Introduction
Worries about health are a common human experience thought to fall along a continuum in the general population (Salkovskis and Warwick, Reference Salkovskis, Warwick, Starcevic and Lipsitt2001). At the upper end of the continuum, individuals experience an obsessive fear of illness (Bilani et al., Reference Bilani, Jamali, Chahine, Zorkot, Homsi, Saab and Chaaya2019) which may fall within the realm of health anxiety. Health anxiety as a diagnostic entity is characterised by a pre-occupation with either having or developing a serious physical illness, which is maintained by behaviours which are designed to ameliorate distress, but serve to inadvertently increase or maintain physical symptoms and anxiety. Recently changed to ‘illness anxiety disorder’ in the Diagnostic Statistical Manual [DSM-5; American Psychiatric Association (APA), 2013], the term health anxiety (HA) is still in common use by mental health professionals as this also refers to the evidence-based cognitive behavioural model of HA that is used in research and clinical settings (Salkovskis et al., Reference Salkovskis, Warwick and Deale2003; Warwick and Salkovskis, Reference Warwick and Salkovskis1990). In this paper, we seek to extrapolate evidence from the HA literature to inform how health-related worries in children and young people may be managed in practice, and more specifically, how this might relate to infectious disease pandemics such as COVID-19.
Health anxiety in children and young people
HA as a disorder typically presents in early or middle adulthood (APA, 2013; Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016). There is some evidence to suggest that HA does occur in childhood and adolescence (Eminson et al., Reference Eminson, Benjamin, Shortall, Woods and Faragher1996; Oliver et al., Reference Oliver, Wright, Kakadekar, Pharis, Pockett, Bradley and Erlandson2018; Rask et al., Reference Rask, Elberling, Skovgaard, Thomsen and Fink2012; Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016; Sirri et al., Reference Sirri, Ricci Garotti, Grandi and Tossani2015; van Geelen et al., Reference van Geelen, Rydelius and Hagquist2015; Wright and Asmundson, Reference Wright and Asmundson2003), yet studies examining the prevalence of HA in children and young people suggest that few meet the full diagnostic criteria (Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016). This may be partly due to a lack of tailored, developmentally appropriate descriptions of how HA presents in children and young people (Fritz et al., Reference Fritz, Fritsch and Hagino1997; Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016).
The DSM-5 diagnostic criteria for illness anxiety disorder (previously known as HA) specifies that the following symptoms need to be present for at least 6 months: pre-occupation with illness, absence of somatic symptoms, hypervigilance of own health, self-monitoring for signs of illness, complete avoidance of medical care or conversely frequent seeking of medical care (APA, 2013). There are likely to be key differences in the presentation of HA in children and young people which relate to stages of development, particularly in relation to safety-seeking behaviours and ability to articulate what has precipitated the behaviour. For example, the pre-occupation with already having or contracting an illness may manifest as more generic concerns about health as detailed knowledge of disease and disease processes may be absent, especially in younger children. Like adults, children may display checking behaviours and seek reassurance directly from parents, while adolescents may be more prone to seeking reassurance more tacitly from friends or by searching for information online. Avoidance is also likely to be present, but the ability to articulate the root of the avoidance is likely to vary according to developmental abilities.
Parental reassurance, acquiescence and inadvertent collusion with safety-seeking behaviours will serve to maintain anxiety through prevention of disconfirmation and the associated physiological and emotional impact of safety-seeking behaviours we see in adults. Retrospective studies of adults with HA indicate that key symptoms, such as fears about becoming unwell, were present in childhood (Fink et al., Reference Fink, Ornbol, Toft, Sparle, Frostholm and Olesen2004; Noyes et al., Reference Noyes, Stuart, Langbehn, Happel, Longley and Yagla2002), suggesting that the hallmark symptom of HA diagnosis, feeling pre-occupied by the idea that one might be ill, is present from an early age; we know less about the behavioural maintenance at this early age, however we may apply the mechanisms we see in other anxiety disorders.
Health-related worries and behaviours are common in children and young people (Rask et al., Reference Rask, Elberling, Skovgaard, Thomsen and Fink2012; Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016; Sirri et al., Reference Sirri, Ricci Garotti, Grandi and Tossani2015; Wright and Asmundson, Reference Wright and Asmundson2003), with 15.7% of a sample of 14- to 19-year-olds reporting ‘clinically significant hypochondriacal symptoms’ (Sirri et al., Reference Sirri, Ricci Garotti, Grandi and Tossani2015) and the parents of 2.7% of 5- to 7-year-olds reporting ‘considerable’ health anxiety symptoms in their children (Rask et al., Reference Rask, Elberling, Skovgaard, Thomsen and Fink2012). Thus, even though prevalence of HA as a recognised disorder may not have been established, health-related worries appear to be relatively common.
