LEARNING OBJECTIVES
After reading this article you will be able to:
• recognise the various possible associations with pica, both physical and psychiatric
• understand how to approach the assessment of pica
• understand possible treatment options for pica behaviour and the limitations of the current evidence base.
The term pica comes from the Latin word for magpie (McNaughten Reference McNaughten, Bourke and Thompson2017), possibly in reference to the bird's indiscriminate feeding habits. As defined in ICD-11, pica involves regular consumption of ‘non-nutritive substances’ (such as soil, plastic and paper) or raw food ingredients (such as large quantities of flour) to an extent that requires clinical attention and at a developmental age (approximately 2 years) at which the person should be able to distinguish between edible and non-edible substances (World Health Organization 2021). There are other conditions that can involve the abnormal consumption of substances, such as self-harm by consumption of inedible items, hyperorality (‘socially inappropriate licking and a strong compulsion to place objects inside the mouth’; Das Reference Das and Siddiqui2021) and hyperphagia (excessive consumption of food), which may be associated with pica but also occur in its absence.
Pica can be an extremely dangerous behaviour requiring careful assessment and management, but it is not covered in the National Institute for Health and Care Excellence (2017) guidance on the recognition and treatment of eating disorders.
For some people with intellectual disability, pica will be in keeping with their developmental age – indeed, the definition of pica in ICD-10 (World Health Organization 2010) did not include developmental age as a diagnostic criterion. However, pica is a problematic behaviour requiring clinical attention regardless of developmental age and we consider the guidance in this article also to be relevant for this group.
Epidemiology
The groups most commonly affected by pica are children (particularly aged 2–3 years), people with intellectual disability, and pregnant and nursing mothers (often in younger primigravidous women) (McNaughten Reference McNaughten, Bourke and Thompson2017). The more severe the level of intellectual disability, the more common pica is (Matson Reference Matson, Hattier and Belva2011). It has been previously reported to occur in between 5 and 25% of children with intellectual disability (McNaughten Reference McNaughten, Bourke and Thompson2017). A more recent large case–control study of preschool children (aged 30–68 months) identified pica in 28.1% of children with autism and intellectual disability, 23.2% of children with autism and 9.7% of children with intellectual disability, compared with 3.5% of controls (Fields Reference Fields, Soke and Reynolds2021). Pica in young children often remits but it may persist into adulthood, particularly in those with intellectual disability (McNaughten Reference McNaughten, Bourke and Thompson2017).
Associations with pica
A number of physical and neurobiological conditions, mental disorders and social factors have been associated with pica.
Physical and neurobiological conditions
Physical and neurobiological conditions associated with pica are listed in Box 1. Much of the literature on pica is based on case reports, case series and retrospective case-note reviews. There is a dearth of high-quality evidence in the area and it is therefore not possible to attribute causation to associated factors. The causation of pica is therefore unclear and probably multifactorial (McNaughten Reference McNaughten, Bourke and Thompson2017). There have been a number of case reports of pica occurring after gastric bypass surgery and it is suggested that it is linked to poor absorption of iron and iron deficiency anaemia (Tabaac Reference Tabaac and Tabaac2015). However, several studies indicate that the incidence of dietary deficiencies is no more common in children with pica than in those without (Barrett Reference Barrett2008). Some case reports found that pica continued after the deficiencies were corrected (Herguner Reference Herguner, Ozyldrm and Tandr2008; McNaughten Reference McNaughten, Bourke and Thompson2017), whereas others reported that pica resolved completely if, for example, an iron deficiency was corrected (Sinha Reference Sinha and Mallick2010). The role of nutritional deficiencies in pica and whether they are cause or consequence is therefore unclear.
BOX 1 Physical and neurobiological conditions associated with pica
Physical
• Conditions leading to malabsorption, poor nutritional status or anaemia, including gastric bypass surgery and coeliac disease (Gupta Reference Gupta, Rajput and Maduabuchi2007)
• Micronutrient deficiencies (iron/zinc/calcium) (Erickson Reference Erickson, Gambrell and Fulcher2017)
• Malnutrition (Lerner Reference Lerner2008)
• Dental pain (Ayanouglou Reference Ayanouglou, Pernon and Dubois2011)
• Increased appetite due to medication (Erickson Reference Erickson, Gambrell and Fulcher2017)
• Dialysis (Katsoufis Reference Katsoufis, Kertis and McCullough2012)
• Sickle cell anaemia (El-Mekkawy Reference El-Mekkawy, Hosam and Rabah2014)
Neurobiological
• Diminished dopaminergic transmission (Barrett Reference Barrett2008)
• Elevated serotonin levels (Barrett Reference Barrett2008)
• Decreased/increased endogenous opiate (Barrett Reference Barrett2008)
The role of dental pain in causing pica is also unclear. There has been one case report of a child with Pallister–Killian syndrome (a rare chromosomal disorder with features including, among other problems, distinctive dysmorphic facial features and intellectual disability) in whom dental pain was felt to be one of the factors contributing to his pica (Ayanouglou Reference Ayanouglou, Pernon and Dubois2011). However, a study comparing the dental health of children with autism compared with that of controls found no association between the prevalence and severity of caries and additional diagnoses (intellectual disability, cerebral palsy, self-injurious behaviour or pica) (Loo Reference Loo, Graham and Hughes2008).
