Psycho-oncologic trauma is defined as a deeply distressing or disturbing experience related to the experience of being diagnosed with, or treated for, cancer,Reference Abbey, Thompson, Hickish and Heathcote1 and is a risk factor for developing post-traumatic stress disorder (PTSD).Reference Kwakkenbos, Coyne and Thombs2 Cancer-related PTSD is defined as patients who become re-traumatised by here-and-now experiences (such as having cancer) and/or through evoking past traumatic experiences (typically relating to adverse issues pertaining to social deprivation, comorbidities and psychologic trauma from neglect and abuse). There is evidence that cancer-related outcomes may be negatively associated with pre-cancer diagnosis PTSD as a result of adverse childhood experiences and adverse adulthood experiencesReference Brown, Thacker and Cohen3 (see Felitti et alReference Felitti, Anda, Nordenberg, Williamson, Spitz and Edwards4 for their definition and measurement). Prevalence estimates of cancer-related PTSD range between 7 and 14%,Reference Abbey, Thompson, Hickish and Heathcote1 with an additional 10–20% of patients experiencing subsyndromal post-traumatic stress symptoms.Reference Andrykowski, Cordova, Studts and Miller5,Reference Shelby, Golden-Kreutz and Andersen6 There is a developing evidence base in understanding trauma experiences among people living with cancer, and the effect these trauma experiences have on health and well-being outcomes.Reference Henson, Brock, Charnock, Wickramasinghe, Will and Pitman7,Reference Regal, Wheeler, Daire and Spears8 Consequently, mental health services for patients with cancer are urged to accommodate the needs for patients with current and/or past traumatic experiences.9
PTSD is known to reduce quality of life in people living with cancerReference Shand, Cowlishaw, Brooker, Burney and Ricciardelli10 and concordance with cancer care, such as drug adherence; this negatively effects morbidity and mortality.Reference Neigh and Ali11,Reference Cavalcanti-Ribeiro, Andrade-Nascimento, Morais-de-Jesus, de Medeiros, Daltro-Oliveira and Conceição12 There is considerable diagnostic heterogeneity and diagnostic overlap in this group of patients, who may present to cancer services with pre-existing PTSD, and those that develop de novo PTSD as a result of their cancer experience.Reference Smith, Zimmerman, Williams, Benecha, Abernethy and Mayer13 Recent authors have commented on the alteration of criteria in the DSM-5, and argue that cancer may not necessarily constitute a traumatic event if no sudden or catastrophic events occur.Reference Cordova, Riba and Spiegel14,Reference Dimitrov, Moschopoulou and Korszun15 It has also been suggested that careful consideration ought to be paid to distinguishing between PTSD and adjustment disorder, anxiety and depression, and that cancer-related PTSD remains a complex diagnostic issue.Reference Dimitrov, Moschopoulou and Korszun15 This diagnostic ambiguity is relevant given the complexity of mental health problems in patients that is further compounded by risk factors for pre-existing PTSD, which include deprivation, adverse childhood experiences and adverse adulthood experiences.Reference Nelson, Zulfiqar and Burke Harris16 (The DSM-5 criteria for PTSD are: stressor, intrusion symptoms, avoidance, negative alterations in cognitions or mood, alterations in arousal and reactivity, duration and functional significance.17)
PTSD is known to be prevalent (14%) in the oncology population, alongside other psychiatric comorbidities such as depression (16.3%), adjustment disorder (19.4%) and anxiety (10.3%).Reference Chaturvedi, Uchitomi, Grassi and Riba18 Although concordance with cancer treatment is important, it is also known that when patients have mental health problems, their physical health outcomes in general are worse.Reference Grassi and Riba19–Reference Osborn21 This narrative review will update the evidence base for psychological interventions in patients living with cancer-related PTSD and part of addressing these needs in the psychiatric population.
Method
This narrative review identified the evidence base of existing and applicable psychological approaches to cancer-related PTSD that can translate across to people living with cancer (Quality Improvement and Clinical Audit Committee 3055).
Narrative literature review approach
A narrative literature review aims to answer a specific clinical question by using defined criteria for the literature search. The results of the search are then reviewed and critiqued for the quality of the evidence. The question posed was: ‘What are the evidence-based psychological approaches to PTSD in people living with cancer?’. To answer the question, the PICO method was used, which addresses the population of interest (P), the intervention to be considered (I), the relevant control population or intervention (C) and the outcomes (O).22 The PICO method was therefore formulated with P as patients with cancer and post-traumatic stress symptoms (PTSD), I as psychological approaches to PTSD, C as patients with cancer without PTSD and O as improvement in PTSD symptoms and/or engagement into cancer care.