HA has a significant impact on functioning in children and young people; health-related anxiety symptoms have been found to be significantly positively associated with mental health problems (including emotional disorders, distress and somatisation) across a range of age groups (Rask et al., Reference Rask, Elberling, Skovgaard, Thomsen and Fink2012; Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016; Sirri et al., Reference Sirri, Ricci Garotti, Grandi and Tossani2015). Additionally, younger children with higher levels of HA-related symptoms are more likely to present with functional somatic health problems than their peers (Rask et al., Reference Rask, Elberling, Skovgaard, Thomsen and Fink2012; Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016). There are also economic costs. The medical costs for children with the highest levels of HA-related symptoms have been found to be 150 Euros more than those with the lowest levels of HA symptoms over a 2-year period, even when controlling for physical health conditions (Rask et al., Reference Rask, Munkholm, Clemmensen, Rimvall, Ornbol, Jeppesen and Skovgaard2016).
Health related worries in the context of COVID-19
COVID-19 is an infectious disease caused by a novel coronavirus, SARS-CoV-2 [World Health Organization (WHO), 2020a] which, in most cases, results in mild symptoms such as a dry cough and fever. In a minority of cases, SARS-CoV-2 can lead to more severe complications (including acute respiratory distress syndrome) and can be fatal (Sohrabi et al., Reference Sohrabi, Alsafi, O’Neill, Khan, Kerwan, Al-Jabir and Agha2020). Children and young people are reported to be asymptomatic or relatively more mildly affected with few severe cases reported (Lu et al., Reference Lu, Zhang, Du, Zhang, Li and Qu2020).
Since the global spread of COVID-19, and the declaration of a pandemic by the World Health Organization on 11 March 2020 (WHO, 2020b), the worldwide health context is far from typical. There is a genuine and unprecedented threat to health and survival, which results in health concern. This threat is compounded by media focus on numbers of positive cases and deaths (Taylor, Reference Taylor2019) rather than negative cases and recoveries. This is likely to increase public perception of risk of contracting the virus, as well as over-estimation of risk if they do (Wheaton et al., Reference Wheaton, Abramowitz, Berman, Fabricant and Olatunji2012).
In the face of an unprecedented infectious disease pandemic, it is natural to feel anxious and to be concerned about one’s own health and the health of others. For most, anxiety will be a proportionate and adaptive response to the threat posed by the virus, motivating individuals to engage in sensible, precautionary health behaviours (Taylor, Reference Taylor2019). However, for a minority, particularly those who may be pre-disposed to anxiety and/or who lack coping resources, COVID-19 might act as a ‘critical incident’ that triggers health-related worries. In these individuals, ‘normal’ health anxiety escalates and becomes distressing and debilitating; while for others, health-related fears are transitory and simmer down once the threat begins to pass. It is the former that we focus on in this review.
Health-related worries in children and young people and COVID-19
There are both individual and systematic factors that may render children and young people particularly vulnerable to health-related worries in the context of COVID-19. It is important to acknowledge that there are key differences in the presentation of anxiety between children and adolescents (Waite and Creswell, Reference Waite and Creswell2014), such as the expression of affect through physical sensations in younger children. We distinguish between these two groups where possible and where there is an evidence base to support such differentiation.
Individual factors – cognitive and developmental
For children and young people, COVID-19 will probably be the first major global health threat they will have been exposed to. This may shape or disrupt the formation of their emergent beliefs about the world being a ‘safe place’ with regard to health. There are a multitude of messages about the omnipresent threat: significant changes to behaviour have been enforced, including school closures as disease containment measures, alarming public health messages about staying home, avoiding people and keeping ‘safe’ being repeatedly communicated through various media.