In terms of medication being linked to pica, there has been one case report of coprophagic asphyxiation in a woman with severe intellectual disability (Erickson Reference Erickson, Gambrell and Fulcher2017). She had high blood olanzapine levels at autopsy and it was postulated that her antipsychotic was a driver of pica. It has been hypothesised that pica is associated with dialysis, possibly related to anaemia, electrolyte derangements or the stress of end-stage renal disease (Katsoufis Reference Katsoufis, Kertis and McCullough2012). There are several possible explanations for the link between sickle cell disease (SCD) and pica. It has been proposed that brain injury resulting from silent infarction can occur in children with SCD, and this could be associated with behavioural difficulties as well as cognitive deficits contributing to the development of pica (El-Mekkawy Reference El-Mekkawy, Hosam and Rabah2014). Also, children with SCD seem to have a greater risk for developing depression compared with those with other chronic conditions such as diabetes, cancer and cystic fibrosis, which may then be linked to pica (El-Mekkawy Reference El-Mekkawy, Hosam and Rabah2014).
Mental disorders
Mental/developmental disorders associated with pica are listed in Box 2. In people with intellectual disability and autism, pica was previously thought to result from their inability to differentiate between food and non-food but is now thought to be likely due to learned behaviours (McNaughten Reference McNaughten, Bourke and Thompson2017). In one study, pica in adults with intellectual disability was associated with severely impaired expressive communication abilities, younger age, autism, poorer cognitive performance, greater aggression and male gender; it was found to be less common in those who had Down syndrome and who did not have impaired self-care skills (Ashworth Reference Ashworth, Hirdes and Martin2009).
BOX 2 Mental/developmental disorders that may be associated with pica
• Intellectual disability (Aksoy Reference Aksoy, Kilic and Demir2014)
• Autism (Aksoy Reference Aksoy, Kilic and Demir2014)
• Fetal alcohol spectrum disorder (Wygant Reference Wygant and Cohle2019)
• Attention-deficit hyperactivity disorder (Herguner Reference Herguner and Herguner2010)
• Obsessive–compulsive disorder (Aksoy Reference Aksoy, Kilic and Demir2014)
• Depression (Erickson Reference Erickson, Gambrell and Fulcher2017)
• Anorexia nervosa (Yalug Reference Yalug, Kirmizi-Alsan and Tufan2007)
• Psychosis (Aksoy Reference Aksoy, Kilic and Demir2014)
• Behavioural phenotype of some genetic syndromes, e.g. hyperphagia in Prader–Willi syndrome (Barrett Reference Barrett2008)
• Neurodegenerative disease (e.g. dementia) (Funyama 2017)
• Acquired brain injury (e.g. Kluver–Bucy syndrome (hyperorality secondary to damage to bilateral medial temporal lobes) (Funayama Reference Funayama, Muramatsu and Koreki2017)
• Sensory processing difficulties (Barrett Reference Barrett2008; Call Reference Call, Simmons and Mevers2015; Liu Reference Liu, Pesch and Lumeng2015)
Fetal alcohol spectrum disorder has been associated with pica (Wygant Reference Wygant and Cohle2019). It is thought that alcohol exposure in utero adversely affects the development of the myenteric plexus, increasing the risk of pseudo-obstruction, which can be exacerbated by pica with potentially fatal consequences such as asphyxia (Wygant Reference Wygant and Cohle2019). It has been suggested that the link between attention-deficit hyperactivity disorder (ADHD) and pica could be due to poor impulse control or dysfunctions in the dopaminergic system (Herguner Reference Herguner and Herguner2010).