PTSD as the primary outcome was defined with the criteria determined by specific psychometric tools: Structured Clinical Interview for DSM-IV or -5 (SCID),17 Clinician-Administered PTSD Scale (CAPS),Reference Blake, Weathers, Nagy, Kaloupek, Gusman and Charney23 Post-Traumatic Diagnostic Scale (PDS),Reference Foa, Cashman, Jaycox and Perry24 Short Post-Traumatic Disorder Rating Interview (SPRINT),Reference Connor and Davidson25,Reference Horowitz, Wilner and Alvarez26 the Impact of Events Scale (IES)Reference Horowitz, Wilner and Alvarez26 or revised Impact of Events Scale (IES-R),Reference Weiss, Marmar, Wilson and Keane27 and the PTSD Checklist (both the civilian version and revised versions) (PCL-C).Reference Blanchard, Jones-Alexander, Buckley and Forneris28 By doing so, this updated narrative review is consistent with the psychometric tools used in the two previous reviews.Reference Dimitrov, Moschopoulou and Korszun15,Reference Nenova, Morris, Paul, Li, Applebaum and Duhamel29
Search strategy
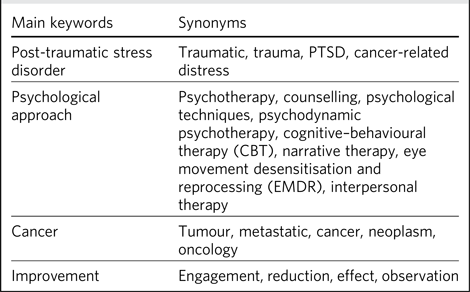
Each database was searched for keywords and results were added to the synonym column (see Table 1).
Table 1 Search strategy

Inclusion and exclusion criteria
Papers were included if the following criteria were met: the study was published in a peer-reviewed journal; the entire paper published in the English language; it was a primary research paper; the study was related to cancer; the study addressed the relationship between cancer and PTSD, using the validated psychometric tools from the two previous reviews; and studies using mixed tools to measure multiple psychiatric diagnoses were included if the outcome data presented those scoring highly specifically for PTSD.
Studies that did not meet the above criteria were excluded after inspecting the title and abstract. For those studies that were included, entire papers were obtained and assessed for eligibility. There was a preference for papers published in the past 20 years, to provide the most relevant evidence-based for current cancer care.
Databases searched
A narrative review of healthcare databases was conducted in December 2021. The following electronic databases were subsequently searched: Medline (general medical database), EMBASE (Excerpta Medica Database), CINAHL (Cumulative Index to Nursing and Allied Health Literature), PsycINFO (Psychology and Allied Fields), BNI (British Nursing Index) and PubMed (general medical database). Medical Subject Headings (MeSH), keywords and synonyms used are detailed in Table 1. Each paper was reviewed for usefulness, and general review papers, single-case studies and non-intervention papers were excluded. Papers that had been included in previous reviews were included as part of previous narrative and systematic review papers, but were not separately considered so as to avoid duplication and were therefore excluded from the search.
Data extraction
An analytical framework was created to extract relevant themes. Data was recorded on standardised forms that checked eligibility, recorded the details of the paper and extracted the main themes. The two authors (D.A. and V.J.) independently performed the data extraction, using a standardised form. The results were organised by author, year of publication, objective, study design and results. Papers were then critically appraised with a standardised method (Critical Appraisal Skills Programme checklists).30 This tool has been validated to ensure a standardised rigour to the approach. The following variables were extracted and used to focus each review to the specific aim of the study:
(a) general: author, year, title, journal, country, total number of participants and study design;
(b) participants: gender, age range, cancer type and PTSD psychometric tool used in the study;
(c) intervention: type of intervention, frequency, delivery mode (face to face, telephone, group or individual), randomisation method if discussed, drop-out data;
(d) results: main outcome measures, narrative findings and effect sizes if available.