Children’s cognitive ability to process and understand complex information is more limited and concrete in comparison with adults (Inhelder and Piaget, Reference Inhelder and Piaget1958). This makes it more difficult for children to understand abstract information, such as a ‘viral’ health-related threat. Their emergent beliefs are also more malleable than those of adults and are influenced and shaped by significant others (Cantor et al., Reference Cantor, Osher, Berg, Steyer and Rose2018). Over the course of adolescence, the individual’s own ideas and beliefs develop, often influenced by those of peers. Their cognitive abilities develop so that they can make sense of the world and events in more abstract, complex ways, and can hold several possibilities in mind. Adolescents are also increasingly able to take ownership over health-relevant behaviours (Turner-Cobb, Reference Turner-Cobb2013); however, this and earlier childhood is a sensitive time in terms of their formative development of their understanding of the world.
Individual factors – pre-existing mental health or physical health problems
Some children and young people are more vulnerable to developing health-related worries in this context due to pre-existing anxiety and/or experiences. In university students, prior anxiety sensitivity and obsessive-compulsive symptoms and beliefs increased the risk of experiencing pandemic-related anxiety in the context of swine flu (Brand et al., Reference Brand, McKay, Wheaton and Abramowitz2013). This may also be relevant for children and young people who have pre-existing anxiety and a heightened sense of the world as a ‘dangerous’ place prior to COVID-19. Those who experience the death or serious illness of someone in their personal or social network as a result of the disease, and those who live with parents who are particularly worried about the virus and its impact, may be more vulnerable to developing health-related worries.
Some children and young people have underlying physical health problems which render them more vulnerable to respiratory-type illnesses like COVID-19, including those with asthma and the immunosuppressed. These individuals will need to take a higher level of precautionary measures to keep ‘safe’; it is these additional measures and higher sense of threat of illness that leave them at higher risk of ongoing health-related worries. Due to lack of complex cognitive abilities at a young age, children may generalise the perception of threat.
Systemic factors – parent and carer mental health
Children’s beliefs about illness and their responses to symptoms are shaped by those of significant others, particularly their primary caregivers, most typically their parents (Turner-Cobb, Reference Turner-Cobb2013). There is evidence of an association between parent and child HA symptoms (Koteles et al., Reference Koteles, Freyler, Kokonyei and Bardos2015; Marshall et al., Reference Marshall, Jones, Ramchandani, Stein and Bass2007; Remmerswaal and Muris, Reference Remmerswaal and Muris2011; Wright et al., Reference Wright, Reiser and Delparte2017). This may arise in several ways. Firstly, a significant proportion of learning takes place, particularly at a young age, through observation and imitation of significant others. Secondly, the responses of those significant others reinforce particular behaviours that the child displays (Bandura, Reference Bandura1977). Thus, interacting with others is a key social-cognitive process that inevitably shapes the child’s belief system.
Emerging evidence suggests that anxiety levels in adults in the general population have increased since ‘lockdown’ (Bentall, Reference Bentall, Lvita, Hartman, Martinez, Stocks, Shelvin, Murphy, McBride, Manson, McKay and Hyland2020), with HA in the adult population estimated to have increased by around 10% (Rettie and Daniels, Reference Rettie and Daniels2020). The psychological impact of ‘lockdown’ for adults is likely to be profound and long lasting for many (Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020). Adults are likely to be experiencing stress and general pressures associated with lack of access to normal activities of daily living, and financial concerns due to the economic consequences of lockdown (Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020). In addition, many parents have the pressure of home-schooling their children whilst also working themselves.
When parental mental health is compromised, there is undoubtedly some degree of impact on the child. This may be directly through modelling of anxious behaviour or reduced capacity for the parent to support the child with their own anxiety, for example. Indeed, there is a large body of evidence to support the notion of intergenerational transmission of anxiety (Lawrence et al., Reference Lawrence, Murayama and Creswell2019). This is likely to be further compounded by the curtailed access to both adult and child mental health support, and to other supportive adults such as educational professionals during school closures.
Assessment
There is a high degree of co-morbidity in anxiety disorders (Creswell et al., Reference Creswell, Waite and Cooper2014; Kendall et al., Reference Kendall, Compton, Walkup, Birmaher, Albano, Sherrill and Piacentini2010; Leyfer et al., Reference Leyfer, Gallo, Cooper-Vince and Pincus2013) and mood disorders (Essau, Reference Essau2003) across the age range. However, research indicates it is possible to separate diagnostic features of different forms of anxiety reliably (Spence, Reference Spence2017). Even though anxiety disorders share transdiagnostic processes, they can be separated by their primary focal point of anxiety (Ferdinand et al., Reference Ferdinand, Dieleman, Ormel and Verhulst2007), therefore accurate and thorough assessment is imperative to access the right support.