As regards neuropsychiatric associations of pica, a study comparing adults with acquired brain injury and no pre-existing neuropsychiatric, developmental or degenerative diseases who demonstrated hyperorality alone with those who demonstrated pica found that those with pica had more severe semantic memory deficits and fewer frontal release signs. Neuroimaging revealed that those with pica all had a lesion in the posterior part of the middle temporal gyrus. It was therefore proposed that in this patient group semantic memory deficits (i.e. a difficulty recognising objects) were associated with pica (Funayama Reference Funayama, Muramatsu and Koreki2017). This is different from the suggested primary mechanism in people with intellectual disability and underlines that pica has many possible underlying aetiologies.
Social/environmental factors
Some see pica as a stand-alone disorder triggered and maintained by operant/environmental factors mainly to seek engagement from others, escape/avoid a disliked situation, as a display of non-social behaviour such as stealing or refusing food or, most commonlythe person enjoys eating the pica item so the behaviour is self-reinforcing (Matson Reference Matson, Hattier and Belva2011) (Box 3).
BOX 3 Social/environmental factors associated with pica
• Imitation (e.g. of a pet or carer) (Barrett Reference Barrett2008)
• Deprivation (McNaughten Reference McNaughten, Bourke and Thompson2017)
• Parental neglect (Gupta Reference Gupta, Rajput and Maduabuchi2007)
• Stress (Gupta Reference Gupta, Rajput and Maduabuchi2007)
• Not having a strong and supportive relationship with family (Ashworth Reference Ashworth, Hirdes and Martin2009)
• Lack of social contact (Ashworth Reference Ashworth, Hirdes and Martin2009; Call Reference Call, Simmons and Mevers2015)
• Absence of participation in activities of prolonged interest (Ashworth Reference Ashworth, Hirdes and Martin2009)
• Absence of involvement in a day programme (Ashworth Reference Ashworth, Hirdes and Martin2009)
• Lack of involvement in recreational activities (Ashworth Reference Ashworth, Hirdes and Martin2009)
Complications of pica
Pica can result in a wide range of complications (Box 4). Evidence indicating that pica has potentially fatal effects, for example that it commonly causes acute abdomen, has been recognised in the literature for a long time. One article reporting on 25 institutionalised individuals with severe intellectual disability treated for acute abdomen found that pica was the cause in 48% of admissions, perforation was seen in 41% and the mortality rate in those with pica was 21% (Voitk Reference Voitk1987). Many items ingested in pica will pass through the gut causing little damage (Stringel Reference Stringel, Parker and McCoy2012), but some can be extremely hazardous. The risk of oesophageal injury from ingesting items such as lithium batteries has been increasingly recognised in recent years (Bolton Reference Bolton, Saker and Bass2018), but seemingly innocuous substances may also be very harmful owing to changes that they undergo in the gastrointestinal tract. For example, vinyl gloves can become hard and sharp enough to cause perforation (Stringel Reference Stringel, Parker and McCoy2012).
BOX 4 Complications of pica
• Death (Erickson Reference Erickson, Gambrell and Fulcher2017)
• Asphyxiation (Erickson Reference Erickson, Gambrell and Fulcher2017)
• Gut obstruction/perforation/abscesses (Stringel Reference Stringel, Parker and McCoy2012)
• Gastric irritation (e.g. when soap is eaten) (Moore Reference Moore2017)
• Need for major GI surgery (Matson Reference Matson, Hattier and Belva2011)
• Malabsorption (e.g. cellulose in paper) (Moore Reference Moore2017)
• Poisoning (e.g. lead, mercury) (Matson Reference Matson, Hattier and Belva2011)
• Electrolyte disturbances (e.g. hypercalcaemia from chalk) (Moore Reference Moore2017)
• Parasitic infestations (when earth/snails eaten), including meningitis (Hsueh Reference Hsueh, Chen and Li2013)
• Dental injury (Ayanouglou Reference Ayanouglou, Pernon and Dubois2011)
Pica can result in poisoning, with lead poisoning being particularly harmful. As well as the effects listed in Box 5, we have encountered hyperactivity in the context of lead ingestion. This highlights that mental disorders can be both a cause and consequence of pica and that behavioural changes in people with intellectual disability need careful assessment for possible underlying organic causes. There has been a single case report of mercury exposure associated with the repeated ingestion of paper treated with a mercury-containing antifungal (Olynyk Reference Olynyk and Sharpe1982). Poor dentition could possibly fuel pica, but pica of hard substances could in itself damage teeth, hindering mastication and contributing to complications such as asphyxiation and gastrointestinal obstruction.
