ageing. This implies the necessity for studies that empirically focus on how older adults perceive and negotiate COVID-19-related risk and how it relates to their experiences of age and ageing. Levy (Reference Levy2009) has shown that negative age stereotypes, including images and attitudes of ageing (e.g. the hashtag #boomerremover that has surfaced in social media during the pandemic; Monahan et al., Reference Monahan, Macdonald, Lytle, Apriceno and Levy2020) have negative consequences for older adults' cognition, emotion and physical status. In line with stereotype embodiment theory, this suggests that negative stereotypes and the age-based assessment of COVID-19-related risk might result in the unconscious endorsement of negative age stereotypes in older adults, fuelling negative self-images and attitudes towards ageing. Studies on loneliness of older adults during the COVID-19 pandemic have found that older adults with more negative subjective ageing experiences are more likely to experience feelings of loneliness during the pandemic (Shrira et al., Reference Shrira, Hoffman, Bodner and Palgi2020). However, more empirical evidence is needed to understand the relationship between perceived COVID-19-related risk and subjective images and experience of ageing in older adults.
Second, research has criticised that addressing older adults as a COVID-19 risk group draws upon an unjustified homogenisation of higher age groups and underestimates the heterogeneity of older adults (Ehni and Wahl, Reference Ehni and Wahl2020; Rahman and Jahan, Reference Rahman and Jahan2020). There is currently hardly any evidence on how older adults in different social positions (e.g. with regard to education, class, race and/or gender) perceive COVID-19-related risk differently. Research before the COVID-19 crisis has shown that negative images towards ageing and internal ageism highly depend on socio-economic variables, including education (Nunes et al., Reference Nunes, Menéndez, Martins and Martins2018), gender (Bodner et al., Reference Bodner, Bergman and Cohen-Fridel2012; Smith et al., Reference Smith, Bergeron, Cowart, Ahn, Towne, Ory, Menn and Chaney2016), age (Bodner et al., Reference Bodner, Bergman and Cohen-Fridel2012) and ethnicity (Smith et al., Reference Smith, Bergeron, Cowart, Ahn, Towne, Ory, Menn and Chaney2016). First empirical studies on loneliness during the COVID-19 pandemic revealed that especially women and lower-income individuals experienced increased levels of loneliness during the pandemic (Seifert and Hassler, Reference Seifert and Hassler2020). Hebblethwaite et al. (Reference Hebblethwaite, Youn and Martin Rubio2020) argue that the marginalisation of older adults during the COVID-19 pandemic might be especially prevalent for those who are already marginalised in Western societies. This necessitates research on how social differences and social position shape the experience of COVID-19-related risk in older adults and its associations with perceptions of age and ageing.
Third, while research has so far focused on the effects that age-based categorisations have on ageism and images of ageing in a society, there is a lack of broader conceptual reflection that situates the age-based categorisation of COVID-19-related risks into larger debates within gerontology and the sociology of ageing outside the ongoing pandemic. Before the discussion surrounding COVID-19 risk groups surfaced during the pandemic, cultural ageing studies and critical gerontology have introduced the term precarious ageing (Grenier et al., Reference Grenier, Phillipson, Rudman, Hatzifilalithis, Kobayashi and Marier2017, Reference Grenier, Hatzifilalithis, Laliberte-Rudman, Kobayashi, Marier and Phillipson2019) to understand how risks and insecurities influence and shape later life. Such studies put forward an understanding of precarity that situates it as an ontological condition (Butler, Reference Butler2009; Grenier et al., Reference Grenier, Phillipson, Settersten, Grenier, Phillipson and Settersten2020) and understands the vulnerability of an ageing body as an expression of precariousness (as adults experience biological decline in later life), and precarity (as older adults – also those without health limitations – are addressed and depicted as a group at high of risk of being frail). From such a perspective, it is argued that even though an ageing body is biologically vulnerable to COVID-19, due to chronic illness or general health decline in later life, older adults are also socially made vulnerable, or ‘vulnerableized’ (Hebblethwaite et al., Reference Hebblethwaite, Youn and Martin Rubio2020: 171), by systematic, institutional and cultural circumstances, such as age-based categorisations of COVID-19 risk groups and its related policies and media discourses. From this perspective, we can question whether addressing older adults as a risk group of COVID-19 can be understood as a process of vulnerablising age and ageing – a process of creating the lived experience of vulnerability in later life through systematic, institutional and cultural circumstances.