In children and young people, a multi-method (including interviews, questionnaires and observational approaches) and multi-informant (self-, parent- and possibly teacher-report) approach to assessment is recommended (Hudson et al., Reference Hudson, Newall, Rapee, Lyneham, Schniering, Wuthrich and Gar2014; Kazdin, Reference Kazdin2003; Silverman and Ollendick, Reference Silverman and Ollendick2005).
Structured diagnostic interviews are generally considered to be the gold standard assessment to identify mental health disorders in children and young people (Spence, Reference Spence2017). These tend to seek information from multiple informants, most often the affected child or young person and a parent. The most used measures include the Anxiety Disorders Interview Schedule (Silverman and Albano, Reference Silverman and Albano1996) and the Kiddie Schedule of Affective Disorders and Schizophrenia (Kaufman et al., Reference Kaufman, Birmaher, Brent, Rao, Flynn, Moreci and Ryan1997), both of which include questions pertaining to health-related worries, although sections pertaining to a diagnosis of health anxiety are comparatively brief.
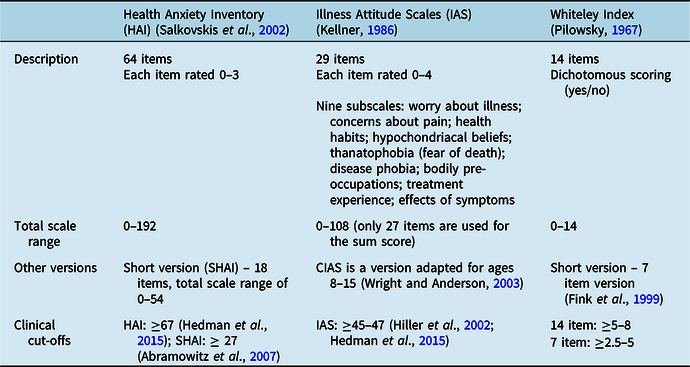
Self-report questionnaires can be useful as a screening tool to complement a clinical interview; however, there are no specific questionnaires or subscales on generic questionnaires which measure HA in children and young people. A version of the Illness Attitudes Scale (IAS; Kellner, Reference Kellner1986) has been developed for children, although its psychometric properties are yet to be established. Validated and reliable self-report measures developed for use in adults may be useful (see Table 1), although their psychometric properties in children and young people are unknown. There are also several questionnaires that have been developed for research purposes to examine parental report of children’s health-related worries; however, these have not been extensively used in clinical practice (Rask, Reference Rask2019). These include the parent version of the Illness Worry Scale (IWS-p; Garralda and Rangel, Reference Garralda and Rangel2001), Fetal Health Anxiety Inventory (Reiser and Wright, Reference Reiser and Wright2019) and the Protect subscale of the Adult Responses to Children’s Symptoms (ARCS; Van Slyke and Walker, Reference Van Slyke and Walker2006).
Table 1. Self-report measures of health anxiety developed for use with adult populations
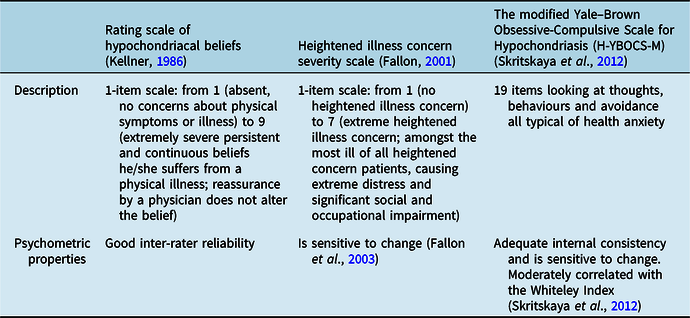
Additionally, there are clinician rating scales for HA (see Table 2), although these also have not been developed specifically with children and young people in mind.