The risk of bias was examined for each paper. National Institutes of Health quality assessment tools were used for controlled intervention studies, randomised controlled trials (RCTs), case series and studies with no control group. One narrative review had already performed a quality assessment with such tools and was therefore not repeated.Reference Dimitrov, Moschopoulou and Korszun15 A meta-analysis was not possible because of the clinical variability of the interventions and outcomes measures, as well as methodological variability. Measures used include the PTSD Symptom Scale, SCID (for the DSM-IV), PCL, IES, SPRINT, CAPS, PDS and Posttraumatic Stress Syndrome Scale. Of the individual studies, two commented on the cut-off score used,Reference Rissanen, Nordin, Ahlgren and Arving31,Reference Roberts32 whereas others did not comment on cut-off scores at all, rather discussing the comparison in scores pre- and post-intervention.
Results
Table 2 and Fig. 1 detail the results of the narrative review, and Table 3 shows the quality assessment of the studies.
Table 2 Summary of included papers

PTSD, post-traumatic stress disorder; PSS, PTSD Symptom Scale; COMET, competitive memory training; MEST, memory specificity training; CBT, cognitive–behavioural therapy; PCL, PTSD checklist; SCID, Structured Clinical Interview for DSM-IV or -5; RCT, randomised controlled trial; IES, Impact of Event Scale (original or revised); PPT, positive psychotherapy technique; EMDR, eye movement desensitisation and reprocessing; SPRINT, Short Post-Traumatic Disorder Rating Interview; CAPS, Clinician-Administered PTSD Scale; PDS, Post-Traumatic Diagnostic Scale; PTSS, Posttraumatic Stress Syndrome Scale.
Table 3 Quality review

NIH, National Institutes of Health.

Fig. 1 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) summary. The following electronic databases were searched: Medline (general medical database), EMBASE (Excerpta Medica Database), CINAHL (Cumulative Index to Nursing and Allied Health Literature), PsycINFO (Psychology and Allied Fields), BNI (British Nursing Index) and PubMed (general medical database). PTSD, post-traumatic stress disorder.
Of the 11 included papers, the studies broadly fell into three distinct groups: predominantly cognitive–behavioural therapy (CBT)-based studies, predominantly eye movement desensitisation and reprocessing (EMDR)-based studies and other modalities. Two studies provided an overview of treatment in cancer-related PTSD, through narrative reviewReference Dimitrov, Moschopoulou and Korszun15 and a review of RCTs.Reference Nenova, Morris, Paul, Li, Applebaum and Duhamel29 The narrative review examined eight studies that address EMDR, CBT, complimentary therapies and counselling over a range of formats, such as individual, group, self-management and telephone therapy. The review of RCTs examined 19 studies that used CBT in various formats (individual, group and couples); 68% of these studies were found to not be helpful in cancer-related PTSD. Although there was significant heterogeneity between the studies, individual EMDR seemed to have the best evidence when trialled head-to-head with CBT.
One study used a CBT approach,Reference Rissanen, Nordin, Ahlgren and Arving31 one study used EMDRReference Roberts32 and one study focused on acceptance and commitment therapy.Reference Sarizadeh, Boogar, Talepasand and Gharemanfard33 Finally, six studies used novel approaches, including neuro-emotional techniques, cognitive–emotional training, competitive memory training, meditation, ‘positive psychotherapy techniques’ and expressive writing.Reference Monti, Stoner, Zivin and Schlesinger34–Reference Chu, Wu and Lu39 There were noticeable differences in type of intervention, participant characteristics and outcome assessments across the studies. Duration of intervention also differed, ranging from 3 weeks to 22 weeks, and post-intervention follow-up varied from 90 days up until 12 months.
There was a large variability in types and stages of cancer studied, ranging from haematological malignancies to oral cancer, and some studies focused on one cancer type only, whereas others included participants with a range of different cancers. There was also considerable variability in patient demographics, including gender, age and social circumstances. These factors contribute to notable heterogeneity in this narrative review.
CBT and derivative approaches
An outcome of the narrative review by Dimitrov et alReference Dimitrov, Moschopoulou and Korszun15 examined CBT versus other modalities, including EMDR (both individual and group), counselling, complimentary therapy and psychoeducation. Telephone CBT was compared with a resource workbook done over ten sessions across 10–16 weeks). No control group was included; however, it seemed that telephone CBT provided the best outcome. CBT was also compared with counselling (six sessions over 6 weeks, with a booster session at 10 weeks), with CBT resulting in the best improvement for PTSD symptoms.