In this paper, we aim to explore how the categorisation of older adults as a COVID-19 risk group unfolds its meaning in the everyday lives of older adults, how social position influences these dynamics and which consequences such categorisations have for the experience of old age as a precarious stage of life. This paper therefore asks:
RQ1: To what extent do older adults perceive themselves as being at risk due to COVID-19?
RQ2: Which differences exist in subjective risk perception due to COVID-19 within the older population?
RQ3: How do older adults negotiate these perceived risks in their everyday lives and how do they influence their images of ageing?
Methods
This paper draws upon data from a mixed-methods study on older adults' subjective risk perception during the COVID-19 pandemic. Data collection and analysis followed a parallel mixed-methods design (Kuckartz, Reference Kuckartz2014) that combined quantitative and qualitative methods.
Study design
First, this paper uses quantitative data from a standardised, representative telephone survey with 521 residents of Lower Austria aged 60 and older, which was conducted between 30 April and 8 May 2020, a time when extensive social distancing measures were in place in Austria (Pollak et al., Reference Pollak, Kowarz and Partheymüller2020). Second, this paper draws upon qualitative data from 20 semi-structured interviews that were conducted with older adults (60+ years) living in Lower Austria in May 2020. The interviews were conducted seven to ten weeks after the COVID-19 social distancing measures came into effect in Austria. Qualitative analysis aimed at exploring reasons for older adults' subjective risk perception as well as the influence of perceived risks during COVID-19 on their everyday lives and images of ageing. As interviews were carried out while social distancing measures were in place in Austria, semi-structured interviews were chosen for data collection, as this method has shown to be particularly promising when conducted via telephone (Cachia and Millward, Reference Cachia and Millward2011). Qualitative data was therefore collected via telephone by three of the authors.
Sampling and participants
For the quantitative part of this study, sampling was conducted based on municipality size using stratified random sampling with age screening. Table 1 denotes the sample distribution compared to official statistics of the same age group in Lower Austria. The unweighted sample of study participants demonstrates good quality; however, respondents with a low level of formal education, single-person households and respondents from moderate-sized municipalities are slightly underrepresented. Weights for bivariate and univariate analysis were used to counteract this underrepresentation.
Table 1. Sample distribution in the survey and the older population (60+ years)
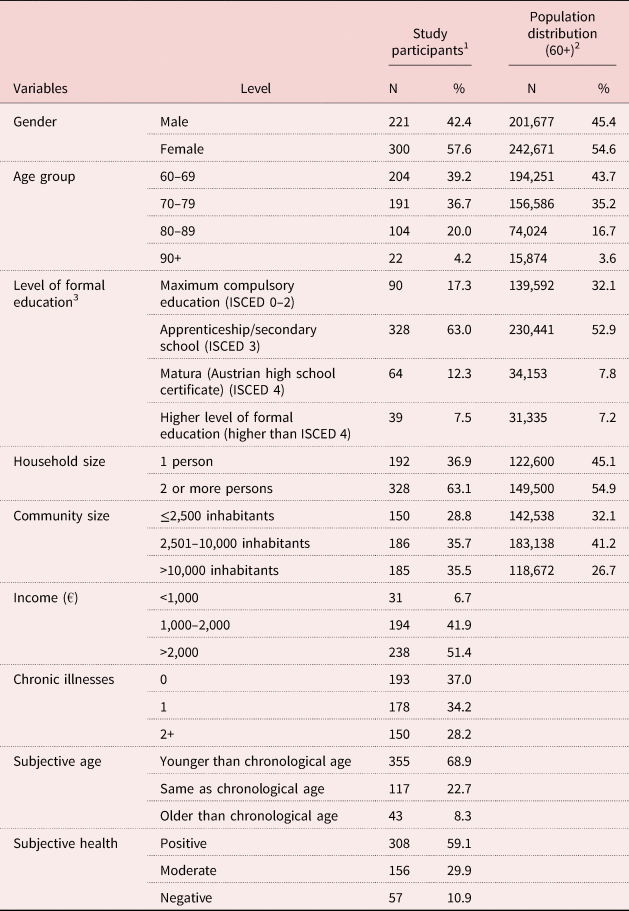
Notes: N = 521. Comparative data provided if possible. 1. Survey. 2. Data taken from official statistics: from 2019 for gender; from 2017 for level of formal education; from 2018 for age group, household size and community size. 3. Levels of formal education follow the national definition of ISCED: International Standard Classification of Education.