Table 2. Clinician-administered measures of health anxiety
Formulation
The current understanding of HA is primarily informed by cognitive behavioural models (Abramowitz et al., Reference Abramowitz, Schwartz and Whiteside2002; Asmundson et al., Reference Asmundson, Carleton, Wright and Taylor2004; Salkovskis et al., Reference Salkovskis, Warwick and Deale2003; Taylor and Asmundson, Reference Taylor and Asmundson2004; Warwick and Salkovskis, Reference Warwick and Salkovskis1990). Cognitive behavioural therapy (CBT) models have the strongest empirical underpinning and evidence base for the treatment of anxiety disorders (e.g. see Abramowitz et al., Reference Abramowitz, Moore, Braddock and Harrington2009; Marcus et al., Reference Marcus, Gurley, Marchi and Bauer2007; Marcus and Norris, Reference Marcus and Norris2014; Rachman, Reference Rachman2012; Taylor and Asmundson, Reference Taylor and Asmundson2004). The Salkovskis et al. (Reference Salkovskis, Warwick and Deale2003) model of HA posits that through experience, health-related beliefs are formed that may lead to misappraisal of innocuous bodily states, then further pre-disposing the person to the development of HA. Once established, episodes of HA are usually triggered by incoming health-related stimuli, which are interpreted to be a relevant threat. This raises anxiety, precipitating use of safety-seeking behaviours to reduce anxiety and prevent feared health catastrophes; however, these behaviours prevent disconfirmation of beliefs and perpetuate this cycle of anxiety.
Figure 1 presents the empirically grounded CBT formulation for HA in adults (Salkovskis et al., Reference Salkovskis, Warwick and Deale2003), adapted for children and young people in the context of COVID-19. This formulation outlines the interrelated cognitive, behavioural, affective and physiological factors in HA outlined above, and includes the role of parents in the maintenance of anxiety in children and young people (e.g. Murray et al., Reference Murray, Creswell and Cooper2009), with further considerations to the wider societal context in which the child or young person lives.

Figure 1. A simplified model of health anxiety as applied to children and young people and their families. Adapted from Salkovskis et al. (Reference Salkovskis, Warwick and Deale2003).
The hypothetical formulation of health anxiety in children and young people presented here is drawn from the known characteristics of health anxiety in adults, and the empirically grounded evidence-based model of health anxiety in adults. It is therefore subject to the inherent limitations of extrapolating mechanisms that underpin anxiety in adults to children, and it is within this context that the model should be considered. Further research is needed to understand the underpinning mechanisms that maintain health anxiety in children and young people and the adaptations that may be required to accommodate particular developmental stages.
For children and young people, triggers for anxiety are likely to take the form of physical sensations (e.g. urge to cough/coughing) or health threat information (e.g. TV programmes, news updates). As children and young people are less likely to scrutinise the quality and relevance of incoming information, a threat response may be triggered at a lower threshold than adults. Cognitions might typically centre on the risk and likelihood of becoming ill with COVID-19, alongside thoughts of how catastrophic this could be (i.e. ultimately death of self/parent). Behaviours resulting from these health-related fears would be strategically aimed at reducing both distress and risk of contracting COVID-19, with the unintended consequence of increasing anxiety through prevention of disconfirmation, e.g. symptom checking, overly restrictive practices, excessive handwashing. This process also serves to increase the perception of worrying physical sensations, through symptom hypervigilance for example, or interoceptive experience of physiological arousal associated with anxiety. This further acts as a health-related stimulus, elevating anxiety and perceived health risk, and so the cycle continues. This is particularly problematic due to the limited ability that children may have to understand and express their own emotions, therefore the experience of emotions themselves may be perceived as threatening.
Within this adapted formulation we also present key mechanisms between the parent and child that may contribute to the maintenance of distress, albeit inadvertently. Illness beliefs in the anxious parent trigger safety-seeking strategies that are designed to keep both themselves, and the child, emotionally and physically safe. However, parental safety-seeking behaviours, and the anxieties that underpin them, are likely to raise salience of the health threat to the child. This in turn drives the child’s own safety-seeking behaviours, which also seek to reduce distress and threat to physical health. Parental safety-seeking behaviours are also likely to influence the child’s behaviours without an explicit cognitive route, e.g. parent repeatedly checks for signs of illness, this behaviour is repeated by the child, learned via modelling and reinforced by the absence of negative consequences. This, within a societal context of public health messages that everyone must stay home in order to be safe and keep others safe, and with schools and workplaces closed, may lead to intensifying difficult dynamics within the family home.