BOX 5 Features of lead toxicity
• Irritability
• Lethargy
• Ataxia
• Headache
• Cranial nerve paralysis
• Papilloedema
• Encephalopathy
• Seizures
(McNaughten Reference McNaughten, Bourke and Thompson2017)
Despite all of these potential complications, in comparison with other types of aberrant behaviour among people with intellectual disability, pica remains under-researched (Matson Reference Matson, Hattier and Belva2011).
Assessment of pica
Pica presents in a variety of forms depending on what the person is eating, and assessment should therefore be tailored to address potential complications of the substance being ingested (McNaughten Reference McNaughten, Bourke and Thompson2017). It is important to ask about coexisting medical conditions that may predispose to pica (as listed in Boxes 1 and 2) and to inquire about symptoms of possible complications or predisposing factors such as anaemia or lead poisoning (McNaughten Reference McNaughten, Bourke and Thompson2017). Thorough developmental and social histories are also important. It is imperative to ask about the living environment to ascertain the likelihood of ingestion of, for example, lead or mercury (McNaughten Reference McNaughten, Bourke and Thompson2017). This may require the involvement of environmental/public health services to identify environmental sources of toxicity.
Physical examination is usually normal; if it is abnormal, this is usually due to the effects of the consumed substance (Boxes 5 and 6) (McNaughten Reference McNaughten, Bourke and Thompson2017). Fig. 1 shows investigations recommended in cases of pica. Many individuals who have pica will have severe levels of intellectual disability, may have extremely limited means of communicating physical symptoms and may find it difficult to engage in assessment. Consequently, comprehensive investigation of possible underlying physical causes of pica is essential before pursuing primarily psychological/psychiatric causes.
BOX 6 Possible signs on physical examination in individuals with pica
• Signs of toxic ingestion e.g. lead.
• Signs of infection or parasitic infection especially toxocariasis
• GI effects – bowel obstruction/perforation
• Dental signs – damage to teeth
(McNaughten Reference McNaughten, Bourke and Thompson2017)
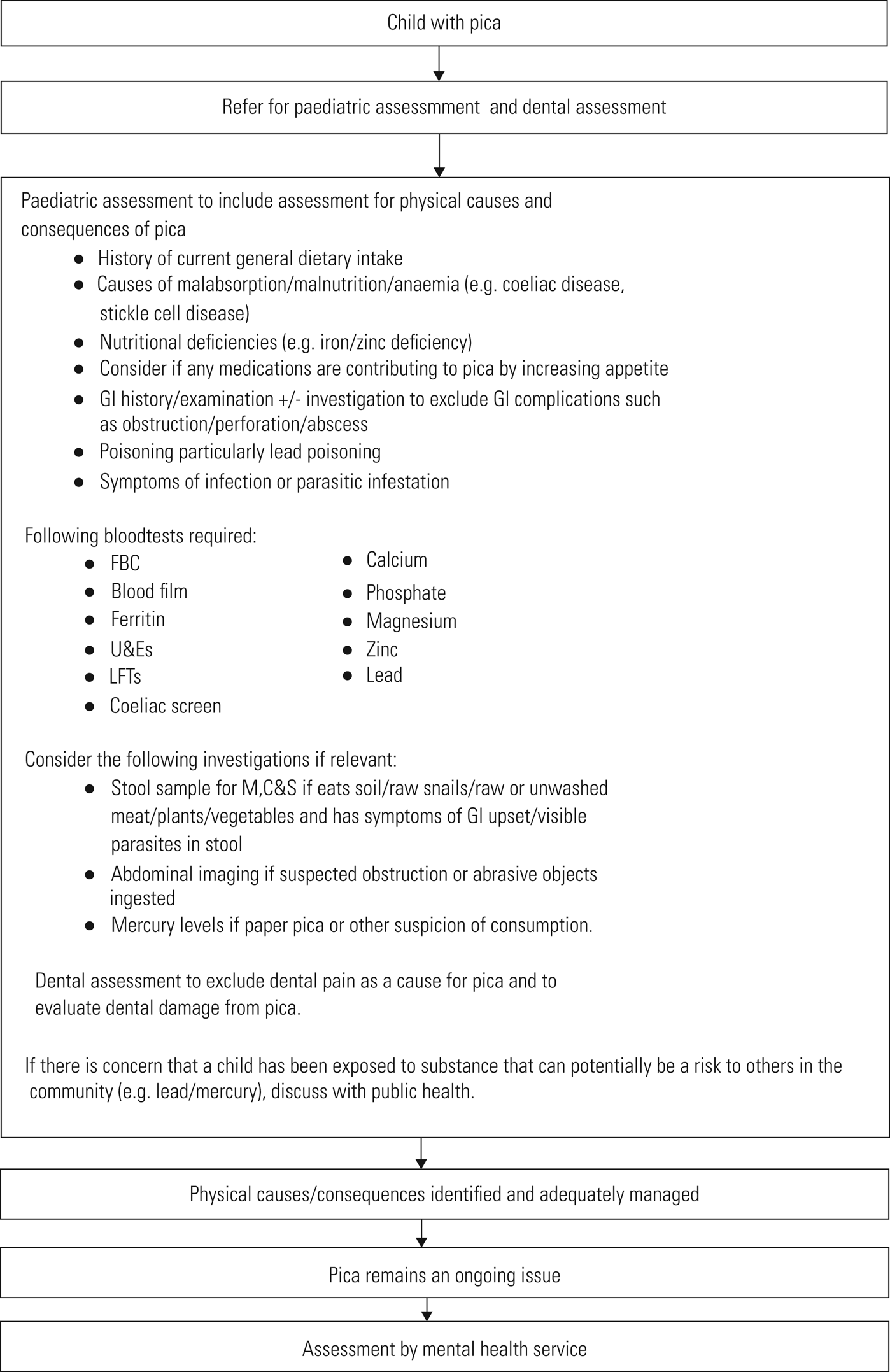
FIG 1 The following guidance is based on the NHS Fife management pathway for children with intellectual disability who have pica (details available from the corresponding author on request). These recommendations are based on clinical agreements in the NHS Fife health board which expanded upon guidance from the NHS Greater Glasgow and Clyde health board and McNaughten (Reference McNaughten, Bourke and Thompson2017).