For the qualitative part of this study, an open call to participate in the study was distributed via seniors' organisations and education centres. During the selection process, special attention was paid to a balanced distribution of gender, age groups (under 75, 75+ years) and household size (living alone, living with others) within the sample. Respondents living in a multi-person household were mostly heterosexual couples and were interviewed separately. The final sample consisted of 20 people aged between 62 and 79 with a mean age of 69.5. Six respondents were men, seven respondents were older than 75 and 50 per cent of respondents lived in a one-person household at the time of the interview.
Data analysis
Quantitative analysis aimed to explore the association between age and the subjective risk perception due to the COVID-19 pandemic in adults over 60 years old living in Lower Austria. For this article, cross-tabulations, chi-square tests with Cramer's V as a measure of association and a multivariate logistic model were calculated, due to the moderate sample size and the lack of metric data. The logistic model was calculated on the basis of unweighted data of study participants. To assure good model quality, the number of predictor variables was limited to eight, as proposed in previous research (Bujang et al., Reference Bujang, Sa'at, Tg Abu Bakar Sidik and Lim2018). Due to missing values, the final sample used in the logistic regression model included 453 observations. Nagelkerke's R 2 is 0.466, Hosmer–Lemeshow test χ2(8) is 74.209, p is 0.514 and the area under the curve of this ROC curve is 0.867, implying that the model quality is good. All analyses were conducted using IBM SPSS version 26.
For the qualitative part of this study, the content of the interviews was analysed using a summarising qualitative content analysis (Mayring, Reference Mayring2015). The recordings served as a basis for the inductive formulation of categories. To ensure inter-coder reliability (Nili et al., Reference Nili, Tate, Barros, Riemer, Indulska and Tuunainen2017), four authors independently coded and paraphrased the data and then generalised the contents of each interview. Afterwards, these initial analyses were discussed in group sessions. All interviews were analysed over the course of seven meetings in which authors abstracted, interpreted and interconnected interviews, generating an abstract category system of the interview data. Lastly, corrections were made to ensure the inclusion of all paraphrased notes in the finalised category system, which consists of 15 categories and 45 subcategories (Table 2).
Table 2. Overview of categories and subcategories in the interview data

Tools and measures
To measure subjective risk perception in the quantitative survey, respondents were asked to rate to what extent they felt they belonged to a COVID-19 risk group (‘Would you say that you (1) ‘very much’, (2) ‘rather’, (3) ‘rather not’, or (4) ‘not at all’ belong to a so-called risk group of the corona pandemic?’). Risk was therefore considered a subjective rather than an objective concept (Leppin and Aro, Reference Leppin and Aro2009). The participant's subjective risk perception was then used as the dependent variable in binary form (1 = ‘very much’ and ‘rather’, 0 = ‘rather not’ and ‘not at all’) in the logistic regression model. Individuals who reported to be very much, rather or rather not part of a risk group (N = 442 excluding refusals) were further asked to provide reasons for their answer. Participants were asked to choose one or more reasons from a list of factors namely (a) age, (b) pre-existing medical illness, (c) current health status and (d) heavy smoking, which were risk factors identified by epidemiological studies at the time of the survey (CDC COVID-19 Response Team, 2020; Chen et al., Reference Chen, Wu, Chen, Yan, Yang, Chen, Ma, Xu, Yu, Wang, Wang, Guo, Chen, Ding, Zhang, Huang, Han, Li, Luo, Zhao and Ning2020; Promislow, Reference Promislow2020; Vardavas and Nikitara, Reference Vardavas and Nikitara2020).