Treatment
Specific interventions for HA in children and young people are lacking. Therefore, it may be useful to draw together existing adult treatments that address health-related anxiety in complex medical contexts (Daniels et al., Reference Daniels, Parker and Salkovskis2020; Daniels and Sheils, Reference Daniels and Sheils2017; Tyrer et al., Reference Tyrer, Salkovskis, Tyrer, Wang, Crawford, Dupont and Barrett2017) and established knowledge on how psychological treatments are adapted for children and young people. While there is research exploring health-related fears during infectious disease outbreaks, this does not extend to treatment studies, which are primarily focused on trauma and generic anxiety and depression, so we have little new to learn in this respect. The evidence-based model commonly used for HA is described by Salkovskis et al. (Reference Salkovskis, Warwick and Deale2003); however, this requires adaptation for use with children and young people to ensure it is developmentally appropriate (Rask, Reference Rask2019).
The evidence for cognitive behavioural therapy
There is evidence to support the use of CBT for childhood anxiety, ranging from low-intensity interventions (bibliotherapy and E-therapy) to high-intensity interventions (nine to 20 face-to-face sessions: Creswell et al., Reference Creswell, Waite and Cooper2014; Creswell et al., Reference Creswell, Waite and Hudson2020; James et al., Reference James, James, Cowdrey, Soler and Choke2015). The response to CBT is dependent on the type of anxiety presentation; children and adolescents with social anxiety may experience a slower rate of change post-treatment than those suffering from generalised anxiety (Hudson et al., Reference Hudson, Rapee, Lyneham, McLellan, Wuthrich and Schniering2015). Studies have tended not to conduct separate trials for children and adolescents, despite different presentations in these two groups. Zhou et al. (Reference Zhou, Zhang, Furukawa, Cuijpers, Pu, Weisz and Xie2019) conducted a network meta-analysis of psychotherapies delivered within a range of conditions and modalities, e.g. individual and group, internet and face-to-face, with and without parental involvement. CBT treatments had the best outcomes in terms of quality of life and functioning. Schwartz et al. (Reference Schwartz, Barican, Yung, Zheng and Waddell2019) conducted a meta-analysis of anxiety interventions for children and found that 10 of the 11 CBT interventions evaluated were effective in reducing anxiety in children and young people. However, it is important to note that neither of these studies specifically focused on health-related worries.
CBT is effective in treating HA in adults (Cooper et al., Reference Cooper, Gregory, Walker, Lambe and Salkovskis2017; Hart and Bjorgvinsson, Reference Hart and Bjorgvinsson2010; Newby et al., Reference Newby, Smith, Uppal, Mason, Mahoney and Andrews2018). A brief five to 10 sessions of adapted CBT for HA (known as CBT-HA) was effective in improving HA symptoms (Tyrer et al., Reference Tyrer, Cooper, Salkovskis, Tyrer, Crawford, Byford and Barrett2014), improvements were sustained over 5 years and the intervention was cost-neutral (Tyrer et al., Reference Tyrer, Salkovskis, Tyrer, Wang, Crawford, Dupont and Barrett2017). CBT has been found to be more effective than psychoeducation, clinical support and monitoring (Newby et al., Reference Newby, Smith, Uppal, Mason, Mahoney and Andrews2018), whilst cognitive and exposure-based approaches have also both been found to be effective (Weck et al., Reference Weck, Neng, Richtberg, Jakob and Stangier2015).
We propose that formulation-driven CBT for health-related worries and HA is probably the best treatment available for children and young people with HA. This will be most effective if adapted to be developmentally appropriate. Creswell et al. (Reference Creswell, Waite and Hudson2020) suggest that disorder-specific treatments may improve outcomes for young people with anxiety, but that evidence-based models need to be developed and tested in large clinical trials. In this paper we therefore provide an adaptation of the adult disorder-specific model, with developmental considerations. This hypothetical model is underpinned by existing research into health-related fear and anxiety in children and young people and draws together what is known to work for children with anxiety and adults with health anxiety.
What a CBT intervention for health-related worries with a child or young person could involve
The aim of CBT for HA is to reduce distress, reduce unhelpful safety-seeking behaviours and enable consideration of alternative explanations of physical sensations that are being misinterpreted as signs of disease (Daniels and Loades, Reference Daniels and Loades2017; Tyrer et al., Reference Tyrer, Cooper, Salkovskis, Tyrer, Crawford, Byford and Barrett2014).