Once physical causes are excluded, psychiatric/psychological assessment is indicated to try to ascertain what is driving the pica behaviour. This should include functional/behavioural assessment and analysis and might involve baiting (Call Reference Call, Simmons and Mevers2015). Functional analysis of antecedents, behaviour and consequences can help identify potential operant factors maintaining/triggering the behaviour, which can then inform behavioural management. Baiting involves putting edible and inedible items in view of the person to allow observation then intervention as the pica is occurring. Imitations such as cigarettes made of herbal tea may be used in place of harmful pica items (Williams et al Reference Williams, Kirkpatrick-Sanchez and Enzinna2009; Matson Reference Matson, Hattier and Belva2011).
Treatment of pica
General treatment
In young children and pregnant women, pica usually remits spontaneously. Management of persistent pica should involve a multidisciplinary approach including speech and language therapists, occupational therapists, physicians, social workers, dieticians, psychologists and dentists (McNaughten Reference McNaughten, Bourke and Thompson2017). It is important to treat any associated physical conditions first, such as nutritional deficiencies, toxicity, parasitic infections, obstruction and dental problems. Thereafter, interventions should be primarily behavioural in nature (Matson Reference Matson, Hattier and Belva2011). There is only limited evidence to support pharmacological interventions in the management of pica (Matson Reference Matson, Hattier and Belva2013).
General treatment of pica includes:
• education for parents/carers/patients about pica and good nutritional practices (McNaughten Reference McNaughten, Bourke and Thompson2017)
• making parents/carers/patients aware of the potential severity of the condition (McNaughten Reference McNaughten, Bourke and Thompson2017)
• supervision of the patient
• removal of pica items from the environment wherever possible (Barrett Reference Barrett2008)
• an assessment of the patient's capacity to decide what they eat and drink, which will inform the extent to which restrictive practices can be used to manage the pica (Hayes Reference Hayes and Boulter2019).
Behavioural treatment and physical intervention
Possible behavioural interventions for pica are listed in Box 7. Aversive methods for reducing pica have been described in the literature but in today's practice these are unlikely to be considered ethical and so are not included in this article. Most studies of behavioural treatments for pica are small (Call Reference Call, Simmons and Mevers2015), not of robust research design and many are old, so there is limited strong evidence about the best treatment. It is therefore difficult to make any strong recommendations about which of the interventions described below is best. Furthermore, as described above, the possible causes of pica are diverse, so treatment is best tailored to the features of the individual. Therefore, the information in this section is provided to inform clinicians of possible interventions rather than to recommend any particular approach.