Quantitative analysis further aimed to explore whether older adults perceive risks connected to COVID-19 and how these experiences are associated with age and ageing. The multivariate logistic model therefore explored the relationship between chronological age, subjective age (assessed through the question ‘How old do you feel?’) and subjective risk perception relating to COVID-19. Chronological age (1 = 60–69, 2 = 70–79, 3 = 80+) and subjective age (1 = feels younger than chronological age, 0 = feels the same age or older than chronological age) were included in the model. As age and health status had been consistently communicated as risk factors for infection by Austrian media and politics, the multivariate model also included subjective health as well as respondents' number of chronic diseases to explore the association between health status and subjective risk perception. Health status was measured using the number of chronic illnesses (0, 1, 2+) and subjective health (1 = positive, 2 = moderate, 3 = negative).
Lastly, the model explored the heterogeneity of the older population in terms of subjective risk perception. The model therefore included the level of formal education and income level as measures of social stratification in later life. It was assumed that the perception of belonging to a risk group differs according to social position and that people who live in a precarious situation are more likely to consider themselves a part of a risk group. Social differences were operationalised using the level of formal education (1 = maximum compulsory education (International Standard Classification of Education (ISCED) 0–2), 2 = apprenticeship/secondary education (ISCED 3), 3 = high school graduation certificate or higher (ISCED 4 or higher), and the level of monthly household income in euros (1 = <1,000, 2 = 1,000–2,000, 3 = >2,000). Gender (0 = female, 1 = male) and municipality size (<2,500, 2,501–10,000, more than 10,000 inhabitants) were added as control variables in the model.
For the qualitative part of this study, a semi-structured interview guide was developed that included questions about (a) changes in daily life during the COVID-19 pandemic, (b) opinions about the social distancing measures that were in place at the time of the interview, (c) perceptions of risks, and (d) experiences and images of ageing. Interviews lasted between 32 and 91 minutes, were audio recorded and afterwards paraphrased in a short, content-based form. This process also included the verbatim transcription of relevant interview passages. The quotations presented in this article text were translated from German into English by four authors via blind back-translation.
Results
Associations between age and subjective risk perception
Overall, results show that approximately two-thirds of the respondents consider themselves at risk of COVID-19, with 37 per cent seeing themselves as being ‘rather’ and 33 per cent as being ‘very much’ part of a COVID-19 risk group (Table 3). A comparison of age groups revealed statistically significant differences and a positive association between age and subjective risk perception (r s = 0.497; p < 0.001). A majority of participants stated age as a reason for identifying themselves as part of a COVID-19 risk group (82%) (Table 4). Age is named twice as often as pre-existing medical illness (42%) and four times as often as health status (20%) as the reason for higher subjective risk perception. The percentage of adults who listed heavy smoking as a factor in their subjective risk perception, which had been discussed as a possible risk factor in the media prior to the survey (Vardavas and Nikitara, Reference Vardavas and Nikitara2020), was considerably lower but in line with the overall prevalence of smoking in this age group (Klimont and Baldaszti, Reference Klimont and Baldaszti2015), with 9 per cent.