Nenova et alReference Nenova, Morris, Paul, Li, Applebaum and Duhamel29 reviewed several randomised controlled trials that used CBT for cancer-related PTSD (19 studies in total). A range of interventions were examined that used group, couples and individual formats. Additional techniques to modify the CBT included mindfulness, psychoeducation, self-management and anxiety management. Control groups varied across the included studies, including wait-list controls, day-long seminars, treatment as usual, a psychological assessment only, an unstructured psychoeducational support group, supportive counselling, resource directory booklet provision, unstructured supportive counselling, medical information education (no psychological intervention) and coping skills training. In terms of effectiveness, 68% of studies found no an effect on cancer-related traumatic stress symptoms. Four studies found intervention participants experienced reductions in intrusion, avoidance and hyperarousal symptoms compared with controls. One study found a reduction in intrusion and avoidance, but not numbing or hyperarousal; however, participants were less likely to meet the diagnostic criteria for PTSD at 12-month follow-up in the intervention group.
One study found that a CBT-based support group led to greater reductions in re-experiencing symptoms and arousal, but not in avoidance, when compared with complementary and alternative medicine intervention. Overall effect size analysis showed intervention effects were small and ranged from −0.138 to 0.006 for intrusion, and from −0.025 to 0.048 for avoidance. Effect sizes indicated interventions with CBT components did not have a statistically significant effect on either intrusion or avoidance scores.
There were three studies included in this review that used CBT-derivative approaches to modify the original CBT technique. Hamidian et alReference Hamidian, Rezaee, Shakiba and Navidian35 adopted a CBT-derivative approach using so-called group cognitive–emotional training (five sessions delivered twice weekly) compared with treatment as usual, in a cohort of 85 participants. The mean PTSD score in post-test and the mean changes in stress score of the intervention group were significantly less than those in control group. Pre-study PTSD scores were similar in both groups. Farahimanesh et alReference Farahimanesh, Moradi, Sadeghi and Jobson36 compared so-called competitive memory training (seven sessions delivered weekly) and memory specificity training (six sessions delivered weekly). Both interventions appeared to be a combination of CBT and psychoeducation, with the first group more cognitively focused on self-perceptions and the second group focusing on recall of memories. It was not clear within the paper what the interventions used as a psychological approach, and there were no control groups for comparison. Finally, Rissanen et alReference Rissanen, Nordin, Ahlgren and Arving31 performed an RCT of stepped-care stress management that is described as educationally based and uses CBT techniques. Their intervention compared group stress management and a similar individual approach, with a one-off education event used as a control. However, both interventions were not effective for cancer-related PTSD.
EMDR
In their narrative review, Dimitrov et alReference Dimitrov, Moschopoulou and Korszun15 also compared individual EMDR and CBT (delivered weekly for 8 weeks), with EMDR yielding the best outcomes. Participants had numerous cancer types (breast, colon, uterus, thyroid, melanoma, lung and stomach). Analysis showed that EMDR was equally effective in reducing PTSD symptoms in patients undergoing active treatment in addition to those in follow-up treatment. The authors concluded the study was at unclear risk of bias after assessment with a Cochrane quality tool, and the sample size was small, with participants predominantly being female and in their 50's. The review also included a study examining a group EMDR approach of six sessions over 3 days, but no control was mentioned in this study. RobertsReference Roberts32 performed case study research using group EMDR with 35 patients, comparing the treatment group with a delayed treatment group (1 month later). The results were unclear if the intervention was successful, but pre- and post-intervention scores appeared significantly better and were maintained at 90 days.
Other therapeutic modalities
A broad range of other psychological approaches in cancer-related PTSD have been tried. Dimitrov et alReference Dimitrov, Moschopoulou and Korszun15 examined telephone counselling with a resource booklet (16 sessions delivered over 12 months) against the resource booklet alone, with counselling yielding the best outcomes. Complimentary therapy (delivered twice weekly for 12 months) was also compared with a standard support group (delivered weekly for 12 weeks), with the support group showing the best outcomes. Monti et alReference Monti, Stoner, Zivin and Schlesinger34 performed case study research with seven patients, using a novel approach they termed the ‘neuro-emotional technique’ delivered over three sessions, which seems to be a blend of behavioural and cognitive techniques. ‘Short-term relief' of symptoms was noted as an outcome.