BOX 7 Behavioural interventions for pica
• Physical interventions (Matson Reference Matson, Hattier and Belva2013)
• Positive reinforcement (Matson Reference Matson, Hattier and Belva2013)
• Pica exchange (Carter Reference Carter2009)
• Discrimination training (McNaughten Reference McNaughten, Bourke and Thompson2017)
• Environmental enrichment (Matson Reference Matson, Hattier and Belva2013)
• Response blocking with redirection (Liu Reference Liu, Pesch and Lumeng2015)
• Occupational therapy input if pica might be due to a sensory issue (Liu Reference Liu, Pesch and Lumeng2015)
• Exposure and response prevention if part of obsessive–compulsive disorder (Aksoy Reference Aksoy, Kilic and Demir2014)
Several studies have found benefit in positive reinforcement (i.e. if pica is not attempted or an alternative behaviour is carried out) (Matson Reference Matson, Hattier and Belva2013). Pica exchange involves teaching the person to exchange the pica item for another item. In a case study of two boys (Kern Reference Kern, Starosta and Adelman2006) with developmental disabilities, they were taught to hand over a particular pica item for a potato crisp (previously identified as a preferred food item). The exchange started on 1:1 ratio, after which the ratio was reduced to 2:1, then to 3:1. Next, a delay in response was added and the exchange was subsequently extended to other pica items. Pica levels were reduced to near zero. In another case study using pica exchange for preferred food items (such as chocolate, biscuits, coffee and diet soft drink), the distance the individual (a 72-year-old woman) had to move to do the exchange was gradually increased until the exchanger was in the next room. This reduced pica to near zero but took 2 years (Carter Reference Carter2009). There are issues about ensuring the item being exchanged for is not too unhealthy, and indeed unhealthy items were used in both these cases.
Discrimination training involves teaching the person the difference between edible and non-edible substances (McNaughten Reference McNaughten, Bourke and Thompson2017). Environmental enrichment can involve providing alternative stimulating food (e.g. highly spiced and flavoured) and also offering stimulating activities, in combination with non-contingent reinforcement (Matson Reference Matson, Hattier and Belva2013). A number of studies have found this helpful (Matson Reference Matson, Hattier and Belva2013). More broadly speaking, given the influence of social/environmental factors on pica and in behavioural difficulties in general, providing an individual with meaningful activities in a safe environment is likely to be important in most, if not all, people with pica. One study found response blocking with redirection to be successful. This involved removing pica targets from the hands or gently blocking the mouth, combined with redirection to a preferred food item or activity (Liu Reference Liu, Pesch and Lumeng2015). Another study found response blocking helpful only if it was combined with an alternative reinforcer (e.g. popcorn) and that otherwise it led to aggression (Hagopian Reference Hagopian and Adelinis2001). Some small, older studies from the 1970s, 1980s and 1990s found restraint helpful in reducing pica, but other studies found alternative methods to be as effective, such as providing staff interaction when the function of the pica was to seek engagement (Matson Reference Matson, Hattier and Belva2013). In some individuals pica may be related to sensory processing problems and input from occupational therapy may be helpful. For example, if the person has oral hyposensitivity, an occupational therapist would be able to recommend safer yet meaningful ways to fulfil this sensory need, such as ‘chewellery’ or similar-textured food items to avoid pica or substitute for the pica item.
As mentioned above, the existing studies into behavioural interventions for pica have small samples (Hagopian Reference Hagopian, Rooker and Rolider2011; Call Reference Call, Simmons and Mevers2015), but it is often thought that behavioural interventions can be very effective (McNaughten Reference McNaughten, Bourke and Thompson2017). One review paper found that 80.7% of identified studies reduced pica by more than 90% relative to baseline (Hagopian Reference Hagopian, Rooker and Rolider2011). Some argue, however, that a 90% reduction is not enough, given the potentially fatal consequences of pica (Williams Reference Williams and McAdam2012). Many studies did not provide results after long-term follow-up and there may be a problem with publication bias. Also, in many studies the interventions were carried out in a single, often clinical or institutional, setting rather than a natural setting. Although this is necessary for research, it makes it more difficult to extrapolate the findings to community settings.
Furthermore, all the interventions are intensive and require significant resources. A retrospective follow-up study over 9 years of 41 residents of an institution with intellectual disability and pica who had received both various forms of behavioural management and comprehensive management of the environment (i.e. limiting access to items small enough to be eaten) found that 85% showed a 75–100% reduction in pica. However, it was noted that, owing to the measures put in place to manage the pica, these residents led a more constricted life, as they did not go out much or have as many external activities and social opportunities as other residents (Williams Reference Williams, Kirkpatrick-Sanchez and Enzinna2009).