Table 3. Personal risk assessment
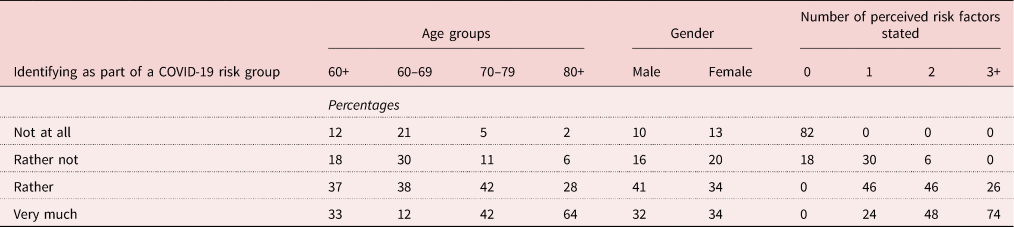
Table 4. Reasons for risk group membership
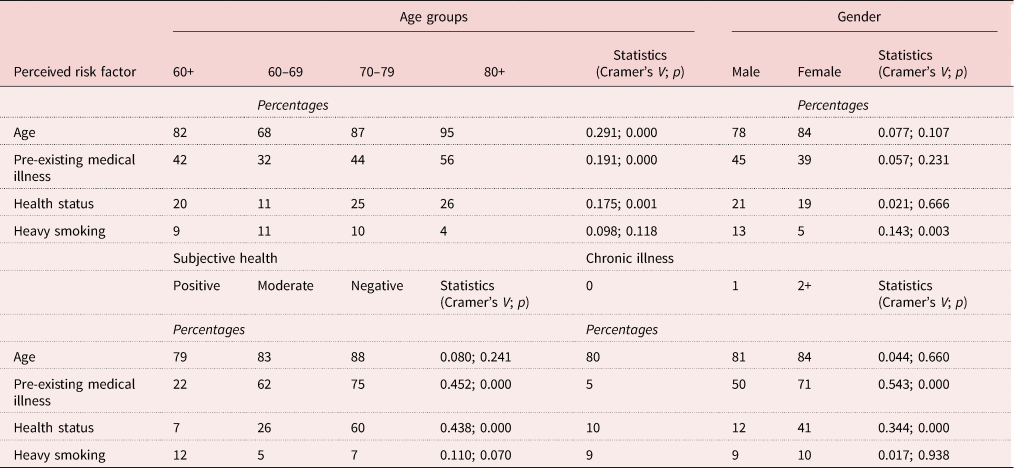
Notes: N = 521. Association with risk group membership: r s age = 0,497, p < 0.001; r s gender = −0.270, p = 0.549; r s number of reasons stated = 0.642, p < 0.001.
Our analyses show that chronological age is the predominant factor in risk assessment across all age groups tested. The association between subjective COVID-19 risk and age seems to intensify in later life, as naming age as a reason for perceived COVID-19 risk significantly correlates with respondents' chronological age (Cramer's V = 0.291; p < 0.001). Naming pre-existing medical illness as a reason for perceiving COVID-19 risk is also associated with chronological age (Cramer's V = 0.191; p < 0.001), subjective health (Cramer's V = 0.452; p < 0.001) and the number of chronic illnesses (Cramer's V = 0.543; p < 0.001).
Multivariate regression model of subjective risk perception
The logistic model (Table 5) demonstrates that, when controlling for all other variables, chronological age (70–79 years odds ratio (OR) = 6.23; 80+ years OR = 4.64) and subjective age (OR = 7.86) remain significant predictors of self-assessments of membership to a COVID-19 risk group. In fact, chronological and subjective age are the two strongest influencing factors in the overall multivariate regression model. Health status plays an independent, however, less central, role in the subjectively perceived COVID-19 risk. Multimorbidity (two or more diseases OR = 3.16) as well as moderate subjective health (moderate health OR = 2.79) further increase the probability of perceiving higher COVID-19-related risk.