Offidani et alReference Offidani, Peterson, Loizzo, Moore and Charlson37 examined a 4-week programme of meditation aimed at improving attention and awareness while building essential skills to deal with stress. A control group was not included. The findings were unclear, but the authors suggested that patients with chronic stress report greater improvement in IES scores than those without stress symptoms using self-meditation techniques. There were specific improvements in the intrusive thoughts score and avoidance score that were statistically significant. Ochoa et alReference Ochoa, Casellas-Grau, Vives, Font and Borràs38 also used a so-called positive psychotherapy technique (12 weekly sessions of 90–120 min duration). The sessions focused on the assimilation of the cancer experience and encouraged personal transformation and psychological growth from the illness experience, using a manualised programme and guide. 126 patients were allocated to the experimental treatment, with patients also allocated to a waiting list control for 3 months. The intervention appeared to promote post-traumatic growth and reduced post-traumatic stress, with the benefits maintained at the 3- and 12-month follow-up.
Sarizadeh et alReference Sarizadeh, Boogar, Talepasand and Gharemanfard33 trialled acceptance and commitment therapy over 8 weeks, delivered as weekly sessions. This trial included a patient group and a survivors’ group. The same two groups were used for controls, with controls offered four sessions of treatment after completing the study. Acceptance and commitment therapy was effective in reducing demoralisation and cancer-related trauma symptoms in patients with breast cancer and in survivors. Finally, Chu et alReference Chu, Wu and Lu39 examined a group-based expressive writing intervention that relied on cognitive reappraisal techniques and emotional disclosure. Three types of writing groups were examined: ‘cancer-fact’ (objective writing about cancer experiences), self-regulation and enhanced self-regulation. Significant differences in PTSD symptoms for all groups were noted. There were no significant differences in follow-up at 1, 3 and 6 months.
Discussion
Group cognitive emotional work appears useful when compared with treatment as usual, and group CBT is also helpful in reducing cancer-specific thought intrusions. EMDR appears useful when compared with treatment as usual. When compared with individual CBT, EMDR appears to perform better. CBT appears to be more effective than counselling, which is more useful than a support booklet. Expressive writing intervention is also useful for hyperarousal and re-experiencing symptoms. Acceptance and commitment therapy is effective in reducing demoralisation and cancer-related trauma. Supportive care (including a one-off clinical appointment and telephone support over 2 months) is effective in reducing post-traumatic stress symptoms compared with controls. Positive psychotherapy intervention, focused on personal transformation and assimilation of cancer experience, promotes post-traumatic growth and reduces post-traumatic stress; the improvements were maintained at 1-year follow-up. It is unclear if meditation intervention worked for PTSD, although the authors did report that patients with chronic stress reported improvements as a result of the intervention.
Implications
No studies in this review mentioned the use of patient and public involvement (PPI) in their study design. PPI is a growing field, and tools like the Involvement Matrix lay out processes to engage patients in study design, from preparation through to implementation.Reference Smits, van Meeteren, Klem, Alsem and Ketelaar40 This review highlights the need to integrate PPI into study development, to ensure that patient and public views are captured and integrated into PTSD and cancer research. In addition to lack of PPI, this review highlights a lack of high-quality screening or robust interventions for cancer-related PTSD. A variety of approaches are used in the studies, including desensitisation and complimentary therapies, EMDR, expressive writing interventions and CBT-based techniques, some of which show promising results.