Given the potentially fatal consequences of pica, restrictive practices may be warranted. Judgement therefore needs to be made on an individual basis about whether the level of risk justifies the level of restriction; this is particularly relevant when considering the use of physical interventions such as those listed in Box 8. It is also essential to ensure that any use of restrictive practices is authorised by the relevant legislative framework of the jurisdiction in which the patient lives (e.g. the Adults with Incapacity (Scotland) Act or the Deprivation of Liberty Safeguards under the Mental Capacity Act 2005 for England and Wales).
BOX 8 Physical interventions for pica
• Self-protection devices that prohibit placement of objects in the mouth (McNaughten Reference McNaughten, Bourke and Thompson2017), e.g. helmets, masks and splints
• Physical restraint (Matson Reference Matson, Hattier and Belva2013)
• Time out if pica is attempted (Matson Reference Matson, Hattier and Belva2013; McNaughten Reference McNaughten, Bourke and Thompson2017)
Pharmacological treatment
As with most challenging behaviours, pharmacological treatment is rarely indicated (McNaughten Reference McNaughten, Bourke and Thompson2017), unless it is aimed at treating underlying mental illness. Studies and case reports of pharmacological treatments for pica in people with intellectual disability are summarised in Table 1. As with behavioural interventions for pica, the evidence base is poor and tends to be limited to a small number of uncontrolled case reports/series.
TABLE 1 Pharmacological treatments reported in the literature for pica in people with intellectual disability
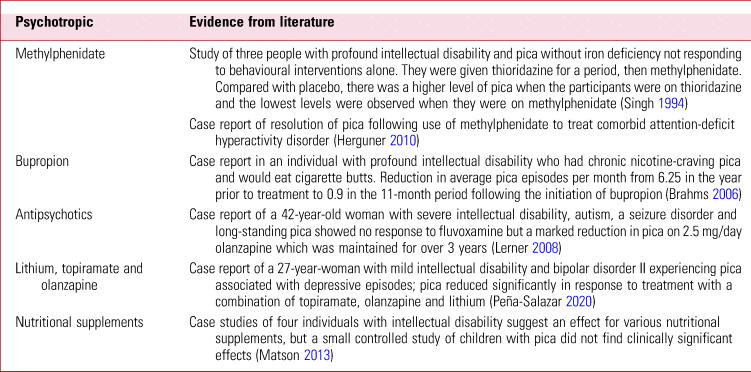
Notably the studies involving individuals with comorbid ADHD have suggested a role for dopamine in pica. In the first case series mentioned in Table 1, there was a suggestion that diminished dopamine transmission had a role in the maintenance and exacerbation of pica, hence the worsening on thioridazine (Singh Reference Singh, Ellis and Crews1994). In the other case report it was postulated that stimulants improved pica by increasing dopamine levels and reducing impulsivity (Herguner Reference Herguner and Herguner2010).
There have been case reports of the successful use of other psychotropics in pica, such as asenapine in a woman with anxiety, depression and personality disorders (Tabaac Reference Tabaac and Tabaac2015), selective serotonin reuptake inhibitors (SSRIs) for pica associated with obsessive–compulsive disorder (OCD) (Gundogar Reference Gundogar, Baspinar Demir and Eren2003; Herguner Reference Herguner, Ozyldrm and Tandr2008) and venlafaxine for pica associated with depression (Mehra Reference Mehra, Sharma and Grover2018), but these studies were carried out in patients without intellectual disability so the findings may not be relevant to this patient group.
Conclusions
Pica is a challenging behaviour that has potentially serious, and possibly fatal, consequences. The case study in Box 9 demonstrates some of the complexity of managing it. It is like other challenging behaviours in that it has various biological, psychological and social associations and causes. It is important to routinely ask about pica during physical and mental health assessments of ‘at risk’ groups.
BOX 9 Case studya
Jake is a lively young man with severe intellectual disability and autism. He loves water and has a range of sensory-seeking behaviours and sensory sensitivities. Jake has displayed hyperactivity, severe sleep disturbance and agitation, with food-seeking, aggressive and destructive behaviour since early childhood. His dedicated family made huge changes to the home environment to reduce sensory overstimulation and risk, e.g. locking food cupboards, keeping blinds closed and removing taps when not in use. Jake presented to psychiatry already on aripiprazole and clonidine for these problems. A detailed history revealed unrecognised severe constipation and overflow diarrhoea. Jake would have been unable to manage in a hospital setting so his family supported a disimpaction regime at home. He subsequently passed a whole banana skin including the stalk, leading to a significant improvement in well-being and behaviour. However, it took many months for Jake to regain continence, greatly increasing his care needs.