Table 5. Logistic regression model of determinants of older adults' experiences of being at risk
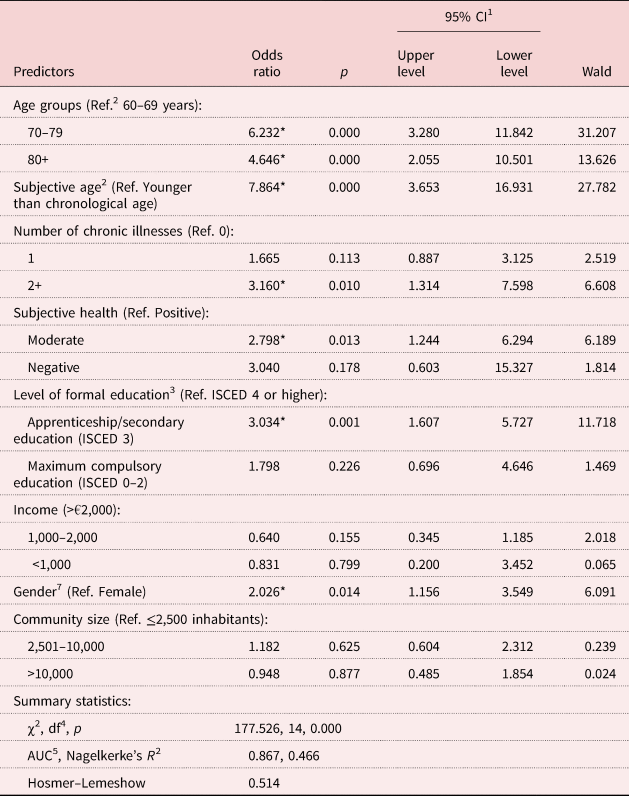
Notes: N = 453. 1CI: confidence interval 2Ref.: reference category with OR of 1 3ISCED: International Standard Classification of Education 4df: degrees of freedom 5AUC: area under the curve.
Significance level: * p < 0.05.
With regard to social position, data show that while income level does not have an influence on risk assessment, formal education plays a role in assessing the subjective COVID-19 risk. Respondents with a moderate level of formal education (ISCED 3) have an increased likelihood of self-assessment for being at higher risk for developing a (more severe) COVID-19 infection (OR = 3.03). Although the direction and size of the effect is similar to that of respondents of a moderate education level, lower education level does not significantly predict subjective risk perception. However, this may be due to a limited number of observations in this category of education in the analysed sample. Particularly remarkable were the results on gender: after controlling for all other variables in the model, men were twice as likely as women to self-identify as a member of a COVID-19 risk group (OR = 2.02).
The everyday experience of risk
Quantitative analysis revealed a significant association between subjective age and subjective risk perception, which spread across all age groups included in the sample. What are the everyday experiences of this relationship between age and COVID-19-related risk?
First and foremost, qualitative data highlighted that subjectively identifying as belonging to a risk group seemed to be less clear than indicated by quantitative data. Even though many interview partners initially identified as being part of a COVID-19 risk group, this was often the basis for manifold, ambiguous and inconsistent negotiations about the meaning of risk that took place during the interviews. Interviewees considered themselves to be fit and healthy (IP (interview person) 10, IP 15, IP 16) and used these attributes to justify why they did not identify as being at greater risk related to COVID-19. Despite this often-ambivalent self-perception, notions of being at higher risk were, however, introduced into the everyday lives of our interview partners by the media, as well as by younger family members, who offered support in grocery shopping (IP 5, IP 20) or asked them to maintain as little personal contact with others as possible (IP 7, IP 16, IP 20). Interview partners' own images of active and healthy ageing therefore often did not match with the emergence of images of older people as vulnerable, at risk and in need of protection that were put forward by relatives and the media: ‘I generally feel fit and then, I am put into this box, I feel pushed into it’ (IP 17).