The heterogenous psychological approaches identified in this review contrast starkly to established guidelines for treating PTSD in the general population (as opposed to the cancer population). For example, in the UK, National Institute for Health and Care Excellence guidelines clearly outline a stepped approach to PTSD, using cognitive-based or EMDR approaches in the first instance.41 This narrative review also found that EMDR- and cognitive-based interventions were effective, alongside other approaches, and developing interventional RCTs to test out these approaches would be a useful next step. Although the UK clearly outlines treatment approaches to managing PTSD, there is a lack of robust policy specific to managing cancer-related PTSD; the 2022 10-year plan for cancer is delayed,42 and the latest National Health Service cancer programme report from 2020 is non-specific regarding meeting the emotional needs of people living with cancer.43 This is in contrast to the USA, where the National Cancer Institute advocates for screening and treatment of cancer-related PTSD.44 Furthermore, although not specific to cancer-related PTSD, development and rollout of a bespoke distress-screening tool in Toronto, Canada, led to a screening uptake of over 70% across the oncology department, suggesting that there is an appetite for screening and successful implementation of distress-screening tools, which could ultimately include cancer-related PTSD.Reference Li, Macedo, Crawford, Bagha, Leung and Zimmermann45
In addition to screening, there is a clear identified need for cancer-related PTSD treatment that is bespoke to the cancer type and individual needs. Diagnostic clarity is important in the first instance, and this review shows a variety of diagnostic tools employed across the studies. Standardising the approach to diagnosis (e.g. by using DSM-5 criteria) would help to robustly identify affected patient populations and treatment needs. Furthermore, ongoing research is needed to develop an approach to identifying de novo cancer-related PTSD as opposed to pre-existing PTSD that has been triggered by a cancer-related experience. In addition, developing and testing bespoke interventions tailored to cancer type and patient population would be useful.
Study and clinical limitations
There are limitations to this narrative review. Because of resource limitations, only English language papers were included, which could cause information bias as published research in other languages is missed from the review. Publication bias was not assessed because of the relatively small number of studies. Furthermore, there is known heterogeneity of PTSD diagnosis in included patient groups (pre-cancer diagnosis PTSD versus cancer-related PTSD). Definitions of ‘trauma’ and ‘distress’ vary in the literature, and, by restricting this review solely to patients with cancer with diagnosable PTSD, other studies that address fear of recurrence and post-traumatic stress symptoms have been omitted but may be relevant and applicable to the patient experience.Reference Kangas, Henry and Bryant46 There is also considerable heterogeneity in study participants, cancer types and quality of studies included, meaning it is difficult to draw firm conclusions about psychological interventions in PTSD in people living with cancer.
This review also noted low methodological quality in the studies included. RCTs typically failed to disclose the randomisation method used and the allocation concealment. It was unclear if the participants were subsequently informed if they were having the intervention or the control. Few studies described the drop-out rates and factors behind participants dropping out. No study mentioned intention-to-treat analysis as a management strategy and few studies calculated effect sizes.
In conclusion, PTSD in cancer is common, but there is a lack of high-quality intervention studies for PTSD in cancer. A need for diagnostic clarity and associated intervention RCTs has been identified. Additionally, a need for interventional RCTs for managing PTSD in people living with cancer has also been identified. Diagnostic clarity, using updated DSM-5 criteria for PTSD, and a consistency of patient population in terms of demographics and cancer type and stage, may enable sufficient homogeneity of studies to permit a meta-analysis. However, given the diversity of PTSD and cancer needs identified, this is unlikely to be achievable. In this regard, bespoke and specific studies that tailor the PTSD intervention to particular cancer populations under investigation is a pragmatic argument based on psychological formulation that will permit meaningful real-world data to be generated. In a similar vein, research that differentiates de novo cancer-related PTSD from patients with cancer with pre-existing PTSD is required.
Consequently, it is the authors’ intentions that this narrative review, alongside forthcoming interviews of people living with cancer and their experiences of PTSD, will inform a novel intervention to screen, diagnose and manage cancer-related PTSD. No studies to date have mentioned use of PPI in study design, and there is seemingly a lack of patient and public engagement in the designing of effectiveness studies in current PTSD and cancer research, which is a concern. Furthermore, there is a lack of robust UK policy specific to managing cancer-related PTSD, which differs from the National Institutes of Health in the USA, which advocates for screening and treatment of cancer-related PTSD.44 It is hoped the narrative reviews to date, alongside this review and PPI, will generate better-designed trials to inform local policy.
About the authors
Daniel Anderson is a consultant psychiatrist at the Department of Psych-oncology, The Christie NHS Foundation Trust, Manchester, UK. Victoria Jones is a specialty trainee (ST4) psychiatrist in adult psychiatry, Greater Manchester Mental Health NHS Foundation Trust, Manchester, UK.
Data availability
Data is available on reasonable request from the corresponding author.
Author contributions
Both authors contributed equally to the literature search, quality assessment of the literature and the production of the final text.
Funding
The study was partially funded by a grant awarded by the Manchester Academic Health Sciences Centre to the Christie NHS Foundation Trust.
Declaration of interest
None.







eLetters
No eLetters have been published for this article.