Jake's pica had previously been unrecognised – he was secretive when eating non-food items and he had used the toilet relatively independently. His incontinence revealed that a wide variety of items had been eaten, including: stones; plastic seals from pipes; parts of headrests and mattress covers; foam from mattresses; and rubber/wooden doorstoppers. This was despite a high level of observation and vigilance of family and carers. Consideration was given to endoscopy/scans to see whether there were items still in his gut, but it was not thought that the general anaesthetic required would be justified as it would have been unlikely to alter his management unless presenting with symptoms of an acute abdomen. He was treated empirically for H. Pylori.
Jake often ate items with silicone/rubbery textures and attempts were made to meet this apparent sensory need in safer ways. Chewellery (jewellery designed to be chewed by those who experience oral hyposensitivity) was unsuccessful as this is designed for small children and Jake was able to bite right through it. Dog chews were tried instead but he did not accept them. Family, school and respite carers primarily managed Jake's pica through close observation and offering him edible items when he was seeking non-food items. This was not entirely successful owing to his drive and secrecy around pica. Careful bowel monitoring and management of constipation and abdominal pain helped reduce agitated and aggressive behaviours, although these remained intermittently severe in association with abdominal pain. It was recognised that Jake's psychotropic medication may have contributed to his constipation. Improvements in agitation made it possible to wean Jake off aripiprazole, but he continued to require clonidine for hyperactivity and sleep disturbance.
Jake subsequently cracked a tooth (probably secondary to eating stones) and required a general anaesthetic to allow dental treatment. The induction process was extremely difficult, and despite significant amounts of sedation, restraint by multiple staff members was required. The state of Jake's teeth meant that total dental clearance was required. Following this Jake was able to eat food well and there was a dramatic and sustained reduction in pica. Jake's pica may have contributed to the dental problems, but the pica may have escalated as he then used it to attempt to soothe his dental pain. Unfortunately, the pica subsequently gradually increased again and ongoing close supervision and monitoring is required.
a. Written consent to publish this case study was provided by the welfare guardian. The patient's real name has not been used.
The evidence base for treatment is poor, as it is gathered largely from single cases, case series and retrospective case reviews which have lacked controls. Treatment should be tailored to the individual. It is essential to first identify and treat any underlying physical health condition. A flowchart for doing so is shown in Fig. 1. Once associated physical health conditions are excluded, behavioural/environmental interventions should be the mainstay of treatment. Psychotropic medication can be helpful in the few cases where an underlying psychiatric diagnosis accounts for the pica.
Further research to provide a basis for development of tools and resources to guide management of pica is required. In the meantime, a positive behaviour support plan (PBSP) may provide a helpful framework to incorporate a number of the treatment strategies mentioned in this article, such as functional analysis, sensory input, pharmacological approaches and environmental enrichment.
Acknowledgement
We thank Fiona Vaughan, occupational therapist, NHS Fife, for her contribution regarding sensory assessment and intervention in pica.
Author contributions
F.W. conducted the literature review and wrote the original draft and subsequent drafts. S.G. wrote the case vignette and assisted in reviewing and amending the drafts. A.S.A. assisted reviewing and amending the drafts.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bja.2022.24.
MCQs
Select the single best option for each question stem
1 Pica:
a is especially prevalent in postmenopausal women
b usually has an easily identifiable single cause
c in younger children usually does not remit without intervention
d is always culturally inappropriate
e occurs in up to 25% of children with intellectual disability.
2 As regards the causes of pica:
a it has been commonly associated with iron deficiency
b there is a large body of robust evidence that identifies the causes of pica
c it is never associated with underlying physical health problems
d it has never been associated with use of medications
e it is never associated with underlying mental disorder.
3 The following has not been described as a complication of pica:
a poisoning
b bowel carcinoma
c gut perforation
d death
e dental damage.
4 The initial investigation of pica should include:
a blood tests for urinary Bence Jones protein
b podiatry review
c MRI of the abdomen
d blood tests for trace elements
e skin biopsy.
5 Pharmacological treatments successfully tried for pica in people with intellectual disability have included:
a atomoxetine in ADHD
b SSRIs in OCD
c bupropion in nicotine craving
d quetiapine in schizophrenia
e clozapine in treatment-resistant schizophrenia.
MCQ answers
1 e 2 a 3 b 4 d 5 c






eLetters
No eLetters have been published for this article.