Interview partners also highlighted that they felt that the media and policy were – at times unfairly – attributing higher COVID-19-related risk to older adults, regardless of their health status or pre-existing illness. During the interviews, interview partners expressed how they had perceived a change in the images of age and ageing in Austria during the COVID-19 pandemic, stating that they experienced how age and ageing were being reframed from being a lifestage that called for active and successful ageing, to a lifestage that was characterised by vulnerability, risk and the need for protection:
You are put into a box: ‘We are the old people who need protection’ … Why am I being locked up now, why am I so old all of a sudden? … I've always told my friends: ‘We are at the prime of our lives, we have worth … we are still young, even at 80’. But for now, that is over. (IP 11)
How did the interview partners negotiate these changes in images of ageing during the COVID-19 pandemic in their everyday lives? Generally, interview partners reported following the recommendations made by the Austrian government very diligently (IP 2, IP 3, IP 7, IP 11, IP 15) and described how they found their own individual solutions to coping with COVID-19-related risk. Interview partners strengthened their immune system (IP 13, IP 16), implemented more cautious hygiene measures or maintained a high grade of activity to avoid illness (IP 3, IP 7). Many described how they tried to compensate for the loss of activities outside their home by looking for other tasks (IP 5, IP 7), such as household chores (IP 9, IP 11, IP 8), gardening (IP 3, IP 8) or sports (IP 5). While these strategies ensured a sense of stability and continuity in times of lockdown for our interview partners, interviews also revealed how COVID-19-related risk was understood as an individualised risk, which depended on the individual strategies and safety measures that interview partners were implementing in their everyday lives.
In the interviews, pandemic risk was therefore neither absent nor present, but had to be constantly negotiated and evaluated based on individual factors, social resources and much more. Often, individual attributes (e.g. activity or health status, education, or social capital) were used as the basis for arguing why the COVID-19-related risk was particularly low for a person (IP 11). One interview partner described how he evaluates his social contacts, keeping in mind the individual risk each person in his social network might pose for him:
You need to think about with whom you can keep in contact. Ask where that person has been or how often this person is going out, and where that person is from. (IP 16)
In other interviews, participants shared stories about how they evaluated the places they could go, the groceries they could buy or the food they could eat (IP 11) in order to keep the individual risk of COVID-19 infection as low as possible. Interview partners therefore not only understood themselves as part of a COVID-19 risk group, but also as managers of their COVID-19 individual risk, and managing the risk of COVID-19 infection became a daily activity for the older adults interviewed.
Discussion
As one of the first studies, this paper empirically sheds light on how perceived COVID-19 risk affects the everyday lives of older adults. What do the results reveal about how older adults perceive COVID-19 risk and how this relates to images of age and ageing?
First, data show that two-thirds of older adults in Lower Austria identified as being part of a COVID-19 risk group and named chronological age, in addition to pre-existing illness or chronic disease, as contributing factors in this risk perception. Thirty-seven per cent see themselves as being ‘rather’ and 33 per cent as being ‘very much’ part of a COVID-19 risk group. After controlling background variables, chronological and subjective age were found to be the two strongest predictors of subjectively perceived COVID-19-related risk. These results highlight that the ageist assumption that connects chronological age (rather than pre-existing illness or health status) with COVID-19 risk has been internalised by a majority of the older population in Lower Austria and indicates that age-based categorisations of older adults as a COVID-19 risk group as currently discussed by media and policy are influencing the subjective perceptions of older adults. This finding expands literature that has shown how the COVID-19 pandemic has reinforced negative images of ageing (Jimenez-Sotomayor et al., Reference Jimenez-Sotomayor, Gomez-Moreno and Soto-Perez-de-Celis2020; Lichtenstein, Reference Lichtenstein2020; Meisner, Reference Meisner2020). These results are also connected to studies that show that ageism and negative age stereotypes that have surrounded debates around COVID-19 are accompanied by internalised ageism of older adults. Ageism can be directed towards individuals of any age group, towards others or oneself (Ayalon and Tesch-Römer, Reference Ayalon and Tesch-Römer2017), and while other studies have highlighted how ageism has arisen in the media during COVID-19, this study provides some first evidence that this is also true for older adults' internalised ageism. However, this study also highlights that more in-depth research on the relationship between perceived COVID-19 risk and internalised age stereotypes and ageism is needed.