As with adult HA interventions and good practice in CBT for children and young people (Fuggle et al., Reference Fuggle, Dunsmuir and Curry2012; Stallard, Reference Stallard2002, Reference Stallard2005), assessment and formulation is the necessary foundation of individualised treatment. Once a shared understanding is reached of how health-related worries manifest, including the cyclical nature and the role of safety-seeking behaviours, it is the latter which becomes the focus of the intervention. In the context of COVID-19, the intervention might also involve a focus on tolerance of uncertainty, and recognition that the excessive use of precautionary measures may be increasing rather than decreasing anxiety about contracting COVID-19. This will foster an understanding of what constitutes necessary precautionary measures which are no more, or no less than required (see Table 3). Adaptations must be made to ensure efficacy of treatment for children and young people. Rask (Reference Rask2019) suggests that duration and creative content of sessions (role play, using cartoons, drawing or using play) should be key considerations when adapting a CBT intervention for children, in addition to adjustments for cognitive and social developmental stages. This might include simplification of concepts, scaffolding knowledge and emotional literacy through increased psychoeducation about both illness and about emotions, including family members in treatment, and use of creative, fun activities to engage children and young people (Stallard, Reference Stallard2002). Some of the intervention strategies commonly used in CBT for HA are conceptually abstract and require cognitive reasoning, which would require adaptation to stage of cognitive emotional development.
Table 3. What CBT for health-related worries in children and young people in the COVID-19 context might involve (adapted from Tyrer et al., Reference Tyrer, Cooper, Tyrer, Salkovskis, Crawford, Green and Barrett2011)

How parents might be involved in treatment
Rask (Reference Rask2019) outlines three fundamental differences between child HA and adult HA, which point towards a central role of parents/caregivers in the treatment of HA and health-related worries in children:
-
(1) There is a qualitative difference to a child’s thinking processes compared with an adult, and they will have a different understanding of illness and disease.
-
(2) Reassurance seeking will often be directed to adults in the child’s life such as parents, caregivers and teachers rather than health professionals.
-
(3) Maintaining factors will be inextricably linked to the beliefs and psychosocial functioning of parents.
While there are differences between HA in adults and in those aged under 18, it is also important to consider that there are also likely to be developmental differences between children and young people (Waite and Creswell, Reference Waite and Creswell2014). For example, the child’s age and developmental stage may influence decision-making and relevance of parental involvement in therapy. This may be helpful for younger children but may actually feel disempowering and inhibit engagement for adolescents. It may be that involving parents in some but not all sessions, or at the beginning or end of sessions only could be useful in this circumstance. Evidence regarding parental involvement in children’s anxiety treatment is mixed. Two recent meta-analyses included studies reflecting a wide range of ages (3–18 years) and concluded that parental involvement has little or no impact on outcome (Thulin et al., Reference Thulin, Svirsky, Serlachius, Andersson and Ost2014; Zhou et al., Reference Zhou, Zhang, Furukawa, Cuijpers, Pu, Weisz and Xie2019), whilst other studies report that for children aged 4–12 years, parent-led CBT is effective in treating anxiety (Cartwright-Hatton et al., Reference Cartwright-Hatton, McNally, Field, Rust, Laskey, Dixon and Symes2011; Creswell et al., Reference Creswell, Violato, Fairbanks, White, Parkinson, Abitabile and Cooper2017; Waters et al., Reference Waters, Ford, Wharton and Cobham2009). Parent-led treatment for HA in children could therefore be a useful approach and warrants further exploration.
Creswell and colleagues (Reference Creswell, Waite and Hudson2020) suggest that parental involvement is not binary; it is the quality of involvement that is important, recommending a nuanced approach to involving parents, which may be dependent on the individual formulation for that child. There is evidence that involvement of parents in online CBT programmes produces significantly larger effect sizes than programmes that do not involve parents (Grist et al., Reference Grist, Croker, Denne and Stallard2018). There is also evidence that if parental involvement in low-intensity therapy such as bibliotherapy is closely supported by a therapist, outcomes are enhanced (Cobham, Reference Cobham2012; Lyneham and Rapee, Reference Lyneham and Rapee2006; Thirlwall et al., Reference Thirlwall, Cooper, Karalus, Voysey, Willetts and Creswell2013).