Multivariate models further show that the subjective COVID-19 risk perception was further influenced by older adults' subjective health as well as number of chronic diseases. The analysis on socio-economic differences revealed that there is no significant association between income and subjective risk perception and only a weak association between education and subjective risk perception. Furthermore, in line with the higher risk of mortality of older men compared to women (Jin et al., Reference Jin, Bai, He, Wu, Liu, Han, Liu and Yang2020), women showed a lower probability of identifying as belonging to a COVID-19 risk group. Although the association found between social position and COVID-19-related risk perception is weak in the present study, other empirical studies have shown that socio-economic resources help manage COVID-19-related risk and stress in later life (López et al., Reference López, Perez-Rojo, Noriega, Carretero, Velasco, Martinez-Huertas, López-Frutos and Galarraga2020). Future studies are needed to examine the connection of subjective risk perception and socio-economic differences in later life more closely in order to understand the mechanisms and practices through which current COVID-19 discourses feed into the marginalisation of already-marginalised older adults and how this affects men and women differently.
Third, qualitative analysis showed that older adults reported that they experienced being ‘suddenly seen as old’ or being ‘put into a box’ during the pandemic, which influenced their experiences of ageing. This was due to the media discourse our interview partners were following closely during the pandemic; however, it was somewhat intensified by family members who offered support and help during the pandemic. This adds to literature suggesting that benevolent or compassionate ageism (Binstock, Reference Binstock2010; Vervaecke and Meisner, Reference Vervaecke and Meisner2020) has been prevalent during the global COVID-19 pandemic.
Lastly, qualitative data highlighted that there is a considerable shift in understandings of risk and riskiness and how it connects to later life. Even though the entirety of older adults were addressed as a risk group by Austrian policy and media, the interviews showed that older adults constructed their COVID-19 risk as an individualised risk. In the data, examples show how older adults evaluated their individual COVID-19 risk based on individual resources or everyday practices: belonging to a COVID-19 risk group (or not) was therefore not dependent on their age, but rather their individual resources in dealing with the pandemic. Interviewees further described how their positions and roles in everyday life were changing during the pandemic – as their self-perceptions changed from feeling as ambassadors for active and successful ageing towards experiencing themselves as managers of individual risk. Therefore, the ethical implication of this study is that a turn in the discourses about risk groups of COVID-19 is needed. Addressing older adults as a risk group because of their age reinforced external and internalised ageism as well as negative images of ageing leading to psychological and emotional stress for older adults. Focusing on health instead of age as an indicator for an infection risk might strengthen a perspective that perceives older adults as a heterogeneous and autonomous group.
There are several limitations to keep in mind when interpreting the results of this exploratory study. Most importantly, this paper is based on a study that was conducted in Lower Austria. While this rather narrow focus of the study enabled an in-depth analysis, this limitation should be kept in mind when interpreting these results. Quantitative results on the role of social position in subjective risk perception in later life should also be interpreted with care and inspire future studies on the topic. While our study revealed first signs of an association between subjective risk assessment and level of education, the mechanisms behind this association need to be studied in greater depth and with larger samples than this study could have provided. Lastly, this study was based in Austria, which could call the applicability of the results to other welfare states into question. However, we do believe that a shift towards more negative images of ageing and ageism during COVID-19 is not limited to the Austrian context but characterises experiences of age and ageing in all Western societies. We therefore hope that future studies will produce similar results and will further explore these changes in the subjective experience of later life that COVID-19 has brought to light.
Data
The data used in this study are available through the authors upon reasonable request.
Acknowledgement
This work was supported by the Department of Sociology, University of Vienna.
Financial support
This work was supported by Land Niederösterreich and NOEGUS. The financial sponsors played no role in the design, execution, analysis and interpretation of data, or writing of the study.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The study was conducted according to the ethical standards of the University of Vienna. Informed consent was obtained from all subjects involved in the study before data collection, explicitly explaining the goal of the study, data protection and data utilisation, as well as participants' rights. Consent was expressed orally at the start of each interview and was audio-recorded digitally. All study participants participated voluntarily in this study.