Delivering psychological therapies in the COVID-19 context
Dalton et al. (Reference Dalton, Rapa and Stein2020) indicate that it is of utmost importance to talk about the pandemic with children and young people in a developmentally appropriate manner. This is particularly the case if children and young people experience distress related to COVID-19. In the context of lockdown measures, social isolation and physical distancing, face-to-face therapy is not practical or safe, therefore it is important to consider alternative methods in delivering treatment. There is a body of evidence indicating that computerised CBT is effective in child, young people and adult populations (Grist et al., Reference Grist, Croker, Denne and Stallard2018; Hollis et al., Reference Hollis, Falconer, Martin, Whittington, Stockton, Glazebrook and Davies2017; Newby et al., Reference Newby, Haskelberg, Hobbs, Mahoney, Mason and Andrews2020; Olthuis et al., Reference Olthuis, Watt, Bailey, Hayden and Stewart2016; Thew, Reference Thew2020; Vigerland et al., Reference Vigerland, Lenhard, Bonnert, Lalouni, Hedman, Ahlen and Ljótsson2016). Evidence also suggests that transdiagnostic online CBT for anxiety in children and young people can be as effective in emergency contexts: in 2012, after a series of violent earthquakes in New Zealand, an online therapist-assisted CBT package was found to be effective at reducing anxiety (Moor et al., Reference Moor, Williman, Drummond, Fulton, Mayes, Ward and Stasiak2019). Moreover, many therapists are now delivering CBT via video platforms during the pandemic out of necessity. In response to these and other changes, the British Psychological Society (BPS) (2020) have produced guidance on adaptation for this mode of delivery which recommends working creatively with children on a video call by utilising screen sharing; managing expectations through having a set session format; ensuring privacy; and being alert to signs of distress and having a plan as to how to respond to this remotely. The BPS guidance is also clear that therapy delivered via video may not be appropriate for all children and young people.
In the absence of online HA-specific interventions for children and young people, adapting existing online evidence-based programmes for anxiety to address health-related worries relevant to COVID-19 specifically may hold promise. The adaptations needed would include specific content about coronaviruses and COVID-19, and about concerns children and young people may have about the health threat to adults as well as to themselves. This would need to acknowledge the ongoing uncertainty about COVID-19 and to include a focus on coping with this uncertainty, as well as uncertainty about how long disease containment measures will be in place and how they will be lifted. Content and techniques, including practical exercises, would need to consider physical distancing and disease containment measures. Specific suggestions about how to seek social support and to maintain social contact within these limitations may also be helpful. Further research is needed to establish if existing transdiagnostic programmes, delivered online, are effective in the pandemic context at reducing health-related worries.
Conclusion
In the context of a global pandemic, some degree of health-related fear is normal and adaptive. However, for a minority of children and young people, this health-related fear may become particularly distressing. It may interfere substantially with their functioning and persist over time, in a way that we recognise in HA. For these children and young people, adopting a multi-informant approach to assessment, including using existing HA scales to complement clinical interview, could help to establish the extent of their HA. An individualised formulation of the problem, including the cognitive, behavioural and emotional components, based on the CBT model, should be developed. Consideration of developmental factors such as cognitive ability, emotional literacy, intergenerational transmission of beliefs and parental modelling or reinforcement of behaviours, is an important part of the formulation. Adapting existing evidence-based HA treatments for adults and offering these to children and young people may be most helpful. More research is needed to establish age-appropriate diagnostic criteria and standardised tools for assessment of HA in younger children, and to evaluate developmentally appropriate treatment intervention/programmes.
Acknowledgements
The original idea for this review came from Dr Maria Loades and Dr Jo Daniels. The authors would like to thank Megan Armond (research assistant) and Ross Robinson (trainee clinical psychologist) for their support with some background searches for this review. The authors are also grateful to Megan McManus for her assistance with referencing.
Financial support
Dr Loades is funded by the National Institute for Health Research (NIHR Doctoral Research Fellowship, DRF-2016-09-021). Dr Cooper is funded by the NIHR (ICA-CDRF-2018-04-ST2-047). This report is independent research. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, NIHR or the Department of Health and Social Care.
Conflicts of interest
There are no conflicts of interest to declare.
Key practitioner messages
-
(1) Raised health-related worries during the COVID-19 pandemic are normal and do not necessarily require treatment.
-
(2) For some, the level of anxiety experienced during the pandemic may be understood in terms of HA, which is treatable using cognitive behavioural models.
-
(3) Although the majority of research into HA focuses on adults, evidence suggests that children and young people also develop health-related worries and HA, and may be particularly susceptible during global health crises.
-
(4) When treating HA in children and young people, it is important to make development adaptations and consider involvement of parents in treatment.
-
(5) Given the current government mandated measures to manage the spread of COVID-19, alternatives to face-to-face treatment should be considered, such as internet-delivered CBT.







Comments
No Comments have been published for this